Académique Documents
Professionnel Documents
Culture Documents
Angina
Transféré par
Cheryl SmithDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Angina
Transféré par
Cheryl SmithDroits d'auteur :
Formats disponibles
TESTBANK
Chapter Title: Cardiovascular Disorders
Chapter #: 16
1. Data concerning coronary artery disease (CAD) and specific risk factors has demonstrated: 1. a low correlation of modifiable risk factors to coronary artery disease. 2. the onset of coronary artery disease in middle age. 3. an association between development of specific risk factors and CAD. 4. no decisive correlation between risk factors and CAD. 2. Which of the following values, when elevated, places the patient at lowest risk for CAD? 1. Very low-density lipoproteins (VLDL) 2. Triglycerides 3. Low-density lipoproteins (LDL) 4. High-density lipoproteins (HDL) 3. The major hemodynamic effect of CAD is: 1. decreased left ventricular end-diastolic volume. 2. decreased left ventricular end-diastolic pressure. 3. disturbance in the balance between myocardial oxygen supply and demand. 4. increased coronary artery vessel lumen. 4. One differentiating factor between stable angina and unstable angina is that stable angina: 1. responds predictably well to vasodilators. 2. is not precipitated by activity. 3. has a low correlation to coronary artery disease. 4. is a result of coronary artery spasm. 5. Nursing management of the patient with angina is directed toward: 1. immediate administration of nitrates. 2. assessment of history of previous anginal episodes. 3. assessment and documentation of chest pain episodes. 4. administration of prophylactic lidocaine for ventricular ectopy. 6. The mechanism most responsible for a myocardial infarction (MI) is: 1. coronary artery thrombi. 2. plaque fissure or hemorrhage. 3. coronary artery spasm. 4. preinfarction angina. 7. The most frequent dysrhythmia seen initially with sudden cardiac death is: 1. premature ventricular contractions. 2. ventricular tachycardia. 3. ventricular fibrillation. 4. asystole.
Copyright 2003, Elsevier Science (USA). All rights reserved.
8. Assessment of the patient with pericarditis may reveal which of the following signs and symptoms? 1. Ventricular gallop; substernal chest pain 2. Narrowed pulse pressure; shortness of breath 3. Pericardial friction rub; pain 4. Pericardial tamponade; widened pulse pressure 9. Clinical manifestations of right-sided heart failure include: 1. elevated central venous pressure and sacral edema. 2. pulmonary congestion and jugular venous distention. 3. hypertension and chest pain. 4. liver tenderness and pulmonary edema. 10. An essential aspect of teaching that may prevent reoccurrence of heart failure is: 1. notifying the physician if there is a 2-pound weight gain in 24 hours. 2. compliance with diuretic therapy. 3. taking nitroglycerin if chest pain occurs. 4. assessment of an apical pulse. 11. Compensatory mechanisms may be activated when heart failure occurs. In general, these mechanisms: 1. may worsen the degree of heart failure. 2. are effective in maintaining cardiac output for prolonged periods of time. 3. assist in decreasing preload and afterload. 4. minimize hypertrophic changes in the ventricles. 12. Which of the following assessment findings is most specific for acute onset of pulmonary edema? 1. Pulmonary crackles 2. Peripheral edema 3. Pink, frothy sputum 4. Elevated central venous pressure 13. Medical management of hypertrophic cardiomyopathy includes: 1. beta-blockers. 2. positive inotropes. 3. intensive exercise regimen. 4. aortic valve replacement. 14. Patient teaching regarding valvular heart disease should include which of the following? 1. Increase fluid intake to increase cardiac output. 2. Monitor and increase sodium intake to replace sodium lost with diuretics. 3. Increase daily activity until shortness of breath occurs. 4. Prophylactic antibiotics should be taken before undergoing any invasive procedure. 15. Which medication may be administered to the patient with hypertensive crisis? 1. Digitalis 2. Vasopressin 3. Verapamil 4. Sodium nitroprusside
Copyright 2003, Elsevier Science (USA). All rights reserved.
16. The classic description of pain associated with aortic dissection is: 1. substernal pressure. 2. tearing in the chest, abdomen, or back. 3. numbness and tingling in the left arm. 4. patient is asymptomatic. 17. Which of the following clinical manifestations is usually the first symptom of arterial peripheral vascular disease? 1. Intermittent claudication 2. Thrombophlebitis 3. Pulmonary embolism 4. Cordlike veins 18. You are teaching a patient with endocarditis about his diagnosis. Which statement below is correct? 1. Endocarditis is a viral infection that is easily treated with antibiotics. 2. The risk of this diagnosis is occlusion of the coronary arteries. 3. A long course of antibiotics is needed to treat this disorder. 4. Complications are rare once antibiotics have been started. 19. Questions 19-22 refer to the following situation. Mr. M. is a 66-year-old man admitted to the coronary care unit with a
diagnosis of acute inferior myocardial infarction. A 12-lead ECG is taken to validate the area of infarction. Which finding on the ECG is most conclusive for infarction? 1. Inverted T waves 2. Tall, peaked T waves 3. ST-segment depression 4. Q waves
20. Which leads on Mr. M.s ECG correlate with an inferior wall MI? 1. II, III, aVF 2. I, aVL 3. V2-V4 4. V5-V6 21. Complications post-MI are common. The nurse should anticipate which of the following as the most common complication? 1. Pulmonary edema 2. Cardiogenic shock 3. Dysrhythmias 4. Sudden cardiac death 22. Which classification of dysrhythmia is most common following an inferior wall myocardial infarction? 1. Sinus tachycardia 2. Premature atrial contractions 3. Atrial fibrillation 4. AV heart block 23. Which of the following cholesterol values indicate a heightened risk for the development of coronary artery disease? 1. Total cholesterol level of 170 mg/dL 2. HDL-C level of 30 mg/dL 3. Triglyceride level of 120 mg/dL 4. LDL-C level of 90 mg/dL
Copyright 2003, Elsevier Science (USA). All rights reserved.
24. A patient with known CAD in the CCU with chest pain is suddenly awakened with severe chest pain. Three NTG sublingual
tablets are administered 5 minutes apart without relief. A 12-lead ECG reveals non-specific ST segment elevation. This patient is probably suffering from which of the following? 1. Silent ischemia 2. Stable angina 3. Unstable angina 4. Prinzmetals angina
25. A patient has been newly diagnosed with stable angina. He tells you he knows a lot about his diagnosis already because his
father had the same thing 15 years ago. You ask him to tell you what he already knows about angina. Which of the following responses by the patient have a sound scientific basis? 1. He can not drink iced, cold beverages. 2. He can no longer drink colas or coffee. 3. He can no longer get a strong back massage. 4. He should not strain when going to the bathroom.
26. A patient presents with severe substernal chest pain. The patient states, This is the most severe pain I have ever felt! The
patient reports that the pain came on suddenly about 2 hours ago and that three NTG sublingual tablets have not relieved the pain. The 12-lead ECG reveals only the following abnormalities: T-wave inversion in leads I, aVL, V4 and V5 Pathologic Q-waves in leads II, III, and aVF ST segment elevation in leads V1, V2, V3, V4 Which of the following is probably accurate about this patient? 1. This patient has had an old lateral wall infarction. 2. This patient is having an inferior wall infarction. 3. This patient is having an acute anterior wall infarction. 4. This patient is having a posterior wall infarction.
27. A patient, 3 days following an anterior wall MI, is in the CCU. She is currently receiving, O2 at 4 L/min via nasal cannula,
NTG paste 1 q6 hours, and the beta blocker Lopressor 25 mg PO q12 hours. The monitor shows that she begins to have PVCs. Over the course of the next several hours, the PVCs increase in frequency, to more than 15 per minute, with occasional runs of multifocal bigeminal PVCs. The patient's vital signs are: HR 84 SR with described PVCs, BP 124/68, RR 20, SpO2 92%. Laboratory values are blood pH 7.44, potassium 4.4, and magnesium 1.2. Which of the following, if ordered, would be inappropriate for this patient? 1. Lidocaine 100 mg IVP 2. Increase O2 to 6 L/min via nasal cannula 3. Potassium chloride 40 mEq in 250 cc 0.9% saline IVPB over 4 hours 4. Magnesium sulfate 2 gm IVPB over 2 hours
28. A 45-year-old patient is admitted to the CCU with a diagnosis of acute myocardial infarction. Nitroglycerin is infusing at 10
mcg/min and heparin at 1000 units/hr. Which of the following statements would be appropriate at this time? 1. You will be able to resume normal sexual activity when you are discharged. 2. You will need to decrease your fat intake to reduce the risk of another heart attack 3. You have been admitted to the critical care unit because there has been damage to your heart muscle. 4. Angina is usually relieved by rest, but a heart attack isnt.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Vous aimerez peut-être aussi
- Heart Failure in ChildrenDocument47 pagesHeart Failure in ChildrenDr.P.NatarajanPas encore d'évaluation
- ShockDocument11 pagesShockNatalia WiryantoPas encore d'évaluation
- ACLS Drugs (2010)Document16 pagesACLS Drugs (2010)RN333100% (2)
- High Acuity Exam 1 Study Guide - 2Document12 pagesHigh Acuity Exam 1 Study Guide - 2Angelica WilliamsPas encore d'évaluation
- Questions & Answers: CardiologyDocument77 pagesQuestions & Answers: CardiologyDev Yadav100% (1)
- Clin Cardiology CasesDocument34 pagesClin Cardiology CasesSunny Singh0% (1)
- Cardio ExamDocument6 pagesCardio ExamDemp Almiranez100% (1)
- Ischemic Heart Disease PWDocument13 pagesIschemic Heart Disease PWEunica RamosPas encore d'évaluation
- Acynotic DiseaseDocument55 pagesAcynotic DiseaseTesfamichael AbathunPas encore d'évaluation
- MOH Pocket Manual in Emergency MedicineDocument244 pagesMOH Pocket Manual in Emergency MedicineAli Al-Brahim (AlucardAli)Pas encore d'évaluation
- Self-Assessment: BOFs for MRCP(UK) and MRCP(I) Part ID'EverandSelf-Assessment: BOFs for MRCP(UK) and MRCP(I) Part IPas encore d'évaluation
- CVS & Hypolipidemic Drugs-NursingDocument71 pagesCVS & Hypolipidemic Drugs-NursingManikanta Guptha100% (1)
- Peripheral Vascular Diseases NCLEXDocument6 pagesPeripheral Vascular Diseases NCLEXPotchiee PfizerPas encore d'évaluation
- NCLEX Practice ExamDocument10 pagesNCLEX Practice ExamJune DumdumayaPas encore d'évaluation
- NCLEX Exam Cardiovascular Surgery CareDocument5 pagesNCLEX Exam Cardiovascular Surgery CareHeather ClemonsPas encore d'évaluation
- Myocardial Infarction and Heart Failure NCLEXDocument22 pagesMyocardial Infarction and Heart Failure NCLEXPotchiee PfizerPas encore d'évaluation
- Hypertension NCLEX Quiz Questions: A. I Will Make Sure I Consume Foods High in PotassiumDocument5 pagesHypertension NCLEX Quiz Questions: A. I Will Make Sure I Consume Foods High in PotassiumMelodia Turqueza GandezaPas encore d'évaluation
- Ekg QuestionsDocument18 pagesEkg QuestionsEvidence Chaibva100% (1)
- Coronary Artery Disease & Hypertension NCLEX ReviewDocument15 pagesCoronary Artery Disease & Hypertension NCLEX ReviewPotchiee Pfizer0% (1)
- NCLEX Exam 2 Prioritization QuestionsDocument5 pagesNCLEX Exam 2 Prioritization QuestionsParallelPas encore d'évaluation
- Coronary Artery Disease (CAD) NCLEX QuestionsDocument7 pagesCoronary Artery Disease (CAD) NCLEX QuestionsMelodia Turqueza GandezaPas encore d'évaluation
- Cardio Quiz For NSG 128 HDocument22 pagesCardio Quiz For NSG 128 HMac MacapilPas encore d'évaluation
- Nclex ExamDocument18 pagesNclex Examwaqas_xsPas encore d'évaluation
- Anxiety Nitroglycerin: Myocardial InfarctionDocument135 pagesAnxiety Nitroglycerin: Myocardial InfarctionDefensor Pison Gringgo0% (1)
- MS 1 Examination 2 ReviewerDocument11 pagesMS 1 Examination 2 ReviewerJeon CookyPas encore d'évaluation
- YeDocument39 pagesYeRhea RaveloPas encore d'évaluation
- Laporan Tutorial Kelompok 1 Skenario 2Document11 pagesLaporan Tutorial Kelompok 1 Skenario 2Anita Dwi srirahayuPas encore d'évaluation
- Manage Angina with Morning RoutinesDocument58 pagesManage Angina with Morning RoutinesTherealnazareth 22Pas encore d'évaluation
- Cardiovascular Problems of The Adult ClientDocument16 pagesCardiovascular Problems of The Adult ClientMarylle AntonioPas encore d'évaluation
- Cardiology Question BankDocument45 pagesCardiology Question BankMadhu SowmithaPas encore d'évaluation
- CompilationDocument41 pagesCompilationARNANTE, SOPHIA ROSE D.Pas encore d'évaluation
- Terms in This Set (69) : Coronary Artery Disease & Hypertension Practice Quiz (50 Questions)Document25 pagesTerms in This Set (69) : Coronary Artery Disease & Hypertension Practice Quiz (50 Questions)Melodia Turqueza GandezaPas encore d'évaluation
- Cast Study 1Document4 pagesCast Study 1Thelda Mae Arteche SablanPas encore d'évaluation
- Cric2018 7237454Document4 pagesCric2018 7237454Muhammad Nur Ardhi LahabuPas encore d'évaluation
- Hypertensive Urgency and Emergency ModuleDocument8 pagesHypertensive Urgency and Emergency ModuleWest AfricaPas encore d'évaluation
- Heath Day 4 Care Plan 3Document12 pagesHeath Day 4 Care Plan 3api-639508852Pas encore d'évaluation
- Mitral Stenosis For Non-Cardiac Surgery Case FileDocument4 pagesMitral Stenosis For Non-Cardiac Surgery Case Filehttps://medical-phd.blogspot.comPas encore d'évaluation
- QuestionsDocument55 pagesQuestionsInchic MirandaPas encore d'évaluation
- NCLEX Review Cardiovascular QuizDocument17 pagesNCLEX Review Cardiovascular Quizdany tesemaPas encore d'évaluation
- Internship Exam: 1. Student NameDocument9 pagesInternship Exam: 1. Student NameMohamed fawzyPas encore d'évaluation
- Cardiac MI, HF, Angina and Cardiomyopathy Symptoms and TreatmentDocument13 pagesCardiac MI, HF, Angina and Cardiomyopathy Symptoms and Treatmentacque100% (1)
- CardioDocument7 pagesCardioGerald AndrinPas encore d'évaluation
- Surgery Task 11Document9 pagesSurgery Task 11Qmobile J5Pas encore d'évaluation
- Department of Internal Medicine II and Physiotherapy Myocarditis CaseDocument36 pagesDepartment of Internal Medicine II and Physiotherapy Myocarditis CaseSuba Saravanan 12Pas encore d'évaluation
- Materi MCQDocument15 pagesMateri MCQRaqqi PujatmikoPas encore d'évaluation
- Fluid Management in HFDocument47 pagesFluid Management in HFPandu AnggoroPas encore d'évaluation
- Prophecy General ICU RN A v2 UpdatedDocument6 pagesProphecy General ICU RN A v2 Updatedikazifaith6Pas encore d'évaluation
- Practice Quiz (50 Questions) - You Scored 2 Out of 50. Your Performance Has BeenDocument35 pagesPractice Quiz (50 Questions) - You Scored 2 Out of 50. Your Performance Has BeenMelodia Turqueza GandezaPas encore d'évaluation
- Practice Quiz (50 Questions) - You Scored 2 Out of 50. Your Performance Has BeenDocument35 pagesPractice Quiz (50 Questions) - You Scored 2 Out of 50. Your Performance Has BeenMelodia Turqueza GandezaPas encore d'évaluation
- Patho SGD: Cardiovascular Module Case 1Document4 pagesPatho SGD: Cardiovascular Module Case 1carmina_guerreroPas encore d'évaluation
- UntitledDocument17 pagesUntitledJohanisa SultanPas encore d'évaluation
- PBL PgamboaDocument6 pagesPBL PgamboaLeanne Princess GamboaPas encore d'évaluation
- CVADocument4 pagesCVACloyd Marvin Pajas SegundoPas encore d'évaluation
- Cardiac Disease in Pregnancy: Diagnosis and Management (39Document39 pagesCardiac Disease in Pregnancy: Diagnosis and Management (39Wai Kwong ChiuPas encore d'évaluation
- Orthopedic: Complications of FracturesDocument11 pagesOrthopedic: Complications of FracturesDrAyyoub AbboodPas encore d'évaluation
- Riyadh Ali 4/9/12 MDSC3311Document6 pagesRiyadh Ali 4/9/12 MDSC3311Hugh JacobsPas encore d'évaluation
- Case 5Document16 pagesCase 5Hany ElbarougyPas encore d'évaluation
- April 2018 1522659614 97Document2 pagesApril 2018 1522659614 97Rohit ThakarePas encore d'évaluation
- Nclex PRDocument4 pagesNclex PRJagveer ChauhanPas encore d'évaluation
- Cardiac Case Study on Coronary Artery Disease RiskDocument4 pagesCardiac Case Study on Coronary Artery Disease RiskElizabeth SpokoinyPas encore d'évaluation
- Ojsadmin, 1034Document5 pagesOjsadmin, 1034杨嘉宜Pas encore d'évaluation
- B BlockersDocument5 pagesB BlockersBo GrayPas encore d'évaluation
- How To Detect Long QT in A Heartbeat - Clinical ViewDocument9 pagesHow To Detect Long QT in A Heartbeat - Clinical ViewAlberto MHPas encore d'évaluation
- Curriculum VitaeDocument61 pagesCurriculum VitaeGalal ElsaidPas encore d'évaluation
- Multi-Specialty Hospital: Ram Sharada Healthcare Pvt. LTDDocument48 pagesMulti-Specialty Hospital: Ram Sharada Healthcare Pvt. LTDsubhash goelPas encore d'évaluation
- Levo-Milri 2021Document7 pagesLevo-Milri 2021Fer AlmazanPas encore d'évaluation
- Acute Viral Myocarditis: Diagnosis: Paul A. Checchia, MD Thomas J. Kulik, MDDocument4 pagesAcute Viral Myocarditis: Diagnosis: Paul A. Checchia, MD Thomas J. Kulik, MDCarkos MorenoPas encore d'évaluation
- 1st Case AnswerDocument2 pages1st Case Answersebaelabd777Pas encore d'évaluation
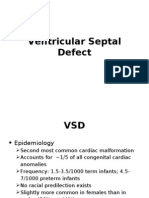
- Ventricular Septal DefectDocument8 pagesVentricular Septal DefectMarina RotaruPas encore d'évaluation
- The Pediatric ECG: Mahrus Abdur Rahman Cardiology Division Pediatric DepartmentDocument34 pagesThe Pediatric ECG: Mahrus Abdur Rahman Cardiology Division Pediatric DepartmentKharisma UtamaPas encore d'évaluation
- CPRDocument45 pagesCPRJames Elwood DoyolaPas encore d'évaluation
- ECG Short Note Chula EP PDFDocument62 pagesECG Short Note Chula EP PDFKhuniok SixcoPas encore d'évaluation
- Acls 11Document13 pagesAcls 11ezzat salemPas encore d'évaluation
- Acyanotic CHDDocument83 pagesAcyanotic CHDmrinmayee deshmukhPas encore d'évaluation
- 01-09 2022 Pharm Chronic Care in Cardiology 2022 R4Document62 pages01-09 2022 Pharm Chronic Care in Cardiology 2022 R4Amira HelayelPas encore d'évaluation
- Pem. Cardiovaskular Dr. MulyadiDocument195 pagesPem. Cardiovaskular Dr. MulyadiBettry Ahmad100% (1)
- 2020 - ESC Guidelines On Sports Cardiology and Exercise in Patients With Cardiovascular DiseaseDocument80 pages2020 - ESC Guidelines On Sports Cardiology and Exercise in Patients With Cardiovascular DiseaseHector VillamarinPas encore d'évaluation
- Bootcamp's Step 1 Study ScheduleDocument8 pagesBootcamp's Step 1 Study Schedulecfqbcm5swbPas encore d'évaluation
- 2022 영어 서울 A 인문 문제Document10 pages2022 영어 서울 A 인문 문제giyean5863Pas encore d'évaluation
- Chest Pain Algorithm Clinical Case Scenarios PDF 243970669Document28 pagesChest Pain Algorithm Clinical Case Scenarios PDF 243970669Romelu MartialPas encore d'évaluation
- CPG Coronary Artery DiseaseDocument44 pagesCPG Coronary Artery DiseaseReuter Lloyd MarianoPas encore d'évaluation
- Building For Change: Comparative Case Study of Hospital ArchitectureDocument14 pagesBuilding For Change: Comparative Case Study of Hospital ArchitectureDayalan 07Pas encore d'évaluation
- CRT Exam Test QuestionsDocument4 pagesCRT Exam Test QuestionsDharlyn MungcalPas encore d'évaluation
- Ventricular Septal DefectDocument9 pagesVentricular Septal DefectpepotchPas encore d'évaluation
- 2019 - SAGE - MICS Aortic Valve Replacement With Sutureless Valves, International Prospective RegistryDocument11 pages2019 - SAGE - MICS Aortic Valve Replacement With Sutureless Valves, International Prospective RegistryOmán P. Jiménez A.Pas encore d'évaluation
- Cardiac TamponadeDocument2 pagesCardiac TamponadechoobiPas encore d'évaluation
- International Journal of Scientific Research: General MedicineDocument4 pagesInternational Journal of Scientific Research: General MedicineTriple APas encore d'évaluation
- Heart Disease and Arrhythmia GuideDocument4 pagesHeart Disease and Arrhythmia GuideSellappan MuthusamyPas encore d'évaluation