Académique Documents
Professionnel Documents
Culture Documents
BBB - Respi&gi Reports
Transféré par
shesah0 évaluation0% ont trouvé ce document utile (0 vote)
72 vues11 pagesCroup is an inflammation of the larynx and trachea and bronchial passageways. It is most often self-limited, but it occasionally is severe and, rarely, fatal. In the fall, it is caused by parainfluenza virus. In winter and spring, it is usually caused by respiratory syncytial virus or an influenza virus.
Description originale:
Titre original
BBB.respi&Gi Reports
Copyright
© Attribution Non-Commercial (BY-NC)
Formats disponibles
DOC, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentCroup is an inflammation of the larynx and trachea and bronchial passageways. It is most often self-limited, but it occasionally is severe and, rarely, fatal. In the fall, it is caused by parainfluenza virus. In winter and spring, it is usually caused by respiratory syncytial virus or an influenza virus.
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme DOC, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
72 vues11 pagesBBB - Respi&gi Reports
Transféré par
shesahCroup is an inflammation of the larynx and trachea and bronchial passageways. It is most often self-limited, but it occasionally is severe and, rarely, fatal. In the fall, it is caused by parainfluenza virus. In winter and spring, it is usually caused by respiratory syncytial virus or an influenza virus.
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme DOC, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 11
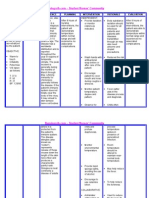
LARYNGOTRACHEOBRONCHITIS • STAGE 1 • Laryngoscopy Provide and encourage fluid intake,
• inflammation of • Fear reveals inflammation in the larygeal IV fluids may be prescribed to
the larynx and trachea and bronchial • Hoarseness spaces. maintain hydration.
passageways. • Croupy cough Medical Management Keep the child comfortable in a semi-
• it usually affects children between the • STAGE 2 Usually not necessary as croup is due seated position
ages of 6 months and 3 years. • Use of accessory muscles to a viral infection. Decrease the child's activity and
• a viral infection of the upper respiratory • Labored respiration Antibiotics are prescribed if it is a encourage rest as long as croup
tract that causes varying degrees of • STAGE 3 bacterial infection. attack persist.
airway obstruction. • Restlessness • Fever is treated with acetaminophen. Administer bronchodilators to relax
• the disease is most often self-limited, but • Anxiety Nebulized Epinephrine smooth muscles and relieve stridor.
it occasionally is severe and, rarely, fatal. • Pallor • adrenergic effects can cause mucosal Administer acetaminophen as
Causes • Sweating • vasoconstriction and subsequently prescribed to lower down fever.
Croup can be caused by a number of • STAGE 4 decreases Have a resuscitation equipment
different viruses. • Permanent cyanosis • subglottic edema Provide appropriate reassurance and
• In the fall, it is caused by • Cessation of breathing • Onset is rapid education.
parainfluenza virus. EARLY signs of impending airway • Peak is observed in 2hours
obstruction: Frequent hand washing and avoiding
• In winter and spring, it is usually • Additional doses: Intensive Care Unit contact with people who have
caused by respiratory syncytial virus 1. Increase pulse and RR ( 20-30 minutes)
2. Increase restlessness respiratory infections can lessen the
or an influenza virus. • Regular Hospital Unit ( 3-4 hours) chance of spreading the viruses that
• In some cases it is diptheric in origin. Telltale signs of croup:
Corticosteroids (Dexamethasone) cause croup.
Pathophysiology • BARKING COUGH
- anti inflammatory effects decrease Avoidance of solid foods for first few
Infiltration of Para Influenza Virus through • STRIDOR
subglottic edema days
the nose Steeple Sign- A sign on the frontal
- onset detectable as early as 6 hours OTITIS MEDIA - Latin for "Inflammation of
↓spreads and eventually involves the larynx radiograph of tracheal narrowing and a
- continued improvement over 12- the Middle Ear"
and trachea suggestive for the DIAGNOSIS OF CROUP.
24hours Description
↓Inflammation and edema of the subglottic Risk Factors
PROGNOSIS (Expectations) • Otitis media is one of the most prevalent
larynx and trachea, especially near the o Allergies
• Viral croup usually goes away in 3 to diseases of early childhood.
cricoid cartilage o Repeated upper respiratory infections
7 days. The outlook for bacterial croup is • an infection of the middle ear, the area
↓Parainfluenzae virus activates chloride o Previous croup
good with prompt treatment. just behind the eardrum. It happens
secretion and inhibits sodium absorption Possible Complications
• If an airway obstruction is not treated when the eustachian tubes, which
across the tracheal epithelium, contributing o Pneumonia
promptly, respiratory distress (severe connect the middle ear to the nose,
to airway edema o Ear infection
difficulty breathing) and respiratory become blocked with fluid. With the
↓limiting airflow o Airway obstruction and death (rare) arrest can occur. infection, mucus, pus, and bacteria can
↓results in the barky cough, turbulent airflow Diagnosis Nursing Considerations also pool behind the eardrum, causing
and stridor, and chest retractions • Diagnosis is generally made on history and pressure and pain.
Signs and Symptoms physical examination.
• Major Objective: Maintaining the airway
• Physical examination may show chest
and providing adequate respiratory • Ear infections usually begin with a cold.
• Stridor- a harsh, raspy vibrating sound exchange Although adults can get ear infections,
heard when the child breathes in. This is retraction and wheezing using a
• Children with severe respiratory distress they are most common in infants and
usually present when the child is agitated stethoscope.
should not be given anything by mouth to young children. That's because a child's
but in severe cases may be present even • Diagnostic tests may include: prevent aspiration and decrease work of eustachian tubes are narrower and
at rest. Stridor occurs when the opening • Thoart Cultures breathing. shorter than an adults', and it's easier for
between the vocal cords becomes identify infecting organisms and their fluid to get trapped in the middle ear.
Maintain patent airway
narrower sensitivity to antibiotic when bacterial Etiology
Assess respiration rate
• Fever infection is the cause Streptococcos pneumoniae, Haemophilus
• Blood Cultures Monitor O2 saturation
• The child's condition may improve in the influenzae, and Moraxella catarrhalis are
morning but worsen at night. Elevate HOB and provide bed rest
Provide humidified o2 vial cool mist the three most common bacteria that
• Croup syndrome usually peaks 2 to 3 distinguish bacterial and viral infections causes AOM. The etiology of noninfectious
days after they start and the illness • X-ray of the neck tent for hospitalized child
OM is unknown, although OM may occur
generally last less than a week. may show upper airway narrowing and because of blocked eustachian tubes from
Progression of Symptoms edema in subglottic folds. the edema of URIs, allergic rhintis, or
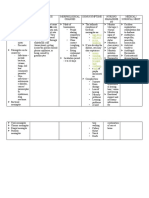
hypertrophic adenoids. Chronic OM is ↓Normal Eustachian tube is closed and cerumen prevents adequate • Second-line antibiotics used to treat OM
usually the extension of the Acute flat preventing organisms in the visualization.So remove the cerumen include amoxicillin-clavulanate,
episode. pharyngeal cavity from entering the first. azithromycin, and cephalosporins such as
Types Of Otitis middle ear. • Diagnosis of AOM is made if visual cefdinir, cefuroxime, and cefpodoxime.
• Otitis media acuta - Myringitis bullosa ↓The Eustachian tube opens to allow inspection of the tympanic IM ceftriaxone is used when the
• Otitis media chronica drainage of secretions produced by the membranereveals a purulent discolored causative organism is highly resistant
mesotympanalis - Influenza middle ear mucosa and to equalize air effusion and a bulging or full, opacified, pneumococcus.
• Acute otitis media is usually of rapid pressure between the middle ear and or very reddened immmobile membrane. • Ibuprofen, acetaminophen -- Ask the
onset and short duration. Acute otitis the outside environment. An immobile tympanic membrane or an doctor about using over the counter oral
media is typically associated with fluid ↓Blockage of the Eustachian tubes may orange discolored membrane indicates medications for pain and/or fever, such
accumulation in the middle ear together be caused by respiratory infection OME. as ibuprofen (Advil, Motrin) or
with signs or symptoms of ear infection; (cold), allergies, exposure to cigarette Surgical Management acetaminophen (Tylenol). Children under
a bulging eardrum usually accompanied smoke, infected or overgrown adenoids • Myringotomy – a surgical incision of the 18 should not take aspirin, due to the risk
by pain, or a perforated eardrum, often (tonsils),for infants, being fed lying eardrum may be necessary to alleviate of developing a rare but serious illness
with drainage of purulent material down (drinking a bottle while lying on the severe pain of AOM. A myringotomy called Reye's syndrome
(pus).Fever can be present. the back). is also performed to provide drainage of • Ear drops – If the child has recurring ear
• The most common bacterial agents for ↓Passive smoking increases the risk of infected middle ear fluid in the presence infections, a perforated eardrum, or
Acute Otitis Media are: persistent middle ear effusion by of complications (mastoiditis, develops infection after ear tubes have
• Streptococcus pneumoniae enhancing attachment of the pathogens labyrinthitis, or facial paralysis) or to been placed, the doctor may prescribe
that cause otitis to the respiratory allow purulent middle ear fluid to drain antibiotic ear drops instead of oral
• Haemophilus influenzae epithelium in the middle ear space, by into the ear canal for culture. antibiotics, to be used over a period of
• Chronic Otitis Media is a persistent prolonging the inflammatory response time (like a few months). If the child
inflammation of the middle ear, typically • Tympanostomy tubes – are tubes placed
and by impeding drainage through the for equalizing pressure or grommets that doesn't have ear tubes in place and
for a minimum of a month. Chronic otitis Eustachian tube. doesn't have any drainage from the ear,
media may develop after a prolonged facilitate continued drainage of fluid and
↓Impaired drainage of the Eustachian allow ventilation of the middle ear. the doctor may also prescribe anesthetic
period of time with fluid (effusion) or tube causes retention of secretions in ear drops to relieve pain.
negative pressure behind the eardrum • Adenoidectomy – removal of the
the middle ear. adenoids. Only performed in children Nursing Management
(tympanic membrane). Chronic otitis ↓Air is unable to escape through the • Don't expose the child to secondhand
media can cause ongoing damage to the with recurrent AOM or chronic OME with
obstructed tubes, is absorbed into the nasal obstruction. smoke.
middle ear and eardrum and there may circulation, and causes negative • Keep the child away from other children
be continuing drainage through a hole in Pharmacological Management
pressure within the middle ear. • Antibiotics -- If the doctor prescribes who are sick.
the eardrum. ↓Negative pressure pulls interstitial fluid • Always hold the infant in an upright,
• Chronic Otitis Media often starts antibiotics, be sure to give the child the
into the tube and creates a serous entire course. The antibiotic most often seated position during bottle feeding.
painlessly without fever. Ear pressure or effusion. This effusion of the middle ear • Breastfeeding for at least 6 months can
popping can be persistent for months. prescribed for an ear infection is
provides a fertile media for microbial amoxicillin, unless the child is allergic to make a child less prone to ear infections.
Sometimes a subtle loss of hearing can growth. If growth is rapid, a middle ear
be due to chronic otitis media. penicillin. If that's the case, there are • Don't use a pacifier while laying the baby
infection develops. several options. Children who are treated
Pathophysiology in a crib.
↓If the tube opens, a difference in with antibiotics are more likely to
Predisposing Factors • The pneumococcal vaccine (Prevnar)
pressure causes bacteria to be swept develop vomiting, diarrhea, or a rash.
• Age prevents infections such as pneumonia
into the middle ear chamber, where the
• Sex • If the etiology is known then drug is used and meningitis, and studies show it
organisms quickly proliferate and invade
• Race aimed against the bacteria. If drug is slightly reduces the risk of ear infections.
the mucosa.
• Siblings or Parents with a history of warranted, oral amoxicillin in high doses BRONCHIOLITIS
↓Complications include pain, fever, and
Chronic OM (80-90mg/kg/day) is the treatment of • swelling of the smallest air passages in
difficulty in hearing, otorrhea, tinnitus,
Precipitating Factors choice for initial episodes of AOM in the lungs (bronchioles), usually due to a
feeling of fullness and pulling of ear.
• URIs children who have not received viral infection (RSV)
Diagnostic Test
• Passive smoking antibiotics within the past month. • most common in infants between 2 and 6
• Pneumatic Otoscopy - assessment of
• Attending daycare Duration of antibiotic therapy is 10-14 months old
tympanic membrane mobility with a
• Using a pacifier days in children 6 years old and older, • Infection is spread by direct contact with
pneumatic otoscope is essential to
• Bottle feeding shorter courses may be sufficient. respiratory secretions
differentiate AOM from otitis media with
ear effusion (OME). If an accumulation of
• transmitted from person to person by • Tachypnea, greater than 70 Cortecosteroids- blocks release of children under the age of fifteen. Asthma in
direct contact with nasal fluids, or by breaths/min(most common physical inflammatory mediators children is a chronic illness that is caused by
airborne droplets. Although RSV sign) • Prednisone (Deltasone) a number of different triggers.
generally causes only mild symptoms in • Tachycardia • Methylprednisolone (Medrol, Solu- Asthma is a chronic disease that causes
an adult, it can cause severe illness in an • Fever, usually in the range of 38.5- Medro the airways to become sore and swollen. It
infant. 39°C • Ribavirin (Virazole)- has an antiviral is characterized by variable and recurring
PATHOPHYSIOLOGY • Nasal flaring activity against RSV by inhibiting the symptoms, airflow obstruction, and
• Risk factors: • Intercostal retractions synthesis of viral structural proteins, bronchospasm.
• younger than 6 months old • Wheezing but ribavirin aerosol treatment for RSV Types of asthma
• Never having been breast-fed • Cyanosis infection is highly controversial • Acute severe asthma
• Premature birth • Apnea ( may be the first recognized Nursing Management • Refractory asthma
• An underlying heart-lung condition indicator in very young infants) • Provide patent airway • Corticosteroid-Resistant asthma
• A depressed immune system • In severe cases,: hypercapnia leading • Position at 30-40 degrees angle with • Brittle asthma
• Exposure to tobacco smoke to respiratory acidosis and neck slightly extended • Aspirin-Sensitive asthma
• Contact with multiple children or hypoxemia • Monitor O2 stat CLASSIFICATION
crowded place DIAGNOSTIC TEST • Encourage adequate intake and assess Asthma is clinically classified according to
• Having siblings who attend school or • Enzyme-linked Immunosorbent Assay for dehydration the frequency of symptoms, forced
child care (ELISA)- technique used mainly in • If fluids by mouth is contraindicated expiratory volume in 1 second (FEV1),
• due to a viral infection of the small immunology to detect the presence of given IV fluids are preferred until acute and peak expiratory flow rate.
airways (Respiratory syncytial virus an antibody or an antigen in a sample crisis of the disease has passed
(RSV) • Immunflouresecent antibody (IFA) - • Plenty of rest
– Respiratory syncitial virus- is a technique used for light Prevention
considered the single most microscopy with a fluorescence • RSV immunoglobulin (RSV-IGIV)-
important respiratory pathogen microscope and is primarily used provides neutralizing antibodies
in infancy and early childhood, on biological samples. This against RSV
highly contagious technique uses the specificity – I V preparation given monthly
• Begins as a URI with symptoms of of antibodies to their antigen to – Have number of disadvantages that
rhinorrhea and low grade fever then target fluorescent dyes to have resulted in a decline in its use in
diseases progresses and becomes a specific bimolecular targets within favor of palivizumab.
respiratory tract infection a cell, and therefore allows • Palivizumab- monoclonal antibody It may also be classified as:
visualization of the distribution of – IM injection, monthly Atopic – extrinsic
• Infection of bronchiolar area and Non-atopic - intrinsic
ciliated epithelial cells produces the target molecule through the – does not interfere with immune
sample response to vaccines, and can be What causes asthma?
increased mucus secretion, cell death,
• Blood gases administered easily, without the need Things that cause asthma are called
and sloughing, followed by a
• Chest x-ray for hospital admission. triggers.
peribronchiolar lymphocytic infiltrate
• Patchy infiltrates • Handwashing Allergens - pollens, foods, dust, molds,
and submucosal edema.
• Air trapping feathers or animal dander
• The combination of debris and edema – Ensure that caregiver are not caring Irritants - dirt, cigarette smoke, gases and
produces critical narrowing and • Focal atelectasis other high risk patient
MANAGEMENTS air pollution
obstruction of small airways. – isolate infected patients or nurse in
Medical Management Odors - household cleaners, perfumes,
• During expiration, the additional cohorts based on laboratory
• Chest clapping as supportive therapy paints, varnishes, fabric softeners, laundry
dynamic narrowing produces confirmation of RSV stat
detergents and cooking fumes
disproportionate airflow • Mechanical ventilation as necessary – Family members with an upper
Irritants in the workplace - fumes and
• Trapping air in the alveoli that causes • Provide cool humidified oxygen respiratory infection should be
vapors from wood products and metals
hyperinflation that may lead to Pharmacologic Management especially careful around infants.
Metabisulfite - found in dried fruits, fruit
atelectasis Adrenergic agents- relieve reversible – use of gloves, aprons or gowns when in juices, beer, wine, salad bars and
• Inadequate gas exchange bronchospasm by relaxing smooth direct contact with the patient vegetables
• Patient experiences the following muscles on the bronchioles ASTHMA Respiratory infections - colds, flu, sore
symptoms: • Albuterol (Proventil, Ventolin, Asthma is the number one chronic illness throat and bronchitis
Salbutamol) among school aged children and is the third
• Epinephrine (Adrenalin) leading cause of hospital visits among
Exercise can trigger an early asthmatic An acute exacerbation of asthma is ≥20% decrease in peak flow following • Older, less selective adrenergic
response. commonly referred to as an asthma attack. exposure to a trigger (e.g., exercise). agonists, such as
Cardinal signs of asthma attack: Peak expiratory flow rate monitoring inhaled epinephrine and ephedrine table
Emotional stress - excessive fear or shortness of breath 1. Place the indicator on the apparatus ts, have also been used. In
excitement Wheezing emergencies, these drugs were
at the bottom of the numbered scale.
Weather conditions - very cold, windy chest tightness 2. Take a deep breath. sometimes administered by injection.
or sudden changes in the weather Signs of asthma in a baby or toddler 3. Place the meter in the mouth and • Anticholinergic medications, such
Medications - aspirin or related drugs, include: blows out as hard and as fast as as ipratropium bromide may be used
as well as some drugs used to • Noisy breathing or breathing possible. instead. They have no cardiac side
treat glaucoma and high blood increased 50 percent above normal 4. Repeat 2 or more times and record effects and thus can be used in patients
pressure • Wheezing or panting with normal the highest number achieved. with heart disease.
Pathophysiology activities “ZONES” – rate of expiratory Long term control
• Interrupted talking compliance Inhaled glucocorticoids are usually
• Pain or tight feeling in the chest considered preventive medications
• Green zone – 80%-100% of their personal
• Flaring of the nostrils when breathing while oral glucocorticoids are often
best; No asthma symptoms are present
in used to supplement treatment of a
• Hyperinflation (appearance of • Yellow zone – 50%-80% of their personal severe attack.
hunched shoulders, hunching forward best; An episode of asthma may be
beginning Long-acting β2-agonists (LABA) are
or preferring not to lie down) similar in structure to short-acting
• Lethargy, disinterest in normal or • Red zone – below 50%; Indicates an selective beta2-adrenoceptor agonists,
favorite activities asthma episode is beginning
but have much longer side chains
• Difficulty sucking or eating Medical Management
resulting in a 12-hour effect.
• Crying sounds softer, different Pharmacology
Prevention
Diagnosis Medications used to treat asthma are
The only preventive agent known is allergen
• Diagnosing asthma in very young divided into two general classes:
immunotherapy. Controller medications
children is difficult. • quick-relief medications used
include the following:
• To help the pediatrician make a correct to treat acute symptoms
Inhaled glucocorticoids such
diagnosis, parents must provide • long-term control
as beclomethasone normally come as
information about family history of medications
inhalers. Deposition of steroids in the
asthma or allergies, the child's overall Babies or toddlers can use most
mouth may result in oral thrush.
behavior, breathing patterns and medications used for older children and
Deposition near the vocal cords can
responses to foods or possible allergy adults. The dosage is lower.
cause hoarse voice. (rinse mouth after
triggers. Medications to treat asthma symptoms in
inhaler use or by using a spacer)
• Lung function tests - often used to make infants and toddlers are usually given in a
a definitive asthma diagnosis. tasty liquid form or with a nebulizer. Leukotriene modifiers such
• Blood tests, allergy testing and x-rays Fast acting as montelukast provide both anti-
may be done to gather additional Short-acting - selective beta2-adrenoceptor spasm and anti-inflammatory effects.
Physical assessment
information. agonists, Mast cell stabilizers such as
Difficulty of breathing
• The basic measurement is peak flow salbutamol (albuterol USAN), levalbuterol, ter (cromoglicate (cromolyn),
Wheezing
rates and the following diagnostic butaline, ventolin and bitolterol and nedocromil). These medications
Decreased O2Sat reading • Tremors, the major side effect, have
criteria: are believed to prevent the initiation of
Hyperresonant upon percussion been greatly reduced by inhaled the allergy reaction, by stabilizing the
≥20% difference on at least three
Expiration phase is longer than delivery. There may also be cardiac side mast cell.
days in a week for at least two weeks;
inspiration effects at higher doses (due to Beta-1
≥20% improvement of peak flow Methylxanthines
Cyanosis may be present agonist activity), such as elevated heart
following treatment, for example: (theophylline and aminophylline).
Pt is on sitting position rate or blood pressure. These agents are bronchodilators with
10 minutes of inhaled β-agonist
Shield-like or barrel-shaped chest • However, levalbuterol has been minimal anti-inflammatory effect.
(e.g., salbutamol);
Clubbing of fingers shown to have fewer cardiac side effects
six weeks of inhaled corticosteroid Antihistamines are often used to treat
Growth restriction and significantly more anti-inflammatory
(e.g., beclometasone) the nasal allergies which can
Signs and Symptoms effects on bronchial smooth muscle.
accompany asthma.
14 days of 30 mg prednisolone.
Asthmatic patients should avoid the Death may occur because of respiratory Clubbing of fingers in older child. Favored preparation is pancrelipase.
triggers as part of their preventive infection and failure. Hyperglycemia, glucosuria with polyuria, Occasionally, antacid is helpful to
measures. Other complications include esophageal and weight loss. improve tolerance of enzymes.
• Concentrate on the bedroom, where varices, diabetes, chronic sinusitis, Sterility in males. Favorable response to enzymes is
very young children spend as much pancreatitis, rectal polyps, Diagnostic Evaluation: based on tolerance of fatty foods,
as 12-18 hours each day. intussusceptions, growth retardation, Sweat chloride test measures sodium decreased stool frequency, absence of
• Cover the pillows, mattress and box and infertility. and chloride level in sweat. steatorrhea, improved appetite, and
springs in allergen-proof casings. OTHER NAMES Chloride level of more than 60 mEq/L is lack of abdominal pain.
• Wash bed linens weekly in 130- CF virtually diagnostic. Gene therapy, in which recombinant
degree water. Use washable area Cystic fibrosis of the pancreas Chloride level of 40 to 60 mEq/L is DNA containing a corrected gene
carpets. Fibrocystic disease of the pancreas borderline and should be repeated. sequence is introduced into the
• Buy only washable stuffed animals. Mucoviscidosis diseased lung tissue by nebulization, is
Duodenal secretions: low trypsin
• Vacuum weekly or more. Don't allow in clinical trials.
Mucoviscidosis of the pancreas concentration is virtually diagnostic.
pets in the bedroom/house. Nursing Interventions:
Pancreas fibrocystic disease Stool analysis:
• Restrict smoking in the house (even Monitor weight at least weekly to assess
if someone smokes in the basement Pancreatic cystic fibrosis Reduced trypsin and chymotrypsin
PATHOPHYSIOLOGY levels-used for initial screening for effectiveness of nutritional
of a multi-storied house, smoke interventions.
filters through the vents to all parts A defective gene that leads to the cystic fibrosis.
making of an abnormal protein. Increased stool fat concentration. Monitor respiratory status and sputum
of the house). production, to evaluate response to
Can a child “out-grow” asthma? àCFTR (cystic fibrosis transmembrane BMC ( Boehringer-Mannheim Corp.)
respiratory care measures.
Approximately 50 percent of children with regulator) meconium strip test for stool includes
lactose and protein content; used for To promote airway clearance, employ
asthma appear to outgrow asthma when they Abnormal movement of sodium and
screening. intermittent aerosol therapy three to
reach adolescence. Once someone develops chloride in the body's cells.
four times per day when the child is
sensitive airways, they remain that way for Leads to thicker secretions Chest X-ray may be normal initially; symptomatic.
life, although asthma symptoms can vary Exocrine glands become obstructed later shows increased areas of infection,
Perform chest physical therapy three to
through the years. As a child's airways Appear histologically abnormal and over inflation, bronchial thickening and
four times per day after aerosol therapy.
mature, they are able to handle airway produce excessive secretions plugging, atelectasis, and fibrosis.
inflammation and irritants better, so their Suction the infant or young child when
(tracheobronchial and Brunner's Pulmonary function studies (after age 4)
asthma symptoms may notably decrease. necessary, if not able to cough.
glands) show decreased vital capacity and flow
About half of those children find their asthma Teach the child breathing exercises
Appear histologically normal but rates
symptoms reappear in varying degrees when using pursed lips to increase duration of
secrete excessive Na and Cl (sweat, Diagnosis is made when a positive
they reach their late thirties or early forties. exhalation.
parotid, and small salivary glands) sweat test is seen
Status Asthmaticus Provide good skin care and position
Assessment: Genetic screening may be done for
- Children who continue to display changes to prevent skin breakdown in
Usually present before age 6 months affected families.
respiratory problems despite vigorous malnourished child.
but severity varies and may present Pharmacologic Interventions:
therapeutic measures. Provide frequent mouth care to reduce
later. Antimicrobial therapy as indicated for
- May develop gradually or rapidly or chances of infection because mucus is
Meconium ileus is found in neonate. pulmonary infection.
with complications such as pneumonia present.
usually present with respiratory Oral or I.V. antibiotics as required.
- Is a medical emergency that can result Restrict contact with people with
in respiratory failure and death if symptoms, chronic cough, and Inhaled antibiotics, such as gentamicin respiratory infection.
untreated. wheezing. or tobramycin, may be used for severe
Encourage diet composed of foods high
CYSTIC FIBROSIS - is an autosomal Parents may report salty taste when lung disease or colonization of
in calories and protein and moderate to
recessive disorder affecting the exocrine skin is kissed. organisms.
high in fat because absorption of food is
glands, in which their secretions become Recurrent pulmonary infections. Bronchodilators to increase airway size incomplete.
abnormally viscous and liable to obstruct Failure to gain weight or grow in the and assist in mucus clearance.
Administer fat-soluble vitamins, as
glandular ducts. presence of a good appetite. Pulmozyme recombinant human DNase prescribed, to counteract
It primarily affects pulmonary and GI Frequent, bulky, and foul smelling stools (an enzyme) administered via malabsorption.
function. (steatorrhea) nebulization to decrease viscosity of
Provide opportunities for parents to
The average life expectancy for the Protuberant abdomen, pot belly secretions.
learn all aspects of care for the child.
cystic fibrosis patient is currently age 30 Bleeding disorders Pancreatic enzyme supplements with
to 40. each feeding.
Teach the parents about dietary Contraindications: If vomiting occurs, keep the child on
regimen and special need for calories, Cleft palate NPO status for 30 mins. and then
fat, and vitamins. o Tonsils help prevent air escape resume clear liquids.
Discuss need for salt replacement, during speech Use acetaminophen for pain relief.
especially on hot summer days or when Acute infection at the time of Do not use aspirin or any medicine
fever, vomiting, and diarrhea occur. surgery containing aspirin.
Increase salt intake during hot weather, Pre-Operative Care: An ice collar can be applied for
fever, or excessive exercise to prevent Take a complete history with special comfort.
sodium depletion and cardiovascular attention given to allergy symptoms, Avoid giving milk and milk products. CLEFT LIP/PALATE
compromise. difficulty swallowing, or airway Discourage the child from coughing, • are facial malformations that occur
TONSILS obstruction. clearing the throat or gargling. during embryonic development and are
Overview: Assess the child for any signs of the most common congenital deformity
Encourage abundant liquid intake.
Masses of lymphoid tissue located in active infection and redness and of the head and neck
Avoid citrus juices for 10 days.
the pharyngeal cavity. exudate of the throat. Avoid red liquids, which will give the • may appear separately or together
Function: Review laboratory results appearance of blood if the child WHAT’S THEIR DIFFERENCE?
Filter and protect the respiratory and ( Prothrombin time, PTT, platelet vomits. CLEFT LIP
alimentary tracts from invasion by count, Hgb, Hct). - results from failure of the maxillary and
Add full liquids on the second day
pathogenic organisms and play a role Check the child for loose teeth to median nasal processes to fuse
and soft foods as the child tolerates
in antibody formation. decrease the risk for aspiration (bet. 5&8wks of IU life)
them.
TONSILLECTOMY during the surgery. CLEFT PALATE
Avoid rough or scratchy foods - is a midline fissure of the palate that
Surgical removal of one or both Explain the need for surgery in a (bacon, chips, popcorn), citrus foods results from the failure of the 2 slides to
tonsils, usually through a sharp wire simple and nonthreatening manner. or spicy foods for 3 weeks. fuse
loop, scalpel, or electrocauterization. Have a calming and reassurig Before discharge, instruct the (9-12wks of IU life)
Performed under general anesthesia attitude to ease the child’s anxiety. parents to:
either as an outpatient or with CLEFTS….
Let the child have a visit to the Encourage the child to chew and
overnight observation. • CL may vary from small notch to a
surgical facility/hospital several days swallow. complete cleft; deformed dental
Surgery takes 30-45 minutes in advance. Not to give the child any straws, structures
Children remain at the hospital 2-4 Reassures the child that talking will forks or sharp pointed toys that could • CP occurs in midline and may involve soft
hours after outpatient surgery or not be a problem after surgery. be put in the mouth. & hard palate
overnight for observation. Instruct the patient to have nothing Call the physician for any bleeding, • When associated, may involve the
Indications: by mouth for 6 hours prior to the persistent earache, or fever greater midline & extend into the soft & hard
Recurrent attacks of tonsillitis time of surgery. than 101 F (38.8 C). palates
More than 7 times a year for one Post – Operative Care: Child may return to school when • UNILATERAL OR BILATERAL
year Assess the child for any excessive directed by the physician, usually in
More than 5 times a year for 2 swallowing, elevated pulse, about 10 days.
years decreasing blood pressure, signs of Bring the child for a follow-up
More than 3 times a year for 3 fresh bleeding in the back of the appointment in 1-2 weeks.
years throat and restlessness that does not
Peritonsillar abscess seem to be associated with the pain
In children – done 4-6 weeks which are an indicator of
after resolution of a peritonsillar postoperative bleeding.
abscess Place the child in a prone or side-
In adults – done after the second lying position.
attack of peritonsillar abscess If bleeding occurs, turned the child to
Enlarged tonsil causing obstructive the side and then notify the
symptoms physician.
Difficulty in respiration Provide clear, cool liquids when the
Difficulty in swallowing child is fully awake.
ITS OCCURRENCE….
Difficulty in speaking • CL/P is more common the CP
• 60%-80% are male – Avoid oral thermometers ↓Contraction and relaxation is absent in demonstrate absence of fecal
• Females have a higher isolated clefts of – Elbow restraints the intestine material in the long segment disease;
the 20 palate – No straws, pacifiers, spoon or fork in and ↓Lack of enervation produces the in short segment disease, rectal
• 86% in palatal; 68% unilateral CL assoc. around the mouth for 7-10days functional defect that results in the impaction may be present and, when
w/ palatal – Place infants in side-lying position absence of propulsive movements the finger is removed, it may cause a
DIAGNOSTIC TESTS: – Stay in place while feeding (peristalsis) rush of stool as the obstruction is
• Thorough assessment of the mouth – Provide comfort to prevent crying ↓No peristaltic waves that move fecal temporary relieved
• Prenatal: soft tissues of the face is – Clean the suture lines w/ sterile H20 or material throughout Abdominal x-ray
visualized until 13-14wks saline q after feeding ↓Stool accumulates with the distention of severe gaseous distention of the
• CL/P assoc with other structural – Elbows may be restrained until palate is the bowel proximal to the defect bowel, with absence of gas in the
anomalies : 100% healed (4-6wks) (megacolon) rectum; this may indicate a bowel
• CL/P: 50% with CP – Teach parents to remove restraints q ↓The internal sphincter fails to relax blockage
WHAT ARE THE CAUSES? 2hrs because the ganglion segment is missing this study only allows physicians to
• Hereditary – Oral packing secured to the palate the inhibitory neurotransmitter, nitric suspect the diagnosis, not
• Environmental (removed after 2-3d) oxide definitively diagnose it
• Teratogenic (phenytoin, smoking) – Opiods may be given ↓The result is an obstruction because the Barium Enema
PATHOPHYSIOLOGY – Acetaminophen evacuation of stool, gas, and liquid is Barium, a chalky liquid, is inserted
Risk Factors: – Clear liquids then blenderized or soft diet prevented through the anus into the colon, and
Modifiable: teratogens and environment – Long term: good mouth care ↓Intestinal distention and ischemia may coats the inside of the colon. When
Non-modifiable: environment Proper brushing defects also occur as a result of distention of the an x-ray of the abdomen is taken,
↓Genetic defects in cell migration HIRSCHSPRUNG DISEASE bowel wall this part lights up. If hirschsprung
↓If tongue( separates the lip &palate) fails - also known as congenital aganglionic ↓This contributes to the development of disease is present, a “transition
to descend megacolon enterocolitis (inflammation of the small zone” may be apparent. In the
↓Delay in merging of the upper lip @ the - mechanical obstruction caused by bowel and colon) segment without nerve cells, the
midline (bet. 7th&11th wk IUL) inadequate motility of part of the Clinical Manifestations colon will appear to be of normal size
↓Delay in fusion of hard& soft palate (bet. intestine Newborn period: anorexia, poor or somewhat constricted. In the area
7th&12th wk IUL - congenital absence of or arrested feeding above, however, the colon will
↓Failure of the maxillary & premaxillary development of parasympathetic Infancy appear dilated. The stool that cannot
processes to come together bet. 3rd&12th ganglion cells in the intestinal wall, o failure to thrive be passed backs up and the colon is
wk of IUL usually in the distal colon o constipation stretched and enlarged. Visualizing
↓Palate /lip never fuses - four times more common in males than o abdominal distention the funnel-like transition zone is a
↓Cleft lip/palate in females o episodes of diarrhea and clue that the individual may have
MEDICAL & SURGICAL MNGT. - usually isolated birth defect but has been hirschsprung disease.
vomiting (including bile)
• Surgical Correction: CL associated with other syndromes This is the most valuable radiologic
o signs of enterocolitis
– Cheiloplasty (lip surgery) including Down Syndrome study for establishing the diagnosis.
o explosive, watery diarrhea
(done @1-2mos) PATHOPHYSIOLOGY Rectal Biopsy
o fever -definitive diagnosis of hirschsprung
– Tennison-Randall triangular flap During normal development, neuroblasts o appears significantly ill disease
– Millard rotational advancement tech will be found in the small intestine by the
Childhood (symptoms may appear -Involves removing a small piece of
• Surgical Correction: CP 7th week of gestation and will reach the
more chronic) tissue from the rectum. Doctor
– Palatoplasty (done 6-18mos) colon by the 12th week
o constipation examine the tissue sample under a
NURSING MNGT. ↓In hirschsprung disease, there is a defect
in the migration of these neuroblasts o stool appears ribbon like, fluid microscope and look for the presence
• Pre-op:
down their path to the distal intestine like, or in pellet form of ganglion cells (nerve cells). If no
– Feed infant in upright position, slowly &
↓Causes an abnormal migration of the o abdominal distention nerve cells are visualized,
burp frequently
precursor ganglion cells o visible peristalsis Hirschsprung disease is diagnosed.
– Use ESSR; (1) enlarged nipple
↓These ganglia control both the o easily palpable fecal mass In infants, a suction rectal biopsy can
(2)stimulate sucking reflex (3)swallow
contraction and relaxation of smooth o undernourished anemic be done at the bedside. Since there
fluid appropriately (4)rest when infant
muscles in the intestine appearance are no sensory nerves at the site of
signals w/ facial expression
↓There’s an impaired colonization of DiagnosticTests biopsy, this is not painful. When a
– Using special or modified nipples suction biopsy is inconclusive,
• Post-op: ganglion cells in the distal portion of the Rectal examination
GI tract resulting in aganglionosis surgical biopsy is performed under
general anesthesia in the operating - Key points are that a retrorectal Enterocolitis -Most serious complication of 6. Suction oral secretions frequently to
room. approach is used and a significant Hirschsprung disease. prevent infection of the tracheobronchial
Anorectal monometry portion of aganglionic rectum is Emergency preooperative care: tree and lungs.
this determines whether normal retained 1. Monitor V/S and blood pressure for 7. In older child, encourage frequent
reflexes involving the rectum and the - The aganglionic bowel is resected signs of shock coughing and deep breathing to maintain
anus are present. Used only in older down to the rectum, and the rectum 2. Monitor fluid and electrolyte respiratory status.
children, the test can be performed is oversewn. The proximal bowel is replacements, as well as plasma or other 8. Allow the infant to cry for a short period
at the bedside. then brought through the retrorectal blood derivatives to prevent atelectasis.
Ultrasonogram space and an end-to-side 3. Observing for symptoms of bowel 9. Change position of infant frequently to
may be done to demonstrate dilated anastomosis is performed on the perforation such as fever, increasing increase circulation and allow for aeration
colon remaining rectum abdominal distention, vomiting, of all lung areas.
Therapeutic Interventions increased tenderness, irritability, 10. Maintain patency of NG tube
• Enema or colonic irrigation with • Soave (endorectal) procedure dyspnea and cyanosis. immediately postoperatively.
physiologic saline solution. - was introduced in 1960’s and – Because, progressive distention of the 11. Maintain NPO status until bowel sounds
• Older child whose symptoms are chronic consist of removing the mucosa and abdomen is a serious sign, the nurse return and the bowel is ready for feedings
but not severe may be treated with submucosa of the rectum and pulling measures the abdominal circumference as determined by the physician.
isotonic enemas, stool softeners, and a the ganglionic bowel through the with a paper tape measure, usually at 12. Provide frequent oral hygiene while on
low residue diet. aganglionic muscular cuff of the the level of the umbilicus or the widest NPO status.
Surgical Interventions rectum. part of the abdomen. 13. Administer fluids to maintain hydration
- the original operation did not Possible Complications: and replace lost electrolytes. Begin oral
• Initially, a colostomy or ileostomy is include a formal anastomosis, relying • Inflammation and infection of the feedings as ordered.
performed to decompress intestine, on scar tissue formation between the intestines may occur before surgery, and 14. Support the parents when teaching
divert fecal stream, and rest the normal pull-through segment and the sometimes during the first 1-2 years them to care for their child’s colostomy.
bowel. Created proximal to the surrounding aganglionic bowel. The afterwards. Symptoms are severe, Reassure parents that colostomy will not
aganglionic segment to relieve procedure has since been modified including swelling of the abdomen, foul- cause delay in the child’s normal
obstruction and allow the normally by Boley to include a primary smelling watery diarrhea,lethargy and development.
enervated and dilated bowel to return to anastomosis of the anus. poor feeding. 15. Involve the entire family in
its normal size PRE-OPERATIVE CARE • Perforation or rupture of the intestine teaching colostomy care to enhance
• Definitive surgery is done to remove the 1. Assist in emptying the bowel by giving • Short bowel syndrome acceptance of body change of the child.
non-functioning bowel segment with repeated enemas and colonic irrigations. POSTOPERATIVE CARE Assess stoma:
various pull-through procedures 2. If abdominal distention is not relieved by 1. Change wound dressing using sterile • Red in color (fully blood vessels)
(abdominoperineal, endorectal, or enemas, discomfort is significant, and technique. • Moist (with mucous membranes
rectorectal). rectal tube insertion fails to give relief, 2. Prevent wound contamination from for lubrication)
• Complete corrective surgery is performed consult doctor for a nasogastric (NG) tube. diaper. • May bleed ( numerous large
usually when the child weighs 3. Offer pacifier for infant to suck if on To prevent contamination of the vessels)
approximately 9 kilograms (20 pounds) parenteral fluids. abdominal wound with urine in the
• The various surgical procedures that can 4. Encourage parents to hold and rock the infant, the diaper should be pinned INTUSSUSCEPTION
be performed are the Swenson, infant. below the dressing. Sometimes, a Foley -a condition in which one part of the
Duhamel, Boley, and Soave procedures 5. Maintain position of comfort with head catheter is used in the immediate intestine becomes pushed into the lumen
• Swenson Procedure elevated. Offer soothing stimulation (eg. postoperative period to divert the flow of an adjoining segment
– the original pull-through procedure music, touch, play therapy). of urine away from the abdomen. -invagination of one portion of the
used to treat Hirschsprung disease 6. Offer small frequent feedings. Low 3. Prevent perianal and anal excoriation by intestine into another
– the aganglionic segment is resected residue diet will aid in keeping the stool thorough cleaning and use of ointments INTUSSUSCEPTUM -the telescoping
down to the sigmoid colon and the soft. after the infant soils (postoperative stools PROXIMAL portion of the bowel
remaining rectum, and an oblique 7. Administer parenteral nutrition if feeding can number 7 to 10 per day). INTUSSUSCIPENS -the adjacent DISTAL
anastamosis is performed between causes additional discomfort because of 4. Use careful handwashing technique. bowel
the normal colon and low rectum. distention and nausea. 5. Report any wound redness, swelling or Medical Management
• Duhamel procedure 8. For older child, provide demonstration drainage, evisceration, or dehiscence • Initial treatment of choice: NONSURGICAL
- was first described in 1956 as a and written and verbal instruction to family immediately. HYDROSTATIC REDUCTION
modification to the Swenson for saline enema administration and use of
procedure stool softeners.
• BARIUM ENEMA-diagnostic and Surgical Management o More prevalent in women than in men • Diarrhea
therapeutic -if enema was unsuccessful o More common among Caucasians • Abdominal pain
Contraindicated: Perforation -pts who show signs of shock or peritonitis o It may occur in adults but usually affects • Distended abdomen/protuberant
• Water-soluble Contrast and Air -symptoms presented longer than 24 hrs children, bet. ages 9 & 18 mos. abdomen
Pressure/Enema -manually reducing the invagination o primarily a childhood disorder • Steatorrhea
• Carbon Dioxide Pressure -LAPAROTOMY – for multiple recurrences o More common among relatives, • Pale, foul-smelling bowel stools
-resection of any nonviable intestine especially siblings • Mm wasting, weakness
Nursing Management • Athralgia/Bone pain
– LISTEN to the parents’ description of the • Easy bruising, Bleeding problems
child’s physical and behavioral symptoms Etiology • Anemia, Smooth, red tongue
– Explain to the parents the need for Exact cause: Unknown • Hypoprothrombinemia
immediate hospitalization. Offer Genetic • Hypomagnesemia & Hypocalcemia
emotional support: parents are S/Sx
Immunologic factors
unprepared - Irritability
Pathophysiology
– Observe/ monitor stools - normal BROWN - Tremor
stool indicates that the intussusception - Convulsions
has reduced itself - Tetany
– Monitor v/s. Infants may become - Bone pain
hypothermic at the onset of infection; - Osteomalacia
↑Temp: sepsis, ↑PR and dec BP: - Dental abnormalities
peritonitis • Dermatitis herpetiformis
Post-procedural care: Diagnostic Exam
– Monitor v/s Intestinal biopsy
– Check for the return of the bowel sounds - confirmative test
– Monitor pt who has undergone - Serology
hydrostatic reduction for passage of - detect antibodies to connective
stools and barium or water-soluble tissue (endomysium & reticulin) &
contrast material gliadin
Pre-operative care: Antireticulin Antibodies (ARA),IgA & IgG
– Maintain NPO status as ordered Antiendomysial Antibodies (EMA), IgA &
– Routine laboratoy testing (CBC and UA) IgG
– PARENTAL CONSENT Antigliadin antibodies (AGA), IgA & IgG
– Preanesthetic sedation The autoantibodies of IgA antireticulin
• SONOGRAM-preferred means of Post-operative care: & antiendomysial IgA are more specific
diagnosis – Monitor V/S markers for active celiac dse. than
• IV fluids, NGT decompression, Antibiotic – Check dressings and the return of bowel circulating IgA antigliadin antibodies,
therapy may be used sounds. Provide meticulous wound care. w/c may be present in other dses. &
– Preserve the parent-child relationship by conditions.
encouraging rooming-in or extended Anti-tissue Transglutaminase Antibody
visiting (tTG), IgA
– Parents’ reactions must be understood - a more specific test recognized by
and accepted antiendomysial antibody
CELIAC DISEASE - tissue transglutaminase is an enzyme
o “Celiac sprue”, “Gluten-induced/sensitive responsible for linking certain
enteropathy” proteins. It has been identified as the
o permanent intestinal intolerance to antigen that the body responds to
gluten *The major pathophysiologic char. of the when it creates Anti-EMA antibodies.
o malabsorption syndrome dse. are atrophy of villi in the upper small Gliadin a peptide derivative of gluten,
o 2nd to cystic fibrosis as a cause of intestine & malabsorption of nutrients. triggers the dev’t. of tTG
malabsorption in children Clinical Manifestation autoantibodies. Although “tssue” is in
the name of this autiantibody, it ordered. If pt. can tolerate iron, give it poisoning; stimulates vomiting in the Induce emesis (NSG! No charcoal if
nevertheless involves testing blood bet. meals, when absorption is best. brain giving antidote)
NOT tissue. Provide a gluten-free diet. Contraindication of Ipecac or no emetic Gastric lavage
Treatment Assess the pt.’s acceptance & induction if: N-acetylcysteine(mucomyst): antidote for
- Lifelong elimination of gluten understanding of the dse. & encourage comatose victim, in shock, convulsing tylenol poisoning
What is gluten? pt. to participate in a local Celiac dse. or has lost gag reflex -alters metabolism & decreases liver
- the protein component of cereal grains. support group. corrosive ingestion damage
- each type of protein is slightly different Six (6) key elements: NSG -> side-lying, sitting or kneeling -S/E: bad taste and smell->NSG dilute in
from the others. Gliadin in wheat, position with head below the chest to avoid juice/soda
hordein in barley, secalin in rye, avenin
C onsultation with a skilled dietitian
aspiration -A/E: watch for bronchospasm
in oats, zein in corn & oryzenin in rice. E ducation about the disease Ipecac dose: ASPIRIN POISONING
- It is important to note that the gluten L ifelong adherence to gluten-free 15 ml – adolescent, school age and S/sx:
found in corn & rice does not cause harm diet pre-school; repeat dosage once if
to those w/ Celiac dse.
Metabolic acidosis -> lung stimulation ->
I dentification & tx of nutritional vomiting does not occur within 20 blows off excess C02 ->tachypnea-
- Gluten-containing foods: “BROW” deficiencies minutes Kussmaul respirations(initial response)
• B arley 10 ml – infant; do not repeat
A ccess to an advocacy group Hypoglycemia, thirst
Administer with 200-300 cc warm water
• R ye C ontinuous long-term ff-up by a Universal antidote: 1.) activated Loss of fluids/electrolytes – dec Na+, K+
• O ats multidisciplinary team charcoal 2.) milk of magnesia 3.) GI irritation
• W heat POISONING burned toast Bleeding -> monitor? Bleeding time
Poison – either ingested, inhaled or Remember: most frequently accidentally ingested by
Gluten-free foods: corn, potatoes, rice, absorbed in the body injures the body by toddlers
soybean flour Never administer the charcoal before
its chemical action ipecac
Gluten-free diet: ↑-calorie, ↑-protein, acute ingestion: 300-500 mg/kg->severe
Goals: Tracheostomy set should always be at TOXICITY
↓-carbohydrate,↓-fat 1. to remove poison before absorbed bed side chronic ingestion: >100 mg/kg per day x
Avoid foods containing “vegetable protein” 2. to provided supportive care (i.e. vital
Kerosene/Gasoline poisoning: give 2days or more
- In some children, who have more severe organs)
mineral oil requires treatment: 1.5 to 5 grains per
mucosal damage, disaccharide digestion 3. to administer antidotes to neutralize
the poison Caustic poisoning (muriatic acid): give pound
is impaired, esp. LACTOSE. Therefore,
4. to implement treatment that hastens vinegar(low % acidity), don’t induce Medical Management/Treatment
LACTOSE-FREE DIET is recommended,
elimination of absorbed poison emesis, prepare tracheostomy set, Induce emesis-syrup of Ipecac/lavage
w/c necessitates elimination all milk
Common accident in infants – falls lavage ->cuffed endotracheal tube with activated charcoal (important in
products.
Common accident in toddlers – poisoning TYLENOL POISONING - Causes liver early toxicity)(if not in
Supplemental Tx include: Vit. D, Iron,
PRINCIPLES damage: cell damage, liver dysfunction, liver coma/convulsing)!!!
Vit.B12, Folic acid failure Cathartics to speed through GI tract
Nursing interventions: Determine the substance taken and
PHASES of tylenol poisoning Possible dialysis (if unresponsive)
Observe pt.’s nutritional status & assess LOC
Initial phase(>150mg/kg-TOXIC; 2-4 Fluids->DHN
progree by daily calorie counts & wt. Unless poisoning was corrosive,
hours after ingestion) - n/v, pallor, Assisted ventilation, PRN
checks. caustic(strong alkali such as lye) or
malaise, vomiting, sweating
Assess fluid status: record intake, urine hydrocarbon = vomiting (most Seizure precautions
effective) Latent phase(24-36 hours) - feel
output, & # of stools. Watch for signs Administer as ordered: IVF, NaHCO3,
relatively well, may recover
of DHN, i.e., dry skin & mucous Strong acid or alkali poisoning electrolytes, volume expander,
(corrosive type) Hepatic involvement(may last up to 7
membranes & poor skin turgor. glucose, Vita K, anticonvulsants, O2
- dilute with water or milk (120cc [4 days & be permanent) - RUQ pain,
Check serum electrolyte levels. Watch Prognosis
ounces]) jaundice, confusion, stupor,
for signs of hypokalemia (weakness, with prompt treatment: GOOD
- do not induce vomiting/do not coagulation abdnormalities, hepatic
lethargy, rapid pulse, & diarrhea), & if with seizures: POOR
neutralize failure, coma, death
low Ca levels (mm twitching & tetany). LEAD TOXICITY
- airway management(priority) - Monitor for? liver enzymes
Monitor PT & Hgb & Hct. Protect pt. - Patients who do not die in hepatic stage Sources: pain, varnish, battery, crayons,
from bleeding & bruising. Administer - e.g. lye, acid pencil, smoke-belching vehicles via
gradually recover
Vit.K, iron,folic acid, & Vit.B12 as Syrup of Ipecac – oral antiemetic to ingestion or inhalation
Medical Management
cause vomiting after drug overdose or Assessment
beginning symptoms of lethargy -6 doses/day for 7 days: therapy: never as
impulsiveness and learning difficulty single-agent therapy; with EDTA
as lead increases, severe Succimer(Chemet)-19-day tx; may be with
encephalopathy with seizures and food/whole
permanent MR ] All meds S/E: nephrotoxicity
NSG ->force fluids, chelates are excreted
Risk Factors: via kidneys
• Poverty Monitor for? Creatinine levels, BUN
• Age less than 6 years old Prognosis:
• Dwelling in the city Massive amounts: encephalopathy,
What happens in lead toxicity? seizures, coma,possible death
pencil, paint, crayon(lead) ->interferes iron Smaller amounts: risk for neurologic
binding onto heme molecule->destruction impairment
of RBC functioning (releases erythrocyte
protoporphyrin -> hypochromic, microcytic
anemia ->lead competes with Ca ->
destroys bones, teeth & kidneys
->accumulation of NH->destroys
endothelial cells in the brain -> crosses the
blood-brain barrier
->encephalopathy
Diagnostic tests
Blood smear: >20mcg/dL: acute
poisoning
Erythrocyte protoporphyrin test N:
<35mcg/100ml blood
Abdominal x-ray
Long bones
Medical management
Remove child from source
If >20mcg/dL: needs chelation therapy
– removes lead from body by binding
with lead & excreted via kidneys
If >45mcg/dL, CaNa2EDTA/EDTA and
Succimer are used
If >70mcg/dL, British Anti-Lewisite is
used with EDTA
MEDS:
Calcium disodium
edetate(CaNa2EDTA/EDTA) po: for
>20mcg/dL lead in blood -helps excrete
in urine 20-50 times the normal rate
-inject procaine with drug/site rotation
-give DEEP IM or IV
!!! MIO, U/A ->nsg: maintain OIF
Dimercaprol(BAL ‘British Anti-Lewisite
Calcium’ in peanut oil)
NSG -> do not give if allergic to peanuts;
DEEP IM
Vous aimerez peut-être aussi
- CD 1Document5 pagesCD 1Iriah Mara100% (1)
- Pedia Rotation CroupDocument2 pagesPedia Rotation CroupKaren ArandiaPas encore d'évaluation
- Internal Medicine Table SummaryDocument31 pagesInternal Medicine Table SummaryShazaan Nadeem100% (1)
- ARIs CME2Document50 pagesARIs CME2JunaidahMubarakAliPas encore d'évaluation
- Q3 HEALTH 8 WK1 LESSON 1 Disease Prevention and Control CommunicableDocument35 pagesQ3 HEALTH 8 WK1 LESSON 1 Disease Prevention and Control CommunicableJaeda EuclidPas encore d'évaluation
- MS 1 Chap 22Document9 pagesMS 1 Chap 22Louise Lorraine TaculodPas encore d'évaluation
- Comparative - URT and PneumoniaDocument4 pagesComparative - URT and Pneumoniange257Pas encore d'évaluation
- Geron-Ppt - 20231206 131738 0000Document29 pagesGeron-Ppt - 20231206 131738 0000Potato TomatoPas encore d'évaluation
- Diphtheria: Sabah Mohsin Al-Maamuri MDDocument3 pagesDiphtheria: Sabah Mohsin Al-Maamuri MDAmmar AlnajjarPas encore d'évaluation
- NCM 118 Medsurg EndtermDocument25 pagesNCM 118 Medsurg EndtermJmarie Brillantes PopiocoPas encore d'évaluation
- Respiratory Emergency and DiseasesDocument5 pagesRespiratory Emergency and DiseaseshanhananicasPas encore d'évaluation
- Cause Agent Type of Agent MOT Signs and Symptoms Prevention and Control Treatment TuberculosisDocument6 pagesCause Agent Type of Agent MOT Signs and Symptoms Prevention and Control Treatment Tuberculosisvanessa patayonPas encore d'évaluation
- Airway Emergencies: ORL PostingDocument58 pagesAirway Emergencies: ORL PostingKimberlyLaw95Pas encore d'évaluation
- Nursing Care of Clients With Upper Airway or Respiratory DisordersDocument6 pagesNursing Care of Clients With Upper Airway or Respiratory DisordersVinzii DrtPas encore d'évaluation
- PICORNAVIRIDAEDocument3 pagesPICORNAVIRIDAEjcpacate1178qcPas encore d'évaluation
- Diseases of The Respiratory SystemDocument9 pagesDiseases of The Respiratory Systemmaryannfrancisco16Pas encore d'évaluation
- Fiji's EpiDocument13 pagesFiji's Epipofegeg809Pas encore d'évaluation
- Pneumonia CBLDocument22 pagesPneumonia CBLImAlien OrGodPas encore d'évaluation
- Internal Medicine Table PDFDocument31 pagesInternal Medicine Table PDFShazaan NadeemPas encore d'évaluation
- DiphtheriaDocument3 pagesDiphtheriakpkr603Pas encore d'évaluation
- Infectious Dieseases Acute Respiratory Infection: Shingles / Herpes ZosterDocument12 pagesInfectious Dieseases Acute Respiratory Infection: Shingles / Herpes ZosterIverson CaparosoPas encore d'évaluation
- Com +Nursing+Care+Plan+Chicken+PoxDocument2 pagesCom +Nursing+Care+Plan+Chicken+PoxDahl Obañana Erojo100% (1)
- Nursingcrib Com NURSING CARE PLAN Chicken Pox PDFDocument2 pagesNursingcrib Com NURSING CARE PLAN Chicken Pox PDFAkeroPas encore d'évaluation
- NURSING CARE PLAN Chicken PoxDocument2 pagesNURSING CARE PLAN Chicken Poxderic87% (62)
- Diphtheria ReportDocument13 pagesDiphtheria ReportAubrey SungaPas encore d'évaluation
- 5 2-DeanDocument7 pages5 2-Deanfiel borataPas encore d'évaluation
- RabiesDocument4 pagesRabiesJamie FabianiaPas encore d'évaluation
- 7.chest and Lower Respiratory Tract DisordersDocument8 pages7.chest and Lower Respiratory Tract Disorders2BGrp3Plaza, Anna MaePas encore d'évaluation
- Finals LecDocument14 pagesFinals LecSheena Patricia ArasulaPas encore d'évaluation
- NCM116 CDN Respiratory LECDocument14 pagesNCM116 CDN Respiratory LECMilcah NuylesPas encore d'évaluation
- Aplikasi Dan Penyakit Pada Sistem PernapasanDocument22 pagesAplikasi Dan Penyakit Pada Sistem PernapasanRakha PradipaPas encore d'évaluation
- CARIDocument3 pagesCARIFirenze FilPas encore d'évaluation
- Actinomycosis and NOMADocument10 pagesActinomycosis and NOMASOUMYA A DR, DEPT.OF DENTAL SCIENCES,SRIHERPas encore d'évaluation
- ENT (Supposedly) 2.4 RhinitidisDocument6 pagesENT (Supposedly) 2.4 RhinitidisDaniel Yakin Eliamar AritonangPas encore d'évaluation
- Cough & ColdsDocument26 pagesCough & ColdsMarcelle DrukerPas encore d'évaluation
- UntitledDocument6 pagesUntitledFritz Angelo BullonPas encore d'évaluation
- Nursing Care of Clients With Upper Airway or Respiratory DisordersDocument6 pagesNursing Care of Clients With Upper Airway or Respiratory DisordersLuna MariePas encore d'évaluation
- Lower Respiratory Tract Diseases - KeyDocument45 pagesLower Respiratory Tract Diseases - KeyYugmaPandyaPas encore d'évaluation
- Dr. Dr. Shahrul Rahman, SP - PD, FINASIMDocument46 pagesDr. Dr. Shahrul Rahman, SP - PD, FINASIMatikaPas encore d'évaluation
- R A B I E S: Dave Jay S. Manriquez RNDocument15 pagesR A B I E S: Dave Jay S. Manriquez RNOdylon CayetanoPas encore d'évaluation
- LaryngitisDocument24 pagesLaryngitisfatihahannisahumaira100% (1)
- Rabies: S.Hudiyono Nursing Division Health Politechnic SemarangDocument10 pagesRabies: S.Hudiyono Nursing Division Health Politechnic SemarangZifa ArdilafPas encore d'évaluation
- Ch. 31 StudyDocument8 pagesCh. 31 StudyPaige Nicole GauthreauxPas encore d'évaluation
- NCM 109Document18 pagesNCM 109Grace Jane HannaPas encore d'évaluation
- Patient Care Pathogen Reservoir Mode of Transmission: Viral Infections of HumansDocument21 pagesPatient Care Pathogen Reservoir Mode of Transmission: Viral Infections of HumansMark Vincent JanoyogPas encore d'évaluation
- 7 Infections of Pharynx, Parapharyngeal Space & RetropharyngealDocument11 pages7 Infections of Pharynx, Parapharyngeal Space & Retropharyngealyq24w9p85sPas encore d'évaluation
- Respiratory Disorders in PediatricsDocument11 pagesRespiratory Disorders in PediatricsMateo Geoff100% (1)
- 8 Clostridial InfectionsDocument39 pages8 Clostridial InfectionsHariharanPas encore d'évaluation
- Week 13 NCMB 312 Lect NotesDocument18 pagesWeek 13 NCMB 312 Lect NotesAngie BaylonPas encore d'évaluation
- High Fever Stiff Neck Severe HeadacheDocument3 pagesHigh Fever Stiff Neck Severe HeadacheDiana Jane LauretaPas encore d'évaluation
- Lec4 TransDocument23 pagesLec4 TransErika PatarayPas encore d'évaluation
- Nursing CS CroupDocument1 pageNursing CS Croupreuben kadarajaPas encore d'évaluation
- Stridor in ChildrenDocument7 pagesStridor in Childrenp4b5Pas encore d'évaluation
- Respiratory SystemDocument69 pagesRespiratory SystemVanitas CartePas encore d'évaluation
- Pneumonia Case PresentationDocument1 pagePneumonia Case PresentationFrancine kimberlyPas encore d'évaluation
- Rabies ScribdDocument78 pagesRabies Scribdbryfar100% (1)
- The Epi Target DiseasesDocument7 pagesThe Epi Target DiseasesElizabeth Ivory ChuaPas encore d'évaluation
- URTIDocument41 pagesURTIGetaneh LiknawPas encore d'évaluation
- Literature Review LichenDocument7 pagesLiterature Review LichenNur Fazrina CGPas encore d'évaluation
- Simple Linear Equations A Through HDocument20 pagesSimple Linear Equations A Through HFresgPas encore d'évaluation
- Sample File: A of TheDocument6 pagesSample File: A of TheMegan KennedyPas encore d'évaluation
- Customer AnalysisDocument6 pagesCustomer AnalysisLina LambotPas encore d'évaluation
- Baccarat StrategyDocument7 pagesBaccarat StrategyRenz Mervin Rivera100% (3)
- CNS Drugs Pharmaceutical Form Therapeutic Group: 6mg, 8mgDocument7 pagesCNS Drugs Pharmaceutical Form Therapeutic Group: 6mg, 8mgCha GabrielPas encore d'évaluation
- Abstraction and Empathy - ReviewDocument7 pagesAbstraction and Empathy - ReviewXXXXPas encore d'évaluation
- A Management and Leadership TheoriesDocument43 pagesA Management and Leadership TheoriesKrezielDulosEscobarPas encore d'évaluation
- TreeAgePro 2013 ManualDocument588 pagesTreeAgePro 2013 ManualChristian CifuentesPas encore d'évaluation
- Partnership & Corporation: 2 SEMESTER 2020-2021Document13 pagesPartnership & Corporation: 2 SEMESTER 2020-2021Erika BucaoPas encore d'évaluation
- Hardy-WeinbergEquilibriumSept2012 002 PDFDocument6 pagesHardy-WeinbergEquilibriumSept2012 002 PDFGuntur FaturachmanPas encore d'évaluation
- CRM Project (Oyo)Document16 pagesCRM Project (Oyo)Meenakshi AgrawalPas encore d'évaluation
- Chargezoom Achieves PCI-DSS ComplianceDocument2 pagesChargezoom Achieves PCI-DSS CompliancePR.comPas encore d'évaluation
- MC2 Sewing Patterns: Dressmaking Learning ModuleDocument91 pagesMC2 Sewing Patterns: Dressmaking Learning ModuleMargie JariñoPas encore d'évaluation
- NURS 406 Concept Map HyperparathyroidismDocument1 pageNURS 406 Concept Map HyperparathyroidismshyannPas encore d'évaluation
- Disciplines, Intersections and The Future of Communication Research. Journal of Communication 58 603-614iplineDocument12 pagesDisciplines, Intersections and The Future of Communication Research. Journal of Communication 58 603-614iplineErez CohenPas encore d'évaluation
- Presentation (AJ)Document28 pagesPresentation (AJ)ronaldPas encore d'évaluation
- Finding Roots of Equations Bracketing MethodsDocument11 pagesFinding Roots of Equations Bracketing MethodsmebrahtenPas encore d'évaluation
- The Distracted Mind - ExcerptDocument15 pagesThe Distracted Mind - Excerptwamu885Pas encore d'évaluation
- Chem31.1 Experiment 2Document28 pagesChem31.1 Experiment 2Mia FernandezPas encore d'évaluation
- Total Recall and SkepticismDocument4 pagesTotal Recall and Skepticismdweiss99Pas encore d'évaluation
- Complexity. Written Language Is Relatively More Complex Than Spoken Language. ..Document3 pagesComplexity. Written Language Is Relatively More Complex Than Spoken Language. ..Toddler Channel TVPas encore d'évaluation
- Project Report On Amazon vs. FlipkartDocument86 pagesProject Report On Amazon vs. FlipkartDimple100% (3)
- Hanssen, Eirik.Document17 pagesHanssen, Eirik.crazijoePas encore d'évaluation
- Thailand Day 2Document51 pagesThailand Day 2Edsel BuletinPas encore d'évaluation
- PPG ReviewerDocument8 pagesPPG Reviewerryanbaldoria.immensity.ictPas encore d'évaluation
- Introduction To Professional School Counseling Advocacy Leadership and Intervention Ebook PDF VersionDocument62 pagesIntroduction To Professional School Counseling Advocacy Leadership and Intervention Ebook PDF Versionmary.krueger918100% (50)
- DLL Template MathDocument3 pagesDLL Template MathVash Mc GregorPas encore d'évaluation
- CB Insights Venture Report 2021Document273 pagesCB Insights Venture Report 2021vulture212Pas encore d'évaluation