Académique Documents
Professionnel Documents
Culture Documents
Abnormal Heart Rate Recovery After Maximal Cardiopulmonary
Transféré par
Arun PaulDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Abnormal Heart Rate Recovery After Maximal Cardiopulmonary
Transféré par
Arun PaulDroits d'auteur :
Formats disponibles
Clinical Endocrinology (2008) 68, 88–93 doi: 10.1111/j.1365-2265.2007.03004.
ORIGINAL ARTICLE
Abnormal heart rate recovery after maximal cardiopulmonary
Blackwell Publishing Ltd
exercise stress testing in young overweight women with
polycystic ovary syndrome
Francesco Giallauria*, Stefano Palomba†, Francesco Manguso§, Alessandra Vitelli*, Luigi Maresca*,
Domenico Tafuri¶, Gaetano Lombardi‡, Annamaria Colao‡, Carlo Vigorito* and Francesco Orio‡,**
*Department of Clinical Medicine, Cardiovascular and Immunological Sciences, Cardiac Rehabilitation Unit, University
‘Federico II’ of Naples, Naples, †Unit of Reproductive Medicine and Surgery, ‘Magna Graecia’ University of Catanzaro,
Catanzaro, ‡Department of Molecular & Clinical Endocrinology and Oncology, and §Department of Clinical and Experimental
Medicine, Gastroenterology Unit, University ‘Federico II’ of Naples, Naples, ¶Chair of Methods and Teaching of Sportive Activity,
Faculty of Exercise Sciences and **Department of Endocrinology, Faculty of Motor Science, University ‘Parthenope’ of Naples,
Naples, Italy
Introduction
Summary Polycystic ovary syndrome (PCOS) is a relatively common
Objective Heart rate recovery (HRR) is a measure derived from endocrine-metabolic disorder predominantly characterized by
exercise test, defined as the fall in heart rate during the first minute chronic anovulation, hyperandrogenism and insulin-resistance
after maximal exercise. Abnormal HRR is a measure of autonomic (IR).1,2
dysfunction associated with an increased mortality. This study was Heart rate recovery (HRR) is an easily obtained measure derived
performed to evaluate the HRR in polycystic ovary syndrome (PCOS). from exercise stress testing and is defined as the fall in heart rate
Design Prospective controlled clinical study. during the first minute after maximal exercise.3 HRR is a marker of
Patients Seventy-five PCOS women compared to 75 healthy women autonomic function and is directly correlated to parasympathetic
matched for age (21·7 ± 2·1 years vs. 21·9 ± 1·8 years, respectively) activity. Abnormal HRR is an independent cardiovascular risk
and body mass index (BMI) (29·0 ± 2·6 kg/m2 vs. 29·1 ± 2·9 kg/m2, (CVR) factor4 and a powerful predictor of all-cause mortality in
respectively). patients with or without coronary artery disease.5–8
Measurements Subjects were studied for their hormonal and PCOS is a multifaceted syndrome associated with a wide range of
metabolic profile, and underwent cardiopulmonary exercise test (CPX). cardiovascular risk (CVR) factors including dyslipidaemia, hyper-
Results PCOS women showed a significantly reduced HRR tension, glucose intolerance and diabetes.9 Although IR is not a key
(12·9 ± 1·8 vs. 20·4 ± 3·1 beats/min, P < 0·001) compared to healthy factor to diagnose PCOS,10 it is clearly documented that subjects
controls, an impairment in maximal oxygen consumption affected by this syndrome are more insulin resistant than healthy
(18·0 ± 2·3 ml/kg/min vs. 29·3 ± 3·9 ml/kg/min) and in oxygen women, even taking into account body weight.2
consumption at anaerobic threshold (13·6 ± 2·6 ml/kg/min vs. Moreover, in a large cohort of PCOS women, we recently
24·2 ± 3·0 ml/kg/min). In PCOS women, abnormal HRR was documented an IR-related impairment of cardiopulmonary
inversely correlated to BMI (r = −0·582, P < 0·001) and to the area functional capacity compared to age- and body mass index (BMI)-
under the curve for insulin (r = −0·596, P < 0·001). matched healthy women.11
Conclusions Our data demonstrate an abnormal HRR after Even if no increased mortality for cardiovascular disease (CVD)
maximal CPX in young overweight PCOS patients, and that HRR has yet been demonstrated in PCOS,12 several observations suggest
should be investigated as a further potential marker of increased that subjects affected by this syndrome show a complex mixture of
cardiovascular risk in PCOS. risk factors that may predispose to an elevated CVR.13–15
Abnormal autonomic function as evaluated by HRR is strongly
(Received 2 April 2007; returned for revision 22 April 2007; finally associated with elevated fasting plasma glucose levels16 and with
revised 24 May 2007; accepted 22 June 2007) diabetes.17 It has also been reported that in diabetic patients, an
abnormal HRR was independently predictive of cardiovascular and
all-cause deaths.18
Correspondence: Francesco Orio, Faculty of Exercise Sciences, University of
To date, there are no data available regarding autonomic function
Naples ‘Parthenope’, Naples and Department of Molecular & Clinical
Endocrinology and Oncology, University of Naples ‘Federico II’, Via S. assessment in PCOS. Therefore, this study was aimed at evaluating
Pansini 5, 80131 Naples, Italy. Tel: +39 3477676883; Fax: +39 0892574878; autonomic function as determined by end-exercise HRR in PCOS
E-mail: francescoorio@virgilio.it patients compared to healthy young controls.
© 2007 The Authors
88 Journal compilation © 2007 Blackwell Publishing Ltd
Heart rate recovery in PCOS 89
the University of Naples ‘Federico II’ approved the study protocol.
Subjects and methods
The purpose of the protocol was explained to each subject, and written
informed consent was obtained from each patient before the start
Subjects
of the study.
Seventy-five consecutive young nonsmoking PCOS patients were
enrolled in the study protocol. All the PCOS patients achieved the
Biochemical assays
European Society for Human Reproduction and Embryology/
American Society for Reproductive Medicine criteria for the All blood samples were obtained in the morning between 08·00 h
diagnosis of PCOS.2 and 09·00 h after an overnight fasting during the early follicular
Polycystic ovaries were identified by transvaginal (TV) or pelvic phase (2nd–4th day) of progesterone (P)-induced menstrual cycle.
ultrasonography (USG) examination and hirsutism by Ferriman- Blood samples were collected into tubes containing EDTA after a
Gallwey (FG) score > 8 and an elevated total testosterone (normal 30-min resting period in the supine position. All blood samples were
range < 2·0 nmol/l) levels. immediately centrifuged at 4 °C for 20 min at 1600 g and stored at
Exclusion criteria included pregnancy, glucose intolerance [as –20 °C until assayed.
screened by a 2-h oral glucose tolerance test (OGTT)] and diabetes, Plasma LH, FSH, prolactin (PRL), oestradiol (E2), P, 17α-
hypothyroidism, hyperprolactinaemia, Cushing’s syndrome, hydroxyprogesterone (17-OH-P), T, androstenedione (A) and
nonclassical congenital adrenal hyperplasia, and use of oral con- DHEAS levels were measured by specific radioimmunoassays (RIA)
traceptives, glucocorticoids, antiandrogens, ovulation induction as previously described.13,14 The levels of SHBG were measured using
agents, and antipsychotic, antidiabetic or antiobesity drugs, or other an immunoradiometric assay (IRMA)7,8 and the free androgen index
hormonal drugs within the previous 6 months. Subjects with was calculated [T (nmol/l)/SHBG (nmol/l) × 100]. Blood insulin
neoplastic, hepatic, respiratory and any cardiovascular disorder or and glucose levels were measured by a solid-phase chemiluminescent
other concurrent medical illness (i.e. heart failure, lung or renal enzyme immunoassay and the glucose oxidase method, respectively.13,14
disease) were also excluded from the study. The glucose and insulin area under curve (AUC), and the AUCGLU/
21
Another 75 healthy age- and BMI-matched women acted as controls. AUCINS ratio in response to the OGTT were also calculated.
Each control was defined as age- and BMI-matched with PCOS case Haemochrome analysis was performed according to standard
when the differences between the case and control was < 2 years and evaluation. C-reactive protein (CRP) was measured as recently
< 1 kg/m2 for age and BMI, respectively. The healthy state of the described.22
controls was determined by medical history, physical and pelvic
examination, and complete blood chemistry. Their normal ovula-
Cardiopulmonary exercise test
tory state was confirmed by transvaginal ultrasonography (TV-USG)
and plasma progesterone (P) assay. Both procedures were performed PCOS and healthy control women underwent a symptom-limited
during the luteal phase of the menstrual cycle (7 days before the CPX with Bruce treadmill protocol.23 Heart rate and blood pressure
expected menses). The presence of fluid in the cul-de-sac at TV-USG at baseline and peak exercise, heart rate 1 min into a walking
and a plasma P assay greater than 31·8 nmol/l (> 10 ng/ml) were cool-down period (1·7 mph at 0% grade), and treadmill speed and
considered criteria for ovulation having occurred.19 grade at peak exercise were recorded.
None of the subjects (PCOS and controls) drank alcoholic HRR was calculated as the difference between heart rate at peak
beverages. exercise and heart rate after the first minute (HRR) of the cool-down
period. Abnormal HRR was defined as ≤ 18 beats/min3 for standard
exercise testing.
Study protocol
Both PCOS and healthy women underwent two cardiopulmonary
A common core of assessments was performed at enrolment: blood exercise stress tests at maximal interval of 3 days and in the same
sampling for a hormonal assessment, lipid profile, and fasting conditions. Short-term test-retest concordance of HRR values was
glucose and insulin levels (see below). During the same visit, all assessed for individual patients. The coefficient of variation (CV)
subjects underwent cardiovascular and endocrinological examination, between test-retest HRR values was less than 5%. Respiratory gas
12-lead electrocardiography, TV-USG, cardiopulmonary exercise exchange measurements were obtained breath-by-breath with use of
test (CPX), anthropometric measurements such as height, weight, a computerized metabolic cart (Vmax 29C, Sensormedics, Yorba
BMI (ratio between the weight and the square of the height) and Linda, CA) as previously described.24
waist to hip ratio (WHR, ratio between the smallest circumference
at the torso and the widest circumference at the hip), and completed
Statistical analysis
a leisure-time physical activity (LTPA) questionnaire (No, Low,
Moderate, High).20 2
Pearson χ -test was used for categorical data. Continuous data are
All clinical assessments were performed by the same physician expressed as mean ± SD. The unpaired Student’s t-test was used to
who was blinded to the patient condition. All study procedures were compare the two groups. Bivariate correlations computing Pearson’s
completed under the same conditions. coefficient with their significance levels were calculated between
The study was conducted according to the guidelines of the HRR and other variables. In PCOS women as well as in controls,
Declaration of Helsinki, and the Institutional Ethical Committee of multiple linear regression analysis (stepwise method) was performed
© 2007 The Authors
Journal compilation © 2007 Blackwell Publishing Ltd, Clinical Endocrinology, 68, 88–93
90 F. Giallauria et al.
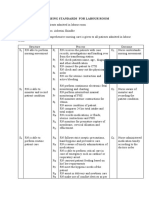
Table 1. Clinical and hormonal profile in polycystic ovary syndrome (PCOS) Table 2. Anthropometrical, metabolic and cardiovascular risk profile of
women and healthy controls polycystic ovary syndrome (PCOS) women and healthy controls
PCOS Controls PCOS Controls
(N = 75) (N = 75) P-value (N = 75) (N = 75) P-value
Age (years) 21·7 ± 2·1 21·9 ± 1·8 0·503 Fasting glucose (mmol/l) 5·18 ± 0·30 5·25 ± 0·34 0·226
BMI (kg/m2) 29·0 ± 2·6 29·1 ± 2·9 0·753 Fasting insulin (mU/l) 19·8 ± 3·3 12·3 ± 2·1 < 0·001
WHR 0·87 ± 0·3 0·85 ± 0·2 0·599 AUCGLU 12 001 ± 2166 11 687 ± 1786 0·290
Ferriman-Gallwey score 13·1 ± 4·1 4·2 ± 1·3 < 0·001 AUCINS 16 661 ± 837 3748 ± 240 < 0·001
FSH (IU/l) 11·5 ± 4·9 11·0 ± 4·7 0·499 AUCGLU/AUCINS ratio 0·72 ± 0·1 3·1 ± 0·5 < 0·001
LH (IU/l) 25·8 ± 8·5 12·8 ± 10·7 < 0·001 CRP (mg/l) 1·81 ± 0·7 0·61 ± 0·3 < 0·001
PRL (mU/l) 216 ± 50 206 ± 34 0·118 Hb (g/dl) 13·3 ± 0·8 13·1 ± 1·0 0·603
E2 (pmol/l) 122·8 ± 69·7 117·9 ± 49·3 0·595
P (nmol/l) 1·4 ± 0·3 1·9 ± 0·4 < 0·001 Data expressed as mean ± standard deviation.
17-OHP (nmol/l) 1·8 ± 0·7 0·9 ± 0·5 < 0·001 AUCGLU, area under curve for glucose; AUCINS, area under curve for insulin;
T (nmol/l) 2·5 ± 1·0 0·8 ± 0·7 < 0·001 AUCGLU/AUCINS, glucose/insulin area under curve ratio; BMI, body mass
A (nmol/l) 5·7 ± 2·8 1·8 ± 0·5 < 0·001 index; CRP, C-reactive protein; Hb, haemoglobin.
DHEAS (μmol/l) 4209 ± 985 2867 ± 754 < 0·001
SHBG (nmol/l) 25·0 ± 6·8 38·7 ± 5·4 < 0·001
FAI 9·8 ± 4·8 2·3 ± 1·0 < 0·001 Table 3. Cardiopulmonary exercise test parameters in polycystic ovary
syndrome (PCOS) women and healthy controls
Data expressed as mean ± standard deviation.
A, androstenedione; BMI, body mass index; DHEAS, PCOS Controls
dehydroepiandrosterone sulphate; E2, oestradiol; FAI, free androgen index; (N = 75) (N = 75) P-value
PRL, prolactin (1 μg/l = 20 mU/l); T, testosterone; WHR, waist to hip ratio;
17-OHP, 17-hydroxyprogesterone.
VO2max (ml/kg/min) 18·0 ± 2·3 29·3 ± 3·9 < 0·001
VO2AT (ml/kg/min) 13·6 ± 2·6 24·2 ± 3·0 < 0·001
VE/VCO2slope 28·2 ± 4·7 28·6 ± 5·4 0·594
to test a relationship between HRR as dependent variable and age, RER 1·08 ± 0·04 1·09 ± 0·06 0·810
HRrest (beats/min) 77·4 ± 4·9 77·5 ± 4·3 0·872
BMI, VO2max, AUCINS, AUCGLU/AUCINS ratio as independent
HRpeak (beats/min) 146·3 ± 13·7 147·4 ± 13·8 0·582
variables. Moreover, we performed another multiple linear regression
SBPrest (mmHg) 118·9 ± 9·6 120·8 ± 8·4 0·147
analysis (stepwise method) pooling the data of PCOS and control SBPpeak (mmHg) 166·6 ± 8·2 167·5 ± 8·8 0·459
subjects using HRR as dependent variable and age, BMI, VO2max, DBPrest (mmHg) 76·1 ± 4·7 75·7 ± 4·9 0·494
AUCINS, and AUCGLU/AUCINS ratio, together with PCOS as a factorial DBPpeak (mmHg) 85·3 ± 4·1 85·8 ± 3·6 0·422
variable (Controls/PCOS coded 0/1). In assessing the suitability of HRR (beats/min) 12·9 ± 1·8 20·4 ± 3·1 < 0·001
the data for linear regression models, the collinearity diagnostics
were evaluated. All tests of significance were two-sided. A P- Data expressed as mean ± standard deviation.
value ≤ 0·05 was considered as significant. SPSS software for DBPpeak, diastolic blood pressure at peak exercise; DBPrest, diastolic blood
pressure at rest; VO2max, maximal oxygen consumption; VO2AT, oxygen
Windows (release 15·0·0, SPSS Inc, Chicago, IL) was used for
consumption at anaerobic threshold; VE, ventilation; VCO2, carbon dioxide
statistical analysis. production (l/min); RER, respiratory exchange ratio; HRrest, heart rate at rest;
HRpeak, heart rate at peak exercise; SBPrest, systolic blood pressure at rest;
SBPpeak, systolic blood pressure at peak exercise; HRR, heart rate recovery at
Results the first minute after maximal exercise.
Clinical and hormonal profiles of the study population are presented
in Table 1. The groups were closely matched for age and BMI. All
PCOS patients showed a significant difference (P < 0·001) in FG concentrations were significantly increased (P < 0·001) in PCOS
score LH, P, 17OH-P, T, A, DHEA-S, SHBG and FAI when compared women compared to the control group.
to the control group (Table 1). Baseline cardiopulmonary exercise stress test parameters are
All PCOS patients (100%) showed polycystic ovaries and summarized in Table 3.
anovulation, 66 (88%) had clinical and 51 (68%) biochemical In PCOS women, we observed a significant impairment in VO2max
hyperandrogenism. (18·0 ± 2·3 ml/kg/min vs. 29·3 ± 3·9 ml/kg/min, P < 0·001) and
Anthropometrical, metabolic and CVR profiles of PCOS and VO2AT (13·6 ± 2·6 ml/kg/min vs. 24·2 ± 3·0 ml/kg/min) and an
control groups are summarized in Table 2. No difference was abnormal HRR (12·9 ± 1·8 beats/min vs. 20·4 ± 3·1 beats/min)
detected in fasting glucose and AUCGLU whereas fasting insulin levels compared to the healthy control group. In PCOS women, abnormal
and AUCINS were significantly higher (P < 0·001) in PCOS than control HRR is inversely correlated to BMI (r = −0·582, P < 0·001) (Fig. 1)
women (Table 2). AUCGLU/AUCINS ratio was also significantly lower and to AUCINS (r = −0·596, P < 0·001) (Fig. 2). No significant difference
(P < 0·001) in PCOS women compared to the control group. CRP was observed in resting and peak exercise heart rate (HR), systolic
© 2007 The Authors
Journal compilation © 2007 Blackwell Publishing Ltd, Clinical Endocrinology, 68, 88–93
Heart rate recovery in PCOS 91
Table 4. Leisure time physical activity (LTPA) levels in polycystic ovary
syndrome (PCOS) women and healthy controls
PCOS Controls
(N = 75) (N = 75) P-value
LTPA, N (%) 0·979
No 26 (35) 26 (35)
Low 22 (29) 24 (32)
Moderate 20 (27) 19 (25)
High 7 (9) 6 (8)
Discussion
Fig. 1 Correlation between baseline values of body mass index (BMI) and The rapid deceleration of heart rate immediately following exercise
heart rate recovery (HRR) in young polycystic ovary syndrome (PCOS)
is regulated by various intrinsic, neural and humoral factors.
women.
However, autonomic nervous system responses, in particular
parasympathetic reactivation, are a major determinant of HRR.25,26
Slower HRR may therefore be indicative of decreased parasympathetic
responsiveness.27
In healthy subjects, HRR has been shown to be inversely associated
to IR and other risk factors that tend to cluster with IR, such as BMI,
abdominal obesity, low HDL-cholesterol28 and triglyceride/
HDL-cholesterol ratio.29
Although IR is not a criterion to diagnose PCOS,2 it is well
known30 that PCOS subjects are more insulin resistant than healthy
women independently of their body weight. In the present study,
an abnormal HRR is shown in PCOS patients when compared to
healthy controls and this alteration is significantly correlated to BMI
and markers of IR, suggesting a close and complex relationship
between autonomic function and glucose metabolism in young
overweight PCOS women. Furthermore, PCOS is probably only
linked to HRR via IR.
Fig. 2 Correlation between baseline values of the area under the curve for
insulin (AUCINS) and heart rate recovery (HRR) in young polycystic ovary This study also highlights the cardiopulmonary impairment
syndrome (PCOS) women. observed in young PCOS women.11,24 Maximal oxygen consumption
represents a validated index for assessing cardiovascular functional
capacity31 and it is also considered a strong determinant of the
blood pressure (SBP) and diastolic blood pressure (DBP) between insulin sensitivity index in both men and women.32
PCOS and control group (Table 3). Abnormal HRR following exercise has been linked to the Metabolic
In PCOS patients, multiple linear regression analysis showed a Syndrome and to several of its components in cross-sectional
significant inverse relationship between HRR, our dependent variable studies.16,28,29,33,34 Recently, Kizilbash et al.35 observed that abnormal
and BMI [unstandardized coefficient (B) ± SE, –0·057 ± 0·018, HRR does not precede development of the Metabolic Syndrome,
standardized coefficient (β) –0·087, P = 0·002], AUCINS (B but appears after syndrome components are present, probably playing
0·000 ± 0·000, β –0·137, P < 0·001), and a direct relationship with a role in increasing cardiovascular diseases (CVD) morbidity and
VO2max (B 0·121 ± 0·051, β 0·156, P = 0·02) and AUCGLU/AUCINS mortality.
ratio (B 10·239 ± 1·052, β 0·698, P < 0·001), with a constant of 9·805. Our data suggest that IR leads to a reduced cardiopulmonary
No other parameter showed a relationship to HRR. Pooling together functional capacity (as expressed by a reduced VO2max) and to
data from PCOS and control subjects, multiple linear regression autonomic dysfunction (as expressed by an abnormal HRR) that
analysis showed a significant inverse relationship between HRR and may be responsible for the increased CVR profile in PCOS women.
AUCINS (B –0·001 ± 0·000, β –1·371, P = 0·003) and a direct relation- In women referred for cardiac rehabilitation, Kavanagh et al.36
ship with VO2max (B 0·162 ± 0·059, β 0·228, P = 0·007), AUCGLU/ reported that oxygen consumption was a strong independent
AUCINS ratio (B 1·301 ± 0·531, β 0·359, P = 0·015) and PCOS status predictor of cardiac mortality and that each increase of 1 ml/kg/min
(B 9·642 ± 3·907, β 1·069, P = 0·015), with a constant of 15·243. of initial maximal oxygen consumption was associated with a 10%
No significant differences between PCOS patients and healthy lower cardiac mortality. Although these results refer to women with
controls were observed in LTPA level (Table 4). proven coronary artery disease, the study have confirmed the
© 2007 The Authors
Journal compilation © 2007 Blackwell Publishing Ltd, Clinical Endocrinology, 68, 88–93
92 F. Giallauria et al.
powerful prognostic significance of maximal oxygen consumption 10 Dunaif, A. (1995) Hyperandrogenic anovulation (PCOS): a unique
also in subjects of both sexes without CVD.37 Therefore, we believe disorder of insulin action associated with an increased risk of
that these results can be extended also to our young PCOS women non-insulin-dependent diabetes mellitus. American Journal of
if we take into consideration their long-term risk. Medicine, 98, 33S – 39S.
11 Orio, F. Jr, Palomba, S., Giallauria, F., Colao, A. & Vigorito, C. (2007)
Abnormal HRR also represents a powerful independent predictor
Impaired cardiopulmonary parameters in young women with
of cardiovascular and all-cause mortality in healthy adults.12–15
polycystic ovary syndrome. Clinical Endocrinology, 66, 152 –153.
Therefore, it appears that the abnormal HRR after maximal exercise
12 Pierpoint, T., McKeigue, P.M., Isaacs, A.J., Wild, S.H. & Jacobs, H.S.
could be used as an outcome tool that could help to identify patients (1998) Mortality of women with polycystic ovary syndrome at
at increased risk for cardiovascular event. long-term follow-up. Journal of Clinical Epidemiology, 51, 581– 586.
Further studies will be necessary to extend our results to a larger 13 Orio, F. Jr, Palomba, S., Spinelli, L., Cascella, T., Tauchmanovà, L.,
and older PCOS women population and long-term follow-up studies Zullo, F., Lombardi, G. & Colao, A. (2004) The cardiovascular risk
are required in order to evaluate if an improvement of autonomic of young women with polycystic ovary syndrome: an observational,
function per se and/or cardiopulmonary function could represent a analytical, prospective case-control study. Journal of Clinical
protective factor for reducing CVR in PCOS women. Moreover, Endocrinology and Metabolism, 89, 3696 – 3671.
adding data on visceral fat mass [i.e. dual energy X-ray absorptiometry 14 Orio, F. Jr, Palomba, S., Cascella, T., De Simone, B., Di Biase, S.,
Russo, T., Labella, D., Zullo, F., Lombardi, G. & Colao, A. (2004)
(DEXA) measurements] might help to explain the marked differences
Early impairment of endothelial structure and function in young
in VO2max and HRR in PCOS.
normal-weight women with polycystic ovary syndrome. Journal of
In conclusion, PCOS seems to be characterized by several
Clinical Endocrinology and Metabolism, 89, 4588 – 4593.
alterations that could increase the risk for CVD. Among these factors, 15 Orio, F., Palomba, S. & Colao, A. (2006) Cardiovascular risk in
cardiopulmonary impairment and abnormal HRR should be women with polycystic ovary syndrome. Fertility and Sterility, 86,
considered as further markers of cardiovascular risk. S20 – S21.
16 Panzer, C., Lauer, M.S., Brieke, A., Blackstone, E. & Hoogwerf, B.
(2002) Association of fasting plasma glucose with heart rate recovery
References
in healthy adults. Diabetes, 51, 803 – 807.
1 Azziz, R., Marin, C., Hoq, L., Badamgarav, E. & Song, P. (2005) 17 Seshadri, N., Acharya, N. & Lauer, M.S. (2003) Association of
Healthcare-related economic burden of the polycystic ovary syndrome diabetes mellitus with abnormal heart rate recovery in patients
(PCOS) during the reproductive lifespan. Journal of Clinical without known coronary artery disease. American Journal of
Endocrinology and Metabolism, 90, 4650 – 4658. Cardiology, 91, 108 –111.
2 Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop 18 Cheng, Y.J., Lauer, M.S., Earnest, C.P., Church, T.S., Kampert, J.B.,
Group. (2004) Revised 2003 consensus on diagnostic criteria and Gibbons, L.W. & Blair, S.N. (2003) (2003) Heart rate recovery
long-term health risks related to polycystic ovary syndrome. Fertility following maximal exercise testing as a predictor of cardiovascular
and Sterility, 81, 19 – 25. disease and all-cause mortality in men with diabetes. Diabetes Care,
3 Shetler, K., Marcus, R., Froelicher, V.F., Vora, S., Kalisetti, D., 26, 2052 – 2057.
Prakash, M., Do, D. & Myers, J. (2001) Heart rate recovery: validation 19 Barbieri, R.L. (1999) Infertility. In: S.S.C. Yen, R.B. Yaffe, R.L.
and methogologic issues. Journal of the American College of Cardiology, Barbieri, eds. Reproductive Endocrinology: Physiology, Pathophysiology,
38, 1980 – 87. and Clinical Management, 4th edn. W.B. Saunders, Philadelphia,
4 Kravariti, M., Naka, K.K., Kalantaridou, S.N., Kazakos, N., 562 – 593.
Katsouras, C.S., Makrigiannakis, A., Paraskevaidis, E.A., Chrousos, 20 Roeykens, J., Rogers, R., Meeusen, R., Magnus, L., Borms, J. & de
G.P., Tsatsoulis, A. & Michalis, L.K. (2005) Predictors of endothelial Meirleir, K. (1998) Validity and reliability in a Flemish population
dysfunction in young women with polycystic ovary syndrome. of the WHO-MONICA Optional Study of Physical Activity
Journal of Clinical Endocrinology and Metabolism, 90, 5088 – 5095. Questionnaire. Medicine and Science in Sports and Exercise, 30, 1071–
5 Cole, C.R., Foody, J.M., Blackstone, E.H. & Lauer, M.S. (2000) Heart 1075.
rate recovery after submaximal exercise testing as a predictor of 21 Tai, M.M. (1994) A mathematic model for the determination of total
mortality in a cardiovascular healthy cohort. Annals of Internal area under glucose tolerance and other metabolic curves. Diabetes
Medicine, 132, 552 – 555. Care, 17, 152 –154.
6 Cole, C.R., Blackstone, E.H., Pashkow, F.J., Snader, C.E. & Lauer, M.S. 22 Orio, F. Jr, Palomba, S., Cascella, T., Di Biase, S., Manguso, F.,
(1993) Heart-rate recovery immediately after exercise as a predictor Tauchmanovà, L., Nardo, L.G., Labella, D., Savastano, S., Russo, T.,
of mortality. New England Journal of Medicine, 341, 1351–1357. Zullo, F., Colao, A. & Lombardi, G. (2005) The increase of leukocytes
7 Nishime, E.O., Cole, C.R., Blackstone, E.H., Pashkow, F.J. & Lauer, M.S. as a new putative marker of low-grade chronic inflammation and
(2000) Heart rate recovery and treadmill exercise score as predictors early cardiovascular risk in polycystic ovary syndrome. Journal of
of mortality in patients referred for exercise ECG. Journal of the Clinical Endocrinology and Metabolism, 90, 2 – 5.
American Medical Association, 284, 1392 –1398. 23 Weber, C.T., Janicki, J.S. & McElroy, P.A. (1986) Cardiopulmonary
8 Vivekananthan, D.P., Blackstone, E.H., Pothier, C.E. & Lauer, M.S. Exercise Testing (CPX). In: C.T. Weber, J.S. Janicki, eds. Cardiopulmo-
(2003) Heart rate recovery after exercise is a predictor of mortality, nary Exercise Testing. W.B. Saunders, Philadelphia, 151–167.
independent of the angiographic severity of coronary disease. Journal 24 Orio, F., Giallauria, F., Palomba, S., Cascella, T., Manguso, F., Vuolo, L.,
of the American College of Cardiology, 42, 831– 838. Russo, T., Lombardi, G., Colao, A. & Vigorito, C. (2006) Cardio-
9 De Fronzo, R. & Ferranini, E. (1991) Insulin resistance: a multifaceted pulmonary impairment in young women with polycystic ovary
responsible for NIDDM, obesity, hypertension, dyslipidemia and syndrome. Journal of Clinical Endocrinology and Metabolism, 91,
atherosclerotic cardiovascular disease. Diabetes Care, 14, 173 –194. 2967 – 2971.
© 2007 The Authors
Journal compilation © 2007 Blackwell Publishing Ltd, Clinical Endocrinology, 68, 88–93
Heart rate recovery in PCOS 93
25 Imai, K., Sato, H., Hori, M., Kusuoka, H., Ozaki, H., Yokoyama, H., 32 Clausen, J.O., Borch-Johnsen, K., Ibsen, H. & Pedersen, O. (1996)
Takeda, H., Inoue, M. & Kamada, T. (2004) Vagally mediated heart Insulin sensitivity index, acute insulin response, and glucose
rate recovery after exercise is accelerated in athletes but blunted in effectiveness in a population-based sample of 380 young healthy
patients with chronic heart failure. Journal of the American College Caucasians: analysis of the impact of gender, body fat, physical
of Cardiology, 24, 1529 –1535. fitness, and life-style factors. Journal of Clinical Investigation, 98,
26 Pierpont, G.L. & Voth, E.J. (2004) Assessing autonomic function by 1195 –1209.
analysis of heart rate recovery from exercise in healthy subjects. 33 Spies, C., Otte, C., Kanaya, A., Pipkin, S.S., Schiller, N.B. & Whooley, M.A.
American Journal of Cardiology, 94, 64 – 68. (2005) Association of metabolic syndrome with exercise capacity and
27 Pierpont, G.L., Stolpman, D.R. & Gormick, C.C. (2000) Heart rate heart rate recovery in patients with coronary heart disease in the
recovery post-exercise as an index of parasympathetic activity. heart and soul study. American Journal of Cardiology, 95, 1175 –1179.
Journal of the Autonomic Nervous System, 80, 169 –174. 34 Carnethon, M.R., Jacobs, D.R. Jr, Sidney, S. & Liu, K. (2003)
28 Lind, L. & Andren, B. (2002) Heart rate recovery after exercise is Influence of autonomic nervous system dysfunction on the devel-
related to the insulin resistance syndrome and heart rate variability opment of type 2 diabetes: the CARDIA study. Diabetes Care, 26,
in elderly men. American Heart Journal, 144, 666 – 672. 3035 – 3041.
29 Shishehbor, M.H., Hoogwerf, B.J. & Lauer, M.S. (2004) Association 35 Kizilbash, M.A., Carnethon, M.R., Chan, C., Jacobs, D.R., Sidney, S.
of triglyceride-to-HDL cholesterol ratio with heart rate recovery. & Liu, K. (2006) The temporal relationship between heart rate
Diabetes Care, 27, 936 – 941. recovery immediately after exercise and the metabolic syndrome: the
30 Dunaif, A. (1997) Insulin resistance and the polycystic ovary CARDIA study. European Heart Journal, 27, 1592 –1596.
syndrome: mechanism and implications for pathogenesis. Endocrine 36 Kavanagh, T., Mertens, D.J., Hamm, L.F., Beyene, J., Kennedy, J.,
Reviews, 18, 774 – 800. Corey, P. & Shephard, R.J. (2003) Peak oxygen intake and cardiac
31 Fleg, J.L., Pina, I.L., Balady, G.J., Chaitman, B.R., Fletcher, B., Lavie, C., mortality in women referred for cardiac rehabilitation. Journal of the
Limacher, M.C., Stein, R.A., Williams, M. & Bazzarre, T. (2000) American College of Cardiology, 42, 2139 – 2143.
Assessment of functional capacity in clinical and research applications: 37 La Monte, M.J., Barlow, C.E., Jurca, R., Kampert, J.B., Church, T.S.
an advisory from the Committee on Exercise, Rehabilitation, and & Blair, S.N. (2005) Cardiorespiratory fitness is inversely associated
Prevention, Council on Clinical Cardiology, American Heart with the incidence of metabolic syndrome: a prospective study of
Association. Circulation, 102, 1591–1597. men and women. Circulation, 112, 505 – 512.
© 2007 The Authors
Journal compilation © 2007 Blackwell Publishing Ltd, Clinical Endocrinology, 68, 88–93
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- UabDocument20 pagesUabAnonymous n7RT07fzUdPas encore d'évaluation
- Sample Birthing PlanDocument2 pagesSample Birthing PlanChuohPas encore d'évaluation
- ATT Induced Hepatotoxicity: Dr. K. K. SharmaDocument36 pagesATT Induced Hepatotoxicity: Dr. K. K. SharmaSucharita Ray100% (1)
- History and P.E. of The Integumentary SystemDocument6 pagesHistory and P.E. of The Integumentary SystempazucenaPas encore d'évaluation
- Geistlich Bio-Oss Collagen and Geistlich Bio-Gide in Extraction SocketsDocument6 pagesGeistlich Bio-Oss Collagen and Geistlich Bio-Gide in Extraction SocketsErdeli StefaniaPas encore d'évaluation
- History, Diagnosis and Treatment Planning in Removable Partial DenturesDocument96 pagesHistory, Diagnosis and Treatment Planning in Removable Partial DenturesPriya BagalPas encore d'évaluation
- Restraints Assignment on Definitions, Types, Indications and Nurses RoleDocument8 pagesRestraints Assignment on Definitions, Types, Indications and Nurses RolemacmohitPas encore d'évaluation
- Probiotics vs Prebiotics: Differences, Advantages, TrendsDocument5 pagesProbiotics vs Prebiotics: Differences, Advantages, TrendsNaevisweloveuPas encore d'évaluation
- Answer Sheet For Module 6: Pauline P. Dela CruzDocument4 pagesAnswer Sheet For Module 6: Pauline P. Dela CruzPauline PascuaDPas encore d'évaluation
- Lowering Blood Pressure GuideDocument11 pagesLowering Blood Pressure GuideHilma NadzifaPas encore d'évaluation
- Strategi RS Dalam Pemenuhan Dan Pengaturan SDM CompressedDocument37 pagesStrategi RS Dalam Pemenuhan Dan Pengaturan SDM CompressedLilik SeptiyaPas encore d'évaluation
- Child Abuse and NeglectDocument89 pagesChild Abuse and NeglectdrvarshaPas encore d'évaluation
- Methods For The Euthanasia of Dogs and Cats - EnglishDocument28 pagesMethods For The Euthanasia of Dogs and Cats - Englishapi-266985430Pas encore d'évaluation
- Nursing Standards for Labour RoomDocument3 pagesNursing Standards for Labour RoomRenita ChrisPas encore d'évaluation
- 328 IndexDocument29 pages328 IndexDafi SanPas encore d'évaluation
- Prescribing Information: 1. Name of The Medicinal ProductDocument5 pagesPrescribing Information: 1. Name of The Medicinal Productddandan_20% (1)
- Hipopresivos y Dolor Lumbar Cronico 2021Document9 pagesHipopresivos y Dolor Lumbar Cronico 2021klgarivasPas encore d'évaluation
- Eliminate Papillomas and Warts at Home in 1 Treatment Course - PapiSTOP® PHDocument9 pagesEliminate Papillomas and Warts at Home in 1 Treatment Course - PapiSTOP® PHkiratuz1998Pas encore d'évaluation
- Research Paper Brianna BartonDocument11 pagesResearch Paper Brianna Bartonapi-530899175Pas encore d'évaluation
- Chapter 38 - Pediatric and Geriatric HematologyDocument3 pagesChapter 38 - Pediatric and Geriatric HematologyNathaniel Sim100% (2)
- Complications After CXLDocument3 pagesComplications After CXLDr. Jérôme C. VryghemPas encore d'évaluation
- Nursing Diagnosis and Plan of Care for Anemia with Chronic DiseaseDocument6 pagesNursing Diagnosis and Plan of Care for Anemia with Chronic DiseaseChristine Joy FloresPas encore d'évaluation
- SA Psych MAY 2016 FIn Final WebDocument82 pagesSA Psych MAY 2016 FIn Final WebAKNTAI002Pas encore d'évaluation
- Assessment of The Intermediate Care Unit Triage SystemDocument6 pagesAssessment of The Intermediate Care Unit Triage SystemJHPas encore d'évaluation
- Neonatal Breast Hypertrophy RevisitedDocument2 pagesNeonatal Breast Hypertrophy Revisitedabas karimPas encore d'évaluation
- Prevalence of Soil Transmitted Helminths infection in adults in North SulawesiDocument4 pagesPrevalence of Soil Transmitted Helminths infection in adults in North SulawesiSahrul hamidPas encore d'évaluation
- CHN Exercise 1 - Paola Mariz P. CeroDocument3 pagesCHN Exercise 1 - Paola Mariz P. CeroPaola Mariz P. CeroPas encore d'évaluation
- Microchem Non GLP ASTM E1052 Study Report NG14797Document6 pagesMicrochem Non GLP ASTM E1052 Study Report NG14797MaryDianne RamosPas encore d'évaluation
- Cytotoxins Pose Risks for Healthcare WorkersDocument2 pagesCytotoxins Pose Risks for Healthcare WorkersMaria Nesen NuezPas encore d'évaluation
- The Different Types of Sleeping DisordersDocument5 pagesThe Different Types of Sleeping DisordersRadee King CorpuzPas encore d'évaluation