Académique Documents
Professionnel Documents
Culture Documents
Diabetes
Transféré par
suzluDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Diabetes
Transféré par
suzluDroits d'auteur :
Formats disponibles
Diabetes-
eat a meal, beta cells in pancreas will produce insulin which picks up glucose from blood &
stores it in tissues; pancreas also secretes glucagon which promotes higher glucose levels
(glucagon for people who are severely hypoglycemic & can’t be given IV dextrose, etc; there are
other ancillary mechanisms that regulate glucose as well)
Type I versus type II diabetes-
Type 1: childhood/ autoimmune, body attacks & destroys own beta cells; underproduce or don’t
produce insulin; tx is insulin replacement; polydipsia, polyuria, polyphagia (lotsa peeing, very
thirsty, very hungry) Hyperglycemia beyond 400-500, sx of confusion, cardiovascular collapse,
long-term damage
Type 2: tissues are resistant to effects of insulin, not a lack of insulin until late-stages, usually
developed in middle age, result of obesity/diet, no sx while body is compensating, elevated
insulin in body & then will no longer sustain & drop levels; latter part of disease less efficient/no
production of insulin in pancreas
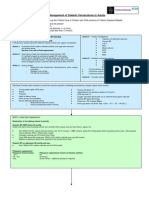
Factors affecting glucose control
Diagnostic Criteria:
A1C ≥6.5%
OR
Fasting plasma glucose (FPG)
≥126 mg/dl (7.0 mmol/l)
OR
Two-hour plasma glucose ≥200 mg/dl (11.1 mmol/l) during an OGTT
OR
A random plasma glucose ≥200 mg/dl (11.1 mmol/l)
2. Epidemiology- Estimated 23.6 million adults in the United States; 5.7 million are undiagnosed.
Ped diabetes estimated in 57 million Americans
N677 – SPRING 2011 – J. LOPEZ, PHARM.D. 1
Predictive Factors for Developing Type 2 DM - Metabolic syndrome
NCEP criteria: (3 or more are present)
1. Increased body weight & Waist circumference >40” in men, >35” in women
2. High triglycerides >150
3. Low HDL- Less than 40 in men or less than 50 in women
4. Insulin resistance- Fasting >100 or DM treatment
5. Hypertension- BP >130/>85 or on treatment
• The prevalence of metabolic syndrome is 20% of the population >20 years old and 40%
greater than 50 years old – and it is increasing!
• The risk of developing diabetes increases with the number of factors present. With 3
factors the risk is approximately 7-9 X more likely to develop diabetes as compared to having
no factors present.
• A public health strategy is to reduce metabolic syndrome in order to prevent diabetes.
Home blood glucose testing
3. Outcomes
Microvascular: nervous system damage, retinopathy, nephropathy
Macrovascular: coronary artery disease, stroke
4. Therapeutic goals (ADA)
N677 – SPRING 2011 – J. LOPEZ, PHARM.D. 2
Alternative goals are based on specific patient factors- other co-existing diseases present, may
want to remain at lower A1C (ex- CA with mets) Long-term benefits examined
Key studies of diabetes treatment
The DCCT and the UK Prospective Diabetes Study
UKPDS Key findings:
Conventional vs intensive control:
12% decrease in any diabetes endpoint
25% decrease in microvascular endpoints
16% decrease in MI
21% decrease in retinopathy at 12 years
33% decrease for microalbuminuria at 12 years
Sulfonyulurea vs Insulin:
No differences in glucose control
No differences in risk reduction
No increased evidence of cardiac effects with sulfonylureas
No evidence of increased atheroma formation with insulin
Metformin:
Vs conventional therapy
32% risk reduction in any diabetes endpoint
42% decrease in any diabetes related death
36% reduction in mortality
39% reduction in myocardial infarct
Metformin may be advantageous in obese type 2 diabetics.
In hypertensive diabetics either beta blockers or ACE inhibitors had equal effects in
reducing BP and diabetes related endpoints.
Treatment goals: beta blockers ok in type 1 diabetics, but not if have hypoglycemia since they
are usually using intense insulin
Ideal Goal – Normal A1c of less than 6
Tight control (HgbA1c less than 7)
N677 – SPRING 2011 – J. LOPEZ, PHARM.D. 3
70-105 before meals
<150 2 hrs postprandial
Practical control (HgbA1c less than 8)
90-140 before meals
<180 2 hrs postprandial
fasting less than 140
no value less than 60
Reasonable control in older patients
HgbA1c less than 9 and minimize DM symptoms.
INSULIN
1. Human insulin
2. Types of insulin
Insulin name Onset Peak Duration
Regular 0.5-1 hr 2-5 hr 6-8 hr
NPH 1-2 hr 6-12 hr 18-26 hr
(Lente, semilente and ultralente taken off the market)
Newer insulins:
lispro insulin: very quick onset; short duration of action.
insulin aspart: ditto
insulin glulisine (Apidra) ditto
insulin glargine (Lantus): very long acting insulin
insulin detemir (Levemir) also very long acting
3. Dosing strategies
In type 1 you want to provide basal control (Glargine or Detemir) & quick-acting insulin; another
strategy includes the pump for continuous delivery, boluses for when eating
In type 2, can begin 2 ways- if pt is failing oral meds, begin with nighttime dosing NPH or can
start immediately with insulin/ morning NPH, possibly single dose to last entire day or can be
split between morning & evening (to control lunch/dinner hyperglycemia, can add regular insulin
to regiment; can buy pre-mixed)
Single dose
Split dosing
Mixed insulin
Insulin pumps
4. Adjusting insulin dosing
Work backwards from glucose results to when the insulin should be having its peak
effect:
_8_________________12___________________6_____________________
AM NPH Dinner glucose
AM regular Lunch glucose
Evening regular ->Bedtime
N677 – SPRING 2011 – J. LOPEZ, PHARM.D. 4
Evening NPH -> fasting glucose
5. Tight control strategy
Baseline long acting
PLUS regular before meals (adjusted)
6. Initiation of insulin in type 2 diabetes (combination with oral drugs)
7. Patient education, administration technique, storage, supplies (syringes, swabs),
hypoglycemia management
8. Inhaled insulin (Exubera) – off the market in 2008, will Oralin arrive soon?
ORAL ANTI-DIABETIC MEDICATIONS
Oral Sulfonylureas
1. Pharmacology
√ Stimulates beta cells to release insulin
√ Increases tissue sensitivity to insulin
√ ~ 1.5-2% drop in A1c with proper titration
2. Dosing
Drug Total Daily Dose Frequency
Tolbutamide (Orinase) 500 - 3000 mg BID - TID
Tolazamide (Tolinase) 100 - 1000 mg QD - BID
Chlorpropamide (Diabenese) 100 - 500 mg QD
Glipizide (Glucotrol) 2.5 - 40 mg QD-BID
Glyburide (Diabeta, Micronase) 1.25 - 20 mg QD-BID
Glyburide Prestab (Glynase) 1.5 - 12 mg QD- BID
Glimepiride (Amaryl) 1 - 8 mg QD - BID
3. Adverse effects
Hypoglycemia
Rarely: hepatitis, allergic reactions, rash, nausea, SIADH, antabuse reactions
Primary and secondary failure to oral sulfonylureas
4. Drug Interactions
5. Patient education
Metformin (Glucophage®) – only drug in its class (phenformin in 60’s associated with lactic
acidosis) Contraindicated in decreased renal function & risk of accumulation
The higher the A1C level, the quicker the reduction when given Metformin (11.5-8 in one
month for instance)
1. Pharmacology:
√ Increased glucose uptake by muscle
√ Decreased hepatic glucose production
√ Decreased intestinal glucose availability
N677 – SPRING 2011 – J. LOPEZ, PHARM.D. 5
Pharmacokinetics:
Bioavailabiltiy = 50-60%
Excreted unchanged in urine
Half-life = 6 hrs
2. Clinical Efficacy Summary:
The US Pivotal Trial:
143 patients given metformin versus 146 patients given placebo
length: 29 weeks
fasting plasma glucose: 189 vs 244 mg/dl
HgA1c 7.1% versus 8.5%
The US metformin + glyburide study
632 patients already on oral sulfonylureas who did not have acceptable fasting
plasma glucose on maximal glyburide dose (20 mg/day). They were randomized
to continue glyburide, switch to metformin or receive the combination of both
drugs for a 5 week titration phase followed by 24 weeks maintenance.
Patients receiving combination therapy had significant decreases in both fasting
plasma glucose (187 vs 261 mg/dl) and HgA1c (7.1% vs 8.7%)
3. Adverse Effects and Other Cautions
GI: diarrhea, nausea, abdominal pain, anorexia, metallic taste. May be transient and dose
related. Minimize with gradual dose titration.
HEMATOLOGICAL: Lowered vitamin B-12 levels, usually asymptomatic. There are
very rare cases of megaloblastic anemia.
THE ISSUE ABOUT LACTIC ACIDOSIS
Symptoms are vague: GI complaints, altered sensorium, tachypnea.
Incidence is about 0.03 cases/1000 patient-yrs of treatment
At highest risk are patients with decreased renal function who might accumulate the drug.
Do not use in patients with decreased renal function. Withhold in situations with
anticipated decreases in renal function: surgery, trauma, dehydration, use of
iodinated contrast media, excessive alcohol use.
Avoid use in patients with significant hepatic disease as lactic acid is cleared by the liver.
4. Dosing: Available in 500, 850 and 1,000 mg tablets. Start at either 500 BID or 850 QD.
With 500 mg tablets increase by one tablet every week until control is achieved or a maximum
2,500 mg dose is reached. With 850 mg tablets increase by one tablet every other week until
response or a maximum dose of 2,550 mg is reached. Higher doses are split. Also available in
SA tablets dosed QD/BID (Glucophage XR)
5. New formulations: Fixed combination with glyburide: Glucovance
N677 – SPRING 2011 – J. LOPEZ, PHARM.D. 6
Avandamet (metformin plus rosiglitazone)
6. Place in Therapy- Comparable glucose control to oral sulfonylureas. Positive metabolic
changes and no weight gain suggest best used in significantly overweight patients. Guidelines
recommend this drug for use in most type 2 patients as 1st drug.
Alpha Glucosidase Inhibitors-
Acarbose (Precose®)
1. Pharmacology- A reversible inhibitor of alpha glucosidase: slows down
breakdown of complex carbohydrates thereby preventing post-prandial glucose surge. Acarbose
works intraluminally; almost no drug is absorbed systemically.
2. Clinical Efficacy Summary- Achieves a 0.5-1% reduction in HgA1c
3. Adverse Effects and Other Cautions- Abdominal pain, diarrhea and flatulence are
common. These adverse effects are related to increased delivery of undigested carbohydrate to
the large colon. They tend to abate with time and are minimized by gradual titration.
Note that excessive intake of disaccharides will increase GI side effects. Maltose and sucrose
have a relatively fast transit time through the intestine and will reach the large colon where they
will be fermented by colonic bacteria. Gas and cramping will result. Advise patients to avoid
consuming concentrated sucrose (cake with frosting) and maltose (beer).
There is no risk of hypoglycemia from acarbose used alone. However, hypoglycemia
may develop during combination therapy with oral sulfonylureas. In these cases, it is important
to remind patients that plain glucose should be used to correct hypoglycemia. Sucrose (table
sugar) will not work fast enough because of the enzymatic inhibition with acarbose.
4. Dosing- Available in 50 and 100 mg tablets. Start with 25 mg (1/2) tablet TID
and increase at 4-8 week intervals using 1 hr postprandial glucose measurements as a guide. The
maximum recommended dose is 100 mg TID. Acarbose must be taken with the first bite of food
(start of the meal).
5. Place in Therapy- As an adjunct to dietary changes for type II diabetes mellitus.
Usefulness may be limited in some cases by non-serious but bothersome GI side effects.
Miglitol (Glyset)
1. Pharmacology- Reversible inhibitor of alpha glucosidases; slows down the
breakdown of complex carbohydrates thereby preventing postprandial glucose surge.
2. Clinical Efficacy Summary- In 2 US studies the postprandial glucose surge was
reduced by 63-66 mg/dl with a 50 mg TID dose. Hemoglobin A1c was reduced by 0.58 to
0.69%. Also studied in combination with sulfonylureas. Additional blood sugar lowering seen
with combination.
3. Adverse Effects and Other Cautions: Abdominal pain, diarrhea and flatulence
are common. Similar to acarbose. Same cautions.
The Miglitinides: Repaglinide (Prandin)
N677 – SPRING 2011 – J. LOPEZ, PHARM.D. 7
Pharmacology: Causes pancreatic beta cells to release insulin. While similar in effect to
sulfonylureas, it is more quickly acting and has a short duration of action. It is taken before
meals.
Clinical Efficacy Summary: As monotherapy lowers Hgb A1c by up to 1.9%. In comparison to
sulfonylureas it has approximately the same efficacy.
Adverse Effects: Hypoglycemia - relatively rare
Place in Therapy: as an alternative to sulfonylureas particularly for patients with significant
postprandial hyperglycemia
Phenylalanine derivative (similar to repaglinide)
Nateglinide (Starlix) - also used for postprandial hyperglycemia control
Typical dose is 120 mg tid just before meals
Thiazolidenediones (“Glitazones”)
1. Mechanism of Action: Partially reverses insulin resistance. Works at the level of
the nucleus by modifying gene expression and protein production.
2. Indications: Used in combination with sulfonylureas or metformin and as
monotherapy although the latter is generally not recommended at this time.
3. Clinical Efficacy Summary: Troglitazone was removed from the US market on
3/21/00.
Pioglitazone
Monotherapy: 0.3-1.6% decrease in Hgb A1c - greater effect in therapy naive
patients. Effects are sustained for at least 1 year.
Combination: Sulfonylurea + pioglitazone = 0.9 - 1.3% HgbA1c drop.
Metformin + pioglitazone = 0.8% drop in HgbA1c
Insulin + pioglitazone = 0.7 to 1.0% drop in HgbA1c
Rosiglitazone
Monotherapy: 0.3-0.7 decrease in HgbA1c; effects sustained for 1 yr.
Combination: Metformin + rosiglitazone = 0.6 to 0.8% decrease in Hgb A1c
4. Adverse Effects and Other Cautions:
Adverse effects during clinical trials:
Pioglitazone
Upper Respiratory Tract Infection 13 .2
Headache 9 .1
Sinusitis 6 .3
Myalgia 5 .4
N677 – SPRING 2011 – J. LOPEZ, PHARM.D. 8
Tooth Disorder 5 .3
Diabetes Mellitus Aggravated 5 .1
Pharyngitis 5 .1
Others: Increased intravascular volume, resumption or increase in fertility in women of child
bearing age.
Issues of hepatotoxicity:
Troglitazone: higher incidence (1.9% in LFT’s during studies, many reported cases of
hepatic failure). Removed from the US market for this reason.
Pioglitazone and Rosiglitazone have similar incidence of LFT elevation as placebo
during premarketing trials and thus far no clearly documented cases of hepatic failure.
Recommended monitoring: Every 2 months for the first year and the periodically thereafter.
Edema and heart failure: glitazones are now contraindicated.
The rosiglitazone (Avandia) scare of 2007; requirement for REMS in 2010
4. Dosing:
Pioglitazone: Monotherapy: 15-30 mg/day. Maximum 45 mg/day
Combination with metformin or sulfonylurea: use 15 - 30 mg and beware of need
to adjust doses of other antidiabetic medication.
Rosiglitazone: Monotherapy or combination with metformin: 4 mg/day. May increase to 8
mg/day.
Newer therapies for diabetes management:
Introduction to the amylin system
a. Incretin mimetics and insulin secretion signaling
N677 – SPRING 2011 – J. LOPEZ, PHARM.D. 9
b. GLP-1 and related compounds – basic pharmacology
Glucagon-like peptide 1 belongs to a group of hormones secreted by specialized
intestinal cells in response to a meal. Collectively termed incretins, they signal to the pancreas
prompting release of insulin and amylin
The activity of GLP-1 is terminated by dipeptidyl peptidase-4.
c. Exenatide (Byetta) and Luraglitide (Victoza)
Exenatide is a 39 amino acid peptide found in the salivary venom of the Gila
monster. It is a GLP-1 agonist but it is resistant to inactivation by DPP-IV.
Luraglitide is an analog of exenatide that is longer acting; injected once daily as
compared to exenatide twice daily.
Effects: enhanced insulin secretion, suppression of glucagons, slows gastric
emptying, decreased food intake and body weight.
d. Pramlintide (Symlin): synthetic amylin for type 1 DM
e. DDP4 inhibitors: Sitagliptin (Januvia) and Saxagliptin (Onglyza)
Indicated as monotherapy or in combination with metformin or glitazone
Efficacy summary: Lowers A1c by 0.5% – 0.9%
Dose: Sitagliptin100 mg once daily – reduce to 50 mg with moderate renal
dysfunction or 25 mg with severe renal dysfunction; saxagliptin 2.5 – 5 mg once daily – reduce to
2.5 mg daily with renal dysfunction.
Side effects to date: nonspecific URI, nasopharyngitis, headache.
Place in therapy?
Beyond the incretins
- Bromocriptine (Cycloset)
A dopamine receptor agonist that regulates blood glucose in type 2 diabetes. Exact mechanism of
action is unknown but it probably involves regulation of other hormones such as growth
hormone.
N677 – SPRING 2011 – J. LOPEZ, PHARM.D. 10
Available as 0.8 mg tablets given once in the morning. Target dose is 1.6 to 4.8 mg/day. A1c
response is rather small.
Place in therapy is unknown at this point.
- Coveselam: This is a lipid lowering drug; a bile acid binding resin
But, it has also received approval for type 2 diabetes. Mechanism of action is unknown but it
probably slows down carbohydrate absorption.
About a 0.5% reduction in A1c
Dose is 3 tablets BID or 6 QD
General Guidelines for management of type 2 diabetes
American Diabetes Association; published yearly. View at: http://www.diabetes.org; follow the
links to health professionals and click on practice guidelines
Therapeutic Considerations
1. Diabetes care encompasses more that hypoglycemic or antidiabetic drug therapy
a. Dietary/weight management
b. Glucose testing
c. Preventing end-organ damage
d. Comorbidity management (HTN, lipids, etc.)
2. The role of ACE inhibitors/ARB’s in diabetic renal disease. There is some
evidence ACE’s delay DM onset in pre-diabetes patients.
3. Recommendations for the use of aspirin in diabetics- consider for those with
significant CV risk defined as Framingham score of 10% or larger. (This is an important change
that began in 2010)
4. Lipid disorder management in diabetes – as in other patients but TG can be a
major issue. TG tend to correct as BG normalizes
5. Hypertension – target is 130/80 or better
Diabetes care – the big challenge for coordinated multidisciplinary care: Metformin is first
choice, then insulin or sulfidameria; after this use combos of those, then other tx’s
N677 – SPRING 2011 – J. LOPEZ, PHARM.D. 11
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- 2022 Diabetes Secrets by Michael T. McDermottDocument200 pages2022 Diabetes Secrets by Michael T. McDermottPeter Albeiro Falla Cortes100% (4)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Exercise Benefits for Diabetes ManagementDocument77 pagesExercise Benefits for Diabetes ManagementAkshay BangadPas encore d'évaluation
- Diabetes Drug Notes (2022)Document393 pagesDiabetes Drug Notes (2022)evansPas encore d'évaluation
- Treatment of Diabetes MellitusDocument31 pagesTreatment of Diabetes MellitusIrfan IdealistPas encore d'évaluation
- Monitoring side effects of octreotide acetateDocument32 pagesMonitoring side effects of octreotide acetatemelissamichellle100% (2)
- 190 - Gestational Diabetes Mellitus AgogDocument16 pages190 - Gestational Diabetes Mellitus Agogjorge vergara100% (2)
- Getting Started With Insulin InjectionsDocument4 pagesGetting Started With Insulin InjectionsJianhua ShiPas encore d'évaluation
- Quick Reference Guide - Management of Diabetes 1 2022 Version FINALDocument20 pagesQuick Reference Guide - Management of Diabetes 1 2022 Version FINALHigh Class Education (H.C.Education)Pas encore d'évaluation
- Severe Hypoglicemia: Is It Still A Threat For Children and Adolescent With Type 1 DiabetesDocument11 pagesSevere Hypoglicemia: Is It Still A Threat For Children and Adolescent With Type 1 DiabetesSultan Rahmat SeptianPas encore d'évaluation
- Adjustment of OHA During Fasting in RamadanDocument2 pagesAdjustment of OHA During Fasting in Ramadanhk.medicinesoptPas encore d'évaluation
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults: TreatmentDocument35 pagesDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults: TreatmentyorghiLPas encore d'évaluation
- An In-Depth Follow-Up of Healthcare in State Prisons (Report #2023-01)Document84 pagesAn In-Depth Follow-Up of Healthcare in State Prisons (Report #2023-01)Jeff ParrottPas encore d'évaluation
- Dietary Management in Diabetes: BackgroundDocument5 pagesDietary Management in Diabetes: BackgroundEnis SpahiuPas encore d'évaluation
- Simplify Insulin Therapy With Co-FormulationDocument26 pagesSimplify Insulin Therapy With Co-FormulationNatasha LaurentiaPas encore d'évaluation
- Diabetes Mellitus Indian PerspectiveDocument8 pagesDiabetes Mellitus Indian PerspectiveEditor IJTSRDPas encore d'évaluation
- Cannula Calculation-Learning Syringe-Olsen - ch7 PDFDocument33 pagesCannula Calculation-Learning Syringe-Olsen - ch7 PDFzainikamal1975Pas encore d'évaluation
- Pharmacology of Metabolic Drugs: Nurlaili SusantiDocument58 pagesPharmacology of Metabolic Drugs: Nurlaili Susantimillennia zulfaPas encore d'évaluation
- Ins Susp Vial PIL 5Document6 pagesIns Susp Vial PIL 5Kathleen Salvador-RamosPas encore d'évaluation
- Diabetes MellitusDocument75 pagesDiabetes MellitusIndika KarunamuniPas encore d'évaluation
- Dka Guidelines - 2012Document4 pagesDka Guidelines - 2012djizhieePas encore d'évaluation
- 19 Aug - 26 Aug, 2019: Pattern Snapshot For Daffa ArkanantaDocument9 pages19 Aug - 26 Aug, 2019: Pattern Snapshot For Daffa ArkanantaDaffa ArkanantaPas encore d'évaluation
- Design and Development of A Simulating Prototype Cost Effective Insulin Management SystemDocument3 pagesDesign and Development of A Simulating Prototype Cost Effective Insulin Management SystemRazan AlyahyaPas encore d'évaluation
- DM OHA and InsulinDocument33 pagesDM OHA and InsulinPraba NanthanPas encore d'évaluation
- Pharm Nursing Style Practice Questions Exam 4- Endocrine and Reproductive MedicationsDocument2 pagesPharm Nursing Style Practice Questions Exam 4- Endocrine and Reproductive MedicationsHwi GNDCPas encore d'évaluation
- The Basics of Diabetes: Phar 811 Peyton Teets Pharmd Candidate School of Pharmacy - West Virginia UniversityDocument39 pagesThe Basics of Diabetes: Phar 811 Peyton Teets Pharmd Candidate School of Pharmacy - West Virginia UniversityMa'rifatulAuliaPas encore d'évaluation
- Assessment of Insulin Injection Practice of Nurses Working inDocument7 pagesAssessment of Insulin Injection Practice of Nurses Working inBheru LalPas encore d'évaluation
- Type2dm PDFDocument3 pagesType2dm PDFapi-303065684Pas encore d'évaluation
- Inisiasi Insulin DR OctoDocument47 pagesInisiasi Insulin DR Octowulan nurmalasariPas encore d'évaluation
- Topic 3 EndoDocument3 pagesTopic 3 EndoAmol DullatPas encore d'évaluation
- Insulin Injection PDFDocument6 pagesInsulin Injection PDFAulia mulidaPas encore d'évaluation