Académique Documents
Professionnel Documents
Culture Documents
013
Transféré par
lancastd54Description originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
013
Transféré par
lancastd54Droits d'auteur :
Formats disponibles
Section I - Introduction to the Summary of Benefits
for
MD MedicareChoice Florida Optimum MB
January 1, 2008 - December 31, 2008
Alachua, Brevard, Charlotte, Duval, Hernando, Hillsborough,
Lake, Lee, Manatee, Marion, Orange, Osceola, Palm Beach,
Pasco, Pinellas, Polk, Sarasota, Seminole, Volusia Counties, FL.
The name of PartnerCare Health Plan, Inc will now be MD MedicareChoice. We have chosen a
name that is consistent with the member population that we serve.
SECTION I - INTRODUCTION TO SUMMARY OF BENEFITS
Thank you for your interest in MD MedicareChoice Florida Optimum MB. Our plan is offered by
MD MedicareChoice, Inc., a Medicare Advantage Health Maintenance Organization (HMO). This
Summary of Benefits tells you some features of our plan. It doesn't list every service that we cover
or list every limitation or exclusion. To get a complete list of our benefits, please call MD
MedicareChoice Florida Optimum MB and ask for the "Evidence of Coverage".
YOU HAVE CHOICES IN YOUR HEALTH CARE
As a Medicare beneficiary, you can choose from different Medicare options. One option is the
Original (fee-for-service) Medicare Plan. Another option is a Medicare health plan, like MD
MedicareChoice Florida Optimum MB. You may have other options too. You make the choice. No
matter what you decide, you are still in the Medicare Program.
You may join or leave a plan only at certain times. Please call MD MedicareChoice Florida
Optimum MB at the telephone number listed at the end of this introduction or 1-800-MEDICARE
(1-800-633-4227) for more information. TTY users should call 1-877-486-2048. You can call this
number 24 hours a day, 7 days a week.
HOW CAN I COMPARE MY OPTIONS?
You can compare MD MedicareChoice Florida Optimum MB and the Original Medicare Plan using
this Summary of Benefits. The charts in this booklet list some important health benefits. For each
benefit, you can see what our plan covers and what the Original Medicare Plan covers.
Our members receive all of the benefits that the Original Medicare Plan offers. We also offer more
benefits, which may change from year to year.
1 H5729 013_CO0531 (11/07)
WHERE IS MD MedicareChoice Florida Optimum MB AVAILABLE?
The service area for this plan includes: Alachua, Brevard, Charlotte, Duval, Hernando,
Hillsborough, Lake, Lee, Manatee, Marion, Orange, Osceola, Palm Beach, Pasco, Pinellas, Polk,
Sarasota, Seminole, Volusia Counties, FL. You must live in one of these areas to join the plan.
WHO IS ELIGIBLE TO JOIN MD MedicareChoice Florida Optimum MB?
You can join MD MedicareChoice Florida Optimum MB if you are entitled to Medicare Part A and
enrolled in Medicare Part B and live in the service area. However, individuals with End Stage Renal
Disease are generally not eligible to enroll in MD MedicareChoice Florida Optimum MB unless
they are members of our organization and have been since their dialysis began.
CAN I CHOOSE MY DOCTORS?
MD MedicareChoice Florida Optimum MB has formed a network of doctors, specialists, and
hospitals. You can only use doctors who are part of our network. The health providers in our
network can change at any time. You can ask for a current Provider Directory for an up-to-date list
or visit us at www.mdmedicarechoice.com. Our customer service number is listed at the end of this
introduction.
WHAT HAPPENS IF I GO TO A DOCTOR WHO'S NOT IN YOUR NETWORK?
If you choose to go to a doctor outside of our network, you must pay for these services yourself.
Neither MD MedicareChoice nor the Original Medicare Plan will pay for these services.
DOES MY PLAN COVER MEDICARE PART B OR PART D DRUGS?
MD MedicareChoice Florida Optimum MB does cover both Medicare Part B prescription drugs and
Medicare Part D prescription drugs.
WHERE CAN I GET MY PRESCRIPTIONS IF I JOIN THIS PLAN?
MD MedicareChoice Florida Optimum MB has formed a network of pharmacies. You must use a
network pharmacy to receive plan benefits. We may not pay for your prescriptions if you use an
out-of-network pharmacy, except in certain cases. The pharmacies in our network can change at any
time. You can ask for a current Pharmacy Network List or visit us at www.mdmedicarechoice.com.
Our customer service number is listed at the end of this introduction.
WHAT IS A PRESCRIPTION DRUG FORMULARY?
MD MedicareChoice Florida Optimum MB uses a formulary. A formulary is a list of drugs covered
by your plan to meet patient needs. We may periodically add, remove, or make changes to coverage
limitations on certain drugs or change how much you pay for a drug. If we make any formulary
change that limits our members' ability to fill their prescriptions, we will notify the affected
enrollees before the change is made. We will send a formulary to you and you can see our complete
formulary on our Web site at http://www.mdmedicarechoice.com/formulary.pdf.
If you are currently taking a drug that is not on our formulary or subject to additional requirements
or limits, you may be able to get a temporary supply of the drug. You can contact us to request an
exception or switch to an alternative drug listed on our formulary with your physician's help. Call
us to see if you can get a temporary supply of the drug or for more details about our drug transition
policy.
2 H5729 013_CO0531 (11/07)
HOW CAN I GET EXTRA HELP WITH PRESCRIPTION DRUG PLAN COSTS?
If you qualify for extra help with your Medicare prescription drug plan costs, your premium and
costs at the pharmacy will be lower. When you join MD MedicareChoice Florida Optimum MB,
Medicare will tell us how much extra help you are getting. Then we will let you know the amount
you will pay. If you are not getting this extra help you can see if you qualify by calling 1-800-
MEDICARE (1-800-633-4227), TTY users should call 1-877-486-2048. You can call this number
24 hours a day, 7 days a week.
WHAT ARE MY PROTECTIONS IN THIS PLAN?
All Medicare Advantage Plans agree to stay in the program for a full year at a time. Each year, the
plans decide whether to continue for another year. Even if a Medicare Advantage Plan leaves the
program, you will not lose Medicare coverage. If a plan decides not to continue, it must send you a
letter at least 90 days before your coverage will end. The letter will explain your options for
Medicare coverage in your area.
As a member of MD MedicareChoice Florida Optimum MB, you have the right to request a
coverage determination, which includes the right to request an exception, the right to file an appeal
if we deny coverage for a prescription drug, and the right to file a grievance. You have the right to
request a coverage determination if you want us to cover a Part D drug that you believe should be
covered. An exception is a type of coverage determination. You may ask us for an exception if you
believe you need a drug that is not on our list of covered drugs or believe you should get a non-
preferred drug at a lower out-of-pocket cost. You can also ask for an exception to cost utilization
rules, such as a limit on the quantity of a drug. If you think you need an exception, you should
contact us before you try to fill your prescription at a pharmacy. Your doctor must provide a
statement to support your exception request. If we deny coverage for your prescription drug(s), you
have the right to appeal and ask us to review our decision. Finally, you have the right to file a
grievance if you have any type of problem with us or one of our network pharmacies that does not
involve coverage for a prescription drug.
WHAT IS A MEDICATION THERAPY MANAGEMENT (MTM) PROGRAM?
A Medication Therapy Management (MTM) Program is a free service we may offer. You may be
invited to participate in a program designed for your specific health and pharmacy needs. You may
decide not to participate but it is recommended that you take full advantage of this covered service
if you are selected. Contact MD MedicareChoice Florida Optimum MB for more details.
3 H5729 013_CO0531 (11/07)
Please call MD MedicareChoice for more information about this plan.
Visit us at www.mdmedicarechoice.com or, call us:
Customer Service Hours:
Sunday, Monday, Tuesday, Wednesday, Thursday, Friday, Saturday, 8:00 a.m. - 8:00 p.m.
Eastern
Current and Prospective members should call (888)-901-9208 for questions related to the
Medicare Advantage program. (TTY/TDD (866)-268-1800).
Current and Prospective members should call (888)-901-9208 for questions related to the
Medicare Part D Prescription Drug program. (TTY/TDD (866)-268-1800)
For more information about Medicare, please call Medicare at 1-800-MEDICARE (1-800-
633-4227).
TTY users should call 1-877-486-2048. You can call 24 hours a day, 7 days a week.
Or, visit www.medicare.gov on the web.
If you have special needs, this document may be available in other formats.
If you have any questions about this plan's benefits or costs, please contact MD
MedicareChoice for details.
4 H5729 013_CO0531 (11/07)
SECTION II - SUMMARY OF BENEFITS
MD MedicareChoice
Benefit Original Medicare
Florida Optimum MB
IMPORTANT INFORMATION
1 - Premium and $96.40 monthly Medicare Part B General
Other Important Premium. $0 monthly plan premium in addition to your
Information $96.40 monthly Medicare Part B premium.
$135 yearly Medicare Part B MD MedicareChoice will reduce your
deductible. Medicare Part B premium by up to $60.
If a doctor or supplier does not Out-of-Network
accept assignment, their costs are Unless otherwise noted, out-of-network
often higher, which means you services not covered.
pay more.
2 - Doctor and You may go to any doctor, In-Network
Hospital Choice specialist or hospital that accepts You must go to network doctors, specialists,
Medicare. and hospitals.
(For more Referral required for network hospitals and
information, see specialists (for certain benefits).
Emergency - #15
and Urgently
Needed Care -
#16.)
SUMMARY OF BENEFITS
INPATIENT CARE
3 - Inpatient For each benefit period: Days 1 - In-Network
Hospital Care 60: $1024 deductible Days 61 - For Medicare-covered hospital stays:
90: $256 per day Days 91 - 150:
$512 per lifetime reserve day
(includes Please call 1-800-MEDICARE (1- Days 1 - 5: $125 copay per day
Substance Abuse 800-633-4227) for information
and about lifetime reserve days.
Rehabilitation
Services)
Lifetime reserve days can only be Days 6 - 90: $0 copay per day
used once.
$0 copay for additional hospital days
5 H5729 013_CO0531 (11/07)
A "benefit period" starts the day
you go into a hospital or skilled
nursing facility. It ends when you
go for 60 days in a row without
hospital or skilled nursing care. If
you go into the hospital after one
benefit period has ended, a new
benefit period begins. You must
pay the inpatient hospital
deductible for each benefit period.
There is no limit to the number of
benefit periods you can have.
No limit to the number of days covered by
the plan each benefit period.
Except in an emergency, your doctor must
tell the plan that you are going to be admitted
to the hospital.
4 - Inpatient Same deductible and copay as In-Network
Mental Health inpatient hospital care (see For hospital stays:
Care "Inpatient Hospital Care" above).
190 day limit in a Psychiatric Days 1 - 5: $125 copay per day
Hospital.
Days 6 - 90: $0 copay per day
You get up to 190 days in a Psychiatric
Hospital in a lifetime.
Except in an emergency, your doctor must
tell the plan that you are going to be admitted
to the hospital.
5 - Skilled For each benefit period after at General
Nursing Facility least a 3-day covered hospital stay: Prior authorization is required.
Days 1 - 20: $0 per day Days 21 -
100: $128 per day
(in a Medicare- 100 days for each benefit period. In-Network
certified skilled For SNF stays:
nursing facility)
6 H5729 013_CO0531 (11/07)
A "benefit period" starts the day Days 1 - 7: $0 copay per day
you go into a hospital or SNF. It
ends when you go for 60 days in a
row without hospital or skilled
nursing care. If you go into the
hospital after one benefit period
has ended, a new benefit period
begins. You must pay the inpatient
hospital deductible for each
benefit period. There is no limit to
the number of benefit periods you
can have.
Days 8 - 100: $75 copay per day
100 days covered for each benefit period
No prior hospital stay is required.
6 - Home Health $0 copay. General
Care Authorization rules may apply.
(includes
medically In-Network
necessary $10 copay for each Medicare-covered home
intermittent health visit.
skilled nursing
care, home
health aide
services, and
rehabilitation
services, etc.)
7 - Hospice You pay part of the cost for In-Network
outpatient drugs and inpatient You must get care from a Medicare-certified
respite care. hospice.
You must get care from a
Medicare-certified hospice.
OUTPATIENT CARE
8 - Doctor Office 20% coinsurance General
Visits See "Routine Physical Exams," for more
information.
In-Network
$0 copay for each primary care doctor visit
for Medicare-covered benefits
$20 copay for each specialist visit for
Medicare-covered benefits.
9 - Chiropractic 20% coinsurance In-Network
Services $20 copay for Medicare-covered visits.
7 H5729 013_CO0531 (11/07)
Routine care not covered Medicare-covered chiropractic visits are for
manual manipulation of the spine to correct a
displacement or misalignment of a joint or
body part.
20% coinsurance for manual
manipulation of the spine to
correct subluxation if you get it
from a chiropractor or other
qualified provider.
10 - Podiatry 20% coinsurance In-Network
Services $20 copay for each Medicare-covered visit.
Routine care not covered. $20 copay for up to 6 routine visit(s) every
year
20% coinsurance for medically Medicare-covered podiatry benefits are for
necessary foot care, including care medically-necessary foot care.
for medical conditions affecting
the lower limbs.
11 - Outpatient 50% coinsurance for most General
Mental Health outpatient mental health services. Authorization rules may apply.
Care
In-Network
$20 copay for each Medicare-covered
individual or group therapy visit.
12 - Outpatient 20% coinsurance General
Substance Abuse Authorization rules may apply.
Care
In-Network
$0 copay for Medicare-covered visits.
13 - Outpatient 20% coinsurance for the doctor General
Services/Surgery Authorization rules may apply.
20% of outpatient facility In-Network
$0 copay for each Medicare-covered
ambulatory surgical center visit.
$100 copay for each Medicare-covered
outpatient hospital facility visit.
14 - Ambulance 20% coinsurance In-Network
Services $100 copay for Medicare-covered ambulance
benefits.
(medically If you are admitted to the hospital, you pay
necessary $0 for Medicare-covered ambulance benefits.
ambulance
services)
8 H5729 013_CO0531 (11/07)
15 - Emergency 20% coinsurance for the doctor In-Network
Care $50 copay for Medicare-covered emergency
room visits.
(You may go to 20% of facility charge, or a set Out-of-Network
any emergency copay per emergency room visit Not covered outside the U.S. except under
room if you limited circumstances. Contact the plan for
reasonably more details.
believe you need
emergency care.)
You don't have to pay the In and Out-of-Network
emergency room copay if you are If you are admitted to the hospital within 48-
admitted to the hospital for the hour(s) for the same condition, you pay $0
same condition within 3 days of for the emergency room visit
the emergency room visit.
NOT covered outside the U.S.
except under limited
circumstances.
16 - Urgently 20% coinsurance, or a set copay General
Needed Care $20 copay for Medicare-covered urgently
needed care visits.
(This is NOT NOT covered outside the U.S. If you are admitted to the hospital within 48-
emergency care, except under limited hour(s) for the same condition, $0 for the
and in most circumstances. urgent-care visit.
cases, is out of
the service area.)
17 - Outpatient 20% coinsurance General
Rehabilitation Authorization rules may apply.
Services
(Occupational In-Network
Therapy, $20 copay for Medicare-covered
Physical Occupational Therapy visits.
Therapy, Speech
and Language
Therapy)
$20 copay for Medicare-covered Physical
and/or Speech/Language Therapy visits.
OUTPATIENT MEDICAL SERVICES AND SUPPLIES
18 - Durable 20% coinsurance General
Medical Authorization rules may apply.
Equipment
(includes In-Network
wheelchairs, $0 copay for Medicare-covered items.
oxygen, etc.)
9 H5729 013_CO0531 (11/07)
19 - Prosthetic 20% coinsurance General
Devices Authorization rules may apply.
(includes braces, In-Network
artificial limbs 20% of the cost for Medicare-covered items.
and eyes, etc.)
20 - Diabetes 20% coinsurance In-Network
Self-Monitoring $0 copay for Diabetes self-monitoring
Training, training.
Nutrition
Therapy, and
Supplies
(includes $0 copay for Nutrition Therapy for Diabetes.
coverage for
glucose
monitors, test
strips, lancets,
screening tests,
and self-
management
training)
$0 copay for Diabetes supplies.
21 - Diagnostic 20% coinsurance for diagnostic General
Tests, X-Rays, tests and x-rays Authorization rules may apply.
and Lab Services
$0 copay for Medicare-covered In-Network
lab services $0 copay for Medicare-covered:
Lab Services: Medicare covers - lab services
medically necessary diagnostic lab
services that are ordered by your
treating doctor when they are
provided by a Clinical Laboratory
Improvement Amendments
(CLIA) certified laboratory that
participates in Medicare.
Diagnostic lab services are done to
help your doctor diagnose or rule
out a suspected illness or
condition. Medicare does not
cover most routine screening tests,
like checking your cholesterol.
- diagnostic procedures and tests
$0 to $75 copay for Medicare-covered X-
rays.
$0 to $75 copay for Medicare-covered
10 H5729 013_CO0531 (11/07)
diagnostic radiology services.
$20 copay for Medicare-covered therapeutic
radiology services.
PREVENTIVE SERVICES
22 - Bone Mass 20% coinsurance In-Network
Measurement $0 copay for Medicare-covered bone mass
measurement
(for people with Covered once every 24 months
Medicare who (more often if medically
are at risk) necessary) if you meet certain
medical conditions.
23 - Colorectal 20% coinsurance In-Network
Screening $0 copay for Medicare-covered colorectal
Exams screenings.
(for people with Covered when you are high risk or
Medicare age 50 when you are age 50 and older.
and older)
24 - $0 copay for Flu and Pneumonia In-Network
Immunizations vaccines $0 copay for Flu and Pneumonia vaccines.
(Flu vaccine, 20% coinsurance for Hepatitis B $0 copay for Hepatitis B vaccine.
Hepatitis B vaccine
vaccine - for
people with
Medicare who
are at risk,
Pneumonia
vaccine)
You may only need the No referral needed for Flu and pneumonia
Pneumonia vaccine once in your vaccines.
lifetime. Call your doctor for more
information.
25 - 20% coinsurance In-Network
Mammograms $0 copay for Medicare-covered screening
(Annual mammograms.
Screening)
(for women with No referral needed.
Medicare age 40
and older)
Covered once a year for all
women with Medicare age 40 and
older. One baseline mammogram
covered for women with Medicare
between age 35 and 39.
11 H5729 013_CO0531 (11/07)
26 - Pap Smears $0 copay for Pap smears In-Network
and Pelvic $0 copay for Medicare-covered pap smears
Exams and pelvic exams.
(for women with Covered once every 2 years.
Medicare) Covered once a year for women
with Medicare at high risk.
20% coinsurance for Pelvic Exams
27 - Prostate 20% coinsurance for the digital In-Network
Cancer rectal exam. $0 copay for Medicare-covered prostate
Screening cancer screening.
Exams
(for men with $0 for the PSA test; 20%
Medicare age 50 coinsurance for other related
and older) services.
Covered once a year for all men
with Medicare over age 50.
28 - ESRD 20% coinsurance for dialysis General
Authorization rules may apply. Out-of-area
Renal Dialysis services do not require
Authorization.
In-Network
$25 copay for in and out-of-area dialysis
$0 copay for Nutrition Therapy for Renal
Disease
29 - Prescription Most drugs not covered. (You can Drugs covered under Medicare Part B
Drugs add prescription drug coverage to General
Original Medicare by joining a 10% of the cost for Part B-covered drugs (not
Medicare Prescription Drug Plan.) including Part B-covered chemotherapy
drugs).
10% of the cost for Part B-covered
chemotherapy drugs.
Drugs covered under Medicare Part D
General
This plan uses a formulary. The plan will
send you the formulary. You can also see the
formulary at
http://www.mdmedicarechoice.com/formular
y.pdf on the web.
12 H5729 013_CO0531 (11/07)
Different out-of-pocket costs may apply for
people who
- have limited incomes,
- live in long term care facilities, or
- have access to Indian/Tribal/Urban (Indian
Health Service).
The plan offers national in-network
prescription coverage. This means that you
will pay the same amount for your
prescription drugs if you get them at an in-
network pharmacy outside of the plan's
service area (for instance when you travel).
Total yearly drug costs are the total drug
costs paid by both you and the plan.
The plan may require you to first try one drug
to treat your condition before it will cover
another drug for that condition.
Some drugs have quantity limits.
Your provider must get prior authorization
from MD MedicareChoice Florida Optimum
MB for certain drugs.
The plan will pay for certain over-the-counter
drugs as part of its utilization management
program. Some over-the-counter drugs are
less expensive than prescription drugs and
work just as well. Contact the plan for
details.
If the actual cost of a drug is less than the
normal copay amount for that drug, you will
pay the actual cost, not the higher copay
amount.
You may have to pay more than your copay
if you choose to use a higher cost drug when
a lower cost drug is available.
In-Network
$0 deductible.
Initial Coverage
You pay the following until total yearly drug
costs reach $2850:
Retail Pharmacy
Generic
- $0 copay for a one-month (31-day) supply
of drugs
13 H5729 013_CO0531 (11/07)
- $0 copay for a three-month (93-day) supply
of drugs
- $0 copay for a 93-day supply of drugs
Preferred Brand
- $35 copay for a one-month (31-day) supply
of drugs
- $105 copay for a three-month (93-day)
supply of drugs
- $105 copay for a 93-day supply of drugs
Non-Preferred Brand
- $70 copay for a one-month (31-day) supply
of drugs
- $210 copay for a three-month (93-day)
supply of drugs
- $210 copay for a 93-day supply of drugs
Specialty Drugs
- 25% coinsurance for a one-month (31-day)
supply of drugs
- 25% coinsurance for a three-month (93-
day) supply of drugs
- 25% coinsurance for a 93-day supply of
drugs
Long Term Care Pharmacy
Generic
- $0 copay for a one-month (31-day) supply
of drugs
Preferred Brand
- $35 copay for a one-month (31-day) supply
of drugs
Non-Preferred Brand
- $70 copay for a one-month (31-day) supply
of drugs
Specialty Drugs
- 25% coinsurance for a one-month (31-day)
supply of drugs
Mail Order
Generic
- $0 copay for a one-month (31-day) supply
of drugs
- $0 copay for a three-month (93-day) supply
of drugs
14 H5729 013_CO0531 (11/07)
- $0 copay for a 93-day supply of drugs
Preferred Brand
- $35 copay for a one-month (31-day) supply
of drugs
- $105 copay for a three-month (93-day)
supply of drugs
- $105 copay for a 93-day supply of drugs
Non-Preferred Brand
- $70 copay for a one-month (31-day) supply
of drugs
- $210 copay for a three-month (93-day)
supply of drugs
- $210 copay for a 93-day supply of drugs
Specialty Drugs
- 25% coinsurance for a one-month (31-day)
supply of drugs
- 25% coinsurance for a three-month (93-
day) supply of drugs
- 25% coinsurance for a 93-day supply of
drugs
Coverage Gap
You pay the following:
The plan covers All Generics through the
gap.
Retail Pharmacy
Generic
- $0 copay for a one-month (31-day) supply
of drugs
- $0 copay for a three-month (93-day) supply
of drugs
- $0 copay for a 93-day supply of drugs
Long Term Care Pharmacy
Generic
- $0 copay for a one-month (31-day) supply
of drugs
Mail Order
Generic
- $0 copay for a one-month (31-day) supply
of drugs
- $0 copay for a three-month (93-day) supply
of drugs
15 H5729 013_CO0531 (11/07)
- $0 copay for a 93-day supply of drugs
For all other covered drugs, after your total
yearly drug costs reach $2850, you pay 100%
until your yearly out-of-pocket drug costs
reach $4050.
Catastrophic Coverage
After your yearly out-of-pocket drug costs
reach $ 4050, you pay the greater of:
- $ 2.25 copay for generic (including brand
drugs treated as generic) and $ 5.60 copay for
all other drugs, or
- 5% coinsurance.
Out-of-Network
Plan drugs may be covered in special
circumstances, for instance, illness while
traveling outside of the plan's service area
where there is no network pharmacy. You
may pay more than the copay if you get your
drugs at an out-of-network pharmacy.
Out-of-Network Initial Coverage
You pay the following until total yearly drug
costs reach $2850:
Out-of-Network Pharmacy
Generic
- $0 copay for a one-month (31-day) supply
of drugs
- $0 copay for a (29-day) supply of drugs
Preferred Brand
- $35 copay for a one-month (31-day) supply
of drugs
- $35 copay for a (29-day) supply of drugs
Non-Preferred Brand
- $70 copay for a one-month (31-day) supply
of drugs
- $70 copay for a (29-day) supply of drugs
Specialty Drugs
- 25% coinsurance for a one-month (31-day)
supply of drugs
- 25% coinsurance for a (29-day) supply of
drugs
Out-of-Network Coverage Gap
You pay the following:
16 H5729 013_CO0531 (11/07)
Generic
- $0 copay for a one-month (31-day) supply
of drugs
- $0 copay for a (29-day) supply of drugs
Out-of-Network Catastrophic Coverage
After your yearly out-of-pocket drug costs
reach $ 4050, you pay the greater of:
- $ 2.25 copay for generic (including brand
drugs treated as generic) and $ 5.60 copay for
all other drugs, or
- 5% coinsurance.
30 - Dental Preventive dental services (such as In-Network
Services cleaning) not covered. $0 copay for Medicare-covered dental
benefits
$0 copay for the following preventive dental
benefits:
- up to 2 oral exam(s) every year
- up to 2 cleaning(s) every year
- fluoride treatments
- up to 1 dental x-ray(s) every year
31 - Hearing Routine hearing exams and General
Services hearing aids not covered. Authorization rules may apply.
20% coinsurance for diagnostic In-Network
hearing exams. $0 copay for diagnostic hearing exams
- routine hearing tests
- fitting-evaluations for a hearing aid
$0 copay for up to $600 hearing aid(s) every
three years.
32 - Vision 20% coinsurance for diagnosis and General
Services treatment of diseases and Authorization rules may apply.
conditions of the eye.
Routine eye exams and glasses not In-Network
covered. $0 copay for diagnosis and treatment for
diseases and conditions of the eye
Medicare pays for one pair of and up to 1 routine eye exam(s) every year
eyeglasses or contact lenses after
cataract surgery.
Annual glaucoma screenings $0 copay for
covered for people at risk. - one pair of eyeglasses or contact lenses
after each cataract surgery
- up to 1 pair(s) of glasses every year
- up to 1 pair(s) of contacts every year
17 H5729 013_CO0531 (11/07)
33 - Physical 20% coinsurance for one exam In-Network
Exams within the first 6 months of your $0 copay for routine exams.
new Medicare Part B coverage
When you get Medicare Part B, Limited to 1 exam(s) every year.
you can get a one time physical
exam within the first 6 months of
your new Part B coverage. The
coverage does not include lab
tests.
Health/Wellness Not covered. General
Education Authorization rules may apply.
In-Network
This plan covers health/wellness education
benefits.
- Nursing Hotline
Transportation Not covered. General
Authorization rules may apply.
(Routine) In-Network
$0 copay for up to 12 one-way trip(s) to plan-
approved location every year.
18 H5729 013_CO0531 (11/07)
Vous aimerez peut-être aussi
- A Better Medicare. A Better You: MD Medicarechoice, IncDocument19 pagesA Better Medicare. A Better You: MD Medicarechoice, Inclancastd54Pas encore d'évaluation
- Medicare Part D DissertationDocument7 pagesMedicare Part D DissertationPayToWritePaperSingapore100% (1)
- Summary of Benefits: For Bcbsga Mediblue Access (Ppo)Document44 pagesSummary of Benefits: For Bcbsga Mediblue Access (Ppo)J MillerPas encore d'évaluation
- Ppo BR MD Pref Sta PR VaDocument16 pagesPpo BR MD Pref Sta PR VaMichael D ReevesPas encore d'évaluation
- Medicare Part C Medicare AdvantageDocument3 pagesMedicare Part C Medicare AdvantageJonathan CoutiñoPas encore d'évaluation
- HumanaChoice SNP-DE H5216-267 Summary of BenefitsDocument24 pagesHumanaChoice SNP-DE H5216-267 Summary of Benefitsadela EstradaPas encore d'évaluation
- Medicare AssignmentDocument13 pagesMedicare AssignmentmivbciwlfPas encore d'évaluation
- Maximize Your Medicare (2019 Edition): Understanding Medicare, Protecting Your Health, and Minimizing CostsD'EverandMaximize Your Medicare (2019 Edition): Understanding Medicare, Protecting Your Health, and Minimizing CostsÉvaluation : 5 sur 5 étoiles5/5 (1)
- Summary of Benefits: Humana Gold Plus H1036-237 (HMO)Document20 pagesSummary of Benefits: Humana Gold Plus H1036-237 (HMO)Cesar HPas encore d'évaluation
- Scope of Appointment Form 2011 UniversalDocument2 pagesScope of Appointment Form 2011 UniversalvmgreekPas encore d'évaluation
- Welcome To Medicare!: Things To Think About When You Compare Medicare Drug CoverageDocument4 pagesWelcome To Medicare!: Things To Think About When You Compare Medicare Drug CoverageAlsayed General HospitalPas encore d'évaluation
- Summary, Analysis & Review of Philip Moeller’s Get What’s Yours for MedicareD'EverandSummary, Analysis & Review of Philip Moeller’s Get What’s Yours for MedicarePas encore d'évaluation
- Understanding MedicareDocument4 pagesUnderstanding Medicare1224adhPas encore d'évaluation
- 2011 Medicare & You BookletDocument136 pages2011 Medicare & You Bookletgmen869101Pas encore d'évaluation
- Medicare: Socialsecurity - GovDocument24 pagesMedicare: Socialsecurity - Govtreb trebPas encore d'évaluation
- Medicare Private Fee For Service PlansDocument28 pagesMedicare Private Fee For Service PlansMabz BuanPas encore d'évaluation
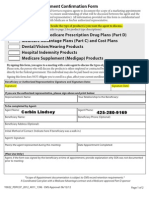
- 2013 Scope of Appointment Form - CORBINDocument2 pages2013 Scope of Appointment Form - CORBINCorbin LindseyPas encore d'évaluation
- Coordination of Benefits: Where Can I Get More Information?Document2 pagesCoordination of Benefits: Where Can I Get More Information?api-309082881Pas encore d'évaluation
- Ba25180st Rev0912 WBDocument6 pagesBa25180st Rev0912 WBJamesMyersPas encore d'évaluation
- Summary of Benefits: Humana Gold Plus H1036-065C (HMO)Document20 pagesSummary of Benefits: Humana Gold Plus H1036-065C (HMO)Cesar HPas encore d'évaluation
- Social Security / Medicare Handbook for Federal Employees and Retirees: All-New 4th EditionD'EverandSocial Security / Medicare Handbook for Federal Employees and Retirees: All-New 4th EditionPas encore d'évaluation
- 2006 Medicare Part D Payments: Total Drug Spend Troop Out of Pocket Cost Portion Covered by MedicareDocument5 pages2006 Medicare Part D Payments: Total Drug Spend Troop Out of Pocket Cost Portion Covered by MedicareVinodh KumarPas encore d'évaluation
- MedicareMedicaid PDFDocument4 pagesMedicareMedicaid PDFAlexanderPas encore d'évaluation
- Scope of Appointment FormDocument2 pagesScope of Appointment Formapi-260208821Pas encore d'évaluation
- 4 Ways To Help Lower Your Medicare Prescription Drug Costs: Revised July 2013Document2 pages4 Ways To Help Lower Your Medicare Prescription Drug Costs: Revised July 2013api-239463541Pas encore d'évaluation
- 2020 Benefits Information Guide: Understanding Your Options Staffing EmployeesDocument28 pages2020 Benefits Information Guide: Understanding Your Options Staffing Employeeseric.risnerPas encore d'évaluation
- Medicare Questions AnsweredDocument8 pagesMedicare Questions Answeredhazareerubina54Pas encore d'évaluation
- N202669852876 Template012 131071016 09 22 2020 05 19 17 ENDocument8 pagesN202669852876 Template012 131071016 09 22 2020 05 19 17 ENmaraki2012Pas encore d'évaluation
- Fan Understanding The Insurance ProcessDocument12 pagesFan Understanding The Insurance ProcessWill SackettPas encore d'évaluation
- ALL Medicare Is Health InsuranceDocument2 pagesALL Medicare Is Health InsuranceJoni RasmantoPas encore d'évaluation
- Coordination of Benefits: Tell Your Insurance Company or Employer Benefits Administrator About ChangesDocument2 pagesCoordination of Benefits: Tell Your Insurance Company or Employer Benefits Administrator About Changesapi-239463541Pas encore d'évaluation
- Medicare Campaign KnowledgeDocument4 pagesMedicare Campaign Knowledgeگل جہان سلیم بگھورPas encore d'évaluation
- PharmacyDocument182 pagesPharmacylancastd54Pas encore d'évaluation
- Membership Handbook PDFDocument44 pagesMembership Handbook PDFAli BariPas encore d'évaluation
- ACA 100 BrochureDocument20 pagesACA 100 BrochureSeverumxPas encore d'évaluation
- What You Should Know If You Need Medicare-Covered Equipment or SuppliesDocument8 pagesWhat You Should Know If You Need Medicare-Covered Equipment or SuppliescartilemeaPas encore d'évaluation
- Different Types of Medicare Insurance PlanDocument7 pagesDifferent Types of Medicare Insurance PlanGetmy PolicyPas encore d'évaluation
- Medicare MedicaidDocument4 pagesMedicare Medicaidarnab dasPas encore d'évaluation
- Version Updated - 3/1/2021: .,.. ... LSTN, FRSTDocument2 pagesVersion Updated - 3/1/2021: .,.. ... LSTN, FRSTRajaPas encore d'évaluation
- Anthem Scope of App.Document2 pagesAnthem Scope of App.family-institutePas encore d'évaluation
- For Your InformationDocument146 pagesFor Your InformationrambabuPas encore d'évaluation
- A Guide for Medical Case Managers: Stop Loss Insurance for Medical ProfessionalsD'EverandA Guide for Medical Case Managers: Stop Loss Insurance for Medical ProfessionalsPas encore d'évaluation
- CMS-10611 MOON 2023 - v508Document2 pagesCMS-10611 MOON 2023 - v508bwiettingPas encore d'évaluation
- Documentation for Skilled Nursing & Long-Term Care: A Guide for Occupational TherapistsD'EverandDocumentation for Skilled Nursing & Long-Term Care: A Guide for Occupational TherapistsPas encore d'évaluation
- Training Manual (New)Document16 pagesTraining Manual (New)fahhad lashari100% (3)
- CME Beginners Gude Medicare EbookDocument5 pagesCME Beginners Gude Medicare EbookAnonymous qEHjKlXjPas encore d'évaluation
- Rapidcare Medical Billing ManualDocument93 pagesRapidcare Medical Billing Manualapi-19789919100% (3)
- UHC Description of BenefitsDocument9 pagesUHC Description of BenefitsSebastián GuevaraPas encore d'évaluation
- State Health Exchanges and Qualified Health PlansDocument49 pagesState Health Exchanges and Qualified Health PlansRajiv GargPas encore d'évaluation
- BCBSIL Multistate Premier 2 SummaryDocument10 pagesBCBSIL Multistate Premier 2 SummaryMark MaPas encore d'évaluation
- ComprKaiehensive FormularyDocument77 pagesComprKaiehensive Formularypeter_rabbitPas encore d'évaluation
- Senior Mag AdDocument1 pageSenior Mag AdmtfifePas encore d'évaluation
- Smileeee 86826468Document7 pagesSmileeee 86826468Frvrkpop LifePas encore d'évaluation
- 2015 CA Eg Vision n2 FlyDocument2 pages2015 CA Eg Vision n2 FlyivotronPas encore d'évaluation
- Assignment of Benefits MedicareDocument6 pagesAssignment of Benefits Medicarepmojoumpd100% (1)
- 11037Document4 pages11037api-309082881Pas encore d'évaluation
- EligibilityResultsNotice PDFDocument13 pagesEligibilityResultsNotice PDFCarla PaezPas encore d'évaluation
- My Docs Mdmedicare InfoDocument4 pagesMy Docs Mdmedicare Infolancastd54Pas encore d'évaluation
- MdmedichaoiceDocument324 pagesMdmedichaoicelancastd54Pas encore d'évaluation
- 001Document18 pages001lancastd54Pas encore d'évaluation
- MD Medicarechoice Florida Optimum MB: Section I - Introduction To The Summary of Benefits ForDocument18 pagesMD Medicarechoice Florida Optimum MB: Section I - Introduction To The Summary of Benefits Forlancastd54Pas encore d'évaluation
- My Docs Mdmedicare InfoDocument4 pagesMy Docs Mdmedicare Infolancastd54Pas encore d'évaluation
- PharmacyDocument182 pagesPharmacylancastd54Pas encore d'évaluation
- PharmacyDocument182 pagesPharmacylancastd54Pas encore d'évaluation
- 001Document18 pages001lancastd54Pas encore d'évaluation
- MD Medicarechoice Florida Optimum MB: Section I - Introduction To The Summary of Benefits ForDocument18 pagesMD Medicarechoice Florida Optimum MB: Section I - Introduction To The Summary of Benefits Forlancastd54Pas encore d'évaluation
- MD Medicarechoice Florida Optimum MB: Section I - Introduction To The Summary of Benefits ForDocument18 pagesMD Medicarechoice Florida Optimum MB: Section I - Introduction To The Summary of Benefits Forlancastd54Pas encore d'évaluation
- PharmacyDocument182 pagesPharmacylancastd54Pas encore d'évaluation
- 001Document18 pages001lancastd54Pas encore d'évaluation
- MD Medicarechoice Florida Optimum MB: Section I - Introduction To The Summary of Benefits ForDocument18 pagesMD Medicarechoice Florida Optimum MB: Section I - Introduction To The Summary of Benefits Forlancastd54Pas encore d'évaluation
- PharmacyDocument182 pagesPharmacylancastd54Pas encore d'évaluation
- PharmacyDocument182 pagesPharmacylancastd54Pas encore d'évaluation
- 001Document18 pages001lancastd54Pas encore d'évaluation
- MdmedichaoiceDocument324 pagesMdmedichaoicelancastd54Pas encore d'évaluation