Académique Documents
Professionnel Documents
Culture Documents
45 PDF
Transféré par
Nur Mutmainnah RahmanTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
45 PDF
Transféré par
Nur Mutmainnah RahmanDroits d'auteur :
Formats disponibles
International Journal of Health Sciences and Research
www.ijhsr.org ISSN: 2249-9571
Review Article
The Increasing Burden of Uncontrolled Hypertension in Nigeria: The Role of
Lifestyle Modification Practices as an Effective Strategy to Reverse the Trend
Iyalomhe GBS1, Iyalomhe SI 2
1
Associate Professor & Head, Department of Pharmacology and Therapeutics, College of Medicine,
Ambrose Alli University, Ekpoma, Nigeria
2
Head, Department of Public Health and Primary Health Care, Central Hospital, Auchi, Nigeria
Corresponding Author: Iyalomhe GBS
Received: 17/11/2014 Revised: 10/12/2014 Accepted: 12/12/2014
ABSTRACT
Background: Globally, uncontrolled hypertension is a serious prevalent risk factor for cardiovascular and
renal diseases. The current approach to the control of hypertension and its complications includes drug
treatment of hypertensive patients and implementation of adequate lifestyle modifications (LMs) which
are beneficial for non-hypertensive and hypertensive individuals. Practices of LMs are abysmally low in
Nigeria.
Aim: This review aims to provide healthcare professionals with useful clinical information to guide their
patient care promote the understanding of LMs and motivate hypertensive patients and the public to adopt
and maintain multiple LMs.
Methodology: Manual literature and computer programmes (Cochrane Library, EMBASE, OVID, Pub
Med, HINARI, Goggle Scholar etc) were searched for relevant information.
Results/Discussion: The search showed that LM practices such as regular physical activity/exercises,
weight loss by the overweight or obese, reduced salt and increase potassium (K +) intake, adoption of the
Dietary Approaches to Stop Hypertension (DASH) diet (that emphasizes consumption of fruits,
vegetables, low-fat dairy products, reduced saturated fat and cholesterol), moderation in alcohol intake
and cessation of smoking, have significant beneficial effects on blood pressure (BP). High religiosity or
spirituality promotes cardiovascular health possibly by its preventive or prohibitive influence on lifestyle
risk factors such as smoking and excessive alcohol drinking.
Conclusion: The current challenge to healthcare providers and the public is evolvement and
implementation of effective clinical and public health strategies that lead to sustained LM practices. There
is urgent need to intensify LM education and counseling to both hypertensive patients and the public,
particularly in Nigeria.
Key words: Uncontrolled hypertension, Lifestyle modification, Strategy for controlling hypertension,
Nigeria.
INTRODUCTION a third of deaths worldwide with about 80%
Cardiovascular diseases (CVDs), of these deaths happening in low and middle
mostly heart disease and stroke, account for income countries.1 The biggest risk factor in
International Journal of Health Sciences & Research (www.ijhsr.org) 309
Vol.5; Issue: 1; January 2015
CVD is hypertension, as it is directly of healthcare resources use and the total
responsible for 62% of strokes and 49% of annual medical expenditure attributed to
heart disease. [1,2] The International Forum hypertension including comorbidities are
for Hypertension Control and Prevention in estimated to range from USD 108-110
Africa suggested that strategies that modify billion. [13,14] The adverse effects such as
the risk factor for hypertension, such as dizziness, headache, fatigue, chest
promoting healthy diets, weight reduction, discomfort, cough, sexual dysfunction,
reducing salt intake, smoking cessation and caused by some antihypertensive drugs, may
moderation in alcohol intake and engaging prompt some patients to discontinue therapy,
in physical exercises, could lower the predisposing them to the danger of
prevalence of high blood pressure and cardiovascular events. But LMs are cheap
subsequently reduce the burden of CVD. [3] and have virtually no side effect. [15-17]
This combination of strategies is also In view of the above considerations, national
recommended in the guidelines on and international policy-making bodies
hypertension by the various Hypertension recommend LM practices as a means to
Writing Groups such as the World Health prevent and treat hypertension and thereby
Organization (WHO)/International Society prevent cardiovascular and renal disease in
of Hypertension (ISH). [4] European Society the whole population. [1-8,10,18]
of Hypertension (ESH)/European Society of
Cardiology (ESC) [5] and the US 8th Joint THE BURDEN OF UNCONTROLLED
National Committee for the Prevention, HYPERTENSION IN NIGERIA
Detection, Evaluation and Treatment of In Nigeria, hypertension is a serious
High Blood Pressure. [6] Aside from other major public health and clinical problem that
risk factors such as tobacco use, causes disability and death among the adult
undernutrition, unsafe water and unsafe sex, population as well as playing an important
hypertension is reported to rank highest as a role in the causation of heart failure, heart
preventable cause of death in both attack, stroke, renal failure, and arterio-
developed as well as in developing countries sclerosis in the population. [19,20] Indeed, it
such as Nigeria where hypertension and has been reported that the incidence of
urbanization have been close companions. hypertension is rising in Nigeria. [21-26] A
[1,5,7,8]
nation-wide survey [27] in 1992 showed that
It has long been recognized that drug 11.2% of adults were hypertensive but
treatment alone is an incomplete solution to recent studies done in different parts of the
the epidemic of high BP. [1-69-11] It is known country have shown prevalence rates that
that the risk of BP-related cardiovascular ranged from 28.8% to 36.6% [22,24-26] This
and renal disease increases progressively increasing burden of hypertension is
throughout the range of BP, including stretching medical facilities in Nigeria and
ranges of BP previously considered normal this is shown by increase rate of in-patient
but now called prehypertension. Although hospital admissions for strokes and heart
the number of patients with hypertension disease. [28-30] Therefore, there is a need for
and prehypertension continues to rise and population-wide strategies to prevent
affects a large portion of the population, hypertension in Nigeria before it becomes an
recognition and adequate treatment are unmanageable epidemic. [31]
grossly inadequate. [12] Recent surveys in Nigeria reveal
The cost of drug treatment of continuing deficiencies in the knowledge,
hypertension represents a significant amount perception, prevention and control of
International Journal of Health Sciences & Research (www.ijhsr.org) 310
Vol.5; Issue: 1; January 2015
hypertension. In most cases, failure to highly motivated individuals who are
achieve BP control was attributed to the consistent with LM practices. [35] In non-
poverty of patients’ knowledge and lack of hypertensives, LMs have the potential to
or inadequate practice of LMs. [21,28,29,32,33] prevent hypertension, and more broadly to
The result is that excess morbidity and reduce BP and its complications in whole
premature mortality from severe (including prehypertensive) population.
hypertension have remained high among Indeed, even an apparently small reduction
Nigerian patients. [34,35] Worse still, the in BP, if applied to an entire population,
coexistence of hypertension and diabetes in could have an enormous beneficial effect on
this group dramatically and synergistically cardiovascular events. For instance, a 3
increases the risk of microvascular and mmHg reduction in systolic BP should lead
macrovascular complications, a worrisome to an 80% reduction in stroke mortality and
condition associated with widespread a 5% reduction in mortality from coronary
disability, excess mortality, reduced capacity heart disease. [9,12]
for work and disruption of social/family life It is remarkable that hypertension,
among the indigenous people. [36-38] the key driver of cardiovascular
Thus hypertension has become a big complications, is mainly associated with
burden in Nigeria, a country experiencing environmental and lifestyle factors rather
the epidemiological transition from than with genetics and has a stronger
communicable to non-communicable association and causal link with the
diseases, a phenomenon referred to as a following modifiable (reversible) risk
double burden of disease. Rural-to-urban factors that can reduce BP if properly
migration coupled with acculturation and utilized. [9,12,35]
modernization has become the trend that is Regular physical activity/exercise
strongly linked with changes in individual Adequate physical activity including
and societal lifestyles such as an increase in regular aerobic (isotonic) exercises such as
tobacco use, excessive alcohol consumption, brisk walking, dancing, swimming, jogging
reduced physical activity and adoption of 30-45 minutes 3-4 days a week, has been
western diets that are high in salt, refined shown to have health promoting benefits and
sugar and unhealthy fats and oils. [32,35] has a direct, independent role in reducing
BP. Hence, even in elderly people, tolerance
THE ROLE OF LIFESTYLE exercise is advised. [35,39-41]
MODIFICATIONS (LMs) AS AN Hitherto, it was thought that a high
EFFECTIVE STRATEGY TO REDUCE level of physical activity could in part
HYPERTENSION explain the low level of chronic disease
LMs, previously referred to as non- found in most of Africa. However, the
pharmacological therapy, have important amount of physical activity has decreased as
roles in hypertensive and non-hypertensive a result of a high rate of urbanization.
individuals. In hypertensive individuals, Adequate physical activity is more prevalent
LMs can serve as initial treatment before the in rural than urban areas of Nigeria, which
commencement of antihypertensive therapy partly explains the high prevalence of
[15,21,35-38]
and as an adjunct to medications in persons obesity in urban areas.
already on drug therapy. [11,12] In Government and stakeholders should
hypertensive individuals with medication- motivate and mobilize the citizenry to
controlled BP, these therapies can facilitate engage in useful physical activities.
drug step-down and drug withdrawal in
International Journal of Health Sciences & Research (www.ijhsr.org) 311
Vol.5; Issue: 1; January 2015
Maintaining a healthy body weight consuming large amounts of salt, such as
Observational studies and virtually Nigeria, [33] could be aborted in the very
every clinical trial, that have examined the beginning by a low-salt diet. [59] Above data
effect of weight loss on BP, have have reinforced current guidelines to limit
documented that weight reduction in the salt intake to 6g per day, the equivalent of
overweight or obese lowers BP. [42-45] 100 mmol of Na+ (2400 mg) per day.
Interestingly, reductions in BP occur before Results from the DASH Na+ feeding study
[52]
(and without) attainment of desirable body have documented that an even lower
weight. Since the mean weight of intake of Na+, approximately 60 mmol/day,
populations is not stable but has increased in further reduces BP in a broad population of
recent years world-wide, lifestyle non-hypertensive and hypertensive
intervention trials have uniformly achieved individuals.
short term weight loss (that is, the efficacy Low salt intake not only reduces BP
of weight control interventions is lost with and its related CVD risk, but also has
time). [5] However, in several instances, additional benefits such as direct effect on
substantial weight loss has been sustained reducing stroke, left ventricular hypertrophy,
for over 3 years. [43,44,46] aortic stiffness as well as chronic kidney
Reducing dietary table salt (sodium (Na+) disease and proteinuria. [9,35,51] Salt reduction
chloride) intake in the diet (low salt in cooking and no
A high intake of salt has adverse additional salt at table) at the population-
effect on BP. Evidence includes results from wide level as a means of reducing the
animal [47] and epidemiologic [48,49] studies burden of hypertension in Nigeria could be
as well as clinical trials. [50-52] These studies one of the best buy strategies due to its
demonstrate that hypertension can be attractive low cost of implementation.
[32,35,60,61]
induced in both salt-sensitive animals and
humans by high dietary salt load. Salt (Na+) Increasing potassium (K+) intake
sensitivity is the hallmark of hypertension in In various human populations (and
the majority of blacks, the obese as well as animals too), high BP is correlated more
the elderly and they respond very well to closely with low K+ intake than with high
Na+ restriction and to diuretics/natriuretic Na+ intake and hypertensive patients have
agents. [17,34,36,52-56] been found to have lower plasma and total
Essential hypertension is seen body K+ as well as lower urine K+ excretion
primarily in societies with average Na+ levels. [53,54,56] Potassium supplementation or
intake above 100 mmol/day (2.3g Na+). high K+ diet including fresh fruits like
[50,57]
These observations suggest that the bananas, oranges, apples and vegetables (the
development of hypertension requires a preferred strategy to increase K+ intake
threshold level of Na+ intake and this effect because this is accompanied by a variety of
appears to be independent of other risk other nutrients), has been demonstrated to
factors for hypertension eg obesity. lower BP (more in hypertensives than
Reducing Na+ intake to 100 mmol/day has normotensives), potentiate the effects of
been reported to lower the mean BP in diuretics and lessen renal K+ wasting. [62]
normotensive adults by approximately 2/1 However, a subsequent report of a
mmHg and in hypertensive adults by 5/3 systematic review of available meta-
mmHg. [58] It has therefore been suggested analyses and randomized controlled trials
that the inexorable and deleterious natural found no statistically significant effect of K+
history of BP rising with aging in societies supplementation on BP excluding one trial
International Journal of Health Sciences & Research (www.ijhsr.org) 312
Vol.5; Issue: 1; January 2015
in an African population with very high were striking, i.e., 11.4 and 5.5 mmHg.
baseline BP that resulted in small overall Similar to the meta-analysis of K+, the
reductions in BP. [63] DASH diet reduced BP to a greater extent in
Other dietary factors that might influence blacks than non-blacks. [74]
BP: Calcium (Ca2+), Magnesium (Mg2+), Moderation in alcohol intake (among
Zinc (Zn2+), high protein intake, DASH- drinkers)
diet Consumption of alcohol is
Hypertension is more common in the increasingly becoming more frequent in
presence of hypercalcaemia and there is Africa including Nigeria. [7,35] The effects of
direct positive relationship between total heavy [75] and even moderate [76,77] drinking
serum Ca2+ and BP. [64] Ca2+ supplements leading to increased BP has been reported in
may lower the blood pressure in those who Nigeria and elsewhere, respectively. Trials
have lower serum Ca2+ [65] and high have also reported that reductions in alcohol
parathyroid hormone level but with the intake can lower BP in normotensive and
potential risk of causing kidney stones. [66] hypertensive men who are heavy drinkers.
Increase in Na+ may increase BP, whereas [78,79]
Evidence supports a recommendation
the reverse is for K+ and Mg2+, hence dietary to limit alcohol intake to < 1drink per day
measures to reduce BP have been reported for women and < 2 drinks per day for men,
to be more effective when intake of several in the absence of binge drinking. One drink
minerals is affected simultaneously. [67] This is defined as 12 oz of regular beer, 5 oz of
is because the cations (Na+, K+, Mg2+, Ca2+) wine (12% alcohol), and 1.5 oz of 80-proof
functionally act in concert. [68,69] Mg2+ spirit, all equivalent to about 15g alcohol.
[80]
deficiency is associated with significant The plausible beneficial effects of this
[70]
hypertension and oral Mg2+ level of alcohol consumption include
supplementation has been reported to reduction in platelet aggregation and
prevent and lower BP. [71] Reducing Na+ thrombotic markers such as fibrinogen,
intake together with increasing Ca+ and increases in HDL cholesterol (about 80%)
Mg2+ intake are important in the prevention [81]
and anti-inflammatory effects such as
and treatment of hypertension. [67] The US lowering C- reactive protein levels. [82]
National Health and Examination Nutrition However, amounts in or near this level have
Survey (NHANES ΙΙ 1976-1980) found an been associated with an increased risk for
inverse relationship between serum Zn2+ hypertension, [76,77] although it is said that
level and BP. [72] this may be due to heavy drinkers who under
Epidemiological studies strongly report their intake. [77,83] Again, this
support the hypothesis that increased protein beneficial effects of moderate alcohol
intake can lower BP. [73] The most effective drinking are not evident in South Asians, [84]
diet, now termed the DASH diet, [9] Indian men [85] and American blacks. [86]
emphasizes fruits, vegetables, and low-fat Thus, according to Naimi and
dietary products; includes whole grains, colleagues, [87] alcohol is not a good
poultry, fish and nuts; and is reduced in fat, candidate as a population-based
red meat, sweets, and sugar-containing hypertension prevention strategy especially
beverages. The diet is rich in K+, Mg2+, and when one considers the special concerns
Ca2+. Among non-hypertensive individuals, about addiction, cost of alcoholism on
this diet reduced systolic and diastolic BP by family life, drunk driving, treatment of liver
3.5 and 2.1 mmHg, respectively. In disease, atrial fibrillation, stroke,
hypertensives, corresponding BP reductions cardiomyopathy, cancer and dementia.
International Journal of Health Sciences & Research (www.ijhsr.org) 313
Vol.5; Issue: 1; January 2015
Hence the current advice of the American religious behaviour such as its prohibitive
Heart Association in relation to alcohol and influence on smoking or alcoholism. [94,95]
prevention of hypertension and other The above is true of many religious groups
cardiovascular diseases is “If you drink in Nigeria and it should be encouraged
alcohol, do so in moderation. If you don’t because it is an effective strategy for
drink,don’tstart.” [80] Interventions to limit controlling these deleterious risk factors for
alcohol use should be introduced in a multi- hypertension. [24,28]
sectoral manner and adapted to the local
situation. Such interventions, like the ones CONCLUSION
utilized for reducing tobacco use, can also Although each LM practice has a
be applicable eg increasing taxes on alcohol, modest effect, the combined (comprehensive
and banning alcohol advertising especially LM) effects, particularly the ones involving
to young people. [88] DASH-diet, exercise and weight loss, can be
Cessation of cigarette smoking substantial. From a public health
Among its many negative effects, perspective, even a small reduction in BP
smoking increases BP and the harms should have a significant beneficial effect on
associated with hypertension by damaging the occurrence in prehypertension/
blood vessels and hardening arteries hypertension and their complications. Given
(atherosclerosis), which can lead to impaired the current high prevalence of BP-related
organ function and blood clots. [89,90] diseases and the established salutary effects
Moreover, as a group, smokers tend to have of LMs on BP, public health policies should
more behavioural risk factors than do non- be focussed on reducing the risk factors of
smokers, including poorer diet, less frequent hypertension. This can be done by
exercises, and higher alcohol consumption, developing and implementing hypertension
which also put them at greater risk for control programmes just like the concerted
developing more severe forms of efforts of the Federal, State and the Local
hypertension. [91] Smoking cessation is Governments that attended the eradication
known to reduce the overall risk of of guinea worm, poliomyelitis and the recent
cardiovascular diseases. [92] In order to ebola virus disease infections in the country.
reduce smoking at the population level, it is Government at all levels should put in place
important to implement multi-sectoral effective monitoring and surveillance
interventions like increasing taxes on programmes in order to track progress in
tobacco products, banning of tobacco reducing the prevalence of hypertension and
advertisements and banning smoking in its control.
public places. [88] There should be a strong focus on
High religiosity or spirituality development and improvement in the health
The concept that religious behaviour, service delivery system to address the
religiosity or spirituality, was associated control of hypertension and its
with longevity was observed in the 1990s, complications. This can be done through
when mortality was found to be lower community based screening programmes
among frequent church-goers than among and strengthening primary health care
non-attenders. [93] One proposed mechanism system to manage simple cases of
for improving mortality among healthy, hypertension but also establishing a strong
religious individuals is reduced referral link to General Hospitals and
cardiovascular risk, possibly related to tertiary health facilities to ensure continuity
lifestyle or other cardioprotective effects of of care. Antihypertensives should be made
International Journal of Health Sciences & Research (www.ijhsr.org) 314
Vol.5; Issue: 1; January 2015
free or highly subsidized and available. 8. WHO. Health statistics information
There should be continued training and systems. The Global Burden of Disease
retraining of medical and allied health staff and injury country estimates (internet).
as well as developing and implementing 2011; Available from:
National standard guidelines for treatment http://www.who.int/healthinfo/global_b
urden_disease/estimates_country/en/ind
and management of hypertension to ensure ex.htm [accessed 11/08/2014].
consistent quality care of hypertensive 9. Appel LJ. Lifestyle modification as a
patients. There is urgent need to intensify means to prevent and treat high blood
LM education and counseling to both pressure. J Am Soc Nephrol. 2003; 14:
hypertensive patients and the public, 599-5102.
particularly in Nigeria. 10. Glynn LG, Murphy AW, Schroeder K,
Fahey TC. Interventions used to
REFERENCES improve control of blood pressure in
1. WHO Global Health Observatory patients with hypertension, Cochrane
(2013). Raised blood pressure: situations Data Base of System Rev, Issue 3 Art
and trends [online).Gxed August 6, No CDOO5182. 2013; DOI:
2014] Available at 0.1002114651858. CDOO5182.pub4.
URL:http://www.who.int/gho/ncd/riskfa 11. Iyalomhe GBS. A review of the current
ctors/bloodpressureprevalencetext/en. trends in the treatment of hypertension. J
2. WHO. Preventing chronic disease, a Appl Bas Sc 2005; 3(1&2):5-9.
vital investment. 2005; Geneva. 12. Li J, Zheng H, Du H, Tian X, Jiang y,
3. Lemogun D, Seedat YK, Mabadeje AF, Zang S et al. The multiple lifestyle
Mendis S, Bovet P, Onwubere B et al. modifications for patients with
Recommendations for prevention, prehypertension and hypertension: a
diagnosis and management of systematic review protocol. BMJ Open.
hypertension and cardiovascular risk 2014: 4: e004920. DOI:
factors in Sub-Saharan Africa, J 10.1136/bmjopen-2014-004920.
Hypertens. 2003; 21: 1993-2000. 13. Balu S, Thomas J III. Incremental
4. Witworth JA et al for the WHO/ISH expenditure of treating hypertension in
Writing Group. WHO/ISH statement on the United States. Am J Hypertens.
management of hypertension. J 2006; 19:810-816.
Hypertens. 2003; 21(ii): 1983-1992. 14. Hodgson TA, Cai L. Medical care
5. Mancia G, Fagard R, Narkiewicz et al. expenditures for hypertension, its
Practice guidelines for the management complications and its comorbidities.
of arterial hypertensive of the ESH/ESC. Med Care. 2001; 39:599-615.
J Hypertens. 2013; 31:1925-1938. 15. Iyalomhe GBS, Omogbai EKI, Isah AO,
6. James PA, Oparil S, Carter BL et al for Iyalomhe OOB, Dada FL, Iyalomhe SI,
the panel members appointed to the US Efficacy of initiating therapy with
8th JNC for the Prevention. Detection, amlodipine and hydrochlorothiazide or
Evaluation and Treatment of High their combination in hypertensive
Blood Pressure. 2014 evidence-based Nigerians. Clin Exper Hypertens Early
guidelines for the management of high online 1-8 2013; DOI:
blood pressure in adults. JAMA. 2014; 10.3109/10641963.776570.
311 (5):507-520. 16. Iyalomhe GBS, Compliance to
7. Ezzati M, et al. Selected major risk antihypertensive therapy. Nig Clin Rev
factors and global and regional burden J. 2007; 63: 12-16.
of disease. Lancet. 2002; 17. Iyalomhe GBS, Current trends in
360(9343):1347-1360. diuretic therapy of hypertension. Nig
Clin Rev J. 2007; 61: 25 – 29.
International Journal of Health Sciences & Research (www.ijhsr.org) 315
Vol.5; Issue: 1; January 2015
18. Federal Ministry of Health, Nigeria. 28. Iloh GUP, Ofoedu JN, Njoku PU,
Standard Treatment Guidelines. Abuja, Amadi AN, Godswill-UKo EU.
Federal Ministry of Health, Nigeria, Medication adherence and blood
2008. pressure control amongst adults with
19. Ayodele OE, Alebiosu CO, Salako BL, primary hypertension attending a
Awoden OG, Adigun A. Target organ tertiary primary care clinic in Eastern
damage and associated clinical Nigeria. Afr J Prim Health Care Fam
conditions among Nigerians with treated Med. 2013; 5:446-501.
hypertension. Cardiovasc J South Afr. 29. Katibi IA, Olarinoye JK, Kuranga SA.
2005; 16: 89-93. Knowledge and practice of hypertensive
20. Arodiwe EB, Ike SO, Nweokediuto SC. patients as seen in a tertiary hospital in
Case fatality among hypertension- the middle belt of Nigeria. Nig J Clin
related admissions in Enugu, Nigeria. Pract. 2010; 13:159-162.
Nig J Clin Pract. 2009; 12:153-156. 30. Ekwunife OL, Aguwa CN, Adibe MO,
21. Akinkugbe OO. Current epidemiology Barikpoar E, Onwuka C. Health state
of hypertension in Nigeria. Arch. Ibadan utilities of a population of Nigerian
Med. 2003; 1:3-5. hypertensive patients. BMC Res Notes.
22. Adedoyin RA, et al. Prevalence and 2011; 4:528. DOI:
pattern of hypertension in a semi-urban 10.1186/1756-05000-4-528.
community in Nigeria. Eur J Cardiovasc 31. Kuller LH. Epidemic hypertension in
Prev Rehab. 2008; 15(6):638-687. Sub-Saharan Africa. Hypertens. 2007;
23. Ike SO. Prevalence of hypertension and 50(6): 1004-1005.
its complications among medical 32. Iyalomhe GBS, Iyalomhe SI.
admissions at the University of Nigeria Hypertension-related knowledge,
Teaching Hospital, Enugu (study 2). Nig attitudes and life-style practices among
J Med. 2009; 18(1):68-72. hypertensive patients in a sub-urban
24. Isezuo SA, Sabir AA, Ohwovoriole AE, Nigerian community. J Pub Health
Fasanmade OA. Prevalence, associated Epidemiol. 2010; 2(4):71-77.
factors and relationship between 33. Amadi AN, Okafor GOC, Ikwudinma
prehypertension and hypertension: a AO, Odu FU, Godswill-Ukoh EU.
study of two ethnic African populations Adherence to lifestyle modifications
in Northern Nigeria. J Hum Hypertens. among adult hypertensive Nigerians
2010: Jun 17. [Epub ahead of print]. with essential hypertension in a primary
25. Ulasi, II, Ijoma CK, Onodugo OD. A care clinic of a tertiary hospital in a
community-based study of hypertension resource-poor environment of Eastern
and cardio-metabolic syndrome in semi- Nigeria. 2014; Br J Med Med Res. 4
urban and rural communities in Nigeria. (18): 3478-3490.
BMC Health Services Res. 2010; 10:71- 34. Akpa MR, Alasia DD, Emem-chioma
78. PC. An appraisal of hospital based blood
26. Ekwunife OL, Udeogaranya PO, Nwatu pressure control in Port Harcourt,
IL. Prevalence, awareness, treatment Nigeria. Nig Health J. 2008; 27-30.
and control of hypertension in a 35. Van de Vijver S, Akinyi H, Oti S,
Nigerian population. Health. 2013; 2 Olajide A, Agyemang C, Aboderin I,
(7):731-735. Kyobutungi C. Status report on
27. Akinkugbe OO, et al. Non- hypertension in Africa- Consultative
communicable Diseases in Nigeria-Final review for the 6th session of the African
report of a National Survey .Lagos: Union Conference of Ministers of
Federal Ministry of Health, Abuja. Health on non-communicable diseases.
1997. Pan Afri Med J. 2013; 16:38-DOI:
10.11604/panj.2013. 16.38.3100.
International Journal of Health Sciences & Research (www.ijhsr.org) 316
Vol.5; Issue: 1; January 2015
36. Iyalomhe GBS, Omogbai EKI, Isah AO, 44. National Hearth, Lung and Blood
Iyalomhe SI, Okhiai O, Dada FL, Institutes: Clinical guidelines on the
Iyalomhe OOB, Comparison of the identification, evaluation and treatment
long-term efficacy and some metabolic of overweight and obesity in adults: The
effects of initiating therapy with evidence report. J Obesity Res. 1998; 6
amlodipine or hydrochlorothiazide in :515-2095.
hypertensive type 2 diabetic Nigerians. 45. Oladapo OO, Salako L, Sodiq O,
Int J Health Sci Res. 2014; 4 (7): 149- Shoyinka K, Adebayo K, Falase AO. A
161. prevalence of cardiometabolic risk
37. Ogunleye OO, Ogundele SO, Akinyemi factors among a rural Yoruba
JO, Ogbera AO. Clustering of Southwestern Nigeria population: a
hypertension, diabetes mellitus and population-based survey. Cardiovasc J
dyslipidemia in a Nigerian population: a Afr. 2010; 21(1): 26-31.
cross sectional study. Afr J Med Med 46. The Trials of Hypertension Prevention
Sci. 2012; 41: 191-195. Collaborative Research Group: Effects
38. Unadike BC, Eregie A, Ohwovoriole of weight loss and sodium reduction
AE. Prevalence of hypertension amongst intervention on blood pressure and
persons with diabetes mellitus in Benin hypertension incidence in overweight
City, Nigeria. Nig J Clin Pract. 2011; people with high-normal blood pressure.
14:300-302. The Trials of Hypertension Prevention,
39. Stewart KJ, Bacher AC, Turner KL, Phase II. Arch Intern Med. 1997;
Fleg JL, Hees PS, Shapero EP, Tayback 157:657-667.
M, Onyang P. Effects of exercise on 47. Dahl LK. Salt and hypertension. Am J
blood pressure. Arch. Int. Med. 2005; Clin Nutr. 1972; 25:231-235.
165: 756-762. 48. Oviasu VO, Okupa PE. Arterial blood
40. McBride P, Einerson J, Hanson P, pressure and hypertension in Benin in
Heindel K. Exercise and the primary the equatorial forest zone of Nigeria.
prevention of coronary heart disease. Trop Geo Med. 1980; 32:232-249.
Med, Exerc, Nutr Health 1992; 1: 5-15. 49. Sever PS, Peart WS, Gordon D,
41. Haskell WL, Leon AS, Caspersen CJ. Brighton P. Blood pressure and its
Cardiovascular benefits and assessment correlates in urban and tribal Africans.
of physical activity and physical fitness Lancet. 1980; 2:60-63.
in adults. Med Sci Sports Exerc. 1992; 50. He FJ, Markandu ND, Sagnella GA,
24(6 Suppl):S201-20. MacGregor GA. Modest salt reduction
42. Blumenthal JA, Babyak MA, Hinderliter lowers blood pressure in both isolated
A. Effects of the DASH diet alone and systolic hypertension and combined
in combination with exercise and weight hypertension. Hypertens. 2005; 46: 66-
loss on blood pressure and 70.
cardiovascular biomarkers in men and 51. Melander O, von Wowern F, Frandsen
women with high blood pressure: the E, Burri P, Wilsteen G, Aurell M,
ENCORE study. Arch Intern Med. Hulthen UL. Moderate salt restriction
2010; 170:126-135. effectively lowers blood pressure and
43. Whelton RK, Appel IJ, Espland MN for degree of salt sensitivity is related to
the Trial of Non-pharmacological baseline concentration of renin and N-
Interventions in the Elderly (TONE) terminal atrial natriuretic peptide in
Collaborative Research Group. Sodium plasma. J Hypertens. 2007; 25(3):619-
reduction and weight loss in the 627.
treatment of hypertension in older 52. Orbarzanek E, Proschan MA, Vollmer
persons. JAMA 1998; 279: 839-846. WM, Moore TJ. Individual blood
pressure responses to changes in salt
International Journal of Health Sciences & Research (www.ijhsr.org) 317
Vol.5; Issue: 1; January 2015
intake: results from the DASH-Sodium evidence to implication, Progress
trial. Hypertens. 2003; 42:459-462. Cardiovasc Dis. 2010; 16(8): 841-843.
53. Iyalomhe GBS, Omogbai EKI, 62. He FJ, Markandu ND, Colhart R, Barron
Iyalomhe OOB, Iyalomhe SI. Serum and J, MacGrogor GA. Effect of short-term
urine electrolyte profiles during supplementation of potassium chloride
amlodipine and hydrochlorothiazide and potassium citrate on blood pressure
combination therapy in Nigerian in hypertension. Hypertens. 2005; 45:
patients with essential hypertension. Br 571-574.
J Med Med Res. 2013; 3 (2): 428-441. 63. Dickinson HO, Nicholson DJ, Campbell
54. Iyalomhe GBS, Omogbai EKI, F, Beyer FR, Mason J. Potassium
Iyalomhe OOB. Long-term electrolyte supplementation in the management of
effects during initiation of primary hypertension in adults.
antihypertensive therapy with Cochrane Data Base of System Rev.
amlodipine or hydrochlorothiazide in 2006; 3: No CD 004641.DO1:
diabetic Nigerians. Am J Med Sci Med. 10:1002/14651858. CD 004691. pub2.
2013; 1 (3): 1-7. 64. Haddy FJ. Roles of salt, potassium,
55. Iyalomhe GBS, Omogbai EKI., Ozolua calcium, and natriuretic factors in
RI. Antihypertensive and biochemical hypertension. Hypertens. 1991; 18(suppl
effects of hydrochlorothiazide and 111): S179-S183.
furosemide in hypertensive Nigerians. J 65. Dwyer JK, Divyer KM, Scribner RA.
Med Sci. 7(6): 977-983. Dietary calcium, calcium
56. Iyalomhe GBS, Omogbai EKI, Ozolua supplementation and blood pressure in
RI, Dada FL, Iyalomhe OOB, 2008 African American adolescents. Am J
Electrolyte profiles in Nigerian patients Clin Nutr. 1998; 68: 648-655.
with essential hypertension. Afr J 66. Grobbee DE, Hofman A. Criteria for
Biotech. 2007; 7(10): 1404-1408. calcium supplementation in essential
57. Adrogue HJ, Madias NE. Sodium and hypertension. Lancet. 1986; 2: 703-708.
potassium in the pathogenesis of 67. Geleijnse JM, Witterman JCM, Bak
hypertension. N Engl J Med. 2007; AAA, den Breijen JH, Grobbee DE.
356:1966-1978. Reduction in blood pressure with a low
58. He FJ, MacGregor GA. How far should sodium, high potassium, high
salt intake be reduced? Hypertens. 2003; magnesium salt in older subjects with
42: 1093-1099. mild to moderate hypertension. BMJ.
59. Fuchs FO, Fuchs SC, Moreira LB, Gus 1994; 309: 436-440.
M, Nobrega AC for PREVER- 68. Nijenhuis T, Vallon V, van der Kemp
prevention trial. Prevention of AW, Loffing J, Hoenderop JG, Bindels
hypertension in patients with RJ. Enhanced passive Ca2+ reabsorption
prehypertension: protocol for the and reduced Mg2+ channel abundance
PREVER-prevention trail. Trial. 2011; explains thiazide-induced hypo-calciuria
12:65. and hypomagnesaemia. J Clin Invest.
60. WHO, World Economic Forum. From 2005; 115 (6): 1651-1658.
burden to best buys: Reducing the 69. Agraharkar M, Rondon – Berrios H,
economic impact of non-communicable Fahlen M. Hypomagnesaemia. eMed
diseases in low and middle-income WebMed. 2006; 1-11.
countries. Geneva, 2001. < 70. Altura BM, Altura BT. Magnesium
http://www.who.int/nmh/publications/be deficiency and hypertension: correlation
st_buys summary.pdf> (Assessed between magnesium deficiency diet and
10/10/2014). microcirculatory changes in situ.
61. He FJ, MacGergor GA. Reducing Science. 1984; 223: 1325-1317.
population salt intake worldwide: From
International Journal of Health Sciences & Research (www.ijhsr.org) 318
Vol.5; Issue: 1; January 2015
71. Witterman JCM, Grobbee DE, Derk 80. American Heart Association (AHA)
FHM, Bouillon AM, Hofman A. Science Advisory: Wine and your heart:
Reduction of blood pressure with oral a science advisory for healthcare
magnesium supplementation in women professionals from the Nutrition
with mild to moderate hypertension. Am Committee Council on Epidemiology
J Clin Nutr. 1994; 60: 129 -135. and Prevention and Cardiovascular
72. Harlan WR, Hull AL, Schmouder RL. Nursing of AHA. Circulation. 2001;
Zinc levels in hypertensives. Am J 103: 472-475.
Epidemiol. 1984; 120: 17-21. 81. Rimm EB, Williams P, Fosher K, Criqui
73. He J, Whelton PK: Effect of dietary M, Stampfer MJ. Moderate alcohol
fiber and protein intake on blood intake and lower risk of coronary heart
pressure: A review of epidemiologic disease: meta-analysis of effects on
evidence. Clin Exper Hypertens. 1999; lipids and haemostatic factors.
21:785-796. BMJ.1999; 319:1523-1528.
74. Appel LJ, Moore TJ, Obarzanek E, 82. Albert MA, Glynn RJ, Ridker PM.
Vollmer WM, Svetkey LP, Sacks FM Alcohol consumption and plasma
for the DASH Collaborative Research concentration of C - reactive
Group: A clinical trial of the effects of protein. Circulation. 2003; 107:443-447.
dietary patterns on blood pressure. N 83. Stockwell T, Greer A, Fillmore K,
Engl J Med. 1997; 339: 1117-1124. Chikritzhs T, Zeisser C. How good is
75. Lawoyin TO, Asuzu MC, Kaufman J, the science? BMJ. 2012; 344:e2276.
Rotimi C, Owoaje E, Johnson L, et al. 84. Joshi P, Islam S, Pais P, et al. Risk for
Prevalence of cardiovascular risk factors early myocardial infarction in South
in an African, urban inner city Asians compared with individuals in
community. West Afr J Med. 2002; other countries. JAMA. 2007; 297:286-
21(3):208-11. 294.
76. Witteman JC, Willett WC, Stampfer MJ, 85. Roy A, Prabhakaran D, Jeemon P, et al.
et al. Relation of moderate alcohol Impact of alcohol on coronary heart
consumption and risk of systemic disease in Indian men. Atherosclerosis.
hypertension in women. Am J Cardiol. 2010; 210:531-535.
1990; 65:633-637. 86. Marschner IC, Simes RJ, Keech A.
77. Klatsky AL, Guderson EP, Kipp Biases in the identification of risk factor
H,Udaltsova N, Friedman GD. Higher thresholds and J-curves. Am J
prevalence of systemic hypertension Epidemiol. 2007; 166:824-831.
among moderate alcohol drinkers: an 87. Naimi T, Xuan Z, Saitz R.
exploration of the role of Immoderately confounding: the effects
underreporting. J Stud Alcohol. 2006; of low-dose alcohol. Addiction. 2013;
67:421-428. 108:1552-1553.
78. Cushman WC, Cutler JA, Hanna E, 88. Beaglehole R, Bonita R, Horton R,
Bingham SF, Follmann D, Harford T, Adams C, et al. Priority actions for the
for the Prevention and Treatment of non-communicable disease crisis. The
Hypertension Study (PATHS): Effects Lancet. 2001; 377(9775):1438-47.
of an alcohol treatment program on 89. Primitesta, Falaschetti E, Gupta S, et al.
blood pressure. Arch Int Med. 1998; Association between smoking and blood
158:1197-1207. pressure: evidence from the health
79. Ryu M, Kimm H, Jo J, Lee SJ, Jee SH. survey from England. Hypertens. 2001;
Association between alcohol intake and 37:187-193.
abdominal obesity among the Korean 90. Virds A, Giannarelli C, Neves MP, et al.
population. Epidemiol Health. 2010; Cigarette smoking and hypertension.
32:79-82.
International Journal of Health Sciences & Research (www.ijhsr.org) 319
Vol.5; Issue: 1; January 2015
Curr Pharm Design. 2010; 16:2518- 93. Strawbridge WJ, Cohen R, Shema S,
2525. Kaplan G. Frequent attendance at
91. Persoskie A, Kaulman AR, Leyva B. religious services and mortality over 28
Receiving and adhering to lifestyle years. Am J Public Health. 1997; 87:
modification counseling for 957-961.
hypertension: Disparities between 94. Lawler-Row KA, Elliot J. The role of
smokers and nonsmokers. J. Clin religious activity and spirituality in the
Hypertens. April 2014; DOI: health and wellbeing of older adults. J
10.1111/jch.12314. Health Psychol. 2009; 14:45-52.
92. Rodgers A, Ezzati M, Vander Hoom S, 95. Roll LL, Klemmack D, Parker M,
Lopez AD, et al. Distribution of major Keomg H, Sawyer-Barker P, Allman R.
health risk: findings from the Global Religiosity, smoking, exercise, and
Burden of Disease study. PLoS Med. obesity among Southern community
Oct 2004; 1(1):e27. dwelling older adults. J Appl
Gerontol. 2005; 24:337-354.
How to cite this article: Iyalomhe GBS, Iyalomhe SI. The increasing burden of uncontrolled
hypertension in Nigeria: the role of lifestyle modification practices as an effective strategy to reverse
the trend. Int J Health Sci Res. 2015; 5(1):309-320.
*******************
International Journal of Health Sciences & Research (IJHSR)
Publish your work in this journal
The International Journal of Health Sciences & Research is a multidisciplinary indexed open access double-blind peer-
reviewed international journal that publishes original research articles from all areas of health sciences and allied branches.
This monthly journal is characterised by rapid publication of reviews, original research and case reports across all the fields
of health sciences. The details of journal are available on its official website (www.ijhsr.org).
Submit your manuscript by email: editor.ijhsr@gmail.com OR editor.ijhsr@yahoo.com
International Journal of Health Sciences & Research (www.ijhsr.org) 320
Vol.5; Issue: 1; January 2015
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Alkaline Diet and LifestyleDocument135 pagesThe Alkaline Diet and LifestyleArtan100% (3)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Zone DietDocument15 pagesThe Zone DietAlejandro Martinez Oviedo50% (2)
- The Dukan Diet Made Easy by Pierre Dukan - ExcerptDocument12 pagesThe Dukan Diet Made Easy by Pierre Dukan - ExcerptCrown Publishing Group100% (4)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Atkins or Fadkins DietDocument14 pagesAtkins or Fadkins Dietlesliev0522Pas encore d'évaluation
- High Frequency Powerlifting Guidelines For Intensity Training Learn How To Structure A High FrequencDocument39 pagesHigh Frequency Powerlifting Guidelines For Intensity Training Learn How To Structure A High Frequenclav the wreckerPas encore d'évaluation
- Classification Essay SampleDocument3 pagesClassification Essay SampleAlvin Malquisto100% (2)
- WheatBelly Diet DR William Davis Ruled A Quack - Weight Loss Doctor Lowcarb Book Author Now Considered Health KookDocument4 pagesWheatBelly Diet DR William Davis Ruled A Quack - Weight Loss Doctor Lowcarb Book Author Now Considered Health KookCrossfitPaleoClasses17% (12)
- Test Bank For Concepts For Nursing Practice 1st Edition, GiddensDocument25 pagesTest Bank For Concepts For Nursing Practice 1st Edition, GiddensILL108Pas encore d'évaluation
- Portion Control GuideDocument1 pagePortion Control GuideTrey HallPas encore d'évaluation
- Meal Plan #1: Meal Food Calories Protein Carbs FATDocument12 pagesMeal Plan #1: Meal Food Calories Protein Carbs FATPradeep ChandraPas encore d'évaluation
- Clinical Gi Case StudiesDocument10 pagesClinical Gi Case Studiesapi-434982019Pas encore d'évaluation
- Health Teaching PlanDocument7 pagesHealth Teaching PlanchloePas encore d'évaluation
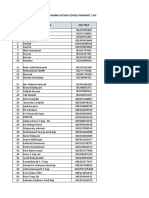
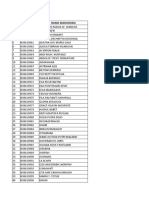
- Sertifikat Relawan Covid19Document36 pagesSertifikat Relawan Covid19Nur Mutmainnah RahmanPas encore d'évaluation
- The Relation of Husband'S Support and Breastfeeding Production Postpartum Maternal in Puskesmas Senori TubanDocument13 pagesThe Relation of Husband'S Support and Breastfeeding Production Postpartum Maternal in Puskesmas Senori Tubanrudy_77Pas encore d'évaluation
- Jurnal Inggris PDFDocument8 pagesJurnal Inggris PDFNur Mutmainnah RahmanPas encore d'évaluation
- Pembagian Nama KMB XxiiiDocument8 pagesPembagian Nama KMB XxiiiNur Mutmainnah RahmanPas encore d'évaluation
- Harvard-MIT Division of Health Sciences and Technology HST.151: Principles ofDocument8 pagesHarvard-MIT Division of Health Sciences and Technology HST.151: Principles ofrobyalfPas encore d'évaluation
- Jurnal InggrisDocument8 pagesJurnal InggrisNur Mutmainnah RahmanPas encore d'évaluation
- 45Document12 pages45Nur Mutmainnah RahmanPas encore d'évaluation
- International Journal of Health Sciences and ResearchDocument8 pagesInternational Journal of Health Sciences and ResearchNur Mutmainnah RahmanPas encore d'évaluation
- Dokumen - Tips Tugas Etika CGCDocument3 pagesDokumen - Tips Tugas Etika CGCnadiraPas encore d'évaluation
- 36Document7 pages36Nur Mutmainnah RahmanPas encore d'évaluation
- Atni Global Index 2016 - 2Document230 pagesAtni Global Index 2016 - 2Nur Mutmainnah RahmanPas encore d'évaluation
- Atni Global Index 2016 - 2Document230 pagesAtni Global Index 2016 - 2Nur Mutmainnah RahmanPas encore d'évaluation
- 2 Telehealth Dalam Pelayanan KeperawatanDocument7 pages2 Telehealth Dalam Pelayanan KeperawatanNur Mutmainnah RahmanPas encore d'évaluation
- Culture ShockDocument4 pagesCulture ShockandradaandonPas encore d'évaluation
- Culture ShockDocument4 pagesCulture ShockandradaandonPas encore d'évaluation
- ArtikelDocument8 pagesArtikelNur Mutmainnah RahmanPas encore d'évaluation
- International Journal of Health Sciences and ResearchDocument8 pagesInternational Journal of Health Sciences and ResearchNur Mutmainnah RahmanPas encore d'évaluation
- International Journal of Health Sciences and ResearchDocument8 pagesInternational Journal of Health Sciences and ResearchNur Mutmainnah RahmanPas encore d'évaluation
- 2 Telehealth Dalam Pelayanan KeperawatanDocument7 pages2 Telehealth Dalam Pelayanan KeperawatanNur Mutmainnah RahmanPas encore d'évaluation
- BDocument8 pagesBAlpi AnorPas encore d'évaluation
- The Complete Guide To Weight Loss and FitnessDocument4 pagesThe Complete Guide To Weight Loss and FitnessOnika BoteroPas encore d'évaluation
- Listado de Libros BodybuildingDocument4 pagesListado de Libros BodybuildingJuanma GonzalezPas encore d'évaluation
- Eat Right For Your TypeDocument5 pagesEat Right For Your Typeapi-242376719Pas encore d'évaluation
- Angela Kennedy Learner AnalysisDocument12 pagesAngela Kennedy Learner AnalysisadmkennPas encore d'évaluation
- English XIIDocument209 pagesEnglish XIIAnimesh MishraPas encore d'évaluation
- Listening 6 Suzzane HindsDocument9 pagesListening 6 Suzzane HindsjamesPas encore d'évaluation
- Recreational Satisfaction Needs Such As Physiological, Educational, Social, RelaxationDocument7 pagesRecreational Satisfaction Needs Such As Physiological, Educational, Social, RelaxationMarites ParaguaPas encore d'évaluation
- Article ObesityDocument28 pagesArticle Obesityfirdauswakrado893833Pas encore d'évaluation
- Nutritional Situation of Elderly Nursing Home ResidentsDocument10 pagesNutritional Situation of Elderly Nursing Home ResidentsPutri yolanda UtamaPas encore d'évaluation
- 45 Before & After' Photos of People Who Beat Anorexia - True ActivistDocument43 pages45 Before & After' Photos of People Who Beat Anorexia - True Activistassev5.orion5Pas encore d'évaluation
- Elc 231 Evaluative Comentary Group 6Document7 pagesElc 231 Evaluative Comentary Group 6Mohamad HazreenPas encore d'évaluation
- DAY 41 INTRODUCTION of Medical Nutrition and TherapyDocument29 pagesDAY 41 INTRODUCTION of Medical Nutrition and TherapyMadhura KarthikPas encore d'évaluation
- Bmifa Boys Z 5 19 LabelsDocument1 pageBmifa Boys Z 5 19 LabelsRhea JavierPas encore d'évaluation
- M.A. in Yoga and Naturopathy, Regulation, Course Structure and Syllabus DetailsDocument15 pagesM.A. in Yoga and Naturopathy, Regulation, Course Structure and Syllabus DetailsS SarojPas encore d'évaluation
- Mini Nutritional Assessment - Short FormDocument16 pagesMini Nutritional Assessment - Short FormmutiazfPas encore d'évaluation
- Correlation Vs CausalityDocument2 pagesCorrelation Vs CausalityBryan Christian MadeloPas encore d'évaluation
- 2019 Guidelines Bariatric Surgery EAES SAGESDocument29 pages2019 Guidelines Bariatric Surgery EAES SAGESDra Maha HafezPas encore d'évaluation
- Fulmer Spices: Comprehensive Assessment Tool For Older AdultsDocument9 pagesFulmer Spices: Comprehensive Assessment Tool For Older AdultsJan Oliver YaresPas encore d'évaluation