Académique Documents
Professionnel Documents
Culture Documents
Other - LINK 2 - Primary Biliary Cirrhosis PDF
Transféré par
Abhilash Kl0 évaluation0% ont trouvé ce document utile (0 vote)
12 vues2 pagesTitre original
other_LINK-2_Primary-Biliary-Cirrhosis.pdf
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
12 vues2 pagesOther - LINK 2 - Primary Biliary Cirrhosis PDF
Transféré par
Abhilash KlDroits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 2
From the American Liver Foundation
www.liverfoundation.org
Primary Biliary Cirrhosis (PBC)
Explore this section to learn more about primary biliary cirrhosis, including a description of the disease and
how it's diagnosed.
What is primary biliary cirrhosis?
Primary biliary cirrhosis, or PBC, is a chronic, or long-term, disease of the liver that slowly destroys the medium-
sized bile ducts within the liver. Bile is a digestive liquid that is made in the liver. It travels through the bile ducts to
the small intestine, where it helps digest fats and fatty vitamins.
In patients with PBC, the bile ducts are destroyed by inflammation. This causes bile to remain in the liver, where
gradual injury damages liver cells and causes cirrhosis, or scarring of the liver. As cirrhosis progresses and the
amount of scar tissue in the liver increases, the liver loses its ability to function. Cirrhosis also prevents blood from
the intestines from returning to the heart.
PBC advances slowly. Many patients lead active and productive lives for more than 10 to 15 years after diagnosis.
Patients who show no symptoms at the time of diagnosis often remain symptom-free for years. Patients who have
normal liver tests on treatment may have a normal life expectancy. PBC is a chronic illness and may lead to life-
threatening complications, especially after cirrhosis develops.
What are the signs and symptoms of PBC?
Many people with PBC do not have symptoms, especially in the early stages of the disease. When symptoms do
occur the most common is pruritus, or intense itching of the skin, often in the arms, legs and back. Other
symptoms may include fatigue, jaundice, fluid build-up in the ankles and abdomen, and darkening of the skin and
collection of fatty deposits in the skin around the eye. Jaundice, is an indication of how far the disease has
progressed.
Several other disorders often occur with PBC. The most common is problems with the tear and salivary glands,
causing dry eyes or mouth. Arthritis and thyroid problems may also be present. Renal stones and gallstones may
develop. Bone softening and fragility leading to fractures can occur in late stages of the disease.
What causes PBC?
The cause of this disease is unknown. It may be related to problems in the immune system. Although PBC is
technically not a hereditary disease, meaning a disease caused by a specific gene or genetic defect that is passed from
parent to child, there appears to be some family link. PBC is more common among siblings and in families where one
member has been affected.
How is PBC diagnosed?
Because many PBC patients have no symptoms, the disease is often discovered through abnormal results on routine
liver blood tests. Doctors need to do several tests to confirm a diagnosis of primary biliary cirrhosis. One test looks
for the presence of antimitochondrial antibodies (AMA) in the blood. This test is positive in nearly all PBC patients.
Ultrasound exams and a liver biopsy, in which a small sample of liver tissue is removed with a needle, may also be
performed.
How is PBC treated?
Patients most often take a daily dose of a drug called ursodiol. This is urseodeoxycholic acid, a naturally occurring
bile acid. This drug improves the liver’s ability to function in PBC patients. It also extends life expectancy and may
delay the need for a liver transplant. The recommended dose is 15 mg per kilogram of body weight, and the
medication must be taken every day for life, or until a liver transplant. Patients rarely experience side effects from
ursodiol. Other drugs are effective at relieving the symptoms of PBC, including the itching.
If I’ve been diagnosed with PBC, what questions should I ask my doctor about PBC?
“How severe is the liver damage?”
“What treatment do you recommend? Will this slow down the
progression of the disease?”
“Will any medication be prescribed? What are the side effects?”
“Should I change my diet?”
“Are there any supplements you would suggest that I take?”
“What can be done to relieve my symptoms?”
“If cirrhosis develops, is transplantation my only option?”
What lifestyle changes may be helpful for PBC patients?
Maintaining a healthy lifestyle will help patients feel better and may relieve or prevent some of the secondary
symptoms of PBC. Your doctor may recommend:
A reduced sodium diet
Drinking ample water
Taking calcium and Vitamin D supplements
Avoiding or reducing the consumption of alcohol
Reducing stress
Exercising, particularly walking
Skin Care
Regular dental examinations
Artificial tears for dry eyes
Who is at risk for PBC?
Women account for about 90 percent of PBC cases. It is most commonly diagnosed in patients between the age of
35 and 60.
What is being done to find a cure for PBC?
PBC has been known for more than 100 years, but now doctors are able to diagnose it very early. This means that
treatment can begin before the liver is severely damaged. Scientists are continuing to study the disease to find the
cause and understand its development.
In addition, investigators are exploring the use of several additional medications to lessen the symptoms and control
liver damage through drug therapy trials, involving a large number of patients around the world.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- NCP CysticDocument2 pagesNCP Cysticapi-30271420250% (2)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
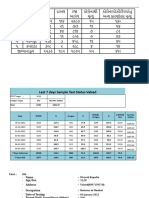
- Statistical Consulting ServicesDocument3 pagesStatistical Consulting Servicesbioepinet1Pas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hand Foot Mouth DiseaseDocument11 pagesHand Foot Mouth DiseaseedelinPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Gangguan Elminasi Pada Ibu HamilDocument10 pagesGangguan Elminasi Pada Ibu HamilRismawatiPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Influenza 1918.0910Document19 pagesInfluenza 1918.0910RafaelPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Diaz 2009Document1 pageDiaz 2009Nasrudin EfendiPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Second MBBS Microbiology SyllabusDocument29 pagesSecond MBBS Microbiology SyllabusUday KolhePas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Kkn5uppzf2x2maa4akdil3ljDocument1 pageKkn5uppzf2x2maa4akdil3ljAtul Sharma0% (1)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Pathophysiology - Pharm D-Ii YearDocument8 pagesPathophysiology - Pharm D-Ii Yearshasvina05Pas encore d'évaluation
- Deadly 'Black Fungus' Surges Among India's COVID-19 PatientsDocument2 pagesDeadly 'Black Fungus' Surges Among India's COVID-19 Patientskaye choiPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Case StudyDocument4 pagesCase StudyMargarita Limon BalunesPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Epidemiology TriangleDocument1 pageEpidemiology TriangleMelDred Cajes BolandoPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Covid PresentationDocument43 pagesCovid PresentationSr. Section Engineer Coaching Depot-ValsadPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Giardiasis: Giardia Enteritis Lambliasis Beaver FeverDocument16 pagesGiardiasis: Giardia Enteritis Lambliasis Beaver FeverAnonymous Ssp49pRWPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Cerebral InfractionDocument2 pagesCerebral InfractionEdsel MagnoPas encore d'évaluation
- EDITABLE School Form 8 SF8 Learners Basic Health Nutritional ReportDocument17 pagesEDITABLE School Form 8 SF8 Learners Basic Health Nutritional ReportSherelyn Labrado LucasPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Mapeh Report of Prevention and Control of Substance and AbuseDocument8 pagesMapeh Report of Prevention and Control of Substance and AbuseCrissa BuenavistaPas encore d'évaluation
- Alsangedy Bullets For Paces Churg-Strauss SyndromeDocument2 pagesAlsangedy Bullets For Paces Churg-Strauss SyndromeGhulamMemonPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Balantidium ColiDocument12 pagesBalantidium Colidaenil_oliverPas encore d'évaluation
- CPG Spinal EmergenciesDocument3 pagesCPG Spinal Emergenciesvashini9151Pas encore d'évaluation
- Hepato Splenomegaly: IAP UG Teaching Slides 2015-16Document20 pagesHepato Splenomegaly: IAP UG Teaching Slides 2015-16AnchalPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Elements of PlotDocument4 pagesElements of PlotNIMALLANPas encore d'évaluation
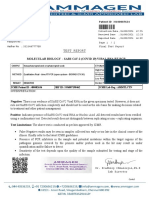
- Test Report: Patient ID 0100007634 Sid NoDocument2 pagesTest Report: Patient ID 0100007634 Sid NoBalamurugan ArumugamPas encore d'évaluation
- Adcon Group 14Document34 pagesAdcon Group 14TMC PGI GENER MICKOPas encore d'évaluation
- Colorectal CancerDocument11 pagesColorectal CancerMithilaa SPas encore d'évaluation
- PAFP Consensus Guidelines On Community-Oriented Care During A COVID-19 EpidemicDocument16 pagesPAFP Consensus Guidelines On Community-Oriented Care During A COVID-19 EpidemicDan Paul AmiscuaPas encore d'évaluation
- LR 364372Document9 pagesLR 364372Fredgar22Pas encore d'évaluation
- GastritisDocument6 pagesGastritisNader Smadi100% (5)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- As Fluid Volume Deficit (FVD), Hypovolemia) Is ADocument2 pagesAs Fluid Volume Deficit (FVD), Hypovolemia) Is ATanya Alyssa Untalan AquinoPas encore d'évaluation
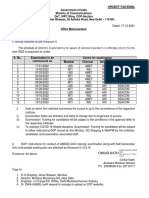
- GMDSS Exam Schedule For Year 2022Document7 pagesGMDSS Exam Schedule For Year 2022Mani ThapaPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)