Académique Documents
Professionnel Documents
Culture Documents
Craniotomy
Transféré par
andrea_zolayvarDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Craniotomy
Transféré par
andrea_zolayvarDroits d'auteur :
Formats disponibles
INTRODUCTION
A craniotomy is a procedure to remove a lesion in the brain through an opening in the skull (cranium). Purpose: A craniotomy is a type of brain surgery. It is the most commonly performed surgery for brain tumor removal . It also may be done to remove a blood clot (hematoma), to control hemorrhage from a weak, leaking blood vessel (cerebral aneurysm), to repair arteriovenous malformations (abnormal connections of blood vessels), to drain a brain abscess, to relieve pressure inside the skull, to perform a biopsy, or to inspect the brain. Demographics :Because craniotomy is a procedure that is utilized for several conditions and diseases, statistical information for the procedure itself is not available. However, because craniotomy is most commonly performed to remove a brain tumor, statistics concerning this condition are given. Approximately 90% of primary brain cancers occur in adults, more commonly in males between 55 and 65 years of age. Tumors in children peak between the ages of three and 12. Brain tumors are presently the most common cancer in children (four out of 100,000). Description :There are two methods commonly utilized by surgeons to open the skull. Either an incision is made at the nape of the neck around the bone at the back (occipital bone) or a curving incision is made in front of the ear that arches above the eye. The incision penetrates as far as the thin membrane covering the skull bone. During skin incision the surgeon must seal off many small blood vessels because the scalp has a rich blood supply. The scalp tissue is then folded back to expose the bone. Using a high-speed drill, the surgeon drills a pattern of holes through the cranium (skull) and uses a fine wire saw to connect the holes until a segment of bone (bone flap) can be removed. This gives the surgeon access to the inside of the skill and allows him to proceed with surgery inside the brain. After removal of the internal brain lesion or other procedure is completed, the bone is replaced and secured into position with soft wire. Membranes, muscle, and skin are sutured into position. If the lesion is an aneurysm, the affected artery is sealed at the leak. If there is a tumor, as much of it as possible is resected
(removed). For arteriovenous malformations, the abnormality is clipped and the repair redirects the blood flow to normal vessels.
Diagnosis/Preparation : Since the lesion is in the brain, the surgeon uses imaging studies to definitively identify it. Neuroimaging is usually accomplished by the following:
CT (computed tomography, uses x-rays and injection of an intravenous dye to visualize the lesion) MRI ( magnetic resonance imaging , uses magnetic fields and radio waves to visualize a lesion)
In a craniotomy, the skin over a part of the skull is cut and pulled back (A). Small holes are drilled into the skull (B), and a special saw is used to cut the bone between the holes (C). The bone is removed, and a tumor or other defect is visualized and repaired (D). The bone is replaced (E), and the skin closed (F). ( Illustration by GGS Inc.
arteriogram (an x-ray of blood vessels injected with a dye to visualize a tumor or cerebral aneurysm)
Before surgery the patient may be given medication to ease anxiety and to decrease the risk of seizures, swelling, and infection after surgery. Blood thinners (Coumadin, heparin, aspirin ) and nonsteroidal anti-inflammatory drugs (ibuprofen, Motrin, Advil, aspirin, Naprosyn, Daypro) have been correlated with an increase in blood clot formation after surgery. These medications must be discontinued at least seven days before the surgery to reverse any blood thinning effects. Additionally, the surgeon will order routine or special laboratory tests as needed. The patient should not eat or drink after midnight the day of surgery. The patient's scalp is shaved in the operating room just before the surgery begins.
Aftercare : Craniotomy is a major surgical procedure performed under general anesthesia. Immediately after surgery, the pa tient's pupil reactions are tested, mental status is assessed after anesthesia, and movement of the limbs (arms/legs) is evaluated. Shortly after surgery, breathing exercises are started to clear the lungs. Typically, after surgery patients are given medications to control pain, swelling, and seizures. Codeine may be prescribed to relive headache. Special leg stockings are used to prevent blood clot formation after surgery. Patients can usually get out of bed in about a day after surgery and usually are hospitalized for five to 14 days after surgery. The bandages on the skull are be removed and replaced regularly. The sutures closing the scalp are removed by the surgeon, but the soft wires used to reattach the portion of the skull that was removed are permanent and require no further attention. Patients should keep the scalp dry until the sutures are removed. If required (depending on area of brain involved), occupational therapists and physical therapist assess the patient's status postoperatively and help the patient improve strength, daily living skills and capabilities, and speech. Full recovery may take up to two months, since it is common for patients to feel fatigued for up to eight weeks after surgery.
Risks : The surgeon will discuss potential risks associated with the procedure. Neurosurgical procedures may result in bleeding, blood clots, retention of fluid causing swelling (edema), or
unintended injury to normal nerve tissues. Some patients may develop infections. Damage to normal brain tissue may cause damage to an area and subsequent loss of brain function. Loss of function in specific areas can cause memory impairment. Some other examples of potential damage that may result from this procedure include deafness, double vision, numbness, paralysis, blindness, or loss of the sense of smell.
Normal results : Normal results depend on the cause for surgery and the patient's overall health status and age. If the operation was successful and uncomplicated recovery is quick, since there is a rich blood supply to the area. Recovery could take up to eight weeks, but patients are usually fully functioning in less time.
Morbidity and mortality rates:There is no information about the rates of diseases and death specifically related to craniotomy. The operation is performed as a neurosurgical intervention for several different diseases and conditions.
Alternatives: There are no alternative treatments if a neurosurgeon deems this procedure as necessary.
WHO PERFORMS THE PROCEDURE AND WHERE IS IT PERFORMED? The procedure is performed in a hospital with a neurosurgery department and an intensive care unit . The procedure is performed by a board certified neurosurgeon, who has completed two years of general surgery training and five years of neurosurgical training.
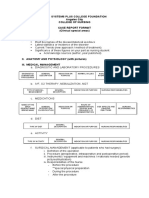
ANATOMY AND PHYSIOLOGY
Skull: Cranium and Facial Bones
Figure 2 The sagittal section and interior view of the skull's bones.
Fontanels are spaces between cranial bones that are filled with fibrous membranes. The spaces provide pliability for the skull when it passes through the birth canal and for brain growth during infancy. Bone growth eventually fills the spaces by age two. Sutural (Wormian) bones are very small bones that develop within sutures. Their number and location vary. The cranial vault denotes the top, sides, front, and back of the cranium. The cranial floor (base) denotes the bottom of the cranium. Cranial fossae are three depressions in the floor of the cranium. These fossae, called the anterior, middle, and posterior cranial fossae, provide spaces that accommodate the shape of the brain. The nasal cavity is formed by cartilage and several bones. Air entering the cavity is warmed and cleansed by mucus lining the cavity. Sinuses (paranasal sinuses) are mucus-lined cavities inside cranial and facial bones that surround the nasal cavity. The cavities secrete mucus that drains into the nasal cavity. The cavities also act as resonance chambers that enhance vocal (and singing) quality.
Pathophysiology
Vous aimerez peut-être aussi
- CraniotomyDocument6 pagesCraniotomychaSephPas encore d'évaluation
- Craniotomy Surgical Case ReportDocument54 pagesCraniotomy Surgical Case ReportTep BinwagPas encore d'évaluation
- CraniotomyDocument8 pagesCraniotomySyed AbudaheerPas encore d'évaluation
- CraniectomyDocument5 pagesCraniectomytabanaoPas encore d'évaluation
- Craniotomy: Brain Tumors Aneurysms AvmsDocument5 pagesCraniotomy: Brain Tumors Aneurysms AvmsMichael Cody SoPas encore d'évaluation
- Craniotomy or CraniectomyDocument14 pagesCraniotomy or CraniectomyEssaj Rosanat100% (2)
- Craniotomy Case ReportDocument19 pagesCraniotomy Case ReportElizar MercadoPas encore d'évaluation
- CraniotomyDocument16 pagesCraniotomyKarell Eunice Estrellado GutierrezPas encore d'évaluation
- Craniotomy and CraniectomyDocument5 pagesCraniotomy and CraniectomyCarlcedrick ManlapusPas encore d'évaluation
- Diagnostic Imaging ProceduresDocument6 pagesDiagnostic Imaging ProceduresMichaela JapsayPas encore d'évaluation
- Mastectomy: Prepared By: Hilario, Eunice Lamoste, Jenebelle Lopez, Maria SofiaDocument34 pagesMastectomy: Prepared By: Hilario, Eunice Lamoste, Jenebelle Lopez, Maria SofiaSofia LopezPas encore d'évaluation
- HNPDocument7 pagesHNPLyka Mae Imbat - Pacnis100% (1)
- Community Diagnosis Sample PDFDocument2 pagesCommunity Diagnosis Sample PDFLisaPas encore d'évaluation
- Case StudyDocument27 pagesCase Studyapi-313356122Pas encore d'évaluation
- Cerebral Aneurysms: Aneurysms Posterior Circulation Basilar Artery Vertebral Arteries Posterior Communicating ArteryDocument10 pagesCerebral Aneurysms: Aneurysms Posterior Circulation Basilar Artery Vertebral Arteries Posterior Communicating ArteryRani SujithPas encore d'évaluation
- Obstructive Uropathy Secondary To Benign Prostatic HyperplasiaDocument74 pagesObstructive Uropathy Secondary To Benign Prostatic HyperplasiaGregory Litang100% (1)
- Cochlear Implant Surgery Treatment & Management - Medical Therapy, Surgical Therapy, Preoperative DetailsDocument9 pagesCochlear Implant Surgery Treatment & Management - Medical Therapy, Surgical Therapy, Preoperative DetailsFityah UfiPas encore d'évaluation
- CVDDocument67 pagesCVDRachel PerandoPas encore d'évaluation
- Case Presentation 1Document70 pagesCase Presentation 1shadow gonzalezPas encore d'évaluation
- Nso AbdurasadDocument4 pagesNso AbdurasadNader AbdurasadPas encore d'évaluation
- Lyceum of The Philippines University - Batangas CollegeDocument120 pagesLyceum of The Philippines University - Batangas CollegeKMPas encore d'évaluation
- Neurological DisordersDocument7 pagesNeurological Disordersomicspublishinggroup100% (1)
- Cerebral AngiographyDocument9 pagesCerebral AngiographyVincent LopezPas encore d'évaluation
- PCAP-C Endorsement NotesDocument2 pagesPCAP-C Endorsement NotesLorraine GambitoPas encore d'évaluation
- Pericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerDocument2 pagesPericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerlhenPas encore d'évaluation
- Teaching Plan Pain Management HandoutDocument1 pageTeaching Plan Pain Management HandoutCassandraPas encore d'évaluation
- Cerebrovascular Accident (Stroke)Document15 pagesCerebrovascular Accident (Stroke)mesdejen100% (1)
- Uremic EncephalophatyDocument48 pagesUremic EncephalophatySindi LadayaPas encore d'évaluation
- Glasgow Coma ScaleDocument13 pagesGlasgow Coma ScaleDanna Christine Gumboc PaguntalanPas encore d'évaluation
- IschemicheartdiseaseDocument11 pagesIschemicheartdiseaseZaimon MaulionPas encore d'évaluation
- DX Fracture PDFDocument8 pagesDX Fracture PDFSherree HayesPas encore d'évaluation
- Mastectomy (Case Analysis)Document7 pagesMastectomy (Case Analysis)Lester_Ocuaman_2248Pas encore d'évaluation
- Cardio QuizDocument100 pagesCardio QuizEvidence ChaibvaPas encore d'évaluation
- Bedside Teaching BenefitsDocument13 pagesBedside Teaching BenefitsDave GawaranPas encore d'évaluation
- Case Study For Pleural-EffusionDocument10 pagesCase Study For Pleural-EffusionGabbii CincoPas encore d'évaluation
- MastectomyDocument6 pagesMastectomyJustinAlmedaPas encore d'évaluation
- Pleural Fluid Analysis: How The Test Is PerformedDocument4 pagesPleural Fluid Analysis: How The Test Is PerformedKevin LlorentePas encore d'évaluation
- Case Study Medical WardDocument4 pagesCase Study Medical WardFrancis Antonio Llenaresas QuijanoPas encore d'évaluation
- EVD Drainage DeviceDocument5 pagesEVD Drainage DeviceSze Ching WanPas encore d'évaluation
- Hirschprungs DiseaseDocument26 pagesHirschprungs DiseaseAndrian PramanaPas encore d'évaluation
- Thoracentesis Reflective EssayDocument2 pagesThoracentesis Reflective EssayAnjae GariandoPas encore d'évaluation
- Pituitary DwarfismDocument9 pagesPituitary DwarfismPuteri Azman100% (1)
- Pulmonary AngiographyDocument3 pagesPulmonary AngiographyBiway RegalaPas encore d'évaluation
- Multiple Choice Question Acn FinalDocument11 pagesMultiple Choice Question Acn FinalIqra rizwanPas encore d'évaluation
- Oesophageal Atresia by GabriellaDocument7 pagesOesophageal Atresia by GabriellaGabriellePas encore d'évaluation
- Triage and Priority SettingDocument10 pagesTriage and Priority SettingekonurcahyaningrumPas encore d'évaluation
- Acute Glomerulonephritis (AGN) : Group A Beta Hemolytic StretococcusDocument3 pagesAcute Glomerulonephritis (AGN) : Group A Beta Hemolytic StretococcusKristine Danielle DejeloPas encore d'évaluation
- Asking Your Question (PICO) - NursingDocument5 pagesAsking Your Question (PICO) - NursingBentaigaPas encore d'évaluation
- Causes, Symptoms and Treatment of AtelectasisDocument4 pagesCauses, Symptoms and Treatment of AtelectasisAshley Jane MacapayadPas encore d'évaluation
- About Critical Care NursingDocument7 pagesAbout Critical Care NursingaivynPas encore d'évaluation
- Cardiac Case Study on Coronary Artery Disease RiskDocument4 pagesCardiac Case Study on Coronary Artery Disease RiskElizabeth SpokoinyPas encore d'évaluation
- Case Study 1 FinalDocument28 pagesCase Study 1 Finalapi-3905968320% (1)
- Assignment On GCSDocument2 pagesAssignment On GCSPraty SawadenPas encore d'évaluation
- Patient ChartDocument2 pagesPatient ChartHydiePas encore d'évaluation
- Spinal Cord Injury Case Study (Physical Assessment)Document3 pagesSpinal Cord Injury Case Study (Physical Assessment)TobiDaPas encore d'évaluation
- TFN Trans 1Document2 pagesTFN Trans 1Chilled Moo MooPas encore d'évaluation
- A Ann CraniotomyDocument41 pagesA Ann CraniotomyF̳̿a̳̿l̳̿a̳̿h̳̿ Opcional S̳̿u̳̿d̳̿i̳̿r̳̿a̳̿d̳̿i̳̿r̳̿e̳̿j̳̿a̳̿Pas encore d'évaluation
- Transcultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodDocument5 pagesTranscultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodeuLa-mayzellPas encore d'évaluation
- Brief Description of The Disease/statistical IncidenceDocument2 pagesBrief Description of The Disease/statistical IncidenceLeanne Princess Gamboa100% (1)
- Careers in Social Work: Outlook, Pay & MoreDocument9 pagesCareers in Social Work: Outlook, Pay & Morejoel lacayPas encore d'évaluation
- STIs O & GDocument59 pagesSTIs O & GNoraPas encore d'évaluation
- Manual On Minimum Standards of Care in Addiction Treatment CentresDocument61 pagesManual On Minimum Standards of Care in Addiction Treatment CentresGlobal Law FirmPas encore d'évaluation
- Epithelioid Hemangioendothelioma of The Superior Vena - 2022 - Archivos de BroncDocument1 pageEpithelioid Hemangioendothelioma of The Superior Vena - 2022 - Archivos de Broncguidance mtisiPas encore d'évaluation
- Culturally Competent For NursesDocument9 pagesCulturally Competent For Nursesleli khairaniPas encore d'évaluation
- DMSCO Log Book Vol.40 1962Document73 pagesDMSCO Log Book Vol.40 1962Des Moines University Archives and Rare Book RoomPas encore d'évaluation
- Acute Care Surgery: Aryono D.Pusponegoro Warko KarnadihardjaDocument9 pagesAcute Care Surgery: Aryono D.Pusponegoro Warko KarnadihardjaDimas ErlanggaPas encore d'évaluation
- Bacon - Size Acceptance and IntuitIve Eating - JADA.05Document8 pagesBacon - Size Acceptance and IntuitIve Eating - JADA.05Evelyn Tribole, MS, RD100% (2)
- Natural Pregnancy and ParentingDocument70 pagesNatural Pregnancy and ParentingAmela SabicPas encore d'évaluation
- Pe-4 GR12 2ndsem 3RDQ Module 3 W5W6Document15 pagesPe-4 GR12 2ndsem 3RDQ Module 3 W5W6Leslie Joy Yata MonteroPas encore d'évaluation
- STRDocument179 pagesSTRJatin AnandPas encore d'évaluation
- KKM AmbulanceDocument49 pagesKKM Ambulanceyasin ghazaliPas encore d'évaluation
- Nursing Care of Children with Physiologic and Hematologic DisordersDocument17 pagesNursing Care of Children with Physiologic and Hematologic DisordersDgjj CompuiterPas encore d'évaluation
- Handwashing NarrativeDocument9 pagesHandwashing NarrativeMaria Angelica BermilloPas encore d'évaluation
- ALLIANCE DEFENSE FUND Demand Letter REGARDING CARYN DUTTON, M.D. AND PLANNED PARENTHOOD IN WISCONSINDocument6 pagesALLIANCE DEFENSE FUND Demand Letter REGARDING CARYN DUTTON, M.D. AND PLANNED PARENTHOOD IN WISCONSINcrush2482Pas encore d'évaluation
- 100 Papers in Clinical Psychiatry Psychosomatic Medicine Malingering in The Medical Setting.Document18 pages100 Papers in Clinical Psychiatry Psychosomatic Medicine Malingering in The Medical Setting.J. M. SolisPas encore d'évaluation
- The New Jose L. Amante Emergency HospitalDocument29 pagesThe New Jose L. Amante Emergency HospitalRiah Ramirez FojasPas encore d'évaluation
- INITIAL DATA BASE Form For Family 1Document5 pagesINITIAL DATA BASE Form For Family 1Reignallienn Inocencio MartinPas encore d'évaluation
- Chapter 3 FINAL Identification of The Impact of Disability & DifferentiatedDocument52 pagesChapter 3 FINAL Identification of The Impact of Disability & DifferentiatedHunde AdamuPas encore d'évaluation
- Case 10 Shutter IslandDocument3 pagesCase 10 Shutter IslandAnkith ReddyPas encore d'évaluation
- RA For SPT Test (Reviewed)Document5 pagesRA For SPT Test (Reviewed)shamshad ahamedPas encore d'évaluation
- The Effects of Foster Care Placement On Young Children's Mental HealthDocument6 pagesThe Effects of Foster Care Placement On Young Children's Mental HealthZefry Wahyu PurnamaPas encore d'évaluation
- Teacher's Guide: To The Magnificent Mei and Friends Comic SeriesDocument44 pagesTeacher's Guide: To The Magnificent Mei and Friends Comic SeriesVarizka SalsabilaPas encore d'évaluation
- TFNVirginia HendersonDocument13 pagesTFNVirginia HendersonJheslyn BalagulanPas encore d'évaluation
- Faculty of Sport Science and Recreation Diploma in Sport Studies (Sr1132D) Sps220 - Nutrition For Health and ExerciseDocument6 pagesFaculty of Sport Science and Recreation Diploma in Sport Studies (Sr1132D) Sps220 - Nutrition For Health and ExerciseSyafiq MiqhaelPas encore d'évaluation
- What Is Healing?Document33 pagesWhat Is Healing?Chef Jem100% (1)
- History and Mental Status Exam GuideDocument17 pagesHistory and Mental Status Exam Guideyeney armenterosPas encore d'évaluation
- Nurse ExamDocument17 pagesNurse ExamRn nadeen100% (2)
- NCM104-FNCP ColladoDocument3 pagesNCM104-FNCP ColladoProplays ytPas encore d'évaluation
- 485 5032 Assignment 1 Greenwich University PassDocument27 pages485 5032 Assignment 1 Greenwich University PassThy ThơPas encore d'évaluation