Académique Documents
Professionnel Documents
Culture Documents
Protective Factors For Child Development at Age 2 in The Presence of Poor Maternal Mental Health: Results From The All Our Babies (AOB) Pregnancy Cohort
Transféré par
AndikTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Protective Factors For Child Development at Age 2 in The Presence of Poor Maternal Mental Health: Results From The All Our Babies (AOB) Pregnancy Cohort
Transféré par
AndikDroits d'auteur :
Formats disponibles
Open Access Research
Protective factors for child development
at age 2 in the presence of poor
maternal mental health: results from the
All Our Babies (AOB) pregnancy cohort
Sheila W McDonald,1 Heather L Kehler,1 Suzanne C Tough2
To cite: McDonald SW, ABSTRACT
Kehler HL, Tough SC. Strengths and limitations of this study
Objective: To identify the combination of factors most
Protective factors for child
protective of developmental delay at age 2 among ▪ A community-based multimethods recruitment
development at age 2 in the
children exposed to poor maternal mental health. strategy was implemented to obtain a socio-
presence of poor maternal
mental health: results from Design: Observational cohort study. economically and ethnically diverse sample of
the All Our Babies (AOB) Setting: Pregnant women were recruited from primary women representative of the parenting popula-
pregnancy cohort. BMJ Open healthcare offices, the public health laboratory service tion in Calgary, Canada.
2016;6:e012096. and community posters in Calgary, Alberta, Canada. ▪ Comprehensive questionnaire and medical record
doi:10.1136/bmjopen-2016- Participants: 1596 mother–child dyads who data were collected spanning pregnancy, birth,
012096 early postpartum and early childhood providing a
participated in the All Our Babies study and who
completed a follow-up questionnaire when their child unique opportunity to consider multiple protect-
▸ Prepublication history and was 2 years old. Among participants who completed ive factors for child development in the context
additional material is the 2-year questionnaire and had complete mental of poor maternal mental health.
available. To view please visit health data (n=1146), 305 women (27%) were ▪ The primary outcome, child development pro-
the journal (http://dx.doi.org/ blems, was based on parent report on standar-
classified as high maternal mental health risk.
10.1136/bmjopen-2016-
Primary measures: Child development at age 2 was dised measures, not clinical diagnoses, and
012096).
described and a resilience analysis was performed therefore the possibility for misclassification
among a subgroup of families at maternal mental must be considered when interpreting the find-
Received 30 March 2016 health risk. The primary outcome was child ings of this analysis.
Revised 8 October 2016 development problems. Protective factors were ▪ The sociodemographics of participants, including
Accepted 13 October 2016 identified among families at risk, defined as maternal the percentage with higher household incomes,
mental health risk, a composite measure created secondary education and committed relation-
from participants’ responses to mental health life ships, while representative of the pregnant and
course questions and standardised mental health parenting population in an urban centre in
measures. Canada, may be higher than that observed in
Results: At age 2, 18% of children were classified other populations, and therefore the generalis-
as having development problems, 15% with ability of our findings to other populations
behavioural problems and 13% with delayed social– should be interpreted with caution.
emotional competencies. Among children living in a ▪ Attrition of the longitudinal sample may further
family with maternal mental health risk, protective limit generalisability.
factors against development problems included
1
Department of Pediatrics,
higher social support, higher optimism, more
Cumming School of relationship happiness, less difficulty balancing work INTRODUCTION
Medicine, University of and family responsibilities, limiting the child’s screen A developmental delay is described as not
Calgary, Calgary, Alberta, time to <1 hour per day and the child being able to reaching a developmental milestone by the
Canada fall asleep in <30 min and sleeping through the night expected age.1 Recent studies in Canada and
2
Departments of Pediatrics by age 2. the USA suggest that developmental delays
and Community Health Conclusions: Among families where the mother has
Sciences, Cumming School
affect an estimated 11–21% of preschool
poor mental health, public health and early aged children.2 3 By kindergarten, at ∼age
of Medicine, University of
intervention strategies that support interpersonal 5 years, current population-level data in
Calgary, Calgary, Alberta,
Canada
relationships, social support, optimism, work–life
Canada suggest that the percentage of chil-
balance, limiting children’s screen time and
establishing good sleep habits in the child’s first
dren with a developmental vulnerability is
Correspondence to
Dr Sheila W McDonald; 2 years show promise to positively influence early 25–30%.4
SheilaW.McDonald@ child development. Early developmental delays are associated
albertahealthservices.ca with future negative outcomes including
McDonald SW, et al. BMJ Open 2016;6:e012096. doi:10.1136/bmjopen-2016-012096 1
Open Access
lower school readiness and poor school performance.5 6 involving primary healthcare offices, community posters
Social–emotional delays and behavioural problems at and the public health laboratory service (Calgary
preschool age are associated with later negative out- Laboratory Service). This multimethod strategy was
comes at school age including ongoing behaviour pro- designed to obtain a socioeconomically and ethnically
blems,7 8 psychiatric disorders8 and negative social diverse sample of women representative of the parenting
outcomes including less social acceptance9 and a limited population in an urban Canadian centre. Recruitment
ability to form and maintain quality friendships.10 began in May 2008 and was completed in December
Maternal depression is an established risk factor for 2010. Women were eligible to participate in the AOB
child developmental delay.11 In a recent review, maternal study if they were <24 weeks and 6 days gestation at the
mental health problems in pregnancy and/or the post- time of enrolment, they were 18 years of age or older,
partum period were found to increase the likelihood that they lived in the greater Calgary area and they were able
school age children experienced suboptimal global, to complete a written questionnaire in English. Women
behavioural, cognitive and socioemotional develop- were excluded from the AOB study if they planned to
ment.11 Poor maternal mental health is common, with move outside the greater Calgary area during their preg-
recent studies reporting that 25% of women are affected nancy. Detailed descriptions of the AOB study design and
at some time between conception and 1 year post- methods have previously been described.14
partum.12 Therefore, children whose mothers experience
poor mental health represent a significant high-risk Participant follow-up
group for early developmental delay. Despite this adver- Eligible participants for each follow-up questionnaire
sity, some children do not experience any delay in devel- were contacted and invited to participate over the tele-
opment and seem to have a resilience that suggests there phone. At follow-up waves, only those participants who
may be factors that can play a protective role. A better were deemed eligible according to their child’s age were
understanding of protective factors has important impli- mailed questionnaires. Starting at the 1 year follow-up,
cations for public health and early intervention strategies the sample size decreased due to timing of questionnaire
to optimise early child development. design and implementation, ethics approval, funding con-
Early child development is a dynamic process occurring straints and attrition. Women who agreed to participate
over time and influenced by genetics, in utero develop- were mailed a written questionnaire and a postage paid
ment and prenatal and postnatal environmental factors.13 return envelope to return the completed questionnaire
Consequently, a comprehensive investigation of factors to the research team. Participants were contacted if ques-
across pregnancy, birth, early postpartum and early child- tionnaire data were missing or clarification of responses
hood would provide the strongest evidence to inform was required. Participants who did not return the com-
early identification and intervention. The All Our Babies pleted questionnaire were contacted by telephone and
(AOB) study, with its prospective data collection strategy email to provide an opportunity for a repeat mail-out or
including five questionnaires from mid-pregnancy to to complete the questionnaire over the phone.
2 years postpartum, provides a unique opportunity to con-
sider multiple protective factors for child development in Data collection
the context of poor maternal mental health. The AOB questionnaires were developed with input
The objective of the present study was to describe from healthcare providers, epidemiologists and commu-
child development at age 2 and to identify factors most nity programme experts. Standardised measures were
protective of developmental and behavioural problems included as part of the questionnaires when available.
among a subgroup of children exposed to poor mater-
nal mental health. Main outcome: child development
Two standardised instruments: (1) the Ages and Stages
Questionnaire (ASQ)15 and (2) the Brief Infant-Toddler
METHODS Social and Emotional Assessment (BITSEA)16 17 were used
The AOB study is a prospective community-based preg- to measure the primary outcome of child development.
nancy cohort of ∼3000 women and their children.14 The ASQ measures five domains of development
Women were recruited during pregnancy and asked to (communication, gross motor, fine motor, problem
complete three questionnaires and to consent to provide solving and personal–social).15 The ASQ shows excellent
the research team with access to their obstetrical and indices of reliability and validity.18 In accordance with
birth records. Those who consented to be contacted for the author’s scoring instructions, the risk category of
future research were asked to participate in subsequent each domain was defined as scoring 1 SD below the
follow-up questionnaires when their child was 1 and mean of the ASQ normative data, which classifies chil-
2 years old. dren as scoring in at least the ‘monitoring zone’ and
potentially the ‘referral zone’.15 At 2 SDs below the
Participant recruitment mean, children are considered to be in the ‘referral
The initial sample for the AOB cohort was obtained zone’. Given the low cell sizes for this latter category in
through a community-based recruitment strategy our sample, we used the 1 SD cut-off. An overall
2 McDonald SW, et al. BMJ Open 2016;6:e012096. doi:10.1136/bmjopen-2016-012096
Open Access
composite measure of child development was defined as Data analysis
scoring ‘at risk’ in at least two of the five domains on Stata (V.12.1) was used to conduct all statistical analyses.
the ASQ, which aligns with an overall proportion of A complete case approach was used for all analyses.
delay as seen in the literature, ranging from 12% to Descriptive statistics were used to describe participant
16%.19 20 characteristics and child development outcomes at age
The BITSEA measures child behavioural problems 2. Frequencies and percentages were calculated for cat-
(aggression, defiance, overactivity, negative emotionality, egorical variables and means and SDs were calculated
anxiety and withdrawal) and social–emotional compe- for continuous variables.
tencies (empathy, prosocial behaviours and compli- Among the subgroup of participants exposed to
ance).16 17 The two BITSEA subscales have been found higher maternal mental health risk, an initial bivariate
to have satisfactory reliability and validity.16 Using the analysis was conducted to identify factors that were pro-
standardised scoring cut-offs from the published norma- tective for each of the child development outcomes.
tive data, children were categorised with behavioural Associations were assessed using Pearson’s χ2 test or
problems if they scored at or below the 25th centile of Fisher’s exact test when cell counts were fewer than five.
normative data and children were categorised with Risk factors identified at the bivariate level based on stat-
delayed social–emotional competencies if they scored at istical significance at the p<0.10 level were considered
or below the 15th centile of normative data.17 for inclusion in the subsequent multivariable models.
For both child development outcomes, multivariable
logistic regression modelling was conducted to identify
Maternal mental health risk
the independent protective factors most strongly asso-
Previous research by our team and others has identified
ciated with child development in the presence of mater-
that the accumulation of adverse experiences confers
nal mental health risk. A manual stepwise approach was
the greatest risk to maternal mental health in the post-
used to build the models, with blocks of variables being
partum period.11 21 Consequently, we incorporated a life
added in sequential steps in the following order: (1)
course approach to the definition of maternal mental
sociodemographic variables; (2) pregnancy and birth
health risk defined as experiencing two or more of the
outcome variables; (3) postpartum variables (up to
following: a history of any abuse; a history of any mental
1 year postpartum); and (4) parenting, childcare envir-
health disorder; depression or anxiety during preg-
onment and community resource use variables (between
nancy; depression or anxiety at 4 months postpartum; or
1 and 2 years postpartum). To best address the research
depression or anxiety at 1 year postpartum. Standardised
objectives, these blocks were ordered conceptually in
measures included the Edinburgh Postnatal Depression
temporal order, and from least to most modifiable.
Scale (EPDS),22 the Centre for Epidemiologic Studies
Statistical significance was set at p<0.05 for inclusion in
Depression Scale (CES-D)23 and the Spielberger State
the next step of the logistic regression modelling; vari-
Anxiety Inventory (SAI).24 This definition of maternal
ables in previous blocks that became non-significant on
mental health risk has been used in previous studies
inclusion of a subsequent block of variables were
examining protective factors for child development
removed at the final step. Model robustness was checked
in the presence of elevated risk and resilience
by adding in, one at a time, variables that were previ-
analyses.2 21 25
ously removed. Adjusted ORs with 95% CIs were calcu-
lated. Final, parsimonious models are presented.
Independent variables
Among the subgroup of families with maternal mental
health risk, protective factors examined included maternal RESULTS
sociodemographics, maternal social support, maternal opti- Maternal participant characteristics
mism, maternal relationship happiness, maternal commu- Two-year follow-up questionnaire data were collected
nity resource use, birth outcomes, childcare arrangement, between October 2011 and October 2013. In total, 2106
child sleep habits, child screen time, child physical activity women from the AOB study were eligible to participate
level, child second language exposure, maternal working in the 2-year follow-up, of whom 1596 completed and
status and parenting outcomes. Standardised measures returned the questionnaire for a participation rate of
included the Medical Outcomes Study Social Support 75.2%.
Survey (MOS-SSS),26 the Life-Orientation Test-Revised The majority of participants were married or in a
(LOT-R),27 the Parenting Morale Index (PMI)28 and the common law relationship (96%), had postsecondary
National Longitudinal Survey of Children and Youth Social education (92%), had household incomes above
Support Scale (NLSCY-SSS).29 All potential protective $60 000 (85%), were born in Canada (81%) and
factors for child development examined in this study are described their ethnicity as white or Caucasian (82%).
described in detail in online supplementary appendix A. The average age of women at the 2-year follow-up was
Participants provided informed consent at the time of 33.9 years (SD=4.4). At 2 years postpartum, 13% of
recruitment and were provided with copies of the women had symptoms of depression and 15% of women
consent form for their records. had symptoms of anxiety (table 1).
McDonald SW, et al. BMJ Open 2016;6:e012096. doi:10.1136/bmjopen-2016-012096 3
Open Access
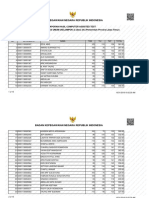
Table 1 Maternal participant characteristics Table 2 Child development outcomes at age 2
Characteristic N N (%) Child characteristics N N (%)
Marital status 1596 Communication development (ASQ) 1403
Married/common law 1536 (96.24) Not delayed 1205 (85.89)
Single/separated/divorced/ 60 (3.76) Delayed 198 (14.11)
widowed Gross motor development (ASQ) 1408
Maternal education 1584 Not delayed 1217 (86.43)
High school or less 132 (8.33) Delayed 191 (13.57)
Some college, university or trade 1202 (75.89) Fine motor development (ASQ) 1400
Postgraduate studies 250 (15.78) Not delayed 1238 (88.43)
Total household income (before 1303 Delayed 162 (11.57)
taxes and deductions) Problem-solving development (ASQ) 1401
>$60 000 199 (15.27) Not delayed 1203 (85.87)
$60 000–$79 999 210 (16.12) Delayed 198 (14.13)
$80 000 or more 894 (68.61) Personal social development (ASQ) 1407
Born in Canada 1585 Not delayed 1183 (84.08)
Yes 1276 (80.50) Delayed 224 (15.92)
No 309 (19.50) Overall child development (ASQ) 1383
Ethnicity 1584 0–1 delayed domains 1139 (82.36)
White/Caucasian 1301 (82.13) 2–5 delayed domains 244 (17.64)
Other 283 (17.87) Social–emotional abilities 1579
Maternal age, mean (SD) 1567 33.91 (4.42) (eg, empathy, prosocial behaviours
Depression (CES-D) 1596 and compliance; BITSEA)
No (CES-D<16) 1396 (87.47) No problems 1369 (86.70)
Yes (CES-D≥16) 200 (12.53) Possible deficit/delay range 210 (13.30)
Anxiety (SAI) 1576 Behavioural problems 1580
No (SAI<40) 1334 (84.64) (eg, aggression, defiance,
Yes (SAI≥40) 242 (15.36) overactivity, negative emotionality,
Data reported from most recent time point available. anxiety and withdrawal; BITSEA)
CES-D, the Centre for Epidemiologic Studies Depression Scale; No problems 1344 (85.06)
SAI, the Spielberger State Anxiety Inventory. Possible problems 236 (14.94)
ASQ, the Ages and Stages Questionnaire; BITSEA, the Brief
Infant-Toddler Social and Emotional Assessment.
Comparison of sample characteristics among those
who participated at baseline and those who remained at
Among women with mental health risk, 77% had a
follow-up showed that continuing participants were
history of mental health disorder(s) and 58% had a
more likely to have higher socioeconomic status (SES),
history of experiencing abuse. Among women cate-
to be older, to be in a stable relationship and to be born
gorised with mental health risk, 20% had symptoms of
in Canada (unpublished results).
depression during pregnancy, 17% at 4 months post-
partum, 21% at 1 year postpartum and 30% at 2 years
Child development outcomes at 2 years postpartum. The proportion of women categorised with
At age 2, 14% of children were identified with a commu- mental health risk with anxiety symptoms during preg-
nication delay, 14% with a gross motor delay, 12% with a nancy, 4 months postpartum, 1 year postpartum and
fine motor delay, 14% with a problem-solving delay and 2 years postpartum was 38%, 42%, 47% and 37%,
16% with a personal–social delay, using the 1 SD cut-off respectively.
(at least the ‘monitoring zone’; table 2). At 2 years of Among children with mothers with high maternal
age, 18% of children scored ‘at risk’ in two or more mental health risk, 18% of children had developmental
domains on the ASQ. Using the BITSEA, 13% of chil- problems. Factors most protective of ‘at-risk’ develop-
dren had delayed social–emotional abilities and 15% ment status at age 2 on the ASQ were having a mother
had behavioural problems at age 2 (table 2). with higher social support during pregnancy, and more
relationship happiness at 1 year postpartum (table 3).
Among children with mothers with high maternal
Resilience analysis: protective factors that mitigate the mental health risk, 16% of children had delayed social–
risk for developmental delay in the context of maternal emotional abilities. Factors most protective of social–
mental health risk emotional problems at age 2 on the BITSEA were having
Among participants who completed the 2-year question- a mother who reported more relationship happiness at
naire (and for whom complete mental health data were 1 year postpartum, less difficulty balancing family, work
available (n=1146)), 305 women (27%) were classified and other responsibilities and the child being exposed to
as high maternal mental health risk. <1 hour of screen time per day (table 4).
4 McDonald SW, et al. BMJ Open 2016;6:e012096. doi:10.1136/bmjopen-2016-012096
Open Access
Table 3 Model of protective factors for overall child development (ASQ) among children with mothers with high maternal
mental health risk (n=266)
Factor OR 95% CI p Value
Social support during pregnancy (MOS-SSS)
Higher (MOS-SSS>69) 2.56 1.29 to 5.09 0.007
Lower (MOS-SSS≤69) Ref . .
Happiness in their relationship at 1 year postpartum
More happiness 2.76 1.31 to 5.81 0.008
Less happiness Ref . .
ASQ, the Ages and Stages Questionnaire; MOS-SSS, the Medical Outcomes Study-Social Support Survey.
Table 4 Model of protective factors for social–emotional development (BITSEA) among children with mothers with high
maternal mental health risk (n=289)
Factor OR 95% CI p Value
Happiness in their relationship at 1 year postpartum
More happiness 2.34 1.10 to 5.00 0.028
Less happiness ref . .
Mother’s perceived ability to fulfil family, work or other responsibilities when child was 2 years old
It is never or sometimes difficult 2.07 1.02 to 4.20 0.044
It is difficult most of the time/it is always difficult ref . .
Screen time per day (television, movies/DVDs, computer/tablet)
>1 hour 2.23 1.09 to 4.53 0.027
1 hour or more ref . .
BITSEA, the Brief Infant-Toddler Social and Emotional Assessment.
Among children with mothers with high maternal performance.31 Our findings extend this research by
mental health risk, 24% of children had behavioural pro- identifying that good sleep habits may act as a protective
blems. Factors most protective of behaviour problems at factor for child social–emotional and behavioural devel-
age 2 on the BITSEA were having a mother who opment when mothers are experiencing poor mental
reported higher optimism during pregnancy, less diffi- health. It is hypothesised that having a child who sleeps
culty balancing family, work and other responsibilities, well provides mothers, especially those with mental
the child being able to fall asleep in <30 min at night health concerns, with a reprieve from the demands of
and sleeping through the night by age 2 (table 5). caring for a young child. Consequently, educating and
Given the importance of SES and certain demo- providing parents with strategies on how to establish
graphic factors (eg, born in Canada, maternal age) for healthy sleep habits, including self-settling skills, may be
child development, all final multivariable models were a low cost, effective strategy to reduce the risk of adverse
checked for robustness by examining the extent to child development outcomes.
which SES or demographic variables confounded the The negative consequences of marital dissatisfaction
associations. None of these variables were significant and marital conflict on child development including
predictors during final model building and did not con- insecure parent–child attachment, externalising and
found the associations for any child outcome. internalising behaviour problems and social difficulties
have previously been reported.32 33 Our findings add
to this research by suggesting that in the presence of
DISCUSSION poor maternal mental health, relationship happiness
Using a community sample of mothers and children in a may protect children from the negative developmental
major urban centre in Canada, this study described consequences of poor maternal mental health. Public
developmental problems at age 2 and identified protect- health well-baby visits and parenting programmes
ive factors for developmental problems in a subgroup of could screen mothers of young children for poor
families with maternal mental health risk. Maternal mental health and relationship happiness to assist with
mental health risk was common, affecting 27% of identifying families who may benefit from additional
women in our sample, which is similar to previously supports and wellness strategies. Programmes that are
reported rates of 25%.12 targeted at parents of young children could include
Poor sleep habits have previously been linked to poor content that addresses the stresses of parenting and
child developmental outcomes including child behav- the value of communication and conflict resolution
iour problems,30 poorer learning capacity and academic strategies.
McDonald SW, et al. BMJ Open 2016;6:e012096. doi:10.1136/bmjopen-2016-012096 5
Open Access
Table 5 Model of protective factors for behavioural development (BITSEA) among children with mothers with high maternal
mental health risk (n=301)
Factor OR 95% CI p Value
Optimism during pregnancy (LOT-R)
Higher (LOT-R>13) 2.18 1.20 to 3.98 0.010
Lower (LOT-R≤13) ref . .
Mother’s perceived ability to fulfil family, work or other responsibilities when child was 2 years old
It is never or sometimes difficult 2.03 1.10 to 3.75 0.023
It is difficult most of the time/it is always difficult Ref . .
Time it takes child to fall asleep at night (in general)
30 min or less 2.17 1.10 to 4.27 0.026
More than 30 min Ref . .
When child started sleeping through the night
Before 2 years 2.83 1.32 to 6.07 0.008
Is not sleeping through the night yet Ref . .
LOT-R, the Life-Orientation Test-Revised; BITSEA, the Brief Infant-Toddler Social and Emotional Assessment.
Maternal social support has previously been identified Mothers were asked to describe their ability to fulfil
as a protective factor for child development out- family, work or other responsibilities (eg, volunteer
comes.21 34 Our findings extend the current research by work, household duties and other children) since giving
suggesting that, among mothers with poor mental birth to their child. Among mothers experiencing poor
health, establishing a strong social support network as mental health, those who reported ‘it is difficult most of
early as possible in pregnancy has ongoing protective the time’ or ‘it is difficult all of the time’ were more
effects on children’s development up to age 2. Primary likely to have a child with a social–emotional delay or
care, public health, prenatal and parenting programmes behaviour problems at age 2 compared with mothers
could inform parents about the importance of establish- who reported ‘it is never or sometimes difficult’. This
ing a social support network, and help parents identify concept of challenges and conflict among women’s life
places where support networks can be developed in roles has been well documented in the literature.40
community and other settings. Indeed, this is supported Challenges with balancing family and work roles is asso-
by a Swedish study that found that participation in child- ciated with increased rates of depression, stress, anxiety
birth and parenthood education classes in the post- and lower life satisfaction.40 Parental stress and poor
partum period expanded the social network for new maternal coping have been found to be associated with
mothers.35 child behaviour problems.41 Our findings suggest that
Optimism was identified as a protective factor for supporting new parents with strategies to prevent
child behavioural development among children cared parents from feeling overwhelmed with balancing their
for by mothers with mental health problems. Optimism roles and responsibilities provides an opportunity to
is defined as a relatively stable, general tendency of indi- improve early child social–emotional and behavioural
viduals to expect positive outcomes in life.36 In this development in contexts of poor maternal mental
study, maternal optimism was measured during preg- health.
nancy, but given the stability of this trait over time, it is An association between early childhood television
likely that mothers reporting higher optimism during exposure and child behaviour problems has previously
pregnancy would continue to report higher optimism in been reported.42–44 Our findings add to the current
the early parenting years. Optimistic individuals are research by suggesting that limiting all forms of screen
more likely to adapt to stressors more effectively,37 sug- time, including television, computers, tablets and smart-
gesting that optimistic mothers may be better able to phones to <1 hour per day, may decrease the risk of
adapt to their new role as a parent and the associated developmental delay in young children exposed to poor
challenges of raising a young child. Optimism has also maternal mental health. Since society, including young
been linked to positive parenting practices.38 These find- children, spends more time on tablets, smartphones and
ings, linking maternal optimism to improved coping computers, it will be important in future research to
with stress and effective parenting practices, may help to consider screen time from all types of media, not just
explain how maternal optimism may play a role in chil- television viewing. Limiting all forms of screen time to
dren’s behavioural development. Although dispositional <1 hour per day at age 2 may provide a simple strategy
optimism is a relatively stable trait, research indicates to share with parents of young children to protect
that, to some extent, optimism can be taught,39 and against developmental delays.
therefore early intervention and parenting programmes We further examined protective factors for child devel-
could include content aimed at cultivating maternal opment problems among the remaining group of fam-
optimism. ilies without identified maternal mental health risk
6 McDonald SW, et al. BMJ Open 2016;6:e012096. doi:10.1136/bmjopen-2016-012096
Open Access
(results not shown). Although some protective factors recruitment to provincial and national statistics show
were common to both groups, others were specific to that a greater proportion of women in AOB had higher
families with mental health risk, which supports the sug- incomes and were married. In addition, there is the
gestion for targeted interventions. Unique protective potential for selection bias given the attrition and differ-
factors in high-risk settings included higher social ent sample characteristics between participants at
support in pregnancy and relationship happiness in the recruitment and those remaining at 2 years; those
first postpartum year; these factors were not found to be remaining at follow-up in the early years were more
protective in low-risk settings. Common protective likely to have higher SES, to be older, to be in a stable
factors, improving mother’s coping skills to balance relationship and to be born in Canada.
work and family life, enhancing maternal optimism in
the early parenting years, limiting children’s screen time
and establishing good sleep habits, suggest opportunities CONCLUSIONS
to apply universal intervention strategies. This study further supports previous findings that poor
A limitation of this study was the use of parent report maternal mental health through the perinatal and first
measures, the ASQ and the BITSEA to operationalise two postpartum years is common, affecting more than
the child development outcomes instead of clinical diag- one in four mothers. We identified key modifiable
nosis. Therefore, the child development outcomes are factors that are protective against developmental delays
based on parents’ perceptions of their child’s develop- at age 2 in the presence of poor maternal mental
ment and the possibility for misclassification must be health. Further research and evaluation of interven-
considered when interpreting the findings of this ana- tions that enhance mother’s social support, relation-
lysis. For example, children whose parents do not ship happiness, optimism, and coping with balancing
express concerns about their child’s development may family, work and life roles is warranted. Similarly, iden-
be delayed, and children whose parents identify con- tifying evidence informed strategies for supporting
cerns may not actually be experiencing clinically rele- parents to optimise children’s sleep from infancy to
vant developmental problems. However, both the ASQ age 2 and educating parents about limiting screen
and BITSEA were selected in this study because of the time from all sources in the early years offers oppor-
established reliability and validity,15–17 their practical use tunities to positively influence early child develop-
in a written questionnaire, and their widespread use in ment. Some potential strategies include engaging
clinical and research settings. We further acknowledge public health nurses during well-child clinic visits,
that these scales have a generally low positive predictive which are visits that occur mainly for the purpose of
value (PPV); despite good reliability and validity, scales immunisation and other needs including postpartum
with low PPVs warrant caution in interpretation, espe- depression screening and psychosocial assessment in
cially in terms of clinical relevance of development and the first postpartum year in Alberta. Further research
behavioural problems. is warranted to examine protective factors in the pres-
We cannot discount the possibility of reporting bias in ence of severe and chronic maternal mental health
that some of the protective factors identified might have problems (ie, trajectories) using more data waves. This
a different meaning among mothers with mental health work is currently underway.
risk (eg, optimism, relationship happiness) or reverse
Acknowledgements The authors acknowledge the contribution and support
causality bias, given that some factors examined of AOB team members and our participants. They are extremely grateful to all
occurred at the same time point as our outcomes. As for the families who took part in this study and the whole All Our Babies team.
the child outcomes, all protective factors were self- The authors are also extremely grateful to the investigators, coordinators,
reported, and a more detailed assessment of important research assistants, graduate and undergraduate students, volunteers, clerical
staff and managers.
protective factors, such as stimulation and nurturance,
was not available, which could also lead to potential mis- Contributors SCT is responsible for the overall integrity, progress,
questionnaire development and timely completion of the AOB study. SWM,
classification and residual confounding. Finally, given
HLK and SCT were involved in the conception and design of this study. SWM
the large number of protective factors examined among and HLK drafted the manuscript. HLK conducted the data analysis. All authors
the subgroup of families at maternal mental health risk, helped to conceptualise ideas, interpret findings, and review and revise drafts
there is risk for type 1 error, even with the conservative of the manuscript.
p value of 0.1 that was used in the bivariate analysis. Funding This work was supported by Alberta Innovates Health Solutions
The sample recruited in this study reflects the sociode- through Interdisciplinary Team Grant #200700595 and by providing salary
mographics of the pregnant and parenting population support for SCT. The Alberta Children’s Hospital Foundation provided
in Calgary, Canada.14 However, these sociodemo- additional funding support for the AOB study for cohort maintenance and
follow-up.
graphics, including the percentage with postsecondary
education, higher income and married/common law, Competing interests None declared.
may be higher than that observed in other populations, Ethics approval This study was approved by the Conjoint Health Research
and therefore the generalisability of our findings to Ethics Board at the University of Calgary (Ethics ID 20821 and 22821).
other populations should be interpreted with caution. Data sharing statement Requests for data from the All Our Babies Study,
Comparison of AOB participants at the time of and other studies, can be made to the Child Data Centre of Alberta, managed
McDonald SW, et al. BMJ Open 2016;6:e012096. doi:10.1136/bmjopen-2016-012096 7
Open Access
by the Alberta Centre for Child, Family and Community Research by emailing 21. Cabaj JL, McDonald SW, Tough SC. Early childhood risk and
data@research4children.com. resilience factors for behavioural and emotional problems in middle
childhood. BMC Pediatr 2014;14:166.
Open Access This is an Open Access article distributed in accordance with 22. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression.
the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, Development of the 10-item Edinburgh Postnatal Depression Scale.
which permits others to distribute, remix, adapt, build upon this work non- Br J Psychiatry 1987;150:782–6.
23. Radloff LS. The CES-D scale: a self-report depression scale for
commercially, and license their derivative works on different terms, provided
research in the general population. Appl Psychol Meas
the original work is properly cited and the use is non-commercial. See: http:// 1977;1:385–401.
creativecommons.org/licenses/by-nc/4.0/ 24. Spielberger CD, Gorsuch RL, Lushene R, et al. Manual for the
state-trait anxiety inventory. Palo Alto, CA: Consulting Psychologists
Press, 1983.
REFERENCES 25. Tough SC, Siever JE, Benzies K, et al. Maternal well-being and its
association to risk of developmental problems in children at school
1. First LR, Palfrey JS. The infant or young child with developmental
entry. BMC Pediatr 2010;10:19.
delay. N Engl J Med 1994;330:478–83.
26. Sherbourne CD, Stewart AL. The MOS social support survey. Soc
2. Tough SC, Siever JE, Leew S, et al. Maternal mental health predicts
Sci Med 1991;32:705–14.
risk of developmental problems at 3 years of age: follow up of a
27. Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from
community based trial. BMC Pregnancy Childbirth 2008;8:16.
neuroticism (and trait anxiety, self-mastery, and self-esteem): a
3. Guevara JP, Gerdes M, Localio R, et al. Effectiveness of
reevaluation of the Life Orientation Test. J Pers Soc Psychol
developmental screening in an urban setting. Pediatrics
1994;67:1063–78.
2013;131:30–7.
28. Trute B, Hiebert-Murphy D. Predicting family adjustment and
4. Hertzman C. The state of child development in Canada: are we
parenting stress in childhood disability services using brief
moving toward, or away from, equity from the start? Paediatr Child
assessment tools. J Intellect Dev Disabil 2005;30:217–25.
Health 2009;14:673–6.
29. Statistics Canada. NLSCY Cycle 5—User Guide. Section 9.5.8
5. Romano E, Babchishin L, Pagani LS, et al. School readiness and
Social Support Scale. 2002-2003. http://www23.statcan.gc.ca/
later achievement: replication and extension using a nationwide
imdb-bmdi/document/4450_D4_T9_V5-eng.pdf (accessed Feb
Canadian survey. Dev Psychol 2010;46:995–1007.
2016).
6. Gray SAO, Carter AS, Briggs-Gowan MJ, et al. Growth trajectories of
30. Lam P, Hiscock H, Wake M. Outcomes of infant sleep problems: a
early aggression, overactivity, and inattention: relations to
longitudinal study of sleep, behavior, and maternal well-being.
second-grade reading. Dev Psychol 2014;50:2255.
Pediatrics 2003;111:e203–7.
7. Briggs-Gowan MJ, Carter AS. Social-emotional screening status in
31. Dewald JF, Meijer AM, Oort FJ, et al. The influence of sleep quality,
early childhood predicts elementary school outcomes. Pediatrics
sleep duration and sleepiness on school performance in children
2008;121:957–62.
and adolescents: a meta-analytic review. Sleep Med Rev
8. Campbell SB, Shaw DS, Gilliom M. Early externalizing behavior
2010;14:179–89.
problems: toddlers and preschoolers at risk for later maladjustment.
32. Howes P, Markman HJ. Marital quality and child functioning: a
Dev Psychopathol 2000;12:467–88.
longitudinal investigation. Child Dev 1989;60:1044–51.
9. Coie JD, Dodge KA, Kupersmidt JB. Peer group behavior and social
33. Katz LF, Gottman JM. Patterns of marital conflict predict children’s
status. In: Asher SR, Coie JD, eds. Peer rejection in childhood.
internalizing and externalizing behaviors. Dev Psychol 1993;29:940.
New York, NY: Cambridge University Press, 1990:17–59.
34. Huang CY, Costeines J, Ayala C, et al. Parenting stress, social
10. Walden T, Lemerise E, Smith MC. Friendship and popularity in
support, and depression for ethnic minority adolescent mothers:
preschool classrooms. Early Educ Dev 1999;10:351–71.
impact on child development. J Child Fam Stud 2014;23:255–62.
11. Kingston D, Tough S. Prenatal and postnatal maternal mental health
35. Fabian HM, Rådestad IJ, Waldenström U. Childbirth and parenthood
and school-age child development: a systematic review. Matern
education classes in Sweden. Women’s opinion and possible
Child Health J 2014;18:1728–41.
outcomes. Acta Obstet Gynecol Scand 2005;84:436–43.
12. Kingston D, Heaman M, Fell D, et al. Factors associated with
36. Scheier MF, Carver CS. Optimism, coping, and health: assessment
perceived stress and stressful life events in pregnant women:
and implications of generalized outcome expectancies. Health
findings from the Canadian Maternity Experiences Survey. Matern
Psychol 1985;4:219–47.
Child Health J 2012;16:158–68.
37. Scheier MF, Weintraub JK, Carver CS. Coping with stress: divergent
13. Walker SP, Wachs TD, Grantham-McGregor S, et al. Inequality in
strategies of optimists and pessimists. J Pers Soc Psychol
early childhood: risk and protective factors for early child
1986;51:1257–64.
development. Lancet 2011;378:1325–38.
38. Taylor ZE, Larsen-Rife D, Conger RD, et al. Life stress, maternal
14. McDonald SW, Lyon AW, Benzies KM, et al. The all our babies
optimism, and adolescent competence in single mother, African
pregnancy cohort: design, methods, and participant characteristics.
American families. J Fam Psychol 2010;24:468–77.
BMC Pregnancy Childbirth 2013;13(Suppl 1):S2.
39. Seligman M. Positive psychology, positive prevention, and positive
15. Limbos MM, Joyce DP. Comparison of the ASQ and PEDS in
therapy. In: Snyder CR, Lopez SJ, eds. Handbook of positive
screening for developmental delay in children presenting for primary
psychology. New York, NY: Oxford University Press, 2002:3–9.
care. J Dev Behav Pediatr 2011;32:499–511.
40. Amstad FT, Meier LL, Fasel U, et al. A meta-analysis of work—
16. Briggs-Gowan MJ, Carter AS, Irwin JR. The brief infant-toddler
family conflict and various outcomes with a special emphasis on
social and emotional assessment: screening for social-emotional
cross-domain versus matching-domain relations. J Occup Health
problems and delays in competence. J Pediatr Psychol
Psychol 2011;16:151.
2004;29:143–55.
41. Crnic KA, Gaze C, Hoffman C. Cumulative parenting stress across
17. Briggs-Gowan MJ, Carter AS. Brief Infant-Toddler Social and
the preschool period: relations to maternal parenting and child
Emotional Assessment (BITSEA) manual, version 2.0. New Haven,
behaviour at age 5. Infant Child Dev 2005;14:117–32.
CT: Yale University, 2002.
42. Christakis DA, Zimmerman FJ, DiGiuseppe DL, et al. Early
18. Squires J, Bricker D, Potter L. Revision of a parent-completed
television exposure and subsequent attentional problems in children.
development screening tool: ages and stages questionnaires.
Pediatrics 2004;113:708–13.
J Pediatr Psychol 1997;22:313–28.
43. Mistry KB, Minkovitz CS, Strobino DM, et al. Children’s television
19. Oberklaid F, Efron D. Developmental delay—identification and
exposure and behavioral and social outcomes at 5.5 years: does
management. Aust Fam Physician 2005;34:739.
timing of exposure matter? Pediatrics 2007;120:762–9.
20. Rydz D, Srour M, Oskoui M, et al. Screening for developmental
44. Cheng S, Maeda T, Yoichi S, et al. Early television exposure and
delay in the setting of a community pediatric clinic: a prospective
children’s behavioral and social outcomes at age 30 months.
assessment of parent-report questionnaires. Pediatrics 2006;118:
J Epidemiol 2010;20(Suppl 2):S482–9.
e1178–86.
8 McDonald SW, et al. BMJ Open 2016;6:e012096. doi:10.1136/bmjopen-2016-012096
Vous aimerez peut-être aussi
- Maternal Adverse Childhood Experiences and Infant DevelopmentDocument11 pagesMaternal Adverse Childhood Experiences and Infant DevelopmentMarcela Dalla PortaPas encore d'évaluation
- (2011) Early Childhood Stimulation Bene Ts Adult Competence and Reduces Violent BehaviorDocument11 pages(2011) Early Childhood Stimulation Bene Ts Adult Competence and Reduces Violent BehaviorEduardo PichardoPas encore d'évaluation
- Lancet 2011 - Papers 1 and 2 PDFDocument31 pagesLancet 2011 - Papers 1 and 2 PDFpyeohhpyePas encore d'évaluation
- 5938 20021 3 PBDocument9 pages5938 20021 3 PBbiswaspritha.18Pas encore d'évaluation
- Mental Health Problems in A School Setting in Children and AdolescentsDocument9 pagesMental Health Problems in A School Setting in Children and AdolescentsRezky PutriPas encore d'évaluation
- Alarcao Shephard 2021 Dev SciDocument12 pagesAlarcao Shephard 2021 Dev ScielisehaasPas encore d'évaluation
- Pola Pengasuhan Pada Anak Dengan Hambatan PerkembanganDocument14 pagesPola Pengasuhan Pada Anak Dengan Hambatan PerkembanganMawar AnggelaPas encore d'évaluation
- Articles: BackgroundDocument12 pagesArticles: BackgroundEduardo PichardoPas encore d'évaluation
- Nutritional Neuroscience and Education1Document11 pagesNutritional Neuroscience and Education1Ingrid DíazPas encore d'évaluation
- Enlow 2012 - Interpersonal Trauma Exposure and Cognitive DevelopmentDocument7 pagesEnlow 2012 - Interpersonal Trauma Exposure and Cognitive DevelopmentRoxana AgafiteiPas encore d'évaluation
- Supporting Families To Protect Child Health: Parenting Quality and Household Needs During The COVID-19 PandemicDocument19 pagesSupporting Families To Protect Child Health: Parenting Quality and Household Needs During The COVID-19 PandemicpangaribuansantaPas encore d'évaluation
- Supporting Families To Protect Child Health: Parenting Quality and Household Needs During The COVID-19 PandemicDocument19 pagesSupporting Families To Protect Child Health: Parenting Quality and Household Needs During The COVID-19 PandemicpangaribuansantaPas encore d'évaluation
- Rifda Azkiatus Salamah - 4411418014Document26 pagesRifda Azkiatus Salamah - 4411418014Rifda AzkiaPas encore d'évaluation
- Annotated Bibliography: Integration To The Social SciencesDocument4 pagesAnnotated Bibliography: Integration To The Social SciencesEmile DufourPas encore d'évaluation
- Ajol File Journals 205 Articles 227090 Submission Proof 227090 2437Document21 pagesAjol File Journals 205 Articles 227090 Submission Proof 227090 2437MusePas encore d'évaluation
- Infant Media Exposure and Toddler DevelopmentDocument7 pagesInfant Media Exposure and Toddler DevelopmentLinPas encore d'évaluation
- Ask The Question Screening For PostpartuDocument13 pagesAsk The Question Screening For PostpartuNovia QomariahPas encore d'évaluation
- Comparison of Skin-to-Skin (Kangaroo) and Traditional Care: Parenting Outcomes and Preterm Infant DevelopmentDocument13 pagesComparison of Skin-to-Skin (Kangaroo) and Traditional Care: Parenting Outcomes and Preterm Infant DevelopmentLambano ZoePas encore d'évaluation
- JMSCR Vol - 04 - Issue - 12 - Page 14641-14649 - December: Study of Behavioral Problems in Preschool ChildrenDocument9 pagesJMSCR Vol - 04 - Issue - 12 - Page 14641-14649 - December: Study of Behavioral Problems in Preschool ChildrenRavindraPas encore d'évaluation
- Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic ReviewDocument16 pagesMental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic ReviewHeartgwea BuladacoPas encore d'évaluation
- Tha Significance of Early Childhood Adversity ArticleDocument2 pagesTha Significance of Early Childhood Adversity ArticleAriPas encore d'évaluation
- Article 37 Forcada 2006Document10 pagesArticle 37 Forcada 2006Naoual EL ANNASPas encore d'évaluation
- COVID19 Unmasked Survey Executive SummaryDocument2 pagesCOVID19 Unmasked Survey Executive SummaryGEORGIOSMANIAKISPas encore d'évaluation
- Jamapediatrics Cheong 2017 Oi 160101Document7 pagesJamapediatrics Cheong 2017 Oi 160101YsagrimsPas encore d'évaluation
- Effect Nbo-Rct 2020Document14 pagesEffect Nbo-Rct 2020A Dwi Bahagia FebrianiPas encore d'évaluation
- Familiesof Childrenwith Chronic Illnessandthe Relational Family ModelDocument10 pagesFamiliesof Childrenwith Chronic Illnessandthe Relational Family ModelantoPas encore d'évaluation
- Supporting Families Exposed To Adverse Childhood Experiences Within Child Care Settings: A Feasibility PilotDocument12 pagesSupporting Families Exposed To Adverse Childhood Experiences Within Child Care Settings: A Feasibility PilotKaren CárcamoPas encore d'évaluation
- Sobrecarga CuidadoresDocument6 pagesSobrecarga CuidadoresMARIA FRANCISCA VERGARA AGUILARPas encore d'évaluation
- European Journal of Pediatrics SciDocument7 pagesEuropean Journal of Pediatrics ScianimeshPas encore d'évaluation
- Severity of Depression in Mothers of Children Suffering From Cerebral PalsyDocument3 pagesSeverity of Depression in Mothers of Children Suffering From Cerebral PalsyDr Alamzeb JadoonPas encore d'évaluation
- Mothers of Undernourished Jamaican Children Have Poorer Psychosocial FunctioningDocument9 pagesMothers of Undernourished Jamaican Children Have Poorer Psychosocial FunctioningJonique TyrellPas encore d'évaluation
- Nur 330 Health Promotion Final Paper Apa Mental Health in Middle and High School StudentsDocument9 pagesNur 330 Health Promotion Final Paper Apa Mental Health in Middle and High School Studentsapi-490428193Pas encore d'évaluation
- Literature Review On Parental Mental HealthDocument7 pagesLiterature Review On Parental Mental Healthc5p6e5z1100% (1)
- Protecting The Psychological Health of Children Through Effective Communication About COVID-19 PDFDocument2 pagesProtecting The Psychological Health of Children Through Effective Communication About COVID-19 PDFJorge MartínezPas encore d'évaluation
- Neuro 1Document11 pagesNeuro 1cristiana nogueiraPas encore d'évaluation
- Paediatrica IndonesianaDocument8 pagesPaediatrica IndonesianaAnna ClarkPas encore d'évaluation
- Fear of LonelinessDocument25 pagesFear of LonelinessHà Anh Lê VũPas encore d'évaluation
- School ReadinesDocument17 pagesSchool ReadinesnanaPas encore d'évaluation
- Paediatrica Indonesiana: Endy P. Prawirohartono, Detty S. Nurdiati, Mohammad HakimiDocument9 pagesPaediatrica Indonesiana: Endy P. Prawirohartono, Detty S. Nurdiati, Mohammad HakimiMonajusticaPas encore d'évaluation
- Cheng Etal2007Document9 pagesCheng Etal2007eebook123456Pas encore d'évaluation
- MHF Scotland Impacts of LockdownDocument20 pagesMHF Scotland Impacts of LockdownFrancine Mae Tubianosa TebelinPas encore d'évaluation
- Attentiondeficit-Hyperactivity-Disorder-Adhd-In-Children-A-Movetowards-Developmental-Perspectives-2469-9837-1000171 (1) - DikonversiDocument8 pagesAttentiondeficit-Hyperactivity-Disorder-Adhd-In-Children-A-Movetowards-Developmental-Perspectives-2469-9837-1000171 (1) - Dikonversi6558Pas encore d'évaluation
- Lancet Child Dev Series Paper2Document13 pagesLancet Child Dev Series Paper2Nandia NatsagPas encore d'évaluation
- Mental Health of Parents and Preschool-Aged Children During The COVID-19 Pandemic The Mediating Role of Harsh Parenting and Child Sleep DisturbancesDocument9 pagesMental Health of Parents and Preschool-Aged Children During The COVID-19 Pandemic The Mediating Role of Harsh Parenting and Child Sleep DisturbancesToth Fanni-BarbaraPas encore d'évaluation
- Ijst 2016 V9i36 102702Document6 pagesIjst 2016 V9i36 102702Manoela IaconelliPas encore d'évaluation
- Addressing Early Childhood Emotional and Behavioral ProblemsDocument13 pagesAddressing Early Childhood Emotional and Behavioral ProblemsAriPas encore d'évaluation
- Developmental Correlates Persistent Snoring in Preschool Children: Predictors and Behavioral andDocument10 pagesDevelopmental Correlates Persistent Snoring in Preschool Children: Predictors and Behavioral andsambalikadzilla6052Pas encore d'évaluation
- The Bucharest Early Intervention Project - Adolescent Mental Health and Adaptation Following Early DeprivationDocument8 pagesThe Bucharest Early Intervention Project - Adolescent Mental Health and Adaptation Following Early DeprivationMerly JHPas encore d'évaluation
- The Effects of A Stress Management Intervention in Elementary School ChildrenDocument6 pagesThe Effects of A Stress Management Intervention in Elementary School ChildrenGabriela AlinaPas encore d'évaluation
- Cohort StudyDocument11 pagesCohort StudyririsPas encore d'évaluation
- Sleepless in America Inadequate Sleep and RelationDocument12 pagesSleepless in America Inadequate Sleep and RelationmagdalenaPas encore d'évaluation
- Physical and Psychosocial Impacts of Pregnancy On Adolescents and Their Coping Strategies A Descriptive Study in Kuala Lumpur Malaysia PDFDocument9 pagesPhysical and Psychosocial Impacts of Pregnancy On Adolescents and Their Coping Strategies A Descriptive Study in Kuala Lumpur Malaysia PDFJason Jimmy Lee PillayPas encore d'évaluation
- Examining Mental Health Disorders in Overweight and Obese Pediatric PatientsDocument13 pagesExamining Mental Health Disorders in Overweight and Obese Pediatric PatientsAnder MathiasPas encore d'évaluation
- Child Family Social Work - 2022 - Rahmani - Caregiver or Care Receiver Adolescents Experience of Caregiving To A ParentDocument10 pagesChild Family Social Work - 2022 - Rahmani - Caregiver or Care Receiver Adolescents Experience of Caregiving To A ParentLuz Maria RojasPas encore d'évaluation
- 11 - Nutrition and Intelligence - Berkman Lancet 2002Document9 pages11 - Nutrition and Intelligence - Berkman Lancet 2002luishelPas encore d'évaluation
- Consejería Adolescente Rev Med de Chile PDFDocument7 pagesConsejería Adolescente Rev Med de Chile PDFJéssica MorenoPas encore d'évaluation
- Well-Child Care in Infancy: Promoting Readiness for LifeD'EverandWell-Child Care in Infancy: Promoting Readiness for LifePas encore d'évaluation
- High Five Discipline: Positive Parenting for Happy, Healthy, Well-Behaved KidsD'EverandHigh Five Discipline: Positive Parenting for Happy, Healthy, Well-Behaved KidsPas encore d'évaluation
- Parental Monitoring of Adolescents: Current Perspectives for Researchers and PractitionersD'EverandParental Monitoring of Adolescents: Current Perspectives for Researchers and PractitionersPas encore d'évaluation
- Foot Massage To Treat Pain in Patients Post Laparatomy SurgeryDocument5 pagesFoot Massage To Treat Pain in Patients Post Laparatomy SurgeryAndikPas encore d'évaluation
- Serrogate Mother - Id.enDocument7 pagesSerrogate Mother - Id.enAndikPas encore d'évaluation
- Hiperlipidemia Dengan Gangguan Jantung Dan: Pengaruh Derajat Hipertensi, Lama Hipertensi DanDocument14 pagesHiperlipidemia Dengan Gangguan Jantung Dan: Pengaruh Derajat Hipertensi, Lama Hipertensi DanAndikPas encore d'évaluation
- Cerdik 2 PDFDocument101 pagesCerdik 2 PDFAndikPas encore d'évaluation
- Publication Info: Pediatrics Week Atlanta (Atlanta) 08 Oct 2016: 688Document3 pagesPublication Info: Pediatrics Week Atlanta (Atlanta) 08 Oct 2016: 688AndikPas encore d'évaluation
- Translate AnakDocument12 pagesTranslate AnakAndikPas encore d'évaluation
- Abstract (English) : Publication Info: Pediatrics Week Atlanta (Atlanta) 29 Apr 2017: 305Document3 pagesAbstract (English) : Publication Info: Pediatrics Week Atlanta (Atlanta) 29 Apr 2017: 305AndikPas encore d'évaluation
- Referat Hirschsprung DiseaseDocument15 pagesReferat Hirschsprung DiseaseAndikPas encore d'évaluation
- Reti No Blast OmaDocument12 pagesReti No Blast OmaAndikPas encore d'évaluation
- Unit 2 - Mental Health and IllnessDocument12 pagesUnit 2 - Mental Health and IllnessJill MehtaPas encore d'évaluation
- Author: Licensed Psychologist Published: April 1, 2001: Dr. Christopher L. HeffnerDocument58 pagesAuthor: Licensed Psychologist Published: April 1, 2001: Dr. Christopher L. HeffnerAnonymous OCDJg17ZPas encore d'évaluation
- P Mental Health NursingDocument3 pagesP Mental Health Nursingsellyna SaidinPas encore d'évaluation
- Suicide: International Statistics (United States)Document5 pagesSuicide: International Statistics (United States)Sofia Marie ValdezPas encore d'évaluation
- U3A5 Practitioner's Handbook Organizing ChartDocument3 pagesU3A5 Practitioner's Handbook Organizing Chartkael9010 kael9010Pas encore d'évaluation
- Book Review of Peter Bartlett, Oliver Lewis and Oliver Thorold, Mental Disability and The European Convention On Human RightsDocument6 pagesBook Review of Peter Bartlett, Oliver Lewis and Oliver Thorold, Mental Disability and The European Convention On Human RightsJohn RussellPas encore d'évaluation
- Pseudologia FantasticaDocument9 pagesPseudologia FantasticaGita PuspitasariPas encore d'évaluation
- Forensic Psychiatry 2Document33 pagesForensic Psychiatry 2joglekar.vp6207100% (6)
- Music Therapy and Mental Health - Research PaperDocument14 pagesMusic Therapy and Mental Health - Research Paperapi-550020034100% (1)
- Missing The Diagnosis - The Hidden Medical Causes of Mental Disorders by William Matteson, PHDocument134 pagesMissing The Diagnosis - The Hidden Medical Causes of Mental Disorders by William Matteson, PHjonascarvPas encore d'évaluation
- Abnormal Psychology: Session 3: Diagnosis of Mental DisordersDocument38 pagesAbnormal Psychology: Session 3: Diagnosis of Mental DisordersHumanist English ManPas encore d'évaluation
- Chinese Medicine Gu ParasitesDocument8 pagesChinese Medicine Gu Parasitesnepretip100% (2)
- 9.2 Panic Disorder: Etiology Biological FactorsDocument7 pages9.2 Panic Disorder: Etiology Biological FactorsFayePas encore d'évaluation
- Delusional Disorder CompilationDocument11 pagesDelusional Disorder CompilationGrace IgnacoPas encore d'évaluation
- Assignment 3 StartupDocument31 pagesAssignment 3 StartupKunal Ranjan100% (1)
- Counseling Psychology vs. Clinical PsychologyDocument3 pagesCounseling Psychology vs. Clinical PsychologyDivyaDeepthi18Pas encore d'évaluation
- Text: Hurry Sickness: A According To Statistics, It Is Becoming Increasingly Rare in Many WesternDocument5 pagesText: Hurry Sickness: A According To Statistics, It Is Becoming Increasingly Rare in Many WesternTrần Thị Vân HàPas encore d'évaluation
- The Psychodynamic Diagnostic Manual - 2nd Edition (PDM-2) : June 2015Document5 pagesThe Psychodynamic Diagnostic Manual - 2nd Edition (PDM-2) : June 2015Stroe EmmaPas encore d'évaluation
- Importance of Sleep EssayDocument6 pagesImportance of Sleep EssayJohn AnandPas encore d'évaluation
- PPII - 5 (Ch. 18, Biopsychology)Document18 pagesPPII - 5 (Ch. 18, Biopsychology)Sabina RodríguezPas encore d'évaluation
- Nock Kurtz 2005 PDFDocument12 pagesNock Kurtz 2005 PDFWendel NuguidPas encore d'évaluation
- Obsessions: Signs and Symptoms of OCDDocument14 pagesObsessions: Signs and Symptoms of OCDvikas takPas encore d'évaluation
- The Neurobiology of Anorexia Nervosa A SDocument26 pagesThe Neurobiology of Anorexia Nervosa A SSol PennisiPas encore d'évaluation
- Chapters 1 3Document44 pagesChapters 1 3Azriel Mae BaylonPas encore d'évaluation
- Psychiatric Nursing BulletsDocument7 pagesPsychiatric Nursing BulletsLouie John AbilaPas encore d'évaluation
- Mental Health Care EssayDocument5 pagesMental Health Care EssayKedPas encore d'évaluation
- The Beck Depression Inventory: The Pharma Innovation - JournalDocument7 pagesThe Beck Depression Inventory: The Pharma Innovation - JournaldevPas encore d'évaluation
- 5 Paragraph Essay Writing Prompts For Kids PDFDocument2 pages5 Paragraph Essay Writing Prompts For Kids PDFVitoPas encore d'évaluation
- Coexistence of Folie Communique e and Folie SimultaneeDocument4 pagesCoexistence of Folie Communique e and Folie SimultaneeAna Rosa González Barroso0% (1)
- ADHD Focused Adult Couple TherapyDocument269 pagesADHD Focused Adult Couple TherapyezabielskaPas encore d'évaluation