Académique Documents
Professionnel Documents
Culture Documents
Bronchioectasis
Transféré par
Corrine Ivy0 évaluation0% ont trouvé ce document utile (0 vote)
9 vues4 pagesxx
Copyright
© © All Rights Reserved
Formats disponibles
DOCX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentxx
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
9 vues4 pagesBronchioectasis
Transféré par
Corrine Ivyxx
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 4
BRONCHIECTASIS
Bronchiectasis- is a chronic, irreversible dilation of the Coughing up blood or mucus mixed with
bronchi and bronchioles. blood, a condition called hemoptysis.
Predisposing factors: Risk factors for Absent or Dysfunctional CFTR
protein in bronchial cells in cystic fibrosis (CF)
Airway obstruction
Diffuse airway injury Having a whole-body (systemic) disease
Pulmonary infections and obstruction of associated with bronchiectasis like those
the bronchus or complications of long – mentioned above.
term pulmonary infections. Chronic or severe lung infections such as
Genetic disorders such as cystic tuberculosis, or TB that damage the airways.
fibrosis
Abnormal host defense (eg, ciliary
dyskinesia or humoral Medical Management
immunodefieciency)
1. Postural drainage.
Idiopathic causes 2. Chest physiotheraphy, including percussion and
postural drainage is important in secretion
Pathophysiology
management.
Inflammatory process associated with 3. Smoking cessation is important because
pulmonary infections damages the smoking impairs bronchial drainage by
bronchial wall paralyzing ciliary action, increasing bronchial
Weakens/loss supporting structure secretions, and causing inflammation of the
which results to productions of thick mucous membranes.
secretions that obstruct the bronchi. 4. Medications- vaccinations, bronchodilator
Bronchial walls become 5. Antibiotic agents may be prescribed, throughout
distended/distorted permanently thus the winter or when acute upper respiratory tract
impedes mucucilliary clearance. infections occur.
Inflammation/infections extends to the
Nursing Management- focuses on alleviating symptoms
perbronchial tissues.
and assisting the patient to clear pulmonary secretions.
Large amount of exudates drains freely
to the lungs mostly to the upper lobe of Perform postural drainage
the lung. Avoid exposure to others with upper respiratory
Retention of secretions and subsequent and other infections.
obstruction ultimately cause the alveoli Assessed nutritional status and strategies are
distal to the obstruction to collapse implemented to ensure an adequate diet.
(atelectasis)
There is impairment in the matching of
ventilation to perfusion (ventilation-
perfusion imbalance) and hypoxemia. Typical posture of a person with COPD—primary
emphysema- The person tends to lean forward and
Symptoms of Bronchiectasis uses the accessory muscles of respiration to breathe,
focusing the shoulder girdle upward and causing
Coughing up yellow or green mucus supraclavicular fossae to retract on inspiration.
every day
Shortness of breath that gets worse Assessment
during exacerbations.
Feeling run-down or tired, especially Key factors to assess in the COPD Patient’s Health
during exacerbations. History
Fevers and/or chills, usually developing
Exposure to risk factors- types, intensity,
during exacerbations.
duration
Wheezing or a whistling sound while you
breathe.
BRONCHIECTASIS
Past medical history—resp. diseases/problems, Two forms of PTB
including asthma, allergy, sinusitis, nasal polyps,
hx of resp infection. 1. Latent TB: You have the germs in your body,
Family hx of COPD or other chronic resp but your immune system stops them from
diseases spreading. That means you don’t have any
Pattern of symptom development symptoms and youre not contagious. But the
Hx of exacerbations or previous hospitalizations infection is still alive in your body and can one
for resp problems day become active. If you are at high risk for re-
Presence of comorbidities activation----for instance, you have HIV, your
Appropriateness of current medical treatments primary infection was in the last 2 years, your
Impact of disease on quality of life chest X-ray is abnormal or you are
Available social and family support immunocompromised----your doctor will treat
Potential for reducing risk factors (eg. Smoking you with antibiotics to lower the risk for
cessation) developing active TB.
2. Active TB disease: This means the gers
multiply and can make you sick. You can spread
the disease to others. Ninety percent of adult
Pulmonary Tubercolosis (PTB) cases of active TB are from the reactivation of
latent TB infection.
Is a contagious disease bacterial infection that
involves the lungs. It may spread to other Signs and Symptoms
organs.
Most people recover from primary TB infection Cough up phlegm
without further evidence of the disease. The Cough up blood (hemoptysis)
infection may stay inactive (dormant) for years. Have a consistent fever, including low-grade
In some people, it becomes active again fevers
(reactivates) Have night sweats
Most people who develop symptoms of a TB Have chest pains
infection first became infected in the past. In Have unexplained weight loss
some cases, the disease becomes active within Fatigue
weeks after the primary infection.
Pathophysio
Once the bacteria is inhaled (droplet), it
Causative agent settles to the airway, majority of the
bacilli are trapped.
Pulmonary TB is caused by the bacterium
Droplet nuclei with bacilli are inhaled
Mycobacterium tuberculosis. TB is contagious. This
enter the lung and deposit in the alveoli.
means the bacteria is easily spread from an infected
Macrophages and T lymphocytes act
person to someone else.#
together to try to contain the infection by
Mode of Transmission forming granulomas.
In weaker immune systems, the walls
Droplets- cough or sneeze of an infected person loses integrity and the bacilli are able to
escape and spread to other alveoli or
Who are at risk?
other organs.
Older adults Pathophysio (summarized)
Infants
People with weakened immune systems, for Inhalation of bacilli
example due to HIV/AIDS, chemotherapy, Containment in a granuloma
diabetes, or medicines that weaken the immune Breakdown of the granuloma in less
system. immunocompetent individuals.
Poor nutrition
Prevention of Spread:
BRONCHIECTASIS
Take all of your medicines as they’re prescribed, cultured for growth of mycobacteria to
until your doctor takes you off them. confirm the diagnosis.
Keep all your doctor appointements. In may take one to three weeks to detect
Always cover your mouth with a tissue when you growth in a culture, but eight to 12 weeks to
cough or you sneeze. Seal the tissue in a plastic be certain of the diagnosis.
bag, then throw it away. 4. Sputum smear microscopy
Wash your hands after coughing or sneezing. To do the TB test a very thin layer of
Don’t visit other people and don’t invite them to the sample is placed on a glass
visit you. slide, and this is called a smear. A
Stay home from work, school, or other public series of special stains are then
places. applied to the sample, and the
Use a fan or open windows to move around stained slide is examined under a
fresh air. microscope for signs of the TB
Don’t use public transportation. bacteria.
Sputum smear microscopy is
Diagnostics: inexpensive and simple, and people
can be trained to do it relatively
1. Chest X-Ray- the most common diagnostic quickly and easily.
test that leads to the suspicion of infection is Results are available within hours.
a chest xray. The sensitivity though is only about
In primary TB, an xray will show an 50-60%
abnormality in the mid and lower lung
fields, and lymph nodes may be Treatment
enlarged.
Reactivated TB bacteria usually infiltrate Latent TB
the upper lobes of the lungs.
Isoniazid (INH) isonicotinylhydrazide: This is the
Miliary tuberculosis exhibits diffuse
most common therapy for latent TB. (take daily
nodules at different locations in the
for 9 months)
body.
Rifampicin take this antibiotic each day for
2. The Mantoux skin test- also known as
4months, option if you have side effects or
tuberculin skin test (TST or PPD test): This
contraindications to INH
test helps identify people infected with
Isoniazid and rifapentine: once a week for 3
M.tuberculosis but who have no symptoms.
months
A doctor must read the test.
The doctor will inject 5 units of Active TB
purified protein derivative (PPD) into
your skin. If a raised bump of more Ethambutol
than 5 mm (0.2 in) appears at the Isoniazid
site 48 hours later, the test may be Pyrazinamide
positive. Rifampicin
This test can often indicate disease
when there is none (false positive). All of these will be taken for 6-9 months
Also, it can show no disease when
you may in fact have TB (false
negative)
Latent TB
3. Sputum Testing- sputum testing for acud
fast bacilli (AFB) is the only test that TB lives but doesn’t grow in the body.
confirms a TB diagnosis. If sputum (the Doesn’t make a person feel sick or have
mucus you cough up) is available, or can be symptoms.
induced, a lab test may give a positive result Can’t spread from person to person.
in up to 30% of people with active disease. Can advance to TB disease.
Sputum or other bodily secretions such as
from your stomach or lung fluid can be Active TB
BRONCHIECTASIS
TB is active and grows in the body. Promoting airway clearance- the nurse
Makes a person feel sick and have instructs the patient about correct positioning to
symptoms. facilitate drainage and to increase fluid intake to
Can spread from person to person. promote systemic hydration.
Can cause death if not treated. Adherence to the treatment regimen- the
nurse should teach the patient that TB is a
communicable disease and must take his/her
medicines.
Multi Drug Resistance (MDR)
Promoting activity and adequate nutrition
Antibiotics called fluoroquinolones Preventing spreading of tuberculosis
An injectable antibiotic such as amikacin, infection
kanamycin, and capreomycin Acid-fast bacillus isolation
Newer and antibiotic treatments, such as Disposal
bedaquiline, ethanamide, and para-amino Monitor adverse effects
salicylic acid. These are given in addition to
other medications.
A rare and serious type of the disease is called
extensively drug-resistant TB , this means that many
of the common medications --- including isoniazid,
rifampicin, fluoroquinoloness, and atleast one of the
antibiotics that are injected--- don’t knock it out.
Research shows that it can be cured around 30% to
50% of the time.
Medication side effects
Serious side effects of TB drugs aren’t common but can
be dangerous when they do occur. All tuberculosis
medications can be highly toxic to your liver.
Nausea or vomiting
Loss of appetite
A yellow color to your skin (jaundice)
Dark urine
A fever that lasts three or more days and has no
obvious cause
Complication:
If left untreated or mistreated, pulmonary tuberculosis
may lead to:
Respiratory failure
Pneumothorax
Pneumonia
Nursing Intervention
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Why File A Ucc1Document10 pagesWhy File A Ucc1kbarn389100% (4)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- IFR CalculationDocument15 pagesIFR CalculationSachin5586Pas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Drug Study CISPLATINDocument2 pagesDrug Study CISPLATINCorrine IvyPas encore d'évaluation
- ATADU2002 DatasheetDocument3 pagesATADU2002 DatasheethindPas encore d'évaluation
- Building A Pentesting Lab For Wireless Networks - Sample ChapterDocument29 pagesBuilding A Pentesting Lab For Wireless Networks - Sample ChapterPackt PublishingPas encore d'évaluation
- Activity Evaluation Form: "Where Children Come First"Document1 pageActivity Evaluation Form: "Where Children Come First"TuTitPas encore d'évaluation
- Ch06 Allocating Resources To The ProjectDocument55 pagesCh06 Allocating Resources To The ProjectJosh ChamaPas encore d'évaluation
- History of Health EducationDocument6 pagesHistory of Health EducationCorrine Ivy100% (2)
- Benko Gambit-Jacobs and Kinsman, 1999Document163 pagesBenko Gambit-Jacobs and Kinsman, 1999johnson Greker100% (3)
- MMDST Guide: When Giving 9, 11, and 12, Do Not Name The Forms. Do Not Demonstrate 9 and 11Document3 pagesMMDST Guide: When Giving 9, 11, and 12, Do Not Name The Forms. Do Not Demonstrate 9 and 11Corrine IvyPas encore d'évaluation
- Budgetary RequirementsDocument1 pageBudgetary RequirementsCorrine IvyPas encore d'évaluation
- Cavite State University Don Severino de Las Alas CampusDocument7 pagesCavite State University Don Severino de Las Alas CampusCorrine IvyPas encore d'évaluation
- Republic of The Philippines Cavite State University Don Severino Delas Alas Campus Indang, CaviteDocument1 pageRepublic of The Philippines Cavite State University Don Severino Delas Alas Campus Indang, CaviteCorrine IvyPas encore d'évaluation
- Assignment in MedsurgDocument2 pagesAssignment in MedsurgCorrine IvyPas encore d'évaluation
- Module 2 Management TheoriesDocument15 pagesModule 2 Management TheoriesCorrine IvyPas encore d'évaluation
- Post Test Name: Rosenie H. Tanag YR/SEC: BSN 3-1 Score: - Learning ActivityDocument3 pagesPost Test Name: Rosenie H. Tanag YR/SEC: BSN 3-1 Score: - Learning ActivityCorrine IvyPas encore d'évaluation
- Laxatives: Psyllium Mucilloid (Metamucil, Others)Document3 pagesLaxatives: Psyllium Mucilloid (Metamucil, Others)Corrine IvyPas encore d'évaluation
- Assignment No.2: Effect On One of The Spheres EventDocument1 pageAssignment No.2: Effect On One of The Spheres EventCorrine IvyPas encore d'évaluation
- AsdasDocument2 pagesAsdasCorrine IvyPas encore d'évaluation
- CholecystectomyDocument2 pagesCholecystectomyCorrine Ivy100% (1)
- Acute Gastroenteritis Case StudyDocument5 pagesAcute Gastroenteritis Case StudyCorrine IvyPas encore d'évaluation
- Computer Assisted Instruction For Patient EducationDocument9 pagesComputer Assisted Instruction For Patient EducationCorrine IvyPas encore d'évaluation
- Republic of The Philippines Cavite State University Don Severino Delas Alas Campus Indang, CaviteDocument3 pagesRepublic of The Philippines Cavite State University Don Severino Delas Alas Campus Indang, CaviteCorrine IvyPas encore d'évaluation
- Vaccine 1 Dose 2 Dose 3 DoseDocument18 pagesVaccine 1 Dose 2 Dose 3 DoseCorrine IvyPas encore d'évaluation
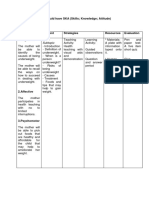
- Assessment and Eval Learning (Callada)Document53 pagesAssessment and Eval Learning (Callada)Corrine IvyPas encore d'évaluation
- Medication-List SheetDocument2 pagesMedication-List SheetCorrine IvyPas encore d'évaluation
- Laxatives: Psyllium Mucilloid (Metamucil, Others)Document3 pagesLaxatives: Psyllium Mucilloid (Metamucil, Others)Corrine IvyPas encore d'évaluation
- Plan of ActivityDocument1 pagePlan of ActivityCorrine IvyPas encore d'évaluation
- Teaching Plan For UnderweightDocument4 pagesTeaching Plan For UnderweightCorrine IvyPas encore d'évaluation
- College of Nursing KardexDocument2 pagesCollege of Nursing KardexCorrine IvyPas encore d'évaluation
- Drug Study CefuroximeDocument2 pagesDrug Study CefuroximeCorrine IvyPas encore d'évaluation
- Paramount Healthcare Management Private Limited: First Reminder Letter Without PrejudiceDocument1 pageParamount Healthcare Management Private Limited: First Reminder Letter Without PrejudiceSwapnil TiwariPas encore d'évaluation
- Acampamento 2010Document47 pagesAcampamento 2010Salete MendezPas encore d'évaluation
- MCQs - Chapters 31 - 32Document9 pagesMCQs - Chapters 31 - 32Lâm Tú HânPas encore d'évaluation
- UnixDocument251 pagesUnixAnkush AgarwalPas encore d'évaluation
- Bajaj CNSDocument3 pagesBajaj CNSAbhijit PaikarayPas encore d'évaluation
- Internship ReportDocument36 pagesInternship ReportM.IMRAN0% (1)
- 100 20210811 ICOPH 2021 Abstract BookDocument186 pages100 20210811 ICOPH 2021 Abstract Bookwafiq alibabaPas encore d'évaluation
- SEC CS Spice Money LTDDocument2 pagesSEC CS Spice Money LTDJulian SofiaPas encore d'évaluation
- Distribution BoardDocument7 pagesDistribution BoardmuralichandrasekarPas encore d'évaluation
- 0 BA Design ENDocument12 pages0 BA Design ENFilho AiltonPas encore d'évaluation
- ThaneDocument2 pagesThaneAkansha KhaitanPas encore d'évaluation
- Assignment Csi104Document11 pagesAssignment Csi104Minh Lê KhảiPas encore d'évaluation
- Toi Su20 Sat Epep ProposalDocument7 pagesToi Su20 Sat Epep ProposalTalha SiddiquiPas encore d'évaluation
- Docsity Detailed Lesson Plan 5Document4 pagesDocsity Detailed Lesson Plan 5Sydie MoredoPas encore d'évaluation
- Usm 1Document47 pagesUsm 1Abhishek KumarPas encore d'évaluation
- HandsoutDocument3 pagesHandsoutloraine mandapPas encore d'évaluation
- BIOBASE Vortex Mixer MX-S - MX-F User ManualDocument10 pagesBIOBASE Vortex Mixer MX-S - MX-F User Manualsoporte03Pas encore d'évaluation
- Fire Technical Examples DIFT No 30Document27 pagesFire Technical Examples DIFT No 30Daniela HanekováPas encore d'évaluation
- How To Present A Paper at An Academic Conference: Steve WallaceDocument122 pagesHow To Present A Paper at An Academic Conference: Steve WallaceJessicaAF2009gmtPas encore d'évaluation
- Buildingawinningsalesforce WP DdiDocument14 pagesBuildingawinningsalesforce WP DdiMawaheb ContractingPas encore d'évaluation
- Course Projects PDFDocument1 pageCourse Projects PDFsanjog kshetriPas encore d'évaluation
- 3rd Page 5Document1 page3rd Page 5api-282737728Pas encore d'évaluation
- Unit 1 and 2Document4 pagesUnit 1 and 2Aim Rubia100% (1)