Académique Documents
Professionnel Documents
Culture Documents
Transverse Myelitis: Clinical Practice
Transféré par
arnabTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Transverse Myelitis: Clinical Practice
Transféré par
arnabDroits d'auteur :
Formats disponibles
The n e w e ng l a n d j o u r na l of m e dic i n e
clinical practice
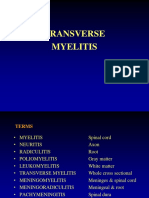
Transverse Myelitis
Elliot M. Frohman, M.D., Ph.D., and Dean M. Wingerchuk, M.D.
This Journal feature begins with a case vignette highlighting a common clinical problem.
Evidence supporting various strategies is then presented, followed by a review of formal guidelines,
when they exist. The article ends with the author’s clinical recommendations.
An otherwise healthy 28-year-old woman presents to the emergency department
with progressive weakness that began 3 days earlier. She reports difficulty walking,
numbness in the body below her breasts, and urinary urgency, and she notes that
neck flexion triggers an electrical sensation that radiates to the coccyx. Physical ex-
amination reveals moderate paraparesis with hyperreflexia, a left extensor plantar
response, impairment of vibratory and proprioceptive sensation, and a sensory level
at T6. Magnetic resonance imaging (MRI) reveals a lower cervical cord lesion that
enhances after gadolinium administration, a finding that is consistent with trans-
verse myelitis. How should she be further evaluated and treated?
The Cl inic a l Probl em
From the Departments of Neurology and The term “transverse myelitis” describes a heterogeneous group of inflammatory
Ophthalmology, University of Texas South disorders that are characterized by acute or subacute motor, sensory, and auto-
western Medical Center at Dallas, Dallas
(E.M.F.); and the Department of Neurol nomic (bladder, bowel, and sexual) spinal cord dysfunction (Table 1).1 The clinical
ogy, Mayo Clinic, Scottsdale, AZ (D.M.W.). signs are caused by an interruption in ascending and descending neuroanatomical
Address reprint requests to Dr. Frohman pathways in the transverse plane of the spinal cord, and a resulting sensory level is
at the Department of Neurology, Uni
versity of Texas Southwestern Medical characteristic of the syndrome. The transverse myelitis syndrome may arise from
Center at Dallas, 5323 Harry Hines Blvd., various causes, but it most often occurs as an autoimmune phenomenon after an
Dallas, TX 75235, or at elliot.frohman@ infection or vaccination (accounting for 60% of the cases in children) or as a result
utsouthwestern.edu.
of a direct infection, an underlying systemic autoimmune disease, or an acquired
N Engl J Med 2010;363:564-72. demyelinating disease such as multiple sclerosis or the spectrum of disorders re-
Copyright © 2010 Massachusetts Medical Society. lated to neuromyelitis optica (Devic’s disease, a demyelinating disease that is de-
fined by transverse myelitis and optic neuritis).2-7 However, after detailed evalua-
tion, 15 to 30% of the cases of transverse myelitis are ultimately categorized as
idiopathic.5,8
Estimates of the annual incidence of idiopathic or postinfectious transverse
myelitis range from 1.3 to 8 cases per million. Although the disorder can develop
An audio version
at any age, there is a bimodal peak in the incidence at 10 to 19 years of age and
of this article
is available at at 30 to 39 years.9,10 The incidence increases to 24.6 cases per million annually if
NEJM.org acquired demyelinating causes, especially multiple sclerosis, are included.11 There
is no clear pattern among cases of idiopathic transverse myelitis with respect to
sex, geographic distribution, or familial susceptibility.
The pathological hallmark of transverse myelitis is the presence of focal collec-
tions of lymphocytes and monocytes, with varying degrees of demyelination, axonal
injury, and astroglial and microglial activation, within the spinal cord.2 Neuro-
myelitis optica lesions contain deposits of immunoglobulin and complement
around small blood vessels, and necrosis can be observed in severe cases.7 The
observation that systemic infection or immunization precedes many cases of trans-
564 n engl j med 363;6 nejm.org august 5, 2010
The New England Journal of Medicine
Downloaded from nejm.org by DAYA KRISHNA JHA on December 3, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
clinical pr actice
verse myelitis suggests that mechanisms such
Table 1. Diagnostic Criteria for Transverse Myelitis.*
as molecular mimicry and the development of
autoantibodies may play roles in the pathogen- Bilateral (not necessarily symmetric) sensorimotor and autonomic spinal
esis of the syndrome.2,4 cord dysfunction
The prognosis after an attack of transverse Clearly defined sensory level
myelitis is highly variable among both adults and Progression to nadir of clinical deficits between 4 hours and 21 days after
children.8,11,12 Patients who have an attack of symptom onset
transverse myelitis associated with multiple scle- Demonstration of spinal cord inflammation: cerebrospinal fluid pleocytosis or
elevated IgG index,† or MRI revealing a gadolinium-enhancing cord lesion
rosis may have a substantial or even complete
recovery, but patients with transverse myelitis or Exclusion of compressive, postradiation, neoplastic, and vascular causes
neuromyelitis optica associated with other dis-
* Clinical events that are consistent with transverse myelitis but that are not as
eases usually have clinically significant residual sociated with cerebrospinal fluid abnormalities or abnormalities detected on
neurologic deficits. Most of the recovery occurs MRI and that have no identifiable underlying cause are categorized as possi
over the course of the first 3 months after the ble idiopathic transverse myelitis.
† The IgG index is a measure of intrathecal synthesis of immunoglobulin and is
event, although improvement may continue for a calculated with the use of the following formula: (CSF IgG ÷ serum IgG) ÷ (CSF
year or longer. In one study of idiopathic myelitis, albumin ÷ serum albumin), where CSF denotes cerebrospinal fluid.
more than one third of the patients had a rapidly
progressive course with a poor outcome (death
or inability to ambulate). The combination of radiate down the spine or limbs with neck flex-
severe weakness, hypotonia, and areflexia — ion) and paroxysmal tonic spasms (involuntary
“spinal shock” — was the only recognized pre- dystonic contractions of limb or trunk muscles).
dictor of a poor outcome.8 Urinary incontinence or retention, bowel inconti-
nence or constipation, and sexual dysfunction are
S t r ategie s a nd E v idence common but vary in severity among patients.
Once the clinical syndrome of myelopathy is
Diagnosis recognized, a knowledge of basic spinal cord
A history of motor weakness, sensory abnormal- anatomy and vascular supply helps to guide the
ities referable to the spinal cord, and bladder or differential diagnosis, which includes compres-
bowel dysfunction point to the diagnosis of my- sive, vascular, metabolic, neoplastic, and other
elopathy. Symptoms and signs of transverse my- causes (see Fig. 1 in the Supplementary Appen-
elitis typically evolve over the course of hours to dix, available with the full text of this article at
days and are usually bilateral; however, unilateral NEJM.org). Figure 1 provides a systematic ap-
or markedly asymmetric presentations can occur.1 proach to the evaluation of myelopathy.1-3 As a
Transverse myelitis is sometimes manifested as first step, MRI is warranted to rule out the pres-
rapid-onset, severe paraparesis or quadriparesis ence of structural lesions, especially those ame-
with areflexia, which may lead to diagnostic con- nable to urgent neurosurgical intervention. The
fusion with other causes of ascending weakness, entire spinal cord should be imaged so that false
such as the Guillain–Barré syndrome; otherwise, negative results that may be caused by mislead-
hyperreflexia and Babinski signs are present, con- ing localizing signs, such as a thoracic sensory
firming a central rather than a peripheral cause level caused by a cervical lesion, can be avoided.
of the muscle weakness. A well-defined truncal The finding of an intrinsic cord lesion (some-
sensory level, below which the sensation of pain times more than one) is characteristic of myelitis;
and temperature is altered or lost, distinguishes in the acute phase, such lesions usually enhance
myelopathy from cerebral lesions and peripheral with intravenous gadolinium administration. An
neuropathies. Neuropathic pain may occur in the assessment of the spinal cord syndrome at pre-
midline (an aching, deep pain) or in a dermato- sentation, together with an evaluation of the
mal distribution (radicular or lancinating pain or number, size, and shape of lesions detected on
a sensation of burning or itching), with the latter MRI, provides the basis for determining whether
pattern providing a clue to the anatomical level the lesion is consistent with myelitis. Lesions as-
of the lesion. Demyelination is responsible for the sociated with idiopathic transverse myelitis usu-
presence of Lhermitte’s sign (paresthesias that ally span at least two vertebral segments, as vi-
n engl j med 363;6 nejm.org august 5, 2010 565
The New England Journal of Medicine
Downloaded from nejm.org by DAYA KRISHNA JHA on December 3, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Clinical presentation: Acute myelopathy
MRI of entire spine with gadolinium
Compressive lesion?
No Yes
Confirm myelitis Neurosurgical consultation
Intramedullary cord lesion?
No Yes
Reconsider myelopathy diagnosis Gadolinium-enhanced lesion on MRI?
Consider acute presentation of Pleocytosis on CSF examination?
metabolic or degenerative Increased IgG index on CSF exami-
myelopathy nation?
Consider repeat MRI in 2–7 days
No Yes
Consider noninflammatory
Determine cause of myelitis
myelopathies
Consider repeat MRI
in 2–7 days
Test for infection
Test for systemic inflam-
matory or autoimmune
disease
Test for cancer
Negative Positive
Further evaluate pattern Specific diagnosis
of myelitis and therapy
Partial TM Longitudinally extensive TM
Demyelination on brain MRI MRI of brain: neuromyelitis optica
Oligoclonal bands or increased spectrum disorder pattern, normal,
IgG index in CSF or not meeting MS criteria
Visual evoked potentials abnormal Positive for NMO-IgG (aquaporin-4
antibodies)
Yes All negative No Yes
High risk for MS Low risk for MS Reconsider history Neuromyelitis optica
spectrum disorder
Antecedent infection Antecedent vaccination
No Yes No Yes
Idiopathic TM Postinfectious TM Idiopathic TM Postvaccination TM
566 n engl j med 363;6 nejm.org august 5, 2010
The New England Journal of Medicine
Downloaded from nejm.org by DAYA KRISHNA JHA on December 3, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
clinical pr actice
of multifocal cerebral involvement.4 Multiple scle-
Figure 1 (facing page). Diagnostic Algorithm for the
Evaluation of Acute Myelopathies and Myelitis. rosis is associated with short lesions (spanning
A systematic approach to the evaluation of acute mye fewer than two vertebral segments) that are lo-
lopathy syndromes allows for early identification of cases cated in the periphery of the cord, affecting
requiring emergency neurosurgical treatment and pro mainly white matter (“partial” transverse myeli-
vides the highest probability of establishing the specific tis) (Fig. 2), and there is usually concomitant
diagnosis of transverse myelitis, as well as determining
MRI evidence of demyelinating brain lesions.17
the cause of the syndrome. CSF denotes cerebrospinal
fluid, MRI magnetic resonance imaging, MS multiple Neuromyelitis optica is strongly associated with
sclerosis, NMO neuromyelitis optica, and TM trans longitudinally extensive transverse myelitis, de-
verse myelitis. fined by a lesion that spans three or more verte-
bral segments on MRI.6,7 Such lesions tend to be
sualized on MRI of the spinal cord (Fig. 2). symmetric and situated centrally within the cord
Normal MRI results should prompt a reconsid- (involving both gray and white matter) and may
eration of the diagnosis of myelopathy in favor extend into the brain stem, causing nausea, vom-
of other disorders of the central or peripheral iting, and hiccups (Fig. 2).18,19 Neuromyelitis
nervous system.2,3 optica is specifically associated with the serum
The transverse myelitis syndrome has an ex- autoantibody marker NMO-IgG, which targets
tensive differential diagnosis. The medical his- the astrocytic water channel, aquaporin-4.20,21
tory, medical review of systems, social and travel Identifying the cause of transverse myelitis
history, and general physical examination can facilitates the prediction of the future clinical
provide clues that point toward possible infec- course and informs the decision about whether
tious or paraneoplastic causes, as well as causes to provide prophylaxis against future neurologic
associated with systemic inflammatory or auto- events. The postinfectious, postvaccination, and
immune diseases such as systemic lupus ery- idiopathic forms of transverse myelitis are usu-
thematosus, Sjögren’s syndrome, and sarcoido- ally monophasic syndromes, whereas multiple
sis.1-3,13,14 Implication of a connective-tissue sclerosis and neuromyelitis optica–spectrum dis-
disease (e.g., systemic lupus erythematosus) as orders are relapsing diseases that are associated
the cause of transverse myelitis requires evidence with a high risk of future attacks of transverse
of systemic disease, and the diagnosis should myelitis and other neurologic events. The presence
not be based solely on the presence of serum on MRI of brain lesions that are characteristic of
autoantibodies (e.g., antinuclear antibody or ex- demyelination indicates a high risk of multiple
tractable nuclear antigen), because such antibod- sclerosis after a partial myelitis event (Fig. 2 in
ies may be present in patients with underlying the Supplementary Appendix). Seropositivity for
multiple sclerosis or neuromyelitis optica.15 Clini- NMO-IgG (and to a lesser extent, ssA autoanti-
cal features, laboratory tests, and diagnostic im- body) in a patient with longitudinally extensive
aging options that are helpful in making the transverse myelitis is highly predictive of relaps-
diagnosis are summarized in Table 2, as well as ing disease and, in the case of NMO-IgG, con-
in Table 1 in the Supplementary Appendix. The version to definite neuromyelitis optica, which
occurrence of transverse myelitis after infection can also be associated with abnormalities on
or vaccination does not preclude the need for MRI of the brain (Fig. 2 in the Supplementary
further evaluation, since infection or immuniza- Appendix).22,23 Factors suggesting that a person
tions may also trigger attacks of myelitis in the who has had a myelitis event is at high risk for
context of an underlying disease (especially mul- clinically definite multiple sclerosis or neuromy-
tiple sclerosis or neuromyelitis optica). elitis optica are summarized in Table 1 in the
Transverse myelitis is a common manifesta- Supplementary Appendix.
tion or presenting feature of acquired demyeli-
nating diseases of the central nervous system.16 Management
Among children, it is a frequent characteristic of Initial Immunotherapy
acute disseminated encephalomyelitis, which typ- The goals of therapy during the acute phase of
ically occurs after an infection or immunization myelitis (Table 2 in the Supplementary Appendix)
and is associated with clinical and MRI evidence are to halt the progression and initiate the reso-
n engl j med 363;6 nejm.org august 5, 2010 567
The New England Journal of Medicine
Downloaded from nejm.org by DAYA KRISHNA JHA on December 3, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
A B C
D E F
Figure 2. Features of Common Myelitis Syndromes on Neuroimaging.
The findings on MRI are a key component of the diagnostic evaluation of transverse myelitis. Acute myelitis events
are associated with a focal lesion within the spinal cord. Panel A shows an example of a lesion associated with idio
pathic myelitis (sagittal plane, T2 weighted sequence). Shortsegment lesions, as shown in Panel B (sagittal plane,
T2 weighted sequence), and those that are asymmetric, as shown in Panel C (axial plane, T2 weighted sequence), are
characteristic of multiple sclerosis. Lesion enhancement after the administration of gadolinium, as shown in Panel D
(sagittal plane, T1weighted sequence), suggests acute inflammation of the spinal cord. In contrast, a longitudinally
extensive lesion (i.e., one that spans several vertebral segments), as shown in Panel E (sagittal plane, T2 weighted
sequence), especially if it extends rostrally into the brain stem and is located centrally within the cord, as in Panel F
(axial plane, T2 weighted sequence), is typical of neuromyelitis optica.
lution of the inflammatory spinal cord lesion, or route of administration is lacking. Oral regi-
thereby speeding clinical recovery. Corticosteroids mens may be used in the case of patients with
are the standard first-line treatment; however, relatively mild episodes of myelitis who do not
because there have been no randomized, con- require hospitalization (e.g., in cases associated
trolled trials of corticosteroid therapy of patients with established multiple sclerosis).25,26 Potential
with transverse myelitis, supporting evidence for adverse effects of pulsed corticosteroid therapy
the use of corticosteroids as first-line therapy is include gastrointestinal symptoms, insomnia,
derived from case studies or extrapolation from headache, anxiety, mania, hypertension, hyper-
trials involving patients with multiple sclero- glycemia, and electrolyte disturbances.
sis.1-5,7,17,24,25 Approximately 50 to 70% of pa- Rescue therapy with plasma exchange may
tients have partial or complete recovery and are benefit patients who do not have a response to
ambulatory with or without aid.8,24 High-dose corticosteroids.27-29 In a randomized, crossover
intravenous regimens are typically used (e.g., trial involving 22 patients with idiopathic in-
1000 mg of methylprednisolone daily, generally flammatory demyelinating syndromes (7 of which
for 3 to 5 days),25 although evidence of the supe- were cases of myelitis) that did not respond to
riority of a particular corticosteroid drug, dose, corticosteroids, 42% of the patients had moder-
568 n engl j med 363;6 nejm.org august 5, 2010
The New England Journal of Medicine
Downloaded from nejm.org by DAYA KRISHNA JHA on December 3, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
clinical pr actice
Table 2. Concise Differential Diagnosis and Diagnostic Testing for Transverse Myelitis.*
Possible Cause Diagnostic Tests
Infection Blood serologic studies; CSF culture, serologic studies, and PCR; chest radiography
and other imaging as indicated
Systemic autoimmune or inflammatory disease Clinical examination; serologic studies; chest and joint radiography; other tests or
imaging as indicated by history and examination
Paraneoplastic cause Chest radiography, computed tomography, or positron-emission tomography;
comprehensive serum and CSF paraneoplastic antibody panel
Acquired CNS demyelinating disease (multiple Brain MRI with gadolinium enhancement; CSF examination for cell count and differ
sclerosis, neuromyelitis optica) ential count, oligoclonal bands, and IgG index; tests of visual evoked potentials;
serum NMO-IgG testing
Postinfectious or postvaccination cause History taking that reveals clear, recent history of infection or vaccination; serologic
confirmation of recent infection; exclusion of other causes
* CNS denotes central nervous system, CSF cerebrospinal fluid, NMO neuromyelitis optica, and PCR polymerase chain reaction.
ate to marked improvement during plasma ex- confirm the specific efficacy of therapeutic or
change, as compared with only 5.9% of patients prophylactic interventions in patients with trans-
undergoing a sham procedure.27 Hypotension, verse myelitis; therefore, recommendations are
electrolyte imbalance, coagulopathy, thrombocy- based on observational studies or clinical experi-
topenia, catheter-related thrombosis, and infec- ence with patients who have multiple sclerosis or
tion are recognized complications of plasma other neurologic diseases. Most patients with
exchange. new-onset myelitis are hospitalized for observa-
In an uncontrolled, retrospective study involv- tion and management of their condition.
ing 122 patients with transverse myelitis from
various causes, 56 patients with severe impair- Respiratory and Oropharyngeal Support
ment that did not respond to corticosteroid ther- Transverse myelitis can cause respiratory failure
apy were further treated with plasma exchange, by involving the upper cervical spinal cord and
cyclophosphamide, or both. Plasmapheresis was brain stem7; therefore, regular reassessment of
associated with an improvement among patients respiratory and oropharyngeal functions are re-
who had some remaining sensorimotor function quired during the evolution of myelitis. Dyspnea,
at the nadir of the attack, but patients who had the use of accessory muscles, or a weak cough
complete loss of sensorimotor function gener- requires further evaluation with the use of tests
ally appeared to have improvement only when of respiratory forces and pulmonary function. In-
they were treated with both cyclophosphamide tubation for mechanical ventilation is required
and plasmapheresis. Adjunctive short-term im- for some patients. Dysarthria, dysphagia, or re-
munosuppressive strategies deserve further inves- duced tongue function or gag reflex warrants a
tigation. formal investigation of the patient’s swallowing
Among patients with underlying demyelinat- function to assess the need for the temporary
ing disease, long-term immunomodulatory or placement of a feeding tube, through which ad-
immunosuppressive therapies have been shown equate nutrition can be provided while the risk of
to reduce the risk of future attacks.30,31 A discus- aspiration pneumonia is minimized.
sion of these therapies is beyond the scope of
this article. Motor Weakness and Complications of Immobilization
Administration of low-molecular-weight heparin
Treatment of Symptoms and Complications for prophylaxis against deep-vein thrombosis is
There are several important stabilizing and pre- warranted for all patients with immobility.32 Non-
ventive measures that can be taken to reduce the ambulatory patients benefit from frequent ad-
symptoms and complications of transverse my- justments of their position while they are sitting
elitis (Table 2 in the Supplementary Appendix). or in bed to promote comfort and maintain skin
No data from randomized trials are available to integrity. Collaboration with a physical medicine
n engl j med 363;6 nejm.org august 5, 2010 569
The New England Journal of Medicine
Downloaded from nejm.org by DAYA KRISHNA JHA on December 3, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
team should be considered so that multidisci- placebo and amantadine for the treatment of fa-
plinary neurorehabilitation can be initiated early.33 tigue associated with multiple sclerosis,44 but larg-
Ambulation can be aided with the use of appro- er, controlled trials are required to corroborate this
priate devices. An oral sustained-release potassi- finding. Stimulants such as dextroamphetamine or
um-channel blocker, 4-aminopyridine, has been methylphenidate are occasionally used to treat se-
shown to improve walking speed in patients with vere, refractory fatigue that occurs after an epi-
multiple sclerosis, possibly by prolonging the du- sode of myelitis, but the usefulness of these agents
ration of the action potential, although this agent in treating patients with myelitis has not been
has not been studied specifically in patients with tested in randomized, controlled trials.
transverse myelitis.34
Genitourinary and Bowel Dysfunction
Abnormalities of Tone The placement of a urethral catheter is usually
Severe myelitis may be associated with hypotonia necessary during the acute phase of transverse
in the acute phase (during spinal shock), but this is myelitis, owing to retention of urine in the blad-
typically followed by the emergence of increased der. After the acute phase, detrusor hyperreflexia
resistance to movement (tonic spasticity), along typically develops and is characterized by urinary
with involuntary muscle spasms (phasic spastic- frequency, urgency, urge incontinence, and the
ity). Spasticity is an adaptive response that can perception of bladder spasms.45 These symptoms
facilitate ambulation, but when it is excessive, are usually reduced with the administration of
painful, or intrusive, it may require treatment anticholinergic agents (e.g., oxybutynin and tolt-
with physical therapy and medications. Data from erodine).30,46 Less frequently, there is inadequate
controlled trials support the benefits of baclofen, relaxation of bladder sphincters during detrusor
tizanidine, and benzodiazepines for the treat- contraction (detrusor–sphincter dyssynergia), re-
ment of patients with spasticity associated with sulting in retention of urine, with an increased
disorders of the brain and spinal cord.35 risk of vesicoureteral reflux, infection, and cal-
culus formation. Urinary symptoms are unreli-
Pain able in differentiating poor bladder compliance
Pain is common during and after an attack of (failure to store urine) from bladder retention.
myelitis and can be caused by direct neural injury Ultrasonographic assessment of residual urine
(neuropathic pain), orthopedic factors (e.g., pain volume in the bladder after voiding is useful to
due to postural derangements or bursitis), spas- rule out urinary retention, but urodynamic studies
ticity, or some combination of these factors. may be required to fully characterize the urinary
Neuropathic pain may respond to treatment with dysfunction.45 Drugs that inhibit α1-adrenergic re-
anticonvulsant agents, antidepressant medica- ceptors can promote urinary sphincter relaxation
tions (tricyclic antidepressants and reuptake in- and bladder emptying in patients with excess
hibitors of serotonin and norepinephrine), non- sphincter activity, but some patients require in-
steroidal analgesics, and narcotics.30,36-40 termittent catheterization to adequately empty
their bladder.47
Fatigue In the acute and chronic phases of transverse
Reduced mobility, medications, pain, and other fac- myelitis, bowel dysfunction is characterized by
tors can contribute to excessive fatigue after an epi- constipation and the risk of impaction, difficulty
sode of myelitis; systematic evaluation and man- with bowel evacuation from the rectal vault, and
agement of the causes of the fatigue are warranted in some cases incontinence, which is usually as-
(Table 2 in the Supplementary Appendix). Phar- sociated with an inadequate bowel program to
macotherapy is reserved for cases in which these reduce constipation and control the timing of
causes have been ruled out or treated.41 Data from defecation.30
randomized, controlled trials have shown the effi- Sexual dysfunction is a frequent consequence
cacy of amantadine for the treatment of fatigue as- of transverse myelitis and may be manifested as
sociated with multiple sclerosis, and in one study 42 reduced genital sensation, pain, reduced ability
— but not another 43 — modafinil was shown to be to achieve arousal, or anorgasmia.48 Therapeutic
beneficial. A randomized, blinded, crossover, pilot options are outlined in Table 2 in the Supple-
study showed that acetyl L-carnitine was superior to mentary Appendix.
570 n engl j med 363;6 nejm.org august 5, 2010
The New England Journal of Medicine
Downloaded from nejm.org by DAYA KRISHNA JHA on December 3, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
clinical pr actice
Psychiatric Considerations ratory tests, and an MRI study of the brain, to-
Mood and anxiety disorders are among the most gether with an assessment of the characteristics
common long-term consequences of transverse of the spinal cord lesion, allow for a rapid assess-
myelitis and influence other symptoms, such as ment of the likelihood that the episode of trans-
pain and sexual function. Pharmacotherapy is verse myelitis is associated with an infection, an
commonly prescribed, either alone or in conjunc- underlying systemic disease, or a demyelinating
tion with psychological counseling. disease such as multiple sclerosis. Admission to
the hospital is warranted for observation of the
A r e a s of Uncer ta in t y evolution of the syndrome and for treatment of
the patient. Data from randomized trials to in-
Identifying the cause of transverse myelitis is of- form the treatment specifically for patients with
ten challenging, and in many circumstances the transverse myelitis are lacking; however, on the
cause remains unknown. The yield of several tests basis of clinical experience and trials involving
appears to be low, and there is no consensus re- patients with other demyelinating diseases, high-
garding the optimal evaluation in terms of cost- dose corticosteroids are considered to be the
effectiveness. Data from randomized trials to guide first-line therapy. Assessments by physical and
decisions regarding initial therapy, indications for occupational therapists and treatment of symp-
intensification of treatment, and the optimal toms such as pain and urinary dysfunction are
management of associated symptoms are scarce. indicated. Counseling about the natural history
of transverse myelitis and the prognosis must be
Guidel ine s given on an individual basis, depending on the
cause of the condition (if it is identified), and
Consensus criteria for the diagnosis of transverse patients and families should be offered support
myelitis have been developed.1 However, to our in managing this debilitating condition.
knowledge, there are no professional guidelines Dr. Frohman reports receiving speaking fees from Biogen
for the management of transverse myelitis. Idec, Teva Neuroscience, Bayer, and Novartis and consulting fees
from Biogen Idec, Teva Neuroscience, Abbott, and Genzyme;
and Dr. Wingerchuk, receiving research support from Alexion,
C onclusions a nd Genzyme, Genentech, Organon (now part of Merck), and the
R ec om mendat ions National Multiple Sclerosis Society and consulting fees from
Novartis, Teva Neuroscience, VLST, and the Guthy–Jackson
Charitable Foundation. No other potential conflict of interest
The patient described in the vignette presented relevant to this article was reported.
with classic clinical and neuroimaging manifes- Disclosure forms provided by the authors are available with
tations of acute transverse myelitis. Information the full text of this article at NEJM.org.
We thank Marvin Ruona, Mayo Clinic Media Support Ser-
obtained from the clinical history, an analysis of vices, for assistance with Figure 1 in the Supplementary Ap-
the cerebrospinal fluid, the results of other labo- pendix.
References
1. Transverse Myelitis Consortium Work- SJ, Lucchinetti CF, Weinshenker BG. Re- 11. Debette S, de Sèze J, Pruvo JP, et al.
ing Group. Proposed diagnostic criteria vised diagnostic criteria for neuromyelitis Long-term outcome of acute and subacute
and nosology of acute transverse myelitis. optica. Neurology 2006;66:1485-9. myelopathies. J Neurol 2009;256:980-8.
Neurology 2002;59:499-505. 7. Wingerchuk DM, Lennon VA, Lucchi- 12. Pidcock FS, Krishnan C, Crawford
2. Kaplin AI, Krishnan C, Deshpande netti CF, Pittock SJ, Weinshenker BG. The TO, Salorio CF, Trovato M, Kerr DA. Acute
DM, Pardo CA, Kerr DA. Diagnosis and spectrum of neuromyelitis optica. Lancet transverse myelitis in childhood: center-
management of acute myelopathies. Neu- Neurol 2007;6:805-15. based analysis of 47 cases. Neurology
rologist 2005;11:2-18. 8. de Seze J, Lanctin C, Lebrun C, et al. 2007;68:1474-80.
3. Jacob A, Weinshenker BG. An approach Idiopathic acute transverse myelitis: appli- 13. Kumar N, Frohman EM. Spinal neuro-
to the diagnosis of acute transverse myeli- cation of the recent diagnostic criteria. sarcoidosis mimicking an idiopathic in-
tis. Semin Neurol 2008;28:105-20. Neurology 2005;65:1950-3. flammatory demyelinating syndrome.
4. Wingerchuk DM. Postinfectious en- 9. Berman M, Feldman S, Alter M, Zilber Arch Neurol 2004;61:586-9.
cephalomyelitis. Curr Neurol Neurosci N, Kahana E. Acute transverse myelitis: 14. Pittock SJ, Lucchinetti CF. Inflamma-
Rep 2003;3:256-64. incidence and etiologic considerations. tory transverse myelitis: evolving con-
5. de Seze J, Stojkovic T, Breteau G, et al. Neurology 1981;31:966-71. cepts. Curr Opin Neurol 2006;19:362-8.
Acute myelopathies: clinical, laboratory 10. Bhat A, Naguwa S, Cheema G, Gersh- 15. Pittock SJ, Lennon VA, de Seze J, et al.
and outcome profiles in 79 cases. Brain win ME. The epidemiology of transverse Neuromyelitis optica and non organ-spe-
2001;124:1509-21. myelitis. Autoimmun Rev 2010;9:A395- cific autoimmunity. Arch Neurol 2008;65:
6. Wingerchuk DM, Lennon VA, Pittock A399. 78-83.
n engl j med 363;6 nejm.org august 5, 2010 571
The New England Journal of Medicine
Downloaded from nejm.org by DAYA KRISHNA JHA on December 3, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
clinical pr actice
16. Scott TF. Nosology of idiopathic trans- tem inflammatory demyelinating disease. for neuropathic pain. Cochrane Database
verse myelitis syndromes. Acta Neurol Ann Neurol 1999;46:878-86. Syst Rev 2005;3:CD005454.
Scand 2007;115:371-6. 28. Watanabe S, Nakashima I, Misu T, et al. 40. Wiffen PJ, McQuay HJ, Moore RA.
17. Compston A, Coles A. Multiple sclero- Therapeutic efficacy of plasma exchange Carbamazepine for acute and chronic
sis. Lancet 2008;372:1502-17. in NMO-IgG-positive patients with neuro- pain. Cochrane Database Syst Rev 2005;3:
18. Wingerchuk DM, Hogancamp WF, myelitis optica. Mult Scler 2007;13:128-32. CD005451.
O’Brien PC, Weinshenker BG. The clinical 29. Bonnan M, Valentino R, Olindo S, 41. Brañas P, Jordan R, Fry-Smith A, Burls
course of neuromyelitis optica (Devic’s Mehdaoui H, Smadja D, Cabre P. Plasma A, Hyde C. Treatments for fatigue in mul-
syndrome). Neurology 1999;53:1107-14. exchange in severe spinal attacks associ- tiple sclerosis: a rapid and systematic re-
19. Misu T, Fujihara K, Nakashima I, Sato ated with neuromyelitis optica spectrum view. Health Technol Assess 2000;4:1-61.
S, Itoyama Y. Intractable hiccup and nau- disorder. Mult Scler 2009;15:487-92. 42. Rammohan KW, Rosenberg JH, Lynn
sea with periaqueductal lesions in neuro- 30. Courtney AM, Treadaway K, Reming- DJ, Blumenfeld AM, Pollak CP, Nagaraja
myelitis optica. Neurology 2005;65:1479- ton G, Frohman EM. Multiple sclerosis. HN. Efficacy and safety of modafinil
82. Med Clin North Am 2009;93:451-76. (Provigil) for the treatment of fatigue in
20. Lennon VA, Wingerchuk DM, Kryzer 31. Wingerchuk DM, Weinshenker BG. multiple sclerosis: a two centre phase 2
TJ, et al. A serum autoantibody marker of Neuromyelitis optica. Curr Treat Options study. J Neurol Neurosurg Psychiatry 2002;
neuromyelitis optica: distinction from mul- Neurol 2008;10:55-66. 72:179-83.
tiple sclerosis. Lancet 2004;364:2106-12. 32. Spivack SB, Aisen ML. A comparison 43. Stankoff B, Waubant E, Confavreux C,
21. Lennon VA, Kryzer TJ, Pittock SJ, of low molecular weight heparin and low et al. Modafinil for fatigue in MS: a ran-
Verkman AS, Hinson SR. IgG marker of dose unfractionated heparin prophylaxis domized placebo-controlled double-blind
optic-spinal multiple sclerosis binds to in subacute myelopathy. J Spinal Cord Med study. Neurology 2005;64:1139-43.
the aquaporin-4 water channel. J Exp Med 1997;20:402-5. 44. Tomassini V, Pozzilli C, Onesti E, et al.
2005;202:473-7. 33. Kesselring J, Beer S. Symptomatic Comparison of the effects of acetyl L-car-
22. Weinshenker BG, Wingerchuk DM, therapy and neurorehabilitation in multi- nitine and amantadine for the treatment
Vukusic S, et al. Neuromyelitis optica IgG ple sclerosis. Lancet Neurol 2005;4:643- of fatigue in multiple sclerosis: results of
predicts relapse after longitudinally ex- 52. a pilot, randomised, double-blind, cross-
tensive transverse myelitis. Ann Neurol 34. Goodman AD, Brown TR, Krupp LB, over trial. J Neurol Sci 2004;218:103-8.
2006;59:566-9. et al. Sustained-release oral fampridine in 45. Lemack GE, Frohman EM, Zimmern
23. Hummers LK, Krishnan C, Casciola- multiple sclerosis: a randomised, double- PE, Hawker K, Ramnarayan P. Urodynam-
Rosen L, et al. Recurrent transverse myeli- blind, controlled trial. Lancet 2009;373: ic distinctions between idiopathic detru-
tis associates with anti-Ro (SSA) autoanti- 732-8. sor overactivity and detrusor overactivity
bodies. Neurology 2004;62:147-9. 35. Groves L, Shellenberger MK, Davis CS. secondary to multiple sclerosis. Urology
24. Greenberg BM, Thomas KP, Krishnan Tizanidine treatment of spasticity: a meta- 2006;67:960-4.
C, Kaplin AI, Calabresi PA, Kerr DA. Idio- analysis of controlled, double-blind, com- 46. Abrams P, Freeman R, Anderström C,
pathic transverse myelitis: corticosteroids, parative studies with baclofen and diaze- Mattiasson A. Tolterodine, a new anti-
plasma exchange, or cyclophosphamide. pam. Adv Ther 1998;15:241-51. muscarinic agent: as effective but better
Neurology 2007;68:1614-7. 36. Namaka M, Leong C, Grossberndt A, tolerated than oxybutinin in patients with
25. Frohman EM, Shah A, Eggenberger E, et al. A treatment algorithm for neuro- an overactive bladder. Br J Urol 1998;81:
Metz L, Zivadinov R, Stüve O. Corticoste pathic pain: an update. Consult Pharm 801-10.
roids for multiple sclerosis: I. Application 2009;24:885-902. 47. Bennett JK, Foote J, El-Leithy TR, et al.
for treating MS exacerbations. Neurothera- 37. Saarto T, Wiffen PJ. Antidepressants Terazosin for vesicosphincter dyssynergia
peutics 2007;4:618-26. for neuropathic pain. Cochrane Database in spinal cord-injured male patients. Mol
26. Martinelli V, Rocca MA, Annovazzi P, Syst Rev 2007;4:CD005454. Urol 2000;4:415-20.
et al. A short-term randomized MRI study 38. Tzellos TG, Papazisis G, Amaniti E, 48. Fletcher SG, Castro-Borrero W, Rem-
of high-dose oral vs intravenous methyl- Kouvelas D. Efficacy of pregabalin and ington G, Treadaway K, Lemack GE, Froh
prednisolone in MS. Neurology 2009;73: gabapentin for neuropathic pain in spinal- man EM. Sexual dysfunction in patients
1842-8. cord injury: an evidence-based evaluation with multiple sclerosis: a multidisciplinary
27. Weinshenker BG, O’Brien PC, Petter- of the literature. Eur J Clin Pharmacol approach to evaluation and management.
son TM, et al. A randomized trial of plas- 2008;64:851-8. Nat Clin Pract Urol 2009;6:96-107.
ma exchange in acute central nervous sys- 39. Saarto T, Wiffen PJ. Antidepressants Copyright © 2010 Massachusetts Medical Society.
collections of articles on the journal’s web site
The Journal’s Web site (NEJM.org) sorts published articles into
more than 50 distinct clinical collections, which can be used as convenient
entry points to clinical content. In each collection, articles are cited in reverse
chronologic order, with the most recent first.
572 n engl j med 363;6 nejm.org august 5, 2010
The New England Journal of Medicine
Downloaded from nejm.org by DAYA KRISHNA JHA on December 3, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
Vous aimerez peut-être aussi
- Multiple Sclerosis: Practical Comprehensive EssentialsD'EverandMultiple Sclerosis: Practical Comprehensive EssentialsPas encore d'évaluation
- A Serum Autoantibody Marker of Neuromyelitis Optica: Distinction From Multiple SclerosisDocument7 pagesA Serum Autoantibody Marker of Neuromyelitis Optica: Distinction From Multiple SclerosistiaraleshaPas encore d'évaluation
- Guillain-Barré Syndrome OtrDocument5 pagesGuillain-Barré Syndrome OtrMariam PlataPas encore d'évaluation
- A Pattern Recognition Approach To Myopathy. CONTINUUMDocument24 pagesA Pattern Recognition Approach To Myopathy. CONTINUUMjorgegrodlPas encore d'évaluation
- Workshop E - Bundle 2019 - Electro-274-295Document22 pagesWorkshop E - Bundle 2019 - Electro-274-295adaptacion neonatal100% (1)
- Chorea Continuum 2019Document35 pagesChorea Continuum 2019nicolasPas encore d'évaluation
- A Clinician's Approach To Peripheral NeuropathyDocument12 pagesA Clinician's Approach To Peripheral Neuropathytsyrahmani100% (1)
- Motor Neuron DiseaseDocument7 pagesMotor Neuron DiseasegeraldineongPas encore d'évaluation
- Neurologyinafrica Bora Complete BookDocument432 pagesNeurologyinafrica Bora Complete Bookgus_lions100% (1)
- 34 - Polyneuropathy Classification by NCS and EMGDocument16 pages34 - Polyneuropathy Classification by NCS and EMGMutiara Kristiani PutriPas encore d'évaluation
- Vol 22.4 - Movement Disorders.2016Document304 pagesVol 22.4 - Movement Disorders.2016paslaru danPas encore d'évaluation
- TuberculomaDocument7 pagesTuberculomaAdelePas encore d'évaluation
- CP Angle TumorsDocument65 pagesCP Angle TumorsDiah VerawatiPas encore d'évaluation
- Middle Cerebral ArteryDocument4 pagesMiddle Cerebral Arterykat9210Pas encore d'évaluation
- Transverse MyelitisDocument19 pagesTransverse MyelitisAnonymous YHQmN8a01100% (1)
- Vertigo and Dizziness in The ElderlyDocument6 pagesVertigo and Dizziness in The ElderlyCarmen DélanoPas encore d'évaluation
- Autoimmune Axonal Neuropathies. 2023Document15 pagesAutoimmune Axonal Neuropathies. 2023Arbey Aponte PuertoPas encore d'évaluation
- Motor Neuron DiseaseDocument8 pagesMotor Neuron DiseaseyigoPas encore d'évaluation
- Approach To Myelopathy.4Document21 pagesApproach To Myelopathy.4NitishPas encore d'évaluation
- Acute and Chronic Chorea in Childhood: Donald L. Gilbert, MD, MSDocument6 pagesAcute and Chronic Chorea in Childhood: Donald L. Gilbert, MD, MSKalindraParahitaPas encore d'évaluation
- Spinal Cord, Root, and Plexus Disorders ComleteDocument221 pagesSpinal Cord, Root, and Plexus Disorders ComleteHastuti Erdianti HsPas encore d'évaluation
- Diagnosis and Management of Dystonia Continuum Agosto 2016Document19 pagesDiagnosis and Management of Dystonia Continuum Agosto 2016Habib G. Moutran BarrosoPas encore d'évaluation
- AAN CONTINUUM Approach To Peripheral Neuropathy Localization and DiagnosisDocument26 pagesAAN CONTINUUM Approach To Peripheral Neuropathy Localization and Diagnosisemilly vidyaPas encore d'évaluation
- Cerebellar InfarctionDocument23 pagesCerebellar InfarctionShane LuyPas encore d'évaluation
- Pediatric EpilepsyDocument6 pagesPediatric EpilepsyJosh RoshalPas encore d'évaluation
- Allen 2017Document22 pagesAllen 2017Jere AyerbePas encore d'évaluation
- Peripheral Nerve Injuries - Medical ApplicationsDocument103 pagesPeripheral Nerve Injuries - Medical ApplicationsJune Epe100% (1)
- Anterior Cruciate Ligament All InsideDocument7 pagesAnterior Cruciate Ligament All InsideVijay KumarPas encore d'évaluation
- Ring Enhancing LesionsDocument50 pagesRing Enhancing LesionsVivek GuptaPas encore d'évaluation
- Brain and Bannisters Clinical Neurology Oxford Medical Publications by Roger Bannister PDFDocument7 pagesBrain and Bannisters Clinical Neurology Oxford Medical Publications by Roger Bannister PDFBennat RajPas encore d'évaluation
- PARANEOPLASTICDocument8 pagesPARANEOPLASTICMuhammad Imran MirzaPas encore d'évaluation
- Sample Emg/Ncv Report - Normal StudyDocument5 pagesSample Emg/Ncv Report - Normal StudyPhysiotherapist AliPas encore d'évaluation
- Electrocardiographic Exercise Stress Testing PDFDocument15 pagesElectrocardiographic Exercise Stress Testing PDFRafaelDavidVillalbaRodriguezPas encore d'évaluation
- 6 - Lumbar Disc HerniationDocument24 pages6 - Lumbar Disc HerniationHADI BADWANPas encore d'évaluation
- Traumatic Brain Injury (TBI) - Definition, Epidemiology, PathophysiologyDocument10 pagesTraumatic Brain Injury (TBI) - Definition, Epidemiology, Pathophysiologypetremure2147Pas encore d'évaluation
- Brain and Bannisters Clinical Neurology Oxford Medical Publications by Roger Bannister PDFDocument7 pagesBrain and Bannisters Clinical Neurology Oxford Medical Publications by Roger Bannister PDFBennat RajPas encore d'évaluation
- False Localising SignsDocument46 pagesFalse Localising SignsVarun B RenukappaPas encore d'évaluation
- Cerebellopontine Angle TumoursDocument11 pagesCerebellopontine Angle TumoursIsmail Sholeh Bahrun MakkarattePas encore d'évaluation
- Avascular NecrosisDocument8 pagesAvascular NecrosisBobyAnugrahPas encore d'évaluation
- Spinocerebellar AtaxiasDocument50 pagesSpinocerebellar AtaxiasAshish DuggalPas encore d'évaluation
- Parkinson's DiseaseDocument17 pagesParkinson's DiseaseRafael Carrillo-BaylonPas encore d'évaluation
- Continuum 2020Document21 pagesContinuum 2020Allan Salmeron100% (1)
- Chapter 10 - Trigeminal NeuralgiaDocument5 pagesChapter 10 - Trigeminal NeuralgiaMuhammad IkbarPas encore d'évaluation
- Sensory PolyneuropathiesDocument26 pagesSensory PolyneuropathiesAnderson TravassosPas encore d'évaluation
- Ataxia Continuum Agosto 2016Document19 pagesAtaxia Continuum Agosto 2016Habib G. Moutran BarrosoPas encore d'évaluation
- Neurology Topics: Degenerative DiseasesDocument57 pagesNeurology Topics: Degenerative Diseasesलुकास विडालPas encore d'évaluation
- Stroke Rehab GuidelineDocument29 pagesStroke Rehab GuidelineDedi SutiaPas encore d'évaluation
- Spinal DysraphismDocument2 pagesSpinal DysraphismkhadzxPas encore d'évaluation
- SSPEDocument8 pagesSSPEJanellah batuaan100% (1)
- Neuromyelitis Optica Spectrum Disorder and Other.15Document30 pagesNeuromyelitis Optica Spectrum Disorder and Other.15Doaa Mokhtar100% (1)
- Cerebellar Ataxia Pathophysiology and RehabilitationDocument23 pagesCerebellar Ataxia Pathophysiology and RehabilitationMikail AtiyehPas encore d'évaluation
- B5W1L9.Peripheral Neuropathy - Lecture Notes 12Document4 pagesB5W1L9.Peripheral Neuropathy - Lecture Notes 12mihalcea alinPas encore d'évaluation
- Transverse MyelitisDocument18 pagesTransverse MyelitisNaveen KumarPas encore d'évaluation
- Approach To Stroke PatientDocument16 pagesApproach To Stroke PatientNEuRoLoGisT CoFFeeCuP100% (2)
- Somatosensory Evoked PotentialsDocument100 pagesSomatosensory Evoked PotentialsIami MenotuPas encore d'évaluation
- Enfrentamiento General ContinuumDocument28 pagesEnfrentamiento General Continuummaria palaciosPas encore d'évaluation
- Basal GangliaDocument40 pagesBasal GangliaEnkefalos KardiaPas encore d'évaluation
- Epilepsy SleepDocument19 pagesEpilepsy SleepValois MartínezPas encore d'évaluation
- Neurological ExaminationDocument23 pagesNeurological ExaminationMuhammad Fahmy100% (1)
- Diagnosis, Differential Diagnosis, And.5Document25 pagesDiagnosis, Differential Diagnosis, And.5Rahul RaiPas encore d'évaluation
- Analyzing Text - Yuli RizkiantiDocument12 pagesAnalyzing Text - Yuli RizkiantiErikaa RahmaPas encore d'évaluation
- 2-Port Antenna Frequency Range Dual Polarization HPBW Adjust. Electr. DTDocument5 pages2-Port Antenna Frequency Range Dual Polarization HPBW Adjust. Electr. DTIbrahim JaberPas encore d'évaluation
- 6.4 Past Simple Affirmative: 0 Called HadDocument1 page6.4 Past Simple Affirmative: 0 Called HadSashkaKoreckajaPas encore d'évaluation
- Public Utility Accounting Manual 2018Document115 pagesPublic Utility Accounting Manual 2018effieladurePas encore d'évaluation
- Factor Affecting Child Dental Behaviour PedoDocument19 pagesFactor Affecting Child Dental Behaviour PedoFourthMolar.comPas encore d'évaluation
- Broken Squares - Unfreezing Team Building ExerciseDocument4 pagesBroken Squares - Unfreezing Team Building Exerciselilywhite786Pas encore d'évaluation
- Animals Living in LithuaniaDocument12 pagesAnimals Living in LithuaniaSuiliwasPas encore d'évaluation
- Thermoplastics Are Defined As Polymers That Can Be Melted and Recast AlmostDocument5 pagesThermoplastics Are Defined As Polymers That Can Be Melted and Recast AlmostMnemosynePas encore d'évaluation
- Your Brain Is NOT A ComputerDocument10 pagesYour Brain Is NOT A ComputerAbhijeetPas encore d'évaluation
- Orthodox Pebbles Raising of LazarusDocument29 pagesOrthodox Pebbles Raising of LazarusMonica DavidPas encore d'évaluation
- The Convergent Parallel DesignDocument8 pagesThe Convergent Parallel Designghina88% (8)
- Binder1 CARENCRODocument27 pagesBinder1 CARENCROAddisu TsehayPas encore d'évaluation
- Chemistry: Presented By: Mrs. Marie Nella T. VictoriaDocument75 pagesChemistry: Presented By: Mrs. Marie Nella T. VictoriaJESPHER GARCIAPas encore d'évaluation
- Simile ListDocument3 pagesSimile ListFiona SohPas encore d'évaluation
- Ring Spinning Machine LR 6/S Specification and Question AnswerDocument15 pagesRing Spinning Machine LR 6/S Specification and Question AnswerPramod Sonbarse100% (3)
- (Promotion Policy of APDCL) by Debasish Choudhury: RecommendationDocument1 page(Promotion Policy of APDCL) by Debasish Choudhury: RecommendationDebasish ChoudhuryPas encore d'évaluation
- Notice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsDocument2 pagesNotice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsJustia.comPas encore d'évaluation
- Age of Sigmar AoS - Battletome - Hedonites of Slaanesh - Errata 2023-01Document4 pagesAge of Sigmar AoS - Battletome - Hedonites of Slaanesh - Errata 2023-01Ughu RajaPas encore d'évaluation
- Vocab Money HeistDocument62 pagesVocab Money HeistCivil EngineeringPas encore d'évaluation
- Dolphin Is An a-WPS OfficeDocument3 pagesDolphin Is An a-WPS Officeinova ilhamiPas encore d'évaluation
- Andrea Falcon - Aristotle On How Animals MoveDocument333 pagesAndrea Falcon - Aristotle On How Animals MoveLigia G. DinizPas encore d'évaluation
- Farewell Address WorksheetDocument3 pagesFarewell Address Worksheetapi-261464658Pas encore d'évaluation
- HUA 3G Capacity OptimizationDocument39 pagesHUA 3G Capacity Optimizationismail_hw91% (11)
- Towards (De-) Financialisation: The Role of The State: Ewa KarwowskiDocument27 pagesTowards (De-) Financialisation: The Role of The State: Ewa KarwowskieconstudentPas encore d'évaluation
- Guidelines On Setting Up A Newman Fellowship 2017-2018Document6 pagesGuidelines On Setting Up A Newman Fellowship 2017-2018Liz McFeelyPas encore d'évaluation
- Theories of EmotionDocument11 pagesTheories of EmotionNoman APas encore d'évaluation
- All This Comand Use To Type in NotepadDocument9 pagesAll This Comand Use To Type in NotepadBiloul ShirazPas encore d'évaluation
- Evolve Instagram Marketing Guide - From Zero To 10k PDFDocument132 pagesEvolve Instagram Marketing Guide - From Zero To 10k PDFAnjit Malviya100% (2)
- Small Scale Business ReportDocument28 pagesSmall Scale Business ReportJatin PahujaPas encore d'évaluation
- Aci - The Financial Markets Association: Examination FormulaeDocument8 pagesAci - The Financial Markets Association: Examination FormulaeJovan SsenkandwaPas encore d'évaluation
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsD'EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsPas encore d'évaluation
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDD'EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDÉvaluation : 5 sur 5 étoiles5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeD'EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeÉvaluation : 2 sur 5 étoiles2/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaD'EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)D'EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Évaluation : 3 sur 5 étoiles3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 4.5 sur 5 étoiles4.5/5 (82)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsD'EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsÉvaluation : 4 sur 5 étoiles4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisD'EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisÉvaluation : 4.5 sur 5 étoiles4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsD'EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsÉvaluation : 5 sur 5 étoiles5/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossD'EverandThe Obesity Code: Unlocking the Secrets of Weight LossÉvaluation : 4 sur 5 étoiles4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesD'EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesÉvaluation : 4.5 sur 5 étoiles4.5/5 (1412)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeD'EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeÉvaluation : 4.5 sur 5 étoiles4.5/5 (254)
- The Comfort of Crows: A Backyard YearD'EverandThe Comfort of Crows: A Backyard YearÉvaluation : 4.5 sur 5 étoiles4.5/5 (23)
- The Marshmallow Test: Mastering Self-ControlD'EverandThe Marshmallow Test: Mastering Self-ControlÉvaluation : 4.5 sur 5 étoiles4.5/5 (60)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisD'EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisÉvaluation : 5 sur 5 étoiles5/5 (8)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.D'EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Évaluation : 4.5 sur 5 étoiles4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityD'EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityÉvaluation : 4 sur 5 étoiles4/5 (5)
- To Explain the World: The Discovery of Modern ScienceD'EverandTo Explain the World: The Discovery of Modern ScienceÉvaluation : 3.5 sur 5 étoiles3.5/5 (51)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedÉvaluation : 4 sur 5 étoiles4/5 (61)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisD'EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryD'EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryÉvaluation : 4 sur 5 étoiles4/5 (46)