Académique Documents
Professionnel Documents
Culture Documents
PALS Algorithms 2019 Certification & Guidelines
Transféré par
darlingcarvajalduqueDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
PALS Algorithms 2019 Certification & Guidelines
Transféré par
darlingcarvajalduqueDroits d'auteur :
Formats disponibles
Register Now Login
PALS Algorithms 2019
(Pediatric Advanced Life
Support)
CPR for Children (CABD)
CPR for Infants (CABD)
Choking Intervention for Adults &
Children
Choking Intervention for Infants
Secondary ABCD (Child)
Airway and Breathing
Advanced Airways
Cardiac/Electrical Therapy
Cardiac Rhythms
CPR at Birth
Tachycardias
Bradycardias
Asystole
Shock
Need PALS Certification?
Certify Recertify
169 119
Continue Continue
PALS Guidelines for Hypotension
! Neonate (0 to 28 days old): SPB < 60 mmHg
! Infants (1month to 12 montsh): SBP < 70
mmHg
! Children (1yr to 10yrs): SBP < 70+(2xage in
years) mmHg
! Children (over 10yrs): SBP
These blood pressures deIning hypotension
commonly overlap with the lower normal SBP
value spectrum.
Hemodynamics
It is important to be able to categorize your
patients by their hemodynamic stability when
choosing an appropriate treatment regimen.
Stable:
! Patient presents with an arrhythmia.
! Vital signs maintain patient asymptomatic
without chest pain, shortness of breath, or
confusion.
! Patient remains conscious.
! There is a high risk for patient becoming
unstable.
Unstable:
! Patient presents with an arrhythmia.
! Vital signs cause patient to become
symptomatic with chest pain, shortness of
breath, or confusion.
! Patient has a high risk of death.
Dead:
! Patient presents with an arrhythmia.
! Patient has no pulse, is without vital signs,
and/or is unconscious.
! Best chance for success is Electrical Therapy
within 10 minutes of event!
ABG (Normal):
pH: 7.35-7.45
PaO2: 80-100 mmHg
PaCO2: 35-45 mmHg
HCO3: 22-26 mEq/L
O2 sat: 95-100% (on room air)
BE +/- 1
Lowest acceptable SBP for patients older than 1 yr
= 70+ (2 x age in years)
Cardiac arrest in the pediatric patient is also
commonly due to progressive shock.
Compensated shock can be detected by
evaluating the patient’s heart rate, presence of
peripheral pulses, intravascular volume status, and
end-organ perfusion. Sustained tachycardia can be
a sign of early cardiovascular compromise.
Bradycardia is a common sign of advanced shock
and is frequently associated with hypotension.
Basic Treatment Associated with
Stability
Stable:
O: Oxygen
M: Monitor
V: vascular access
Unstable & Dead:
I: IV access
C: CPR
E: ET intubation
D: DeIbrillator/monitor
Secondary ABCD
(Airway, Breathing, Circulation,
Differential Diagnosis)
Airway (Two Providers)
! Initially provide rescue breaths using an ambu
bag and a mask at full bow oxygen.
! Perform continued assessment of airway
patency while giving breaths. (Condensation
on mask during exhalation, chest rise, Et CO2)
! Have the person doing chest compressions
pause during the 2 rescue breaths.
If the patient is not ventilating well or if there is a
presumed risk of aspiration, insert an advanced
airway device when prudent:
Endotreacheal Intubation is the preferred method.
(View the advanced airway section)
Breathing
Con9rm correct placement of the advanced airway
device:
! Look for condensation during exhalation.
! Look for equal bilateral chest rise.
! ConIrming equal bilateral breath sounds with
auscultation.
! Auscultate stomach to assure esophageal
intubation didn’t occur.
! End-tidal CO2 should be veriIed during
exhalation using monitor or ETD
! Use portable chest x-ray.
If incorrect placement:
! Remove the airway device, ventilate the
patient using the ambu bag for a short period
of time, and then reattempt placement.
If incorrect placement:
! Secure placement of the airway device.
Continue to monitor:
! oxygenation saturation with pulse oximeter
! end-tidal CO2
Rescue breathing during CPR with an advanced
airway:
! 12-20 breaths per minute
! Chest compressions should be given
continuously at a rate of 100 to 120 per
minute.
Circulation
! Obtain IV or IO access.
! Monitors (ECG, BP cuff, pulse oximeter, et
CO2 monitor)
Identify:
! heart rhythm
! Obtain a 12 lead ECG if possible.
! Initiate therapy of PALS algorithm
corresponding with the identiIed heart
rhythm. (Drug therapy, Electrical therapy,
Pacing, etc.)
Differential Diagnosis
(needed for successful treatment of some
patients)
Consider reversible causes of rhythm/arrhythmia.
Differential Diagnosis Chart:
Airway & Breathing
There are two important principles when
evaluating the airway and breathing. First, is the
airway patent or obstructed. Second, is there
possible injury or trauma that would change the
providers method of treating an obstructed airway
or inehcient breathing.
Patent/obstructed
If the airway is patent there should be noticeable
chest rise/expansion with either spontaneous
respirations or with rescue breaths. The provider
may also be able to hear or feel the movement of
air from the patient.
A completely obstructed airway will be silent. An
awake patient will lose their ability to speak, while
both a conscious or unconscious patient will not
have breath sounds on evaluation. If the patient is
attempting spontaneous breaths without success,
there may be noticeable effort of intercostal
muscles, diaphram, or other accessory muscles
without signiIcant chest rise/expansion. The
provider will also not feel or hear the movement of
air. If the airway is partially obstructed snoring or
stridor may be heard.
Cervical Spine Injury?
If the provider evaluates the patient to have an
obstructed airway, intervention should take place.
If the adverse event of the patient was witnessed
and there is no reason to suspect a cercival spine
injury, the provider should use the head tilt-chin lift
maneuver to open the airway.
If there is a reason to suspect a cervical spine
injury, if the patient’s adverse event went
unwitnessed, if trauma occured, or the patient
suffered drowning the jaw-thrust maneuver should
be used to open the airway. If the jaw-thrust
proves unsuccessful in opening the patient’s
airway attempt an oropharangeal or
nasopharangeal airway. If neither technique works,
attempt an advanced airway using inline
stabilization.
Brain Injury?
The breathing center that controls respirations is
found within the pons and medulla of the brain
stem. If trauma, hypoxia, stroke, or any other form
of injury affects this area, changes in respiratory
function may occur. Some possible changes are
apnea (cessation of breathing), irregular breathing
patterns, or poor inspiratory volumes. If the
breathing pattern or inspiratory volumes are
inadequate to sustain life, rescue breathing will be
required, and an advanced airway should be
placed.
Oral Airway:
! Assure the artiIcial airway is the appropriate
size for the patient.
! The airway should be easily inserted with a
tongue blade.
! Avoid use in patients with an active gag rebex.
Nasal Trumpet Airway:
! Best practice is to lube before insertion.
! Careful not to cause trauma to nasal mucosa
(results in bleeding).
! This is reasonably tolerated by patients with
an active gag rebex.
Advanced Airways
Indications:
! When you are unable to open airway using
head tilt-chin lift or jaw thrust maneuvers.
! If you have dihculty forming a seal with the
face mask.
! If the patient requiring continued ventilatory
support.
! When the patient has a high risk for aspiration
(provide an ETT or Combitube).
Remember, a patient should be unconscious or
sedated without an active gag rebex before
instrumentation of the airway occurs with an ETT,
Combitube, or LMA.
Endotracheal Tube (ETT)
! Requires additional instrument for insertion
(laryngoscope, glidescope, Iberoptic).
! Laryngoscope blades (average adult size):
MAC 3 or 4, Miller 2 or 3
! Same sized laryngoscopes or smaller sizes
can be used for pediatrics.
! ETTs require mastery of technique for
consistent appropriate placement.
Average size of ETT for orotracheal intubation
(mm):
! Uncuffed: tube = (age/4)+4
! Cuffed: tube = (age/4)+3
1) The ETT is placed into the trachea, having direct
visualization of the vocal cords.
! Children over 1 year: Depth of intubation (cm)
= age/2+13
! Children under 1 year: Depth of intubation
(cm) = weight/2+8
2) Tracheal cuff of the ETT is then inbated.
! Allows for positive pressure ventilation.
! Reduces risk of aspiration.
! Helps maintain placement of ETT.
3) ConIrm placement of ETT.
4) Secure the ETT in place.
Laryngeal Mask Airway (LMA)
Visualization of the vocal cords is not required for
insertion.
! When inserting the LMA have the laryngeal
cuff debated.
! Guide in the LMA cuff without folding back the
tip, pressing it against the hard palate.
! Advance the LMA till the cuff lies in the
pharynx.
! After placement, inbate the laryngeal cuff and
check for an adequate seal by using positive
pressure ventilation.
Positive pressure ventilation is generally kept
under 20 CmH2O to prevent inbation of the
stomach.
The patient is still at high risk of aspiration, even
with an appropriately placed LMA.
Cardiac/Electrical Therapy
Transcutaneous Pacemaker
(External Pacemaker)
Used to treat unstable bradycardias not
responding to drug therapy. Provides temporary
pacing through the skin in emergency situations.
! Place pads and electrodes in correct position
to assure an appropriate ECG reading.
! Set the pacer 10-20 beats per min above the
patient’s intrinsic heart rate or 60 beats per
min if there is no intrinsic heart rate.
! Start at O mA and work energy level up until
you have capture (heart pulsation).
! Assure the patient is sedated and comfortable
during pacer delivery.
Cardioversion
! Used if drug therapy and vagal maneuvers fail.
! Used when patient has a pulse.
! Used to treat Atrial Fibrillation, Atrial Flutter,
Atrial Tach, and Symptomatic VT.
! Shock performed at peak of R wave.
! Requires proper lead/pad placement to
monitor ECG.
Pediatric shock energy level:
Monophasic or Biphasic: 0.5-1.0 J/kg
Assure the patient is sedated and comfortable
during shock delivery.
Defibrilation
! Used to treat VF and pulseless VT.
! Delivery within Irst 5 mins of cardiac arrest
has best results.
! CPR before and after each shock improves
outcomes.
Pediatric shock energy level:
Monophasic or Biphasic: 2 J/kg for the Irst
attempt and 4 J/kg for subsequent attempts.
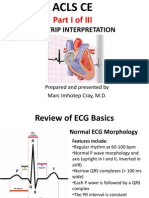
Common Cardiac Rhythms
Normal Sinus Rhythm
Atrial Tachycardia
Supraventricular Tachycardia
Atrial Fibrillation
Atrial Flutter
Sinus Bradycardia
1° Atrioventricular Block
2° Atrioventricular Block- Type 1
(Mobitz I/Wenckebach)
2° Atrioventricular Block- Type 2
(Mobitz II/Hay)
3° Atrioventricular Block
(Complete Heart Block)
Ventricular Tachycardia –
Monomorphic
Ventricular Tachycardia –
Polymorphic
Ventricular Tachycardia –
Torsades de Pointes
Ventricular Fibrillation
Asystole
Pulseless Electrical Activity (PEA)
Cardiopulmonary Resuscitation
at Birth
Vous aimerez peut-être aussi
- The Art of the Iv Start: Common Techniques and Tricks of the Trade for Establishing Successful Peripheral Intravenous LinesD'EverandThe Art of the Iv Start: Common Techniques and Tricks of the Trade for Establishing Successful Peripheral Intravenous LinesPas encore d'évaluation
- Rapid Interpretation of EKG Sixth Edition Free (PDF)Document4 pagesRapid Interpretation of EKG Sixth Edition Free (PDF)usmlematerials.net0% (3)
- Advanced Cardiac Life Support Quick Study Guide 2015 Updated GuidelinesD'EverandAdvanced Cardiac Life Support Quick Study Guide 2015 Updated GuidelinesÉvaluation : 4 sur 5 étoiles4/5 (6)
- 2021 ACLS Study GuideDocument20 pages2021 ACLS Study GuideShane Brown83% (12)
- Acls Study GuideDocument24 pagesAcls Study GuideMohammad Gita100% (17)
- Advance Cardiac Life Support: Short, Sweet and to the PointD'EverandAdvance Cardiac Life Support: Short, Sweet and to the PointÉvaluation : 3 sur 5 étoiles3/5 (2)
- CEN+Online+Review Module+12 Final GENITODocument26 pagesCEN+Online+Review Module+12 Final GENITOTamara Cooper67% (3)
- Paramedic PowerpointDocument43 pagesParamedic PowerpointKayMelton100% (1)
- Pediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesD'EverandPediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesÉvaluation : 5 sur 5 étoiles5/5 (2)
- Study Guide: MandatoryDocument24 pagesStudy Guide: Mandatorybooksir86% (7)
- BLS Acls Aha 2020Document103 pagesBLS Acls Aha 2020Nicholas PetrovskiPas encore d'évaluation
- Manual de RCP - NEONATAL - 7°ED PDFDocument328 pagesManual de RCP - NEONATAL - 7°ED PDFNatanael Librado97% (29)
- ACLS Megacode Testing ScenariosDocument12 pagesACLS Megacode Testing Scenariosealm10100% (2)
- PALS Pamphlet Edited PDFDocument4 pagesPALS Pamphlet Edited PDFsaleem50% (4)
- ACLS Provider Manual Supplementary Material: © 2020 American Heart AssociationDocument75 pagesACLS Provider Manual Supplementary Material: © 2020 American Heart AssociationpolelPas encore d'évaluation
- Acls PDFDocument194 pagesAcls PDFbenny christanto100% (3)
- Third Spacing - Where Has All The Fluid GoneDocument14 pagesThird Spacing - Where Has All The Fluid Gonedbryant0101100% (15)
- Pediatric Advanced Life Support (PALS) Provider HandbookD'EverandPediatric Advanced Life Support (PALS) Provider HandbookPas encore d'évaluation
- PALS Study GuideDocument25 pagesPALS Study GuideVitor Hugo G CorreiaPas encore d'évaluation
- CEN+Online+Review Module+8 FinalDocument36 pagesCEN+Online+Review Module+8 FinalTamara Cooper100% (2)
- Acls Pre Course Self Assessment Study GuideDocument7 pagesAcls Pre Course Self Assessment Study Guidenova939100% (5)
- Pals 2011Document21 pagesPals 2011Saúl Chilón69% (13)
- BLS Cheatsheet for Basic Life Support ExamDocument18 pagesBLS Cheatsheet for Basic Life Support ExamMoxie MacadoPas encore d'évaluation
- Advanced Cardiovascular Life Support Pro PDFDocument194 pagesAdvanced Cardiovascular Life Support Pro PDFAnkitBhandariPas encore d'évaluation
- PALS Study Guide and UpdatesDocument50 pagesPALS Study Guide and UpdatesKellie Pacanowski100% (2)
- Critical Care Transport ParamedicDocument3 pagesCritical Care Transport Paramedicapi-121427596Pas encore d'évaluation
- ACLS Algorithms 2020 (Advanced Cardiac Life Support)Document1 pageACLS Algorithms 2020 (Advanced Cardiac Life Support)evelyn k100% (2)
- PALS Provider Manual PDFDocument57 pagesPALS Provider Manual PDFtimie_reyes90% (21)
- ACLS Study Guide JULY 2021 UPDATEDocument3 pagesACLS Study Guide JULY 2021 UPDATENina Morada100% (2)
- PALS 2020 guidelines-AHA1Document69 pagesPALS 2020 guidelines-AHA1NICU PICUPas encore d'évaluation
- PALS Practice CaseDocument88 pagesPALS Practice CaseSugi Deny0% (1)
- Study Guide Emergency and Trauma NursingDocument11 pagesStudy Guide Emergency and Trauma NursingMarie Angelique Cruz Crestani100% (5)
- ACLS CE-Part I of III - ECG Strip Interpretation W Case Scenarios SupplementalDocument80 pagesACLS CE-Part I of III - ECG Strip Interpretation W Case Scenarios SupplementalMarc Imhotep Cray, M.D.100% (2)
- Tips For PALS ExamDocument3 pagesTips For PALS ExamAy Men Alej91% (11)
- Electrocardiography in Emergency, Acute, and Critical Care, 2nd EditionD'EverandElectrocardiography in Emergency, Acute, and Critical Care, 2nd EditionÉvaluation : 5 sur 5 étoiles5/5 (1)
- Acls StudypackDocument14 pagesAcls Studypackbethchaygwapa100% (2)
- Certified Pediatric Emergency Nurse Review: Putting It All TogetherD'EverandCertified Pediatric Emergency Nurse Review: Putting It All TogetherPas encore d'évaluation
- PALS Pre-course Self-Assessment GuideDocument20 pagesPALS Pre-course Self-Assessment GuideLawrence Gabriel80% (5)
- EMRA Sepsis CardDocument4 pagesEMRA Sepsis Cardsgod34100% (1)
- Pals Studyguide Jan2021Document3 pagesPals Studyguide Jan2021prippon100% (2)
- ACLS Study Guide 2016: Essentials for Passing ExamDocument2 pagesACLS Study Guide 2016: Essentials for Passing Examnova939100% (2)
- ACLS Advanced Cardiovascular Life Support Provider Manual 2023D'EverandACLS Advanced Cardiovascular Life Support Provider Manual 2023Pas encore d'évaluation
- PADIS Guidelines Teaching Slides ImmobilityDocument25 pagesPADIS Guidelines Teaching Slides ImmobilityDaniel Lago BorgesPas encore d'évaluation
- PALS Pre StudyDocument28 pagesPALS Pre Studynursesed100% (7)
- Prehospital Practice: hypothetically speaking: From classroom to paramedic practice Volume 1 Second editionD'EverandPrehospital Practice: hypothetically speaking: From classroom to paramedic practice Volume 1 Second editionPas encore d'évaluation
- ACLS AlgorithmsDocument4 pagesACLS Algorithmsmonickams100% (1)
- PALS Study Guide Short FormDocument11 pagesPALS Study Guide Short FormLenTheRN88% (8)
- Pals Study GuideDocument8 pagesPals Study Guidefredyromanreyes100% (2)
- Early Progressive Mobility Protocol: Step 1: Screen For SafetyDocument2 pagesEarly Progressive Mobility Protocol: Step 1: Screen For SafetydarlingcarvajalduquePas encore d'évaluation
- Early Progressive Mobility Protocol: Step 1: Screen For SafetyDocument2 pagesEarly Progressive Mobility Protocol: Step 1: Screen For SafetydarlingcarvajalduquePas encore d'évaluation
- Pals UptodateDocument28 pagesPals UptodatejdanielcasPas encore d'évaluation
- AHA PALS Core Case Test ChecklistsDocument12 pagesAHA PALS Core Case Test ChecklistsVitor Hugo G CorreiaPas encore d'évaluation
- PALS Interim Material 2020 - Provider Manual ChangesDocument3 pagesPALS Interim Material 2020 - Provider Manual ChangesyossyusPas encore d'évaluation
- ACLS PRE-TEST KEYDocument19 pagesACLS PRE-TEST KEYMohammed Abdou92% (13)
- PALS Algorithms for Shock, Respiratory Emergencies & MoreDocument11 pagesPALS Algorithms for Shock, Respiratory Emergencies & MoreGracia VitaPas encore d'évaluation
- Emergency Department Resuscitation of the Critically Ill, 2nd Edition: A Crash Course in Critical CareD'EverandEmergency Department Resuscitation of the Critically Ill, 2nd Edition: A Crash Course in Critical CarePas encore d'évaluation
- Pediatric Pain AssessmentDocument10 pagesPediatric Pain AssessmentdarlingcarvajalduquePas encore d'évaluation
- Protocolo FATE (Eco TT)Document4 pagesProtocolo FATE (Eco TT)darlingcarvajalduquePas encore d'évaluation
- Drug Doses 2017Document127 pagesDrug Doses 2017Yuliawati HarunaPas encore d'évaluation
- PALS Precourse Self-AssessmentDocument2 pagesPALS Precourse Self-AssessmentGabriel Del RosarioPas encore d'évaluation
- Acls DrugsDocument5 pagesAcls DrugsDebby Christiana SPas encore d'évaluation
- Stollings2021 Article DeliriumInCriticalIllnessCliniDocument15 pagesStollings2021 Article DeliriumInCriticalIllnessCliniJavier BlancPas encore d'évaluation
- Httpswatermark Silverchair Com - Ezproxy.unbosque - edu.Copedsinreview.2022005642.Pdftoken AQECAHi208BE49Ooan9kkhW Ercy7Dm3ZL 9Document10 pagesHttpswatermark Silverchair Com - Ezproxy.unbosque - edu.Copedsinreview.2022005642.Pdftoken AQECAHi208BE49Ooan9kkhW Ercy7Dm3ZL 9darlingcarvajalduquePas encore d'évaluation
- Nihms 1646158Document30 pagesNihms 1646158darlingcarvajalduquePas encore d'évaluation
- 2020 ESPNIC PEMVECC COVID-19 Practice RecommendationsDocument7 pages2020 ESPNIC PEMVECC COVID-19 Practice RecommendationsdmallozziPas encore d'évaluation
- Getattachmentnonopioid Medication Options PDFDocument1 pageGetattachmentnonopioid Medication Options PDFdarlingcarvajalduquePas encore d'évaluation
- Prevención Neumonia Asociada A Ventilación.Document19 pagesPrevención Neumonia Asociada A Ventilación.darlingcarvajalduquePas encore d'évaluation
- Updated Nomenclature of DeliriumDocument3 pagesUpdated Nomenclature of Deliriumken barrios montalvoPas encore d'évaluation
- Misc AbdomenDocument8 pagesMisc AbdomendarlingcarvajalduquePas encore d'évaluation
- ESPNIC Guidance On The Management of The Deteriorating Child or Cardiac Arrest of Suspected or Proven COVID FINAL PDFDocument2 pagesESPNIC Guidance On The Management of The Deteriorating Child or Cardiac Arrest of Suspected or Proven COVID FINAL PDFdarlingcarvajalduquePas encore d'évaluation
- Avances en Ultrasonido Pediatria oDocument7 pagesAvances en Ultrasonido Pediatria odarlingcarvajalduquePas encore d'évaluation
- Post-Intensive Care Syndrome: Its Pathophysiology, Prevention, and Future DirectionsDocument14 pagesPost-Intensive Care Syndrome: Its Pathophysiology, Prevention, and Future DirectionsdarlingcarvajalduquePas encore d'évaluation
- De-Escalation of Critical Care and Prevention of Iatrogenicity Through PICU Liberation Rounding Process and A Daily Rounding ChecklistDocument1 pageDe-Escalation of Critical Care and Prevention of Iatrogenicity Through PICU Liberation Rounding Process and A Daily Rounding ChecklistdarlingcarvajalduquePas encore d'évaluation
- Mortalidad e Hipotermia Vs NormotermiaDocument8 pagesMortalidad e Hipotermia Vs NormotermiadarlingcarvajalduquePas encore d'évaluation
- Torsade de Pointes - The Clinical Considerations PDFDocument6 pagesTorsade de Pointes - The Clinical Considerations PDFdarlingcarvajalduquePas encore d'évaluation
- Q SofaDocument9 pagesQ SofadarlingcarvajalduquePas encore d'évaluation
- Choque Cardiogenico MicrocirculacionDocument6 pagesChoque Cardiogenico MicrocirculaciondarlingcarvajalduquePas encore d'évaluation
- Q SofaDocument9 pagesQ SofadarlingcarvajalduquePas encore d'évaluation
- Posición PronoDocument6 pagesPosición PronodarlingcarvajalduquePas encore d'évaluation
- Pals TachycardiaDocument1 pagePals TachycardiadarlingcarvajalduquePas encore d'évaluation
- Pals Pediatric BradycardiaDocument1 pagePals Pediatric BradycardiadarlingcarvajalduquePas encore d'évaluation
- Pals 2015 Documento CompletoDocument50 pagesPals 2015 Documento CompletodarlingcarvajalduquePas encore d'évaluation
- ANTIARRITMICOSDocument9 pagesANTIARRITMICOSdarlingcarvajalduquePas encore d'évaluation
- 2015 AHA Guidelines Highlights EnglishDocument36 pages2015 AHA Guidelines Highlights EnglishshiloinPas encore d'évaluation