Académique Documents
Professionnel Documents
Culture Documents
Biliary Tract Surgery in Dogs and Cats
Transféré par
Esther ArifinDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Biliary Tract Surgery in Dogs and Cats
Transféré par
Esther ArifinDroits d'auteur :
Formats disponibles
Biliary tract surgery in the dog and cat:
Indications and techniques
Ivan Doran BVSc Cert SAS MRCVS
Alasdair Hotston Moore MA VetMB Cert SAC Cert VR Cert SAS MRCVS
DEPARTMENT OF CLINICAL VETERINARY SCIENCE, UNIVERSITY OF BRISTOL, LANGFORD HOUSE,
LANGFORD, BRISTOL. BS40 5DU
ANATOMY (Fig. 1) l Extramural causes of biliary obstruction include
neoplasia (duodenal, pancreatic) and pancreatitis
(Fig. 3).
l Biliary peritonitis (Fig. 4) occurs when bile leaks
from the extrahepatic biliary system.This can occur
Gall bladder
Hepatic ducts
Cystic duct
Hepatic ducts
Common bile duct
Fig. 2: Biliary obstruction secondary to biliary
Duodenum
carcinoma of the common bile duct in a cat.
Intramural
bile duct
Major duodenal
papilla
Minor pancreatic
papilla
Pancreas
Fig. 1: Normal canine biliary anatomy (redrawn from Miller’s
guide to the dissection of the dog; third Ed).
Fig. 3: Cat with obstructive jaundice secondary to
CLINICAL PRESENTATIONS
pancreatitis.
The extrahepatic biliary tract of dogs and cats can be
affected by a variety of diseases, either due to
primary pathology of the biliary system or as a result
of disease in another organ causing secondary
dysfunction of the biliary tree. Although a wide
range of causes of extrahepatic biliary dysfunction
exist, these all result in either obstruction to bile flow
or to leakage of bile into the peritoneal cavity.
l Intraluminal causes of biliary obstruction include
inspissation of biliary secretion, cholelithiasis and
mucinous debris resulting from gallbladder
mucocoeles.
l Intramural causes of biliary obstruction include Fig. 4: Biliary peritonitis in a dog secondary to blunt
biliary neoplasia (Fig. 2) and cholangitis. abdominal trauma.
UK Vet - Vol 12 No 1 January 2007 SMALL ANIMAL l SURGERY HHH 1
secondary to necrotising cholecystitis (Fig. 5), biliary peritonitis may be suspected following
trauma, usually affecting the biliary ducts or, accumulation of fluid within the peritoneal cavity
rarely, secondary to biliary obstruction. and recovery of bile-containing fluid on
abdominocentesis (Fig. 4).
PREOPERATIVE CONSIDERATIONS
Haemorrhagic diathesis in dogs and cats with liver
disease is seldom a clinical problem, in contrast to the
situation in humans.Vitamin K deficiency can occur
secondarily to chronic biliary obstruction and this
can lead to lowered levels of clotting factors II,VII,
IX and X. Clinical cases of biliary obstruction in
dogs and cats are usually encountered before this
situation develops, but should these deficiencies be
suspected, subcutaneous administration of vitamin
K1 (at 1-2 mg/kg) is usually sufficient to normalise
coagulation within 3 to 12 hours of administration.
There is also strong evidence that chronic
obstructive jaundice, in dogs and in humans,
predisposes the patient to post-operative
Fig. 5: Biliary peritonitis and adhesions following gallbladder hypotension and subsequent acute renal failure.
CHOLECYSTOTOMY
rupture secondary to necrotising cholecystitis.
The commonest causes of biliary tract obstruction in Primary indications for cholecystotomy include
the dog are pancreatitis and neoplasia whilst in the removal of inspissated biliary ‘sludge’ or choleliths
cat, a combination of inflammatory conditions such from the gallbladder.
as cholangitis, cholangiohepatitis, pancreatitis and
inflammatory bowel disease frequently co-exist. Cats Cholecystotomy is only indicated when the
also regularly present with biliary obstruction gallbladder wall remains healthy. It is imperative that
secondary to neoplasia. patency of the cystic duct and common bile duct is
confirmed before the gallbladder is closed. Biliary
Note: the authors have seen several cases of biliary tree cannulation is most readily achieved in a
peritonitis that resulted from bile leaking through a retrograde fashion, via a duodenal incision (Fig. 7).
proximal duodenal perforation, into the peritoneal Anterograde cannulation, via the cholecystotomy
cavity. These perforations were usually a result of incision, is more difficult owing to the acute angle
NSAID toxicity and the biliary tract itself was between the cystic and the common bile ducts.
normal.
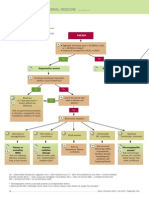
DIAGNOSIS
A full discussion of the diagnosis of biliary
obstruction in dogs and cats is beyond the scope of
this article. Ultrasonography provides the best, readily
available, modality to image the biliary tract. Dilation
of the gallbladder and biliary ducts, along with an
increased tortuosity of the biliary tract (Fig. 6) is
suggestive of biliary obstruction, although it can be
difficult in some cases to distinguish between current
and recent but resolved biliary obstruction. Cases of
Fig. 7: Retrograde cannulation of the canine common
bile duct via a duodenal incision.
1. Laparotomy swabs are used to pack off the
gallbladder to minimise the risk of abdominal
contamination from gallbladder contents.
2. A stay suture is placed, into the fundus of the
gallbladder to facilitate atraumatic manipulation
during the procedure. Fine synthetic monofilament
suture material is used.
3. It may be possible to aspirate some of the
gallbladder contents, using a 16G needle. This
decompression will reduce the risk of spillage of
Fig. 6: Biliary tract dilation and increased tortuosity in luminal contents during incision of the
a cat following fibrosis of the common bile duct. gallbladder.
2 SMALL ANIMAL l SURGERY HHH UK Vet - Vol 12 No 1 January 2007
4. Whilst an assistant applies traction to the stay from the liver surface is controlled by gentle
sutures, a generous incision is made from the pressure with a swab.
fundus towards the neck of the gall bladder. 5. Mobilisation of the gallbladder and proximal
5. Luminal contents are removed using tissue cystic duct is effected and then the cystic duct is
forceps and/or lavage and suction. cross clamped. A distal cystic duct ‘stump’ is left
6. The patency of the common bile duct and cystic so that the hepatic ducts from the central
ducts is checked. An assistant’s fingers are division of the liver are not ‘pinched’ by the
employed to occlude the duodenum either side clamp, at their junction with the cystic duct.The
of the proposed duodenal incision site. An gallbladder and proximal cystic duct are
antimesenteric duodenal incision is made removed. If an obstructive biliary disease is
(centred approximately 4 cm distal to the pylorus suspected, then before the cystic duct is clamped,
in a medium sized dog). Duodenal contents are an incision is made into the gallbladder to permit
suctioned and the major duodenal papilla is retrograde flushing of the biliary tract, via the
identified. A 4 Fr catheter is passed and the duodenum (see cholecystotomy), to ensure the
biliary system flushed. The duodenal incision is patency of the common bile duct. The cystic
closed using a full thickness simple continuous duct and cystic artery are then ligated with a
suture pattern with a synthetic absorbable suture single ligature using synthetic absorbable suture
material. material, before being sectioned proximal to the
7. The cholecystotomy incision is closed using a ligature.The gallbladder should be submitted for
monofilament absorbable suture material. The histological and microbiological analysis (Fig. 8).
suture line is begun at the gallbladder neck and
the initial knot’s short end is retained as a stay
suture. A biopsy of the gallbladder wall may be
taken first, but the authors recommend avoiding
cholecystotomy where mural disease is
suspected. Bacteriological culture and sensitivity
testing are performed on the bile.
CHOLECYSTECTOMY
Cholecystectomy is indicated when the gallbladder
is traumatised or diseased, and also when the
gallbladder is suspected to be the source of recurrent
biliary disease (e.g. gallbladder mucocoeles). Fig. 8: Excised gall bladder from a cat.
Cholelithiasis and cholecystitis (including the
necrotizing form, which may present with CHOLECYSTODUODENOSTOMY
perforation) can often be successfully treated by Cholecystoduodenostomy is indicated to bypass sites
performing a cholecystectomy. If a biliary tract of obstruction or trauma affecting the extrahepatic
obstruction is suspected then the patency of the biliary tree. It is widely considered to be the most
common bile duct must be verified, as previously useful procedure for biliary diversion in dogs and
described. cats. It is used when the gallbladder is not directly
involved in the disease process. It is also used for
1. The region around the gallbladder is packed off management of extrahepatic biliary tract rupture,
as for cholecystotomy. together with ligation of the common bile duct.
2. A stay suture is placed into a non-friable area of
the apex of the gallbladder to facilitate 1. The gallbladder is packed off using laparotomy
manipulation of the organ during dissection. swabs.
Choice of stay suture material is of little 2. A stay suture is placed in the gallbladder, as
consequence. previously described for cholecystotomy. Stay
3. Cholecystocentesis is not necessary and it is sutures are also placed in the antimesenteric
easier to follow an appropriate plane of dissection border of the proximal duodenum, approximately
around a turgid gallbladder. 5 cm apart.
4. Traction is applied using the stay suture and a 3. The gallbladder is mobilised away from the
pair of Metzenbaum scissors are used to incise hepatic fossa, as for cholecystectomy. Care is
the visceral peritoneum between the gallbladder taken not to traumatise the gallbladder wall or
and its hepatic fossa. This visceral peritoneal the cystic artery as it courses with the cystic duct
incision is progressively extended around the to invest the gallbladder wall. Complete
entire liver-gallbladder junction in order that a mobilisation of the gallbladder up to its junction
clean plane of dissection can be subsequently with the cystic duct is crucial to permit a
maintained. Blunt dissection between the tension-free anastamosis to the duodenum, and
gallbladder and the hepatic fossa is continued, so minimise the risks of biliary leakage, wound
using Metzenbaum scissors, a rounded suction dehiscence and stoma stricture post-operatively.
tip or by finger dissection. Minor haemorrhage NB It is easier to achieve a tension free
UK Vet - Vol 12 No 1 January 2007 SMALL ANIMAL l SURGERY HHH 3
anastomosis between the gallbladder and the suture line, ensuring a complete seal around the
jejunum but this is a less physiological technique stoma (Fig. 10).
and predisposes the patient to duodenal
ulceration. Laparoscopic stapling devices (e.g. the EndoGIA,
Tyco) can also be employed to create a swift,
The presence of bile in the duodenum is, in fact, effective and secure cholecystoduodenostomy.
integral to the neuroendocrine mechanisms
responsible for inhibiting gastric acid secretion. It
is not necessary to dissect free the cystic duct
itself to achieve an adequately mobilised
gallbladder, and such a dissection exposes the
cystic artery to the risk of iatrogenic trauma as it
accompanies the cystic duct in its course.
4. An assistant applies traction to both the
gallbladder and duodenal stay sutures, in order to
appose the gallbladder’s longitudinal axis and the
antimesenteric aspect of the proximal
duodenum. Care is taken not to twist the cystic
duct during this manoeuvre.
5. A simple continuous, full thickness suture (Fig. 9)
is placed to appose the duodenum and
gallbladder. Synthetic absorbable suture material
is used. The end of the short limb of the initial
knot can be clamped and employed as a further Fig. 10: Completed cholecystoduodenostomy.
stay suture whilst the suture line is being
constructed. TREATMENT
There is a plethora of surgical techniques described
for treatment of biliary tract disease and trauma. In
veterinary medicine, the vast majority of situations
can be addressed by performing cholecystotomy,
cholecystectomy, or by effecting biliary diversion via
cholecystoduodenostomy. Cases of biliary
obstruction secondary to transient, non-biliary
disease (e.g. pancreatitis) may benefit from biliary
tract decompression via cholecystocentesis under
ultrasonographic guidance, whilst the primary
condition resolves. However, there is a significant
risk of leakage from the needle hole if the cause of
obstruction persists.Techniques of primary repair of
the biliary tract are less applicable to dogs and cats
than to humans. The comparatively narrow
extrahepatic biliary tract of our patients renders the
risks both of post-operative biliary leakage from the
Fig. 9: Cholecystoduodenostomy in a dog. The first suture repair site and of stenosis/stricture of the repair site,
line has been completed. much higher. Furthermore, clinical signs following
biliary tract rupture often have an insidious onset.
6. A full thickness incision is made, along the The time interval elapsing between rupture and
longitudinal axis of the gallbladder, adjacent and surgical intervention may therefore be sufficient to
parallel to the simple continuous suture line.This permit adhesion formation between the biliary tract
incision should be as long as possible to limit the and adjacent tissues, thus rendering primary repair
risk of post-operative stoma stricture. A full more difficult (Fig. 5). Stenting techniques are also
thickness incision, of the same length as the popular in human medicine but are often
gallbladder incision, is made at the inappropriate in dogs and cats because of the higher
antimesenteric border of the proximal risks of stent occlusion and because of difficulties
duodenum, adjacent and parallel to the duodenal with regard to patient compliance.
incision. Biliary and duodenal contents are
aspirated from the vicinity of the incisions. A COMPLICATIONS/PROGNOSIS
second, full thickness, simple continuous suture is The prognosis for a patient following biliary tract
placed to appose the near edges of the surgery is very much influenced by the underlying
gallbladder and duodenal incisions. If the ends of pathology that is present. Cases of biliary tract
the first suture line are tied but not cut, they can obstruction or rupture secondary to a neoplastic
then be tied to the respective ends of the second process, usually pancreatic or biliary adeno-
4 SMALL ANIMAL l SURGERY HHH UK Vet - Vol 12 No 1 January 2007
carcinoma, merit an extremely guarded prognosis.
The prognosis for patients with biliary peritonitis is
very much dependent on the presence of bacteria
within the peritoneal effusion. Animals with a septic
biliary peritonitis carry a considerably worse
prognosis than animals with a sterile biliary
peritonitis. Cats are generally recognized as
representing a greater challenge than dogs, in
achieving a successful outcome following biliary
surgery. The creation of a large stoma when
performing cholecystoduodenostomy will decrease
both the risks of post-operative stoma stenosis and of
reflux cholangiohepatitis.Atraumatic tissue handling,
careful attention to surgical technique, correct choice
of instrumentation and suture material and finally,
the selection of an appropriate procedure performed
on viable tissue are all major factors in the success of
surgery in addressing biliary tract problems.
FURTHER READING
FAHIE et al (1995) JAAHA 31[6]:478-482 Extrahepatic biliary tract
obstruction : a retrospective study of 45 cases (1983-1993).
MEHLER et al (2004) Vet Surg 33 [6]:644-649 Variables associated with
outcome in dogs undergoing extrahepatic biliary surgery : 60 cases
(1988-2002).
MAYHEW et al (2002) JSAP 43[6]:247-253 Pathogenesis and outcome of
extrahepatic biliary obstruction in cats.
PIKE et al (2004) JAVMA 224[10]:1615-1622 Gallbladder mucocoele in
dogs: 30 cases (2000-2002).
HERMAN et al (2005) JAVMA 227[11]:1782-1786 Therapeutic
percutaneous ultrasound-guided cholecystocentesis in three dogs with
extrahepatic biliary obstruction and pancreatitis.
LUDWIG et al (1997) Vet Surg 26[2]:90-98 Surgical treatment of bile
peritonitis in 24 dogs and 2 cats : a retrospective study (1987-1994)
BACON N. J. and WHITE R. A. (2003) JSAP 44[5]:231-235 Extrahepatic
biliary tract surgery in the cat: a case series and review.
© Photographs courtesy of Professor P. E. Holt, Alasdair Hotston
Moore and Ivan Doran.
UK Vet - Vol 12 No 1 January 2007 SMALL ANIMAL l SURGERY HHH 5
Vous aimerez peut-être aussi
- Mucocele 2Document13 pagesMucocele 2FEY YENG SOFIA FUNG GUADALUPEPas encore d'évaluation
- Canine CastrationDocument6 pagesCanine CastrationAnonymous c215Fq6Pas encore d'évaluation
- FELINE-Feline Hepatic Lipidosis TreatmentDocument9 pagesFELINE-Feline Hepatic Lipidosis Treatmenttaner_soysurenPas encore d'évaluation
- Toxin Mechanism of Action Sign of Toxicity Diagnosis Treatment Anticholinesterase InsecticidesDocument2 pagesToxin Mechanism of Action Sign of Toxicity Diagnosis Treatment Anticholinesterase Insecticidesrayrrn00Pas encore d'évaluation
- Neutering in CatsDocument10 pagesNeutering in CatsFatin Amirah RamliPas encore d'évaluation
- Sni 3950-2014Document88 pagesSni 3950-2014Dya Yda'sPas encore d'évaluation
- Diabetic Emergencies in Small AnimalsDocument17 pagesDiabetic Emergencies in Small Animalsdia_diannePas encore d'évaluation
- Pet Nutrition-Zadina 7.11.11Document34 pagesPet Nutrition-Zadina 7.11.11doczadina5428100% (1)
- Diseases, Diagnosis and Management of Ocular FundusDocument111 pagesDiseases, Diagnosis and Management of Ocular FundusThakur Abhishek SinghPas encore d'évaluation
- DiabeticeducationDocument11 pagesDiabeticeducationapi-316157555Pas encore d'évaluation
- A Aha Diabetes GuidelinesDocument10 pagesA Aha Diabetes GuidelinesOvidiu PinteaPas encore d'évaluation
- IDEXX Product Reference GuideDocument6 pagesIDEXX Product Reference GuideHa Le0% (2)
- 2011 Reproductive Cycles of The Domestic BitchDocument11 pages2011 Reproductive Cycles of The Domestic BitchMariaCamilaLeonPerezPas encore d'évaluation
- Wildlife NoteDocument14 pagesWildlife NoteDeep PatelPas encore d'évaluation
- Feline Lower Urinary Tract Disease (FLUTD) - CatDocument5 pagesFeline Lower Urinary Tract Disease (FLUTD) - CatAndrexixPas encore d'évaluation
- 2011 Nestle Purina Veterinary Symposium On Companion Animal MedicineDocument30 pages2011 Nestle Purina Veterinary Symposium On Companion Animal Medicineguadasampaio100% (1)
- EnucleationDocument6 pagesEnucleationRameez SarwarPas encore d'évaluation
- Feline Urologic Syndrome enDocument2 pagesFeline Urologic Syndrome enSitiNurjannahPas encore d'évaluation
- 4 Diabetes MellitusDocument26 pages4 Diabetes MellitusnomiskemalPas encore d'évaluation
- CacingDocument21 pagesCacingIhza SaputraPas encore d'évaluation
- Hints On Veterinary Ophthalmology: By/Sara Ahmed Hassouna BVSC, MSC Surgery Dept. Vet. Med. Alex. UniDocument39 pagesHints On Veterinary Ophthalmology: By/Sara Ahmed Hassouna BVSC, MSC Surgery Dept. Vet. Med. Alex. UniBibek SutradharPas encore d'évaluation
- Anemia DiagnosticTree PDFDocument2 pagesAnemia DiagnosticTree PDFguadialvarezPas encore d'évaluation
- Clinical Veterinary Advisor Dogs and Cats by Etienne Cote DVMDACVIMCardiology and Small Animal Internal Medicine 5 Star ReviewDocument2 pagesClinical Veterinary Advisor Dogs and Cats by Etienne Cote DVMDACVIMCardiology and Small Animal Internal Medicine 5 Star ReviewAndres GarciaPas encore d'évaluation
- Urinary Catheter Placement For Feline ObstructionDocument6 pagesUrinary Catheter Placement For Feline ObstructionWilliam ChandlerPas encore d'évaluation
- African Pygmy Hedgehog CareDocument7 pagesAfrican Pygmy Hedgehog CareLuciano Verzola100% (1)
- Small Animal Spinal Disorders Diagnosis and Surgery, 2nd Edition (Vetbooks - Ir)Document369 pagesSmall Animal Spinal Disorders Diagnosis and Surgery, 2nd Edition (Vetbooks - Ir)ghimboasaPas encore d'évaluation
- UntitledDocument334 pagesUntitledLocalVet TunariPas encore d'évaluation
- CANINE-Mechanism of Thrombocytopenia in Dogs With CancerDocument11 pagesCANINE-Mechanism of Thrombocytopenia in Dogs With Cancertaner_soysuren100% (1)
- Atlas of Gastrointestinal Endoscopy in Dogs and CatsDocument8 pagesAtlas of Gastrointestinal Endoscopy in Dogs and CatsDama Ayu RaniPas encore d'évaluation
- Small Animal Medicine Upper Airways ChartsDocument14 pagesSmall Animal Medicine Upper Airways ChartsBrookePas encore d'évaluation
- ECG Interpretation in DogsDocument107 pagesECG Interpretation in DogsPLABITA GOSWAMI100% (2)
- RUV40404 Certificate IV in Veterinary NursingDocument36 pagesRUV40404 Certificate IV in Veterinary NursingEdward FergusonPas encore d'évaluation
- Feline Hepatic LipidosisDocument46 pagesFeline Hepatic LipidosisAndre Suarez FarfanPas encore d'évaluation
- The Pocket Book of Tips For Practising VetsDocument101 pagesThe Pocket Book of Tips For Practising VetsFabricamargo100% (1)
- Classification of Vaginal Epithelial CellsDocument14 pagesClassification of Vaginal Epithelial CellsShinta PuspitasariPas encore d'évaluation
- Veterinary Cytology by Leslie C. Sharkey, M. Judith Radin, Davis SeeligDocument994 pagesVeterinary Cytology by Leslie C. Sharkey, M. Judith Radin, Davis SeeligBê LagoPas encore d'évaluation
- CANINE-Management Protocol For Acute Gastric Dilatation-Volvulus Syndrom in DogsDocument7 pagesCANINE-Management Protocol For Acute Gastric Dilatation-Volvulus Syndrom in Dogstaner_soysurenPas encore d'évaluation
- UC Davis Koret Shelter Medicine Program - Feline - Guide To Raising Orphan Kittens - 2012-04-25Document9 pagesUC Davis Koret Shelter Medicine Program - Feline - Guide To Raising Orphan Kittens - 2012-04-25Kitt KaosPas encore d'évaluation
- Ophthalmology For The Veterinary Practitioner - Revised and ExpandedDocument272 pagesOphthalmology For The Veterinary Practitioner - Revised and ExpandedJulia Martinez PottierPas encore d'évaluation
- Amputation of Tail in AnimalsDocument8 pagesAmputation of Tail in AnimalsSabreen khattakPas encore d'évaluation
- Kitten Bottle Feeding and Stomach Capacity ChartDocument1 pageKitten Bottle Feeding and Stomach Capacity ChartAmoriHeydenrychPas encore d'évaluation
- 1 GPS Slaughterhouse Respiratory Check SRC PDFDocument29 pages1 GPS Slaughterhouse Respiratory Check SRC PDFAnastasia DivaPas encore d'évaluation
- Veterinary Internal Medicine Handbook for Field CasesDocument88 pagesVeterinary Internal Medicine Handbook for Field CasesShakil MahmodPas encore d'évaluation
- Feline Vocalization - Excessive: Why Is My Cat Persistently Crying?Document4 pagesFeline Vocalization - Excessive: Why Is My Cat Persistently Crying?Brook Farm Veterinary CenterPas encore d'évaluation
- Equine Gastric Ulcers / A Presentation by Wendy Harless Mollat, DVM, DACVIM, Pilchuck Veterinary HospitalDocument47 pagesEquine Gastric Ulcers / A Presentation by Wendy Harless Mollat, DVM, DACVIM, Pilchuck Veterinary HospitalPilchuck Veterinary HospitalPas encore d'évaluation
- How To February 2014 Anesteziezi o PasareDocument6 pagesHow To February 2014 Anesteziezi o PasarelybrakissPas encore d'évaluation
- Suspensory Ligament Rupture Tech During Small Animal OH PDFDocument8 pagesSuspensory Ligament Rupture Tech During Small Animal OH PDFRiesky NudialestariPas encore d'évaluation
- Infectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 14 Feline Immunodeficiency Virus InfectionDocument24 pagesInfectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 14 Feline Immunodeficiency Virus InfectionsoledadDC329Pas encore d'évaluation
- Mini VET GuideDocument186 pagesMini VET GuideemitibiPas encore d'évaluation
- Fluidtherapy GuidelinesDocument11 pagesFluidtherapy Guidelineshamida fillahPas encore d'évaluation
- Michael Schaer-Clinical Signs in Small Animal Medicine-Manson Pub. - The Veterinary Press (2008) PDFDocument289 pagesMichael Schaer-Clinical Signs in Small Animal Medicine-Manson Pub. - The Veterinary Press (2008) PDFRodrigo Lazzarotto100% (1)
- Canine InsulinomaDocument5 pagesCanine Insulinomasoff4ikaPas encore d'évaluation
- DR Jones Cat Health Web Clinic Slides 1222Document222 pagesDR Jones Cat Health Web Clinic Slides 1222Haider Al Zamily100% (1)
- FELINE-Clinical Forms of Acquired Myasthenia Gravis in CatsDocument7 pagesFELINE-Clinical Forms of Acquired Myasthenia Gravis in Catstaner_soysurenPas encore d'évaluation
- Cat PresentationDocument33 pagesCat PresentationNadia Rahma NoviyantiPas encore d'évaluation
- I&IDocument7 pagesI&IJdee XPas encore d'évaluation
- Gallstone Ileus: An Unusual Cause of Intestinal ObstructionDocument7 pagesGallstone Ileus: An Unusual Cause of Intestinal ObstructionSiska Eni WijayantiPas encore d'évaluation
- Anesthetic Consideration For Patients With Obstructive JaundiceDocument47 pagesAnesthetic Consideration For Patients With Obstructive JaundiceagatakassaPas encore d'évaluation
- The Problem of Primary Biliary Cirrhosis - AjmDocument4 pagesThe Problem of Primary Biliary Cirrhosis - AjmClara Cotón BatresPas encore d'évaluation
- CR PrimateDocument5 pagesCR Primateapi-26116142Pas encore d'évaluation
- Rabbit Model For ArthritisDocument5 pagesRabbit Model For ArthritisEsther ArifinPas encore d'évaluation
- Fumonisin in Various AnimalsDocument25 pagesFumonisin in Various AnimalsEsther ArifinPas encore d'évaluation
- Clinical Cytology For Small Animals1-IntroductionDocument8 pagesClinical Cytology For Small Animals1-IntroductionEsther ArifinPas encore d'évaluation
- Canine Hemangiopericytoma Mar2006Document4 pagesCanine Hemangiopericytoma Mar2006Esther ArifinPas encore d'évaluation
- Defining Traction and Fixation TermsDocument25 pagesDefining Traction and Fixation Termsmftaganas100% (1)
- Gallstones: Causes, Symptoms and TreatmentDocument15 pagesGallstones: Causes, Symptoms and Treatmenthisabumohamed100% (1)
- Nursing Care Plan for Mrs. ReyesDocument3 pagesNursing Care Plan for Mrs. ReyesElishah CaprichoPas encore d'évaluation
- Surehands LMNDocument1 pageSurehands LMNapi-383151067Pas encore d'évaluation
- Biopure Case Solution: Havard Business School CaseDocument4 pagesBiopure Case Solution: Havard Business School Caseparoengineer75% (4)
- Foundation Programme Curriculum 2016Document100 pagesFoundation Programme Curriculum 2016breadfanPas encore d'évaluation
- Disease Symptoms and Patient Profile DatasetDocument6 pagesDisease Symptoms and Patient Profile Datasetnavyalohitha49Pas encore d'évaluation
- Ma 11sem. TMP Perio2Document2 pagesMa 11sem. TMP Perio2Karen RosalesPas encore d'évaluation
- KDIGO GN GuidelineDocument143 pagesKDIGO GN GuidelineSamuel Rudolf Maranatha JulioPas encore d'évaluation
- Farmakologi Anti KankerDocument75 pagesFarmakologi Anti KankerromzikerenzPas encore d'évaluation
- Tracer Methodology: Frontline Strategies To Prepare For JCI SurveyDocument23 pagesTracer Methodology: Frontline Strategies To Prepare For JCI SurveyTettanya Iyu Sama Ariqah50% (2)
- Medication Errors FinalDocument7 pagesMedication Errors Finalapi-469407326Pas encore d'évaluation
- Facts and Definition of EclampsiaDocument5 pagesFacts and Definition of EclampsiaChoi Gong JuPas encore d'évaluation
- Casting ProformaDocument2 pagesCasting ProformaPhillip CullenPas encore d'évaluation
- Project Proposal 5 28 19Document5 pagesProject Proposal 5 28 19api-461464117Pas encore d'évaluation
- Medicare Policy: The Independent Payment Advisory Board: A New Approach To Controlling Medicare SpendingDocument24 pagesMedicare Policy: The Independent Payment Advisory Board: A New Approach To Controlling Medicare SpendingCatherine SnowPas encore d'évaluation
- Transitional Care: DR - Vinoli.S.G Professor HOD Medical Surgical Nursing Dept Universal College of Nursing BangaloreDocument15 pagesTransitional Care: DR - Vinoli.S.G Professor HOD Medical Surgical Nursing Dept Universal College of Nursing BangalorevinoliPas encore d'évaluation
- Referat EndocarditisDocument25 pagesReferat EndocarditisNadya Hasna Rasyida DAPas encore d'évaluation
- Readings For Pedia WardDocument6 pagesReadings For Pedia WardShania CabucosPas encore d'évaluation
- How To Identify Adhd ChildrenDocument6 pagesHow To Identify Adhd ChildrenKUNNAMPALLIL GEJO JOHNPas encore d'évaluation
- KELOMPOK 1 - RS2 - PRAKTIK BAHASA INGGRIS DetailDocument12 pagesKELOMPOK 1 - RS2 - PRAKTIK BAHASA INGGRIS Detailseren agathaPas encore d'évaluation
- Reading New E2 PDFDocument50 pagesReading New E2 PDFMary Jis100% (1)
- Interpretation of The Reptile Blood ProfileDocument8 pagesInterpretation of The Reptile Blood ProfileAndre NgoPas encore d'évaluation
- Preoperative Evaluation and Preparation of The Gynecologic Patient - GLOWMDocument13 pagesPreoperative Evaluation and Preparation of The Gynecologic Patient - GLOWMshaliniPas encore d'évaluation
- CGHS Empaneled HospitalsDocument61 pagesCGHS Empaneled HospitalsAshutosh SaxenaPas encore d'évaluation
- NCP EpilepsyDocument1 pageNCP EpilepsyManpreet ToorPas encore d'évaluation
- Antidepressants Ssris, Snris: Selective Serotonin Reuptake Inhibitors Norepinephrine Reuptake InhibitorsDocument23 pagesAntidepressants Ssris, Snris: Selective Serotonin Reuptake Inhibitors Norepinephrine Reuptake InhibitorsJosh SchultzPas encore d'évaluation
- Mr. Abhishek Sharma-1Document3 pagesMr. Abhishek Sharma-1Abhishek SharmaPas encore d'évaluation
- ATROVENTDocument25 pagesATROVENTNúñez AlejandroPas encore d'évaluation
- Cell SaverDocument8 pagesCell SaverFrank QuitianPas encore d'évaluation