Académique Documents
Professionnel Documents
Culture Documents
J Neurosurgery - A Proposed Grading System For Arte Rio Venous Malformations
Transféré par
IngnesDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
J Neurosurgery - A Proposed Grading System For Arte Rio Venous Malformations
Transféré par
IngnesDroits d'auteur :
Formats disponibles
J Neurosurg 65:476-483, 1986
A proposed grading system for arteriovenous
malformations
ROBERT F. SPETZLER, M.D., AND NEIL A. MARTIN, M.D.
Division of Neurological Surgery, Barrow Neurological Institute, Phoenix, Arizona
v- An important factor in making a recommendation for treatment of a patient with arteriovenous malfor-
mation (AVM) is to estimate the risk of surgery for that patient. A simple, broadly applicable grading system
that is designed to predict the risk of morbidity and mortality attending the operative treatment of specific
AVM's is proposed. The lesion is graded on the basis of size, pattern of venous drainage, and neurological
eloquence of adjacent brain. All AVM's fall into one of six grades. Grade I malformations are small, superficial,
and located in non-eloquent cortex; Grade V lesions are large, deep, and situated in neurologically critical
areas; and Grade VI lesions are essentially inoperable AVM's.
Retrospective application of this grading scheme to a series of surgically excised AVM's has demonstrated
its correlation with the incidence of postoperative neurological complications. The application of a standardized
grading scheme will enable a comparison of results between various clinical series and between different
treatment techniques, and will assist in the process of management decision-making.
KEY WORDS 9 arteriovenous malformation 9 grading system 9 surgical resection
prognosis
T
HE surgical treatment of arteriovenous mal- degree of vascular steal, eloquence of adjacent brain,
formations (AVM's) of the brain is primarily and pattern of venous drainage. Other systems are so
intended to eliminate the continued risk of complicated that they are difficult to be applied easily
disastrous intracranial hemorrhage. The decision to and rapidly.ll In order to correct these shortcomings a
recommend surgery rests on an objective comparison simple system that weighs the important features of an
of the long-term risks presented by an untreated AVM, individual AVM, and thus grades the lesion according
with the more immediate risks of operative treatment. to its degree of surgical difficulty, is proposed.
Clearly, the individual patient with an AVM is bene- Description of Grading System
fited only if his operation is accomplished without mor-
tality or disabling morbidity. As there is now infor- Graded Variables
mation on the long-term risks or natural history of The major factors important in determining the dif-
untreated AVM's, educated surgical decision-making ficulty of resecting an AVM include: size, number of
requires an objective method - - a grading system - - feeding arteries, amount of flow through the lesion,
for predicting the risks of operation in individual cases degree of steal from surrounding normal brain, loca-
of AVM's. tion, surgical accessibility, eloquence of adjacent brain,
An ideal grading system would define, for each spe- and pattern of venous drainage. A grading system based
cific AVM, the degree o f difficulty involved in safely on all of the above variables would be too cumbersome
removing the malformation. Such a grading system for practical use. However, experience with the man-
should provide a reasonably accurate estimation of agement of AVM's has established that many of these
operative morbidity and mortality, and be simple yet factors are interrelated, allowing us to simplify the
comprehensive enough to be readily applied to all cere- grading process. By reducing the graded variables to
bral AVM's. Previously proposed grading schemes, three generalized features o f AVM's, the scheme can be
which have been based only on AVM size or on the simplified without ignoring critical factors. The three
number and distribution of feeding arteries, are simple variables considered are: 1) size of the AVM; 2) pattern
enough to be easily applicable. 8 These fail, however, to of venous drainage; and 3) neurological eloquence of
consider such important variables as anatomic location, the brain regions adjacent to the AVM.
476 J. Neurosurg. / Volume 65/October, 1986
Grading system for arteriovenous malformations
Size of the A VM. The size of the AVM is deter-
mined by measuring on angiograms the largest diameter
of the nidus o f the malformation. When magnified
angiographic views are considered, a correction for the
magnification factor is required. The size of the AVM
is determined to be small (< 3 cm), medium (3 to 6
cm), or large (> 6 cm), and the AVM is scored appro-
priately.
The size of the malformation is responsible for much
of the technical difficulty in removing AVM's. The
larger an AVM, the larger the a m o u n t of normal adja-
cent neural tissue that is exposed to injury during
microsurgical resection o f the nidus. Large AVM's
mandate longer operating time, thereby increasing the
risk of anesthesia-related complications. Furthermore,
the criterion of size encompasses several of the other
important factors that determine the degree of surgical
difficulty. In general the size of an AVM determines,
or is closely related to, the number of feeding arteries,
the amount of flow, and the degree of steal.
Pattern of Venous Drainage. The course of the
draining veins is determined from the angiogram. The
venous pattern is considered superficial if all the drain-
age from the AVM is through the cortical venous sys-
tem. The venous pattern is considered deep if any or
all of the drainage is through deep veins (such as
internal cerebral veins, basal veins, or precentral cere-
bellar vein). In the posterior fossa, only cerebellar hemi-
spheric veins that drain directly into the straight sinus
or transverse sinus are considered to be superficial veins.
Clearly, the pattern o f venous drainage is closely
related to the surgical accessibility of an AVM. Deep
venous drainage, no matter how small, further compli- FIG. 1. The anatomic areas considered neurologically el-
cates AVM excision. Often the vast majority of an oquent for the purposes of the grading system are indicated.
The deep eloquent areas (hypothalamus, thalamus, brain
AVM will have been separated from the surrounding stem, and cerebellar peduncles) are highlighted in the upper
brain when the small arterialized subependymal veins image. The eloquent regions of the cerebral cortex (sensori-
of the deep component are encountered. These veins motor areas, language areas, and primary visual area) are
are friable, resist bipolar coagulation, and have the identified on the lower image.
dangerous propensity to retract and bleed into the
parenchyma or ventricle when disrupted.
Eloquence of Adjacent Brain. Eloquent brain re- available, can easily be used for grading brain eloquence
gions are defined as those that speak to readily identi- in this scheme. The removal o f AVM's adjacent to
fiable neurological function and, if injured, result in a eloquent areas carries a m u c h greater risk o f disabling
disabling neurological deficit. For the purpose of this neurological morbidity than does excision o f these le-
grading scheme, the following are considered eloquent sions from less critical regions. The brain that is adja-
areas (Fig. 1): the sensorimotor, language, and visual cent to the AVM is liable to experience damage during
cortex; the hypothalamus and thalamus; the internal surgery from AVM dissection and retraction, and after
capsule; the brain stem; the cerebellar peduncles; and surgery from postoperative hemorrhage or edema.
the deep cerebellar nuclei. Areas with much more subtle
neurological function, or areas in which injury does not Determination of Grade
cause permanent disabling deficit (such as the anterior In order to assign an AVM grade, the size, the venous
portion of the frontal or temporal lobes, or the cerebel- drainage, and the eloquence o f the adjacent brain are
lar cortex) are considered non-eloquent. To preserve determined from angiography, computerized tomogra-
simplicity, it is assumed that eloquent cortical regions phy (CT), and/or magnetic resonance imaging (MRI).
occupy their normal anatomic location. For the purpose Particularly with deep supratentorial or posterior fossa
of grading, Wada testing or electrophysiological map- malformations, CT and MRI are helpful in delineating
ping techniques designed to precisely localize eloquent the topographical relationship of the AVM to eloquent
cortex are not required. Data from these techniques, if regions. A numerical value is assigned for each of the
J. Neurosurg. / Volume 65/October, 1986 477
R. F. Spetzler and N. A. Martin
FIG. 4. Carotid angiograms, lateral view (left) and antero-
posterior view (right), showing a Grade II arteriovenous mal-
FIG. 2. Carotid angiograms, lateral view (left) and antero- formation (AVM). The AVM is less than 3 cm (small: 1
posterior view (right), showing a Grade I arteriovenous mal- point), located in the dominant hemisphere adjacent to the
formation (AVM). This AVM is less than 3 cm in diameter receptive language area (Wernicke's area) (eloquent: 1 point),
(small: 1 point), located in the anterior frontal lobe (non- and has exclusively superficial venous drainage (arrow) (su-
eloquent: 0 points), and drains through cortical veins (arrows) perficial drainage: 0 points).
(superficial drainage: 0 points).
categories (Table 1). The grade o f the lesion is derived
TABLE 1 by s u m m i n g the points assigned for each category. The
Determination of arteriovenous malformation (A VM) grade* lowest grade possible is G r a d e I; such a lesion would be
small (1 point), located in a n o n - e l o q u e n t region such
Graded Feature Points Assigned
as the anterior frontal lobe (0 points), a n d have exclu-
size of AVM sively superficial drainage (0 points) (Figs. 2 and 3).
small (< 3 cm) 1 Complete surgical excision o f such an A V M would
medium (3-6 cm) 2
large (> 6 cm) 3 present relatively m i n o r technical difficulties and would
eloquence of adjacent brain entail very little risk o f resultant m o r b i d i t y or mortality.
non-eloquent 0 The highest grade within this scheme is G r a d e V; an
eloquent 1 A V M o f this type would be larger t h a n 6 c m (3 points),
pattern of venous drainage
superficial only 0 located within or immediately adjacent to eloquent
deep 1 brain (1 point), and a portion o f the drainage would
* Grade = [size] + [eloquence] + [venous drainage]; that is (1, 2, e m p t y into the deep venous system (1 point) (Figs. 7
or 3) + (0 or 1) + (0 or 1).
FIG. 3. Vertebral angiograms, lateral view (left) and an-
teroposterior view (right), showing a Grade I arteriovenous FIG. 5. Carotid angiograms, lateral view (left) and antero-
malformation (AVM). This cerebellar AVM is less than 3 cm posterior view (right), showing a Grade III arteriovenous
in diameter (small: 1 point), located superficially on the cere- malformation (AVM). The AVM is less than 3 cm (small: 1
bellar cortex (non-eloquent: 0 points), and drains only through point), located adjacent to the thalamus (eloquent: 1 point),
superficial cerebellar hemispheric veins (arrows) (superficial and drains into the galenic venous system (arrow) (deep
drainage: 0 points). drainage: 1 point).
478 J. Neurosurg. / Volume 65 /October, 1986
Grading system for arteriovenous malformations
FIG. 6. Carotid angiograms, lateral view (left) and anteroposterior views, arterial phase (center) and venous
phase (right), showing a Grade IV arteriovenous malformation (AVM). This AVM is slightly less than 6 cm
in diameter (medium: 2 points), located in the dominant parietal lobe adjacent to Wernicke's area (eloquent:
1 point), and drains in part into the galenic system (arrow) (deep drainage: 1 point).
and 8). A Grade V lesion is associated with significant representation of all 12 possible combinations of the
risk of surgical morbidity and mortality. These large, graded criteria is found in Fig. 10.
critically located malformations require extensive dis- There are certain lesions that should not currently be
section in close proximity to important brain regions; considered for surgery. Within this group are extremely
their removal m a y be complicated by difficulties with large diffuse A V M ' s that are dispersed through critical
controlling fragile deep veins. Obliteration of the large neurologically eloquent areas, or malformations with a
AVM shunt presents surrounding normal vessels with diffuse nidus that encompasses critical structures such
a sudden increase in perfusion that m a y result in vaso- as the hypothalamus or brain stem (Fig. 9). As surgical
genic edema or even hemorrhage (a p h e n o m e n o n that resection of such lesions would almost unavoidably be
has been termed " n o r m a l perfusion pressure break- associated with a totally disabling deficit or death, these
through"). ~3 Various combinations of lesion size, loca- AVM's fall into a separate category that can be termed
tion, and venous drainage pattern result in the inter- "Grade VI" or, more simply, "inoperable."
mediate grades of A V M (Figs. 4 to 6). A schematic
FIG. 8. Vertebral angiograms, anteroposterior view (left)
FIG. 7. Carotid angiograms, arterial phase (left) and ve- and lateral view, venous phase (right), showing a Grade V
nous phase (right), showing a Grade V arteriovenous malfor- arteriovenous malformation (AVM). This posterior fossa
mation (AVM). This AVM is larger than 6 cm in its greatest AVM is larger than 6 cm (large: 3 points), located in the
diameter (large: 3 points), located in the corpus callosum with cerebellar hemisphere with extension into the inferior cere-
a deep thalamic component (eloquent: 1 point), and drains bellar peduncle and region of the deep cerebellar nuclei (elo-
predominantly into a hugely dilated internal cerebral vein quent: 1 point), and drains primarily into the galenic system
(arrow) (deep drainage: I point). (deep drainage: 1 point).
J. Neurosurg. / Volume 65/October, 1986 479
R. F. Spetzler and N. A. Martin
TABLE 2
Correlation of A VM grade with surgical results*
Minor Major
Grade No. of No Deficit Deficit Deficit Death
Cases (%)
No. % No. % No. %
I 23 23 100 0 0 0 0 0
II 21 20 95 1 5 0 0 0
III 25 21 84 3 12 1 4 0
IV 15 11 73 3 20 1 7 0
V 16 11 69 3 19 2 12 0
total 100 86 86 10 10 4 4 0
* See also Fig. 11. AVM = arteriovenous malformation.
FIG. 9. Vertebral angiograms, anteroposterior view (left)
and lateral view, arterial phase (right), showing an inoperable
(Grade VI) arteriovenous malformation (AVM). This AVM TABLE 3
is fed by multiple vessels from the rostral basilar artery, Details of instances of deficit
encircling and infiltrating the mesencephalon. The diffuse
involvement of the brain stem renders this lesion inoperable. Minor Deficit
1. very mild increase in brain-stem deficit
2. temporary increase in visual field deficit
3. temporary increase in aphasia and weakness
Application o f the Grading S c h e m e 4. mild increase in aphasia (resolved 90%) only detectable
with rapid speech
In order to test the predictive value of this system, 5. temporary mild increased weakness
100 consecutive A V M ' s completely resected by one of 6. increase in trigeminal nerve deficit (anticipated)
us (R.S.) were retroactively analyzed. The lesions were 7. mild temporary increase in hemiparesis
graded on the basis of their radiographic studies, and 8. mild residual ataxia
the complications of surgery for the malformations in 9. temporary mild dysphasia
Major Deficit
each grade were tabulated and presented in numerical 1. hemiparesis
and graphic form (Table 2 and Fig. 11). The compli- 2. increase in aphasia
cations were broken down into the categories of minor 3. homonymous hemianopsia (anticipated)
deficit, major deficit, and mortality. Temporary neu- 4. severe neurological deficit (presumed normal perfusion
pressure breakthrough) with major aphasia and hemi-
rological deficits lasting less than 3 days are not in- paresis
cluded. There was no mortality. The specifics of mor-
bidity are listed in Table 3. The results indicate that the
correlation between A V M grade and the incidence of
neurological complications is good. Grade I and II
lesions were resected with very low incidence of surgi- and a similarly sized AVM located in the thalamus. By
cally induced neurological deficit, while surgery for just using size, both A V M ' s would be considered as
Grade IV and V A V M ' s was accompanied by a signifi- Grade I; however, by including both eloquence and
cant number of neurological complications. deep venous drainage the AVM's are, respectively, in
In order to test the reliability and consistency of the Grades I and III, assessing correctly the expected mor-
grading system, 25 angiograms o f patients with AVM's bidity and mortality in the surgical management of
were graded independently by one o f the authors and each lesion.
by two other neurosurgeons. There was complete agree-
Discussion
ment a m o n g all the observers in 23 of the 25 cases, and
in 24 of 25 cases between one of the authors and a Simply put, surgical removal of an AVM is indicated
neurosurgeon. In two cases the grades varied by one; in if the risk of operation is less than the risk determined
each instance the presence or absence of eloquence was by the natural history of the AVM. As more data have
in question. In one case an A V M was situated in the accumulated, it has become apparent that the long-
anterior portion of the d o m i n a n t temporal lobe, and in term prognosis for patients with A V M ' s is grim. The
the other the AVM was situated in the periventricular ongoing risk of intracranial hemorrhage from an AVM
area of the left frontal horn. Even in retrospect the is 2% to 3% per year, and the risk for recurrent hem-
judgment is difficult. Thus, there is excellent correlation orrhage is higher than this, at least temporarily, after an
between independent observers in grading AVM's based AVM has bled. 4,5 The risk of death associated with
on this system. initial A V M rupture is approximately 10%, and the
The need for all three variables becomes quickly mortality rate increases with each subsequent hemor-
apparent when the operative difficulty is compared rhage? '~2 The incidence of neurological deficit is ap-
between an AVM of 2 cm located in the frontal pole proximately 50% for each episode of hemorrhage. 16 In
480 J. Neurosurg. / Volume 65/October, 1986
Grading system for arteriovenous malformations
FIG. 10. Diagrammatic representation of the combinations of graded variables (size, eloquence, and venous
drainage) that are possible for each grade of arteriovenous malformation. There is one combination each for
Grades I and V, three combinations each for Grades II and IV, and four possible combinations for Grade III.
addition to the complications of intracranial hemor- patient with an AVM requires specific consideration of
rhage, patients with A V M ' s face the lesser risks of certain characteristics of both the AVM itself and the
developing flow-related symptoms, such as ischemic patient harboring the AVM. For instance, untreated
deficit due to steal. AVM's located in the posterior fossa appear to have a
An estimation of the risk that confronts an individual particularly poor prognosis, 4 and small AVM's seem to
J. Neurosurg. / Volume 65/October, 1986 481
R . F. S p e t z l e r a n d N . A . M a r t i n
20% -
m MAJORDEFICIT to take into consideration every possible anatomic and
physiological permutation of AVM's, the scheme would
[~ MINORDEFICIT have to be so complex as to be impractical.
This grading system has demonstrated a relationship
to the technical difficulty of removing individual
AVM's. Virtually all the Grade I and II AVM's were
10% removed without much difficulty in single-staged pro-
cedures. The Grade IV and V lesions, however, often
required pre- and intraoperative embolization and mul-
tistaged surgical resection.
This grading system is designed to be predictive of
the results of complete surgical resection of AVM's.
This remains the "gold standard" for the treatment of
0% ~ J AVM's, as it is the only method that virtually eliminates
I II Ill IV V
GRADES
the risk of future hemorrhage. Long-term follow-up
review of patients whose AVM's were completely ex-
FIG. 11. Correlation of arteriovenous malformation grades cised has confirmed that they are almost fully protected
with surgical results. See also Table 2.
from rebleeding. 3 Incomplete surgical removal and
feeding artery ligation do not prevent later bleeding, z3
Incomplete obliteration of the AVM by embolization
also fails to provide protection from subsequent hem-
have a greater propensity to bleed spontaneously than orrhage. 9 Even in cases that show complete angio-
do large malformations. 5 Children face a greater danger graphic obliteration after embolization, there is no as-
than do adults in that they have before them the period surance that hemorrhage cannot occur in the future. In
of life of highest risk for AVM rupture (ages 15 to 40 such thoroughly embolized cases, the nidus of the AVM
years)/'~2 Patient-specific characteristics such as these nevertheless remains in the brain and the possibility for
must be considered in the formulation of prognosis for delayed recanalization of portions of the malformation
each case. Recently published reviews provide a more through collateral channels exists.
detailed analysis of the clinical features that influence Stereotaxically directed radiation therapy is another
the behavior of individual AVM's and of the natural technique available for the treatment of AVM's. 6'~5Our
history of these lesions as a g r o u p . 7'~6 grading system may be applied to lesions treated either
There is less available information that can be applied by radiation therapy or by embolization for the purpose
to a determination of the risks that attend surgical of comparing the results of these techniques with those
removal of an individual AVM. In the past, this esti- of surgical excision. It is, however, quite possible that
mation has been dependent on the knowledge and this system will not accurately predict the results of
personal experience of the surgeon involved in the case, embolization or radiation therapy, as the complications
and has often been imprecise and nonsystematic. It has of these types of treatment differ from those of surgery.
been difficult to apply the surgical results as reported in A prospective application of this grading scale in
the literature because the AVM's in these reports have AVM cases is currently underway. If this scale in its
been incompletely characterized. 2'~~ simplicity proves to predict operative morbidity in other
As discussed above, categorization of AVM's accord- series, it will provide a useful tool for decision-making
ing to size or number of feeding arteries only is insuf- in the management of patients with AVM's. As a
ficient. For these reasons this grading system was con- further benefit, it will facilitate comparison of AVM
structed. It is simple, easy to learn, and easy to apply. treatment results between series or between techniques.
No relatively simple grading system will accurately
classify all the variations of such complex vascular
lesions. For instance, relatively small AVM's may have Acknowledgments
more or less direct arteriovenous connections resulting The authors would like to thank Marjorie Medina, R.N.,
in very high flows - - a feature that considerably com- and Drs. Issam Awad and Daniele Rigamonti for independ-
plicates their surgical treatment. This system may assign ently assisting in grading the AVM's.
an inappropriately low grade to such a lesion, since size
rather than flow is scored. The location and organiza- References
tion of eloquent areas, particularly those adjacent to an
AVM, may vary from the norm and thus be another 1. Celli P, Ferrante L, Palma L, et al: Cerebral arteriovenous
potential source of error. This may result in under- or malformations in children. Clinical features and outcome
of treatment in children and in adults. Surg Neurol 22:
overestimation of the risk of causing significant neu- 43-49, 1984
rological deficit in a specific case. In spite of occasional 2. Drake CG: Cerebral arteriovenous malformations: con-
inappropriateness of the assigned grade, we believe that siderations for and experience with surgical treatment in
the simplicity of the system is an advantage. In order 166 eases. Clin Neurosurg 26:145-208, 1979
482 J. Neurosurg. / Volume 65 /October, 1986
Grading system for arteriovenous malformations
3. Forster DMC, Steiner L, Hfikanson S: Arteriovenous nous malformations. A study in surgical decision-making.
malformations of the brain. A long-term clinical study. J Acta Neuroehir Suppl 29:1-86, 1980
Ncurosurg 37:562-570, 1972 12. Perret G, Nishioka H: Report on the Cooperative Study
4. Fults D, Kelly DL Jr: Natural history of arteriovenous of Intracranial Aneurysms and Subarachnoid Hemor-
malformations of the brain: a clinical study. Neurosurgery rhage. Section VI. Arteriovenous malformations. An anal-
15:658-662, 1984 ysis of 545 cases of cranio-cerebral arteriovenous malfor-
5. Graf C J, Perret GE, Torner JC: Bleeding from cerebral mations and fistulae reported to the Cooperative Study.
arteriovenous malformations as part of their natural his- J Neurosurg 25:467-490, 1966
tory. J Neurosurg 58:331-337, 1983 13. Spetzler RF, Wilson CB, Weinstein P, et al: Normal
6. Kjellberg RN, Hanamura T, Davis KR, et al: Bragg-peak perfusion pressure breakthrough theory. Clin Neurosurg
proton-beam therapy for arteriovenous malformations of 25:651-672, 1978
the brain. N Engi J Med 309:269-274, 1983 14. Stein BM, Wolpert SM: Arteriovenous malformations of
7. Luessenhop A J: Natural history of cerebral arteriovenous the brain. I. Current concepts and treatment. Arch Neurol
malformations, in Wilson CB, Stein BM (eds): Intracra- 37:1-5, 1980
nial Arteriovenous Malformations. Baltimore: Williams 15. Steiner L: Treatment of arteriovenous malformations by
& Wilkins, 1984, pp 12-23 radiosurgery, in Wilson CB, Stein BM (eds): Intracranial
8. Luessenhop A J, Gennarelli TA: Anatomical grading of Arteriovenoas Malformations. Baltimore: Williams &
supratentorial arteriovenous malformations for determin- Wilkins, 1984, pp 295-314
ing operability. Neurosurgery 1:30-35, 1977 16. Wilkins RH: Natural history of intracranial vascular mal-
9. Luessenhop AJ, Presper JH: Surgical embolization of formations: a review. Neurosurgery 16:421-430, 1985
cerebral arteriovenous malformations through internal
carotid and vertebral arteries. Long-term results. J Neu-
rosurg 42:443-451, 1975
10. Parkinson D, Bachers G: Arteriovenous malformations. Manuscript received July 3, 1985.
Summary of 100 consecutive supratentorial cases. J Neu- Accepted in final form April 10, 1986.
rosurg 53:285-299, 1980 Address reprint requests to: Robert F. Spetzler, M.D.,
11. Pellettieri L, Carlsson CA, Grevsten S, et al: Surgical Editorial Office, Barrow Neurological Institute, 350 West
versus conservative treatment of intracranial arteriove- Thomas Road, Phoenix, Arizona 85013.
J. Neurosurg. / Volume 65 / October, 1986 483
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- GavareskiDocument7 pagesGavareskiMohamed MostafaPas encore d'évaluation
- Urodynamics (Aquick Pocket Guide)Document210 pagesUrodynamics (Aquick Pocket Guide)ZICO100% (2)
- Nursing Shift EndorsementDocument6 pagesNursing Shift Endorsementebrahim102099Pas encore d'évaluation
- MSBOS PrithvirajDocument8 pagesMSBOS Prithvirajkarun1889Pas encore d'évaluation
- Services: Hospital GasesDocument41 pagesServices: Hospital GasesRevati shinde100% (1)
- Advertisement KMTC 2019.2020. CleanedDocument2 pagesAdvertisement KMTC 2019.2020. CleanedMigori ArtPas encore d'évaluation
- Braxton Hicks or True Labor ContractionsDocument2 pagesBraxton Hicks or True Labor ContractionsJellyAnnGomezPas encore d'évaluation
- Part 1 MRCOG - SyllabusDocument6 pagesPart 1 MRCOG - SyllabusDr. Zaheer AliPas encore d'évaluation
- Pregnancy Polarity TherapyDocument3 pagesPregnancy Polarity TherapyJim FultonPas encore d'évaluation
- Advance Instruments For Laparoscopic SurgeryDocument7 pagesAdvance Instruments For Laparoscopic SurgeryAroelPas encore d'évaluation
- Pediatric Neuroanesthesia.3Document4 pagesPediatric Neuroanesthesia.3Mae Importers IncPas encore d'évaluation
- A Study of Patient Satisfaction Level in Out Patient Department (OPD) in A Tertiary Care Hospital in MaharashtraDocument9 pagesA Study of Patient Satisfaction Level in Out Patient Department (OPD) in A Tertiary Care Hospital in MaharashtraVital TejaPas encore d'évaluation
- Displacement of UtreusDocument13 pagesDisplacement of UtreusswethashakiPas encore d'évaluation
- PCOS DR BasimaDocument18 pagesPCOS DR BasimaA.H.APas encore d'évaluation
- Blood Storage Policy and ProcedureDocument3 pagesBlood Storage Policy and ProcedureMohamed AllamPas encore d'évaluation
- Retropubic SpaceDocument4 pagesRetropubic SpacesakuraleeshaoranPas encore d'évaluation
- OR AppendixDocument9 pagesOR AppendixDan HizonPas encore d'évaluation
- Health Family Welfare 3Document225 pagesHealth Family Welfare 3Gopala Sundararaj SPas encore d'évaluation
- VAC Diversified FlowDocument1 pageVAC Diversified FlowWinnie AtienoPas encore d'évaluation
- Colposcopy - UpToDateDocument25 pagesColposcopy - UpToDatemew2xxPas encore d'évaluation
- Relationship Between Maternal Haemoglobin and Fetal Weight: Rana SS, Sharma S, Chand A, Malla RDocument4 pagesRelationship Between Maternal Haemoglobin and Fetal Weight: Rana SS, Sharma S, Chand A, Malla RSatria UtamaPas encore d'évaluation
- Self Applied Topical Fluorides ClassDocument23 pagesSelf Applied Topical Fluorides ClassultraswamyPas encore d'évaluation
- Effects of High Dose Vitamin C Supplementation On Severe Covid19 Patients in The ICU - A Retrospective AnalysisDocument1 pageEffects of High Dose Vitamin C Supplementation On Severe Covid19 Patients in The ICU - A Retrospective AnalysiszipzoinkPas encore d'évaluation
- 1 - Overview of Maternal and Newborn Care - 08022014 - PHA RHMPP and NDPsDocument25 pages1 - Overview of Maternal and Newborn Care - 08022014 - PHA RHMPP and NDPsBoj OdejarPas encore d'évaluation
- 20140424040901417Document8 pages20140424040901417Anonymous h0DxuJTPas encore d'évaluation
- Abdominal Incisions: A Simple Guide For NursesDocument25 pagesAbdominal Incisions: A Simple Guide For Nursesfaris.surgeonPas encore d'évaluation
- Documentation of Nutritional Care ProcessDocument22 pagesDocumentation of Nutritional Care ProcessRojeil Mark Napudo MovillaPas encore d'évaluation
- Maternal & Child NursingDocument10 pagesMaternal & Child Nursingnokolip100% (2)
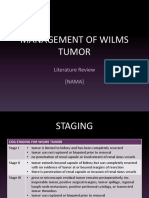
- Management of Wilms Tumor: Literature Review (NAMA)Document15 pagesManagement of Wilms Tumor: Literature Review (NAMA)DeaNataliaPas encore d'évaluation
- Self-Directed Learning (Nur 146 - Clinical Area)Document2 pagesSelf-Directed Learning (Nur 146 - Clinical Area)Dyan Bianca Suaso LastimosaPas encore d'évaluation