Académique Documents
Professionnel Documents
Culture Documents
Resp
Transféré par
Tiffany D'Alessandro Gordon0 évaluation0% ont trouvé ce document utile (0 vote)
56 vues4 pagesrespiratory lecture condensed
Copyright
© Attribution Non-Commercial (BY-NC)
Formats disponibles
DOC, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentrespiratory lecture condensed
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme DOC, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
56 vues4 pagesResp
Transféré par
Tiffany D'Alessandro Gordonrespiratory lecture condensed
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme DOC, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 4
Final Nursing 3, Things to remember
Smoking=cilia dnt work, cough out infection
Resp center = b/w pons upper medulla (co2 compensatory factor)
Neurological impulse= says breath
Breath in = decrease lung pressure/size (lower pressure outside air flow in
Aspirate= right side (most often)
Cilia= if not working can become breeding grounds for infection, cough up mucous to clear it,
hydration thins mucous
Rib cage = thoracic cage
h+h=how much o2 gets into body
Resp assessment = 1)assess chest, (resp and cardio assessment imp.),
Resp distress= retraction, grunting, nose flare, cranky (do spo2), decreased loc, diaphoresis, blue, sob
w/speaking, crowing, wheesing, stritorif under distress take spo2, ABC’S, did they aspirate? Swollow
anything? (can aspirate vomit in sleep) if severe distress only imp info is obtained
Cystic fibrosis = congenital chronic respiratory (genetic)
Know freq of uri, lower problems, allergies and reactions to them, O2 supplements?, surgeries, hx of
illness, asses cough, sputum, tobacco/alcohol use, fuctional health problems, immunizations, resp
equipment, last bm, elimination, hydration, nutritional, sleep (snore), cognitive/perceptual, self perception,
role, occupation (exposures), sex?, coping, values
#packs day x # of years smoking
Assess cough = character, timing, freq., paroxysmal (no relief) productive?
Assess sputum = color, amount, odor consistency, hemoptysis
Cough w/ sputum, blood, wheezing, chest pain or dyspnea = aspiration, airway disease, lung disease,
lft ventricular heart failure
Constipation = pressure on diaphragm cnt breath (vicodin causes constipation)
Tongue = lopsided; 7 nerve damage
Nose = flare, crust, cilia, patent, polyps
Pharynx - tonsils
Neck = trachea, offsided = collapsed lung
Chest examination = IPPA = Inspect PalpatePercussAusculation
Funnel Chest = pectus excavatum, lower sternum depressed and appears hollow
Pigeon chest = pectus carinatum; sternum protrudes out
Barrel Chest thorax is excessively large (birth/geriatric), sign of compensation of chronic lung
problems
Inspection = side of bed, rate, rhythm, depth, slope of ribs, use of accessory muscles, clubbing,
posterior chest
Normal RR = Adult 12-20, 6 yrs to 12yrs 15-25, 1yr to 5 yrs 20-40, baby 30-60
Kussmaul - deep breathing= metabolic acidosis, can be slow/fast but always deep
Chyne Stokes = end of life, slow, increase, apnea, (heart failure, bad stroke)
Kyphosis = spine bent outward (bone disease) geriatric
Scoliosis = S shaped spine
Kyphoscoliosis = hunchback deformity
Uncentered trachea = collapsed lung (deviation is away from affected side), pinpoint areas of pain
Fremitus = hands on back, thumbs together pt says 99, should vibrate same on each side = is the
vibration of mucous if heard unevenly
Percussion = not on bony mass, soft muffled sound heard over liver/spleen
Resonant = normal lung, low pitched
Tympanic = air, hyperinflation or hollow
Flat bone = dense tissue
Dull = mixed solid and lung tissue
hyper resonance = hyper inflated lungs COPD, lower pitched
Auscultation = breathing normal, abnormal, adventitious (you tube to listen), note pitch duration
and type of sound heard, listen to child w/ bell
Bronchial - louder and higher pitched; harsh, heard over the trachea
Brochovesicular = medium pitch and intensity; heard anterior ally over main-stem bronchi on
either side of sternum and posterior between scapulas
Vesicular - soft, low pitched; heard over all lung areas except major bronchi
Hear breath sounds to 10th rib posterior, ausculate to 6th rib (nipple line) anterior, 8th rib mid
axillary, listen 4 - 5 times on each side, back and under axilla
Absent or diminished = r/t decreased air flow
Bronchial or bronchovesicular = sounds heard over lung fields, consolidation or increased
density of lung tissue
Bronchophony = “99” spoken words are not distinguishable but the vocal resonance is increased
in intensity and clarity
Egophony = “E” heard over an area of consolidation or compressed lung above an effusion
Whispered Petrology = “123 whispered” a sign of consolidation
Adventitous lung sounds are caused by mucous
Ronchi = continous rumbling, snoring or rattling sound
Coarse crackles (rales) = series of short low pitched sounds, gurgling on inspiration, like blowing
bubbles in milk
Stridor = continous musical sound of constant pitch “seal bark”
Pleural friction rub = creaking or grating sound from roughened inflamed surfaces of the pleura
rubbing together
Wheeze = inspiraton/expiration = lung field, high pitched musical tone
Lung sounds can only be heard posteriorly on interiorly
Chest x-ray = preceded all other studies!!!
CT =evaluates difficult to see areas (shellfish/iodine allergies?)
Mri - images of body structures, ( No metal, wires, clips, plates)
Ventilation perfusion scan = assesses pulmonary blood flow
Pulmonary Angiography = confirm diagtnosis of PE
PET = distinguishes benign and malignant lung nodules
FVC = amt of air quickly and forcefully exhaled after max inspiration
FEV = Amount of air exhaled in the 1st second of FVC
Peak expiratory flow rate = maximum airflow rate during forced expiration
Tidal Volume - volume of air inhaled and exhaled with each breath
ERV = Air that can be forcefully exhaled after normal exhalation
RV - amount of air in the lungs after forced expiration
IRV - max amt of air that can be forcefully exhaled after normal inhalation
Bronchoscopy - biopsy - insertion of scope to airway for direct viewing and specimen collection
Mediastinoscopy - in suprasternal notch, scope inserted for inspection and biopsy of lymph nodes
Lung Biopsy - Transbronci8al - pass forceps or needle through bronchoscope for specimen, open lung
Thoracentesis - needle through chest wall to pleural space, CHEST TRAY IN ROOM (LUNG CAN
COLLAPSE!!)
Removal of fluid from lungs = better LOC immediately
Geriatric patient assessment
Barrel chest, decreased compliance/elasticity 45-90
Osteoperosis = percussion can cause fractures
Pt may not tolerate deep breaths
Peds patient resp assessment
Louder breath sounds and in abdomenal breather till 6 or 7,
Assessment = palpate, percussion (echoes), use bell
Pharmacology
Bronchodilators
drugs expand the bronchial tube by relaxing bronchial muscles
3 classes; inhalation, orally, subcutaneously, intravenously
Preterm labor bronchial dialator terbuteline subq or oral
Adrenergic - short acting works w/I minutes, last 4-8hrs short term relief of bronchoconstriction
tx of choice for acute exacerbation prevents spasm precipated by exercise/stimuli Albuterol,
Epinephrine, Alupent
Adrenergic = long acting - lasts 8-24 hrs, nocturnal control of asthma, not quick relief, exp Serevent
(seasonal allergies)
Common Bronchodilators s/e = tremors, tachycardia above 120, palpitations, (decreased in pt avoids
contact of the tongue w/ medication), hypocalcaemia
Xanthenes
Stimulates cns and respiration, dilates coronary and pulmonary vessels and causes diuresis
High incidence of side effects = nausea, headache, insomnia, gi distress, tachycardia, arrhythmias,
seizures,
Orally or IV
Caffeine (premature babes, apnea and tachycardia), aminophylline, theophylline,
Anticholinergics
Peaks 1 hr, lasts 4-6 hrs
Aerosol administration, used in combo w/ other bronchodilators
Poor absorption (few systemic effects)
Works in larger airways
Atrovent
Mucolytics
Loosen and liquefy thick mucous allowing expectoration
Dnt mix with other drugs
s/e nausea vomiting, stomatitis, runny nose is an antidote for Tylenol od
Smells and taste like rotten eggs
O2 administration
Only drug that may be administered in an emergency situation w/o order, 8-10 l,
5L copd, (retains CO2), chronic bronchitis, pts will not be able to breath if it is higher
O2 toxicity can inactivate surfactant development of ARDS, pulmonary edema, copious sputum,
fibrosis, numb tingling, hyperventilation (fetal position will help),
O2 WITH CHILDREN HAS TO HAVE HUMIDITY
Humidity above 4l/m
Complications = collapsed alveoli ( a l e ctasis), retrolental fibroplasia (fibrotic changes behind the
lens), induced apnea from co2 retention
Incentive pyrometer
200 - 300 for weak pt
Bed rest - shallow breaths not expanding fully
Flow incentive = freely movable ping pong pall, inhale to elevate ball keep floating as long as possible
Volume incentive - better choice, permits slower inspiration with breath holds up to 10 seconds
Other info
Chest pt needs med order, DOCUMENT
Steriods decrease imflammation
Use suction with lots of mucous
Physiotherapy wait 1 hr before meals and 2 hrs after
Dnt give physiotherapy if abnormal vitals, anticoagulant therapy, osteoperousis, LOC altered, exercise
intolerance
Posteral drainage - rt lung straighter anlgle, can cause hypotension coughing afterwards or suctioned,
dnt do if blue, no suction equipment, pt cnt cough,
Percussion and vibration = clapping the chest wall w/ cupped hand, vibration over affected lung area,
cystic fibrosis pt does 3x a day, dnt do over cancer, bronchospasm is increase, pain is felt, hemorrhage or
seizure is possible, osteoperosis
Nutrition = respiration issues need high protein high calorie diet into 5 or 6 small meals, ice cream will
increase calories, control weight, meds can cause anorexia
NURSE EDUCATES!! Hyperinflative lungs push on belly making them,condense info, cold temps
decrease edema,
Teach = pursed lips, diaphragmatic, used the diaphragm instead the accessory muscles to increase lung
expansion
Walk 15-20 minutes, increase hr to max, 220 - age = max hr, sleep dim lights, prop up pt on wedge,
modify med schedule, train upper extremities
Nasal polyps = bluish glossy projections in the nare,
Diviated septum = chapped lips b/c they are lip breathers, caused by trauma
Nasal fracture = know limitations look for edema, excessive swallowing indicates bleding, miningeal
tears, dx wld be airway, hemorrhage, pain, reduce edema, open airway by doing this,
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Congenital Heart Defects Test Five Nursing FourDocument6 pagesCongenital Heart Defects Test Five Nursing FourTiffany D'Alessandro GordonPas encore d'évaluation
- Bariatric DrugsDocument3 pagesBariatric DrugsTiffany D'Alessandro Gordon100% (1)
- 8/24/2010 Lecture Condensed To 3 PagesDocument3 pages8/24/2010 Lecture Condensed To 3 PagesTiffany D'Alessandro GordonPas encore d'évaluation
- Everything I Have Highlighted From 8/24/10 LecturesDocument1 pageEverything I Have Highlighted From 8/24/10 LecturesTiffany D'Alessandro GordonPas encore d'évaluation
- Nursing Exam Test V Crisis InterventionDocument3 pagesNursing Exam Test V Crisis InterventionTiffany D'Alessandro GordonPas encore d'évaluation
- Nursing Exam Questions Practice Test VDocument6 pagesNursing Exam Questions Practice Test VTiffany D'Alessandro Gordon94% (18)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- EEG ReportDocument2 pagesEEG ReportxiakenliangPas encore d'évaluation
- Referat Letak SungsangDocument13 pagesReferat Letak SungsangIsma Resti PratiwiPas encore d'évaluation
- Yoga at Your DeskDocument8 pagesYoga at Your DeskGuruprashanth Rao100% (2)
- Clinical Biomechanics - Body Alignment, Posture, and GaitDocument53 pagesClinical Biomechanics - Body Alignment, Posture, and Gaitmihaela_moldova91280% (1)
- Murphy Homeopathi Clinical Repertory PrefaceDocument5 pagesMurphy Homeopathi Clinical Repertory PrefaceKrishna25% (4)
- Hunter Education HandbookDocument210 pagesHunter Education HandbookJuan Francisco Lecay Alegre100% (1)
- Trauma: Clinical Practice Guidelines - TraumaDocument41 pagesTrauma: Clinical Practice Guidelines - TraumamuhamadmukhlisPas encore d'évaluation
- Water Seal Chest DrainageDocument5 pagesWater Seal Chest DrainageAmadelle FaithPas encore d'évaluation
- Sample Case StudyDocument38 pagesSample Case Studyanon-387573100% (3)
- ISSN 2347-2375: Conceptual Study On ShoshaDocument7 pagesISSN 2347-2375: Conceptual Study On ShosharakeshPas encore d'évaluation
- Enumeration of Human Body Parts According To AyurvedaDocument13 pagesEnumeration of Human Body Parts According To AyurvedaKrishna Venkat VPas encore d'évaluation
- Notes On Anatomy and Physiology For Yoga PDFDocument195 pagesNotes On Anatomy and Physiology For Yoga PDFPetar MogilskiPas encore d'évaluation
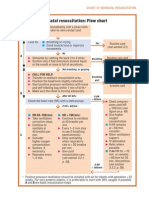
- Neonatal Resuscitation Program Flow ChartDocument3 pagesNeonatal Resuscitation Program Flow ChartChin Nam80% (5)
- Relationship Between Chapman's Reflexes and Acupuncture Meridians by Traditional Chinese Medicine Practitioners in TaiwanDocument22 pagesRelationship Between Chapman's Reflexes and Acupuncture Meridians by Traditional Chinese Medicine Practitioners in TaiwanFrederic Dubois100% (2)
- How To Sing (Meine Gesangskunst) by Lehmann, Lilli, 1848-1929Document88 pagesHow To Sing (Meine Gesangskunst) by Lehmann, Lilli, 1848-1929Gutenberg.org100% (2)
- Breathing TechniquesDocument26 pagesBreathing TechniquessherryPas encore d'évaluation
- Pediatric Chest PhysiotherapyDocument25 pagesPediatric Chest PhysiotherapyShubha DiwakarPas encore d'évaluation
- Flashcards About Medical DefinitionsDocument62 pagesFlashcards About Medical DefinitionsSrikanth PagidiPas encore d'évaluation
- Sternotomi PDFDocument11 pagesSternotomi PDFHeri PrasetyoPas encore d'évaluation
- Criminal Law CasesDocument253 pagesCriminal Law CasesMuli MJPas encore d'évaluation
- Chest PBLDocument2 pagesChest PBLRamish IrfanPas encore d'évaluation
- 1907 Towne Just How To Wake Solar PlexusDocument29 pages1907 Towne Just How To Wake Solar PlexusAlcibiades TeixeiraPas encore d'évaluation
- Illustrated Guide To The Homoeopathic Treatment Harbaris Singh Khaneja.01169 3chestDocument7 pagesIllustrated Guide To The Homoeopathic Treatment Harbaris Singh Khaneja.01169 3chestMarija VelkoskiPas encore d'évaluation
- Nursing Flash CardsDocument5 pagesNursing Flash CardsJan Clarisse RamosPas encore d'évaluation
- Gil Boyne Method of Conditioning TJDocument3 pagesGil Boyne Method of Conditioning TJsshhmmuueell100% (1)
- MRCS Part-A January 2019 RECALL PDFDocument4 pagesMRCS Part-A January 2019 RECALL PDFRajib Pal ChowdhuryPas encore d'évaluation
- Test Bank For Essentials of Medical Language 4th Edition David Allan Rachel BascoDocument61 pagesTest Bank For Essentials of Medical Language 4th Edition David Allan Rachel BascopandoraissacziaePas encore d'évaluation
- Introduction Secrets of SingingDocument26 pagesIntroduction Secrets of SingingAdrian Barilà100% (3)
- Performance Checklist (Pa)Document3 pagesPerformance Checklist (Pa)Kaye Castellano100% (1)
- Compliance and ResistanceDocument5 pagesCompliance and ResistanceNissie DegulacionPas encore d'évaluation