Académique Documents
Professionnel Documents
Culture Documents
Elesevier Knee
Transféré par
Ahmed El YamaniDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Elesevier Knee
Transféré par
Ahmed El YamaniDroits d'auteur :
Formats disponibles
The Knee 14 (2007) 39 45
Proprioception in the ACL-ruptured knee: The contribution of the medial collateral ligament and patellar ligament. An in vivo experimental study in the cat
N. Bonsfills a,, J.J. Raygoza b , E. Boemo b , J. Garrido b , A. Nez c , E. Gmez-Barrena d
a
Unidad de Ortopedia Peditrica, Hospital Universitario La Paz (Hospital Infantil), Paseo de la Castellana, 261, 28046 Madrid, Spain b Escuela Politcnica Superior, Universidad Autnoma de Madrid, Spain c Departamento de Morfologa, Facultad de Medicina, Universidad Autnoma de Madrid, Spain d Departamento de Ciruga, Facultad de Medicina, Universidad Autnoma de Madrid, Spain Received 5 June 2006; received in revised form 29 August 2006; accepted 14 September 2006
Abstract In the absence of anterior cruciate ligament (ACL), secondary restraints such as menisci, ligaments, and tendons restrict anterior knee laxity. Strain detection at these sites could define the contribution of this alternative signalling system to knee proprioception after ACL injury. The hypothesis in this study questions if measurements of anterior tibial translation (ATT) from surface strain gauges on the insertions of the medial collateral ligament (MCL) and the patellar tendon (PT) are sufficiently sensitive and specific to differentiate normal, stable knees from acutely unstable knees due to ACL section. Twelve cats received miniaturized strain gauges on the surface of MCL and PT distal insertions. A purpose-made receiver transformed into measurements any voltage variation obtained during passive knee flexionextension and anterior tibial translation manoeuvres. Variables under evaluation included first peak latency, normalized amplitude, and slope of voltage along time. Femorotibial displacements were video recorded, digitized, and used as the ATT reference. The proposed system detected significant changes in the slope of the voltage/time signal, with higher specificity and sensitivity during ATT after experimental ACL section. Changes were not significant during flexion or extension. It was found that a pattern of earlier and more intense strain in MCL and PT distal insertions was found during ATT in the ACL deficient knee. Enhanced pattern recognition learning from these structures could be a future target for proprioceptive training after ACL injury. 2006 Elsevier B.V. All rights reserved.
Keywords: Knee joint; Anterior cruciate ligament; Strain gauge; Knee instability assessment
1. Introduction In the absence of anterior cruciate ligament (ACL), secondary restraints such as menisci, ligaments, and tendons restrict anterior knee laxity. The most significant secondary restrictors to the ATT are the medial meniscus, the medial collateral ligament (MCL), the patellar tendon (PT) acting as a passive ligament, and the posterolateral corner structures [1]. These not only contribute to mechanical control of anterior knee laxity, but the remaining knee proprioception
Corresponding author. Tel.: +34 917277260. E-mail address: nbonsfills@epersonas.net (N. Bonsfills). 0968-0160/$ - see front matter 2006 Elsevier B.V. All rights reserved. doi:10.1016/j.knee.2006.09.003
after ACL injury is linked to the remaining articular and periarticular structures that intervene in the joint stabilisation during knee motion and activities. It has been hypothesized that these secondary restraints may be the proprioception agents in the ACL deficient knee [2], but their role is unclear. In the long-term, their inefficiency to properly signal the anterior tibial translation (ATT) that elicits a control response, may originate giving-way episodes. The assessment of in vivo instability in ACL-deficient knees would require a new strategy of stressstrain measurements in overloaded structures after ACL injury, like the MCL [3] or the PT [4]. Strain detection at these sites could define the contribution of this alternative signalling system to knee proprioception after
40
N. Bonsfills et al. / The Knee 14 (2007) 3945
Fig. 1. Process of data acquisition. Both electric signal and knee position are obtained simultaneously in video recordings. Anterior knee instability after ACL section in one movement is represented as a distance increase between markers for unstable knees (grey line) compared to stable knees (black lines). Error bars for the maximum tibial displacement are included, showing increased ATT after ACL section, with p b 0.01 for Student's t-test.
ACL injury. However, accurate detection of ATT is a difficult task. An excessive ATT at certain knee flexion angles is the standard evaluation of anterior knee laxity after ACL injury. Anterior translation values have been measured in humans,
with the help of devices such as KT-1000 or KT-2000 [5], and even in animals, with more or less sophisticated methods [6,7]. EMG has been used as an indirect technique of evaluating ATT during time, as muscular activity changes (amplitude and latency) may inform about the quadriceps and
N. Bonsfills et al. / The Knee 14 (2007) 3945
41
made to minimize animal suffering and the number of animals used in the experiments.
2.2. Strain gauges
Commercial strain gauges were used (Tokyo Sokki Kenkyujo Co., Ltd) to measure strain of both MCL and PT. The models used in this study were FLG-02-23 and FLK-1-23, whose resistive element consisted in a metal foil of nickelcopper alloy, on an Epoxy resin base. The size of isolating bases (1.4 to 4.5 mm) was adequate to be located on the selected ligament insertions. Both sensors had a basal resistance of 120 and were connected to the resistive piece through the gauge base, where expansion or contraction really occurs, and this was detected as changes of electrical resistance ( = R / 2.14R, being R the basal resistance of these models of strain gauges, and 2.14 a constant specific for each gauge). A constant current applied to the sensor produced voltage changes due to the resistance variation, proportional to strain. Sensor calibration was performed with a purposedesigned amplifier. Calibration of the baseline was set with the knee at rest, 90 flexed, and its variations in flexionextension were adapted to be detected in the range of 5 V. Post-mortem in vitro calibration showed potential sources of error [18], thus sensor calibration was repeated in each animal, as suggested for other transducers [21].
Fig. 2. Variable representation on a real register. L1 = First peak latency. A1 = First peak amplitude. SL1 = tan(a) = First peak slope.
hamstrings response to knee motion. However, these data are non-specific and highly variable among individuals [8]. Different devices have been developed to directly measure stress and strain in soft tissues. From stress measurement techniques to pressure detection, or even magnetic field properties to deduce strain, different authors explored sensor capabilities to detect knee instability [917]. Surface strain gauges based on electric variations of a metallic resistance [18,19] may be a simple way to detect surface tensile variations at ligament insertions, previously used in biomechanical experiments dealing with ligament stress in human cadaver knees [20]. Insertion location of the gauge would avoid confusion due to viscoelastic hysteresis at the ligament body during knee motion. Its sensitivity could be defined as the relationship of the output voltage per time or the output voltage per applied load [11]. We hypothesized that data from surface strain gauges on the insertions of secondary restraints to anterior tibial displacement due to ACL injury may be sufficiently sensitive and specific to differentiate stable from unstable knees after ACL injury, during anterior tibial displacement manoeuvres. Firstly, we aimed to detect if significant differences exist between gauge measurements at the MCL and the PT before and after ACL section. Secondly, we aimed to differentiate gauge measurements during ATT from those obtained during knee flexion and extension.
2. Methods 2.1. Animals
Twelve cats (weight 2.55 kg) obtained from a specialized dealer (Centro de Animales de Experimentacin, Universidad de Crdoba; Isoquimen Ltd., Barcelona) were anaesthetized with intraperitoneal pentobarbital (33 mg/dl, 100 mg/kg). Extra doses of anaesthesic were added when needed. Before surgery, each knee was examined by two different investigators to clinically ensure normal stability. Experiments were carried out in accordance with the European Community Council Directive (86/609/EEC), and all efforts were
2.3. Implantation surgery
An S-curved anterolateral approach to the knee was performed, from the lateral and proximal region of the knee (around 1.5 cm proximal to lateral femoral epicondyle) to the medial and distal region (1 cm distal to the tibial tuberosity). Then, both the distal insertion of the PT and the distal insertion of the MCL were carefully exposed. Both areas were denuded of any covering soft-tissues and, after careful haemostasis, one gauge was fixed to each ligament with cyanoacrilate of biological use (Histoacryl, Braun). This adhesive was also used to encapsulate and isolate the tips of sensor electrodes. These electrodes ended in a purpose-designed device amplifier where independent signals from each strain gauge were amplified and filtered. These signals were further digitized (100 samples/s) and stored as analogical inputs for off-line analysis by appropriate software (Sonolab, Sonometrics Corporation, Canada). Anterior tibial displacement was performed with a dynamometer up to 24.5 N, pulling from a transtibial Kirschner wire. Finally, reference markers to assess the displacement were inserted on the lateral femoral epicondyle, the anterior tibial tuberosity, and the fibula head.
2.4. Experiment protocol and video recording
Experiments on 15 knees from 12 anaesthetized cats consisted of series with ten repetitions in four different knee displacements: anterior tibial translation (ATT) in the 90 flexed knee, ATT in the 30 flexed knee, flexion, and extension. Anterior tibial translation that demonstrated anterior knee laxity was performed by the pull of a dynamometer at a transtibial Kirschner wire, to mimic clinical manoeuvres (anterior drawer test with the knee at 90 flexion, and Lachman's test with the knee at 30 flexion). Extension was defined as a passive movement of the knee from 90 to 0 flexion, while flexion was defined from 90 flexion to the maximum hyperflexion (usually, 150160 flexion), both with the hip 90 flexed. We performed one to four series (10 to 40 repetitions per movement). When the stable knee was studied, the anterior cruciate ligament was sectioned with a surgical blade through a lateral arthrotomy. After careful closure of the arthrotomy, the whole protocol was repeated again in the ACL-deficient knee. Video recordings of the anterior tibial displacement were performed to synchronize movement with the response of strain gauges. The experiments were video recorded using two Panasonic video cameras (models WVCP470 and WV-CP474E) with a video recording frequency of 50 Hz. To synchronize motion in the sagittal plane during the experiment with the strain gauge signal recordings of the Sonolab screen in one single screen, an image mixer device (Quad Processor, model n AVC704) was used. Signals
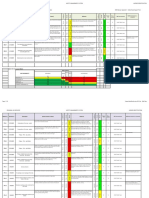
42 Table 1 Changes in the first peak slope after ACL section MCL Stable mean S.E. ATT 90 ATT 30 Flexion Extension 0.32 0.06 0.44 0.07 0.003 0.001 0.002 0.001
N. Bonsfills et al. / The Knee 14 (2007) 3945
PT Unstable mean S.E. 3.51 0.62 8.12 1.77 0.19 0.14 0.12 0.11 p values for the difference (b0.001) (b0.001) 0.5 0.6 Stable mean S.E. 0.29 0.06 0.47 0.07 1.67 1.67 0.08 0.08 Unstable mean S.E. 8.68 2.69 7.46 1.56 0.30 0.21 0.42 0.41 p values for the difference (b0.001) (b0.001) 0.4 0.5
MCL = medial collateral ligament, PT = patellar tendon. p values are given for MannWhitney's test. from the image mixer device was recorded with a VCR Sony SLV-SE620, and digitized through a Sony DV camera PCR110 (Fig. 1). were normalized to the maximum amplitude of each specimen. Increase of slope for both ligaments was calculated as percentage changes to the mean value. We performed a total number of 151 valid series of recordings (243 repetitions) for the MCL and 161 valid series (253 repetitions) for the PT in 12 knees. Results are expressed as mean standard error for all variables. Mean standardized values for stable and unstable knees were compared using MannWhitney's test, as KolmogorovSmirnov's test showed no normal distribution of the data. Significance was considered with p values under 0.05. Strain gauges sensitivity and specificity were calculated by comparison with ATT after clinical evaluation. Briefly, clinical evaluation of anterior tibial translation in ACL injuries, according to the IKDC score [22], includes 4 degrees (1+ to 4+). Each degree indicates increasing anterior displacement related to the tibial plateau sagittal length. We considered knees with an evaluation of 3+ or 4+ to be unstable when anterior tibial displacement was higher than 50% of proximal tibia sagittal length, and all the specimens were clinically classified as unstable after ACL section. The threshold value of each sensor variable to define instability was set on the mean value plus two standard deviations of stable knees values. Sensitivity and specificity were obtained for amplitude and slope of the two strain gauges.
2.5. Data processing
Signals were filtered (0.1100 Hz) and amplified. Continuously recorded data were sampled at 500 Hz and fed to a Macintosh computer for off-line analysis. Analysis of the response of each ligament strain gauge was performed in representative recordings for flexion, extension, and ATT series. The first three repetitions were discarded to avoid any adaptation changes. The recorded electric response of strain gauges was then processed with Sonoview software (Sonometrics Corporation, Canada). For each studied repetition, the obtained variables at both ligaments (MCL and PT) that underwent analysis included first peak latency (L1), first peak amplitude (A1), and first peak slope (Fig. 2). First peak slope (SL1) was the tangent of the first peak angle, and it represented the real timing of strain variations SL1 = A1 L 1. The start reference for each movement was 1 identified from video recording. Anterior tibial displacement was assessed measuring the markers' displacement during each movement, first in the stable knee and then in the same after ACL section. Sensor recording averages were calculated using the onset of the movement as the zero reference. To minimize specimen variability, amplitude and slope values
3. Results 3.1. Changes in anterior tibial translation Under constant traction of 24.5N, ATT as obtained from video recordings increased significantly after ACL section (Fig. 1). Mean values for ATT increased from 0.96 0.16 mm to 2.96 0.25 mm at 90 knee flexion, and from 1.27 0.20 mm to 2.37 0.57 mm at 30 knee flexion, both p b 0.001. This was parallel to an increase in the instability score of two grades. 3.2. Changes in ligament strain with anterior tibial traction After ACL section, the first peak amplitude increased when recorded both at the MCL (from 0.38 to 2.61 mV; p b 0.001) and at the PT gauge (from 0.36 to 3.26 mV; p b 0.001) during ATT with a 90 flexed knee. At the 30 flexed knee, voltage variations were similar (0.43 to 3.36 mV, p b 0.001, for MCL; 0.64 to 3.33 mV, p b 0.001 for PT). The first peak latency showed a statistically significant decrease during ATT 90 (MCL: 795.57 to 409.44 ms, p b 0.001; PT: 723.71 to 398.57 ms, p = 0.005), but not so clearly at ATT 30 (MCL: 532.32 to 371.79 ms, p = 0.03; PT: 495.2 to 360.55 ms, p = 0.09). However, the first peak slope was the variable that showed the most definite changes when the ACL was sectioned, and these are summarized in Table 1. The slope increase during ATT both at 90 and 30 flexion showed large increases at the MCL and at the PT. Percentage changes for slope are shown in Fig. 3, and revealed more than a 10-times increase during ATT. Thus, both sensors
Fig. 3. The first peak slope percentage changes after ACL section. MCL = Medial Collateral Ligament, PT = Patellar tendon. Significant changes with ACL section at the MannWhitney test are pointed.
N. Bonsfills et al. / The Knee 14 (2007) 3945 Table 2 Sensitivity and specificity for strain gauges variables to detect knee instability Amplitude Sens MCL ATT 90 ATT 30 Flexion Extension PT ATT 90 ATT 30 Flexion Extension 61.54% 76.19% 20.00% 27.27% Spec 86.67% 100.00% 100.00% 90.91% Latency Sens 30.77% 40.48% 33.33% 36.36% Spec 96.67% 93.55% 86.67% 81.82% Slope Sens 74.36% 80.95% 13.33% 9.09% Spec 90.00% 100.00% 93.33% 90.91%
43
48.65% 54.76% 16.67% 38.46%
97.06% 96.77% 94.44% 100.00%
5.41% 30.95% 16.67% 0.00%
97.06% 93.33% 83.33% 100.00%
72.97% 78.57% 0.00% 7.69%
85.29% 96.67% 94.44% 92.31%
Threshold for each variable was set on mean value + 2 S.D., for amplitude and slope, and mean S.D. for latency. MCL = medial collateral ligament, PT = patellar tendon, Sens = sensitivity, Spec = specificity.
showed high specificity to detect changes after ACL section (over 85%) during ATT, although sensitivity was not so high (over 70%), as shown in Table 2. 3.3. Changes in ligament strain with flexionextension Flexion and extension, however, produced a different effect in the gauges signals. No significant changes were observed in either the MCL or the PT gauges after ACL section (slope values are seen in Table 1). The increase in the signal amplitude, latency, and slope after ACL section, detected during ATT, was not present during knee flexion or extension. Besides, sensitivity to changes after ACL section was low during flexion or extension (between 0% and 40%, see Table 2). When the gauges response to knee flexion and ATT at 90 knee flexion were compared after ACL section, significantly higher values ( p b 0.001) were obtained after ATT at 90 for the slope (MCL gauge in flexion: 0.66, in ATT 90: 2.61; and PT gauge in flexion: 1.12, in ATT 90: 8.68), as well as for the amplitude and latency. Also, when the response to extension and ATT at 30 were compared after ACL section, significantly higher values ( p b 0.001) were obtained after ATT at 30 for the slope (MCL gauge in extension: 0.11, in ATT 30: 3.36; and PT gauge in extension: 0.42, in ATT 30: 3.33).
4. Discussion Biomechanical studies on ACL deficiency are abundant, as this injury is one of the most commonly addressed in orthopaedic biomechanics. Strain gauges have long been used in this research. Our approach, based on the investigation of secondary restraints to anterior tibial displacement when the ACL is absent, provides a different view of the problem that may help to explain changes of instability with time [7]. It also characterises periarticular muscle reaction in the evolution of an ACL deficient knee [2], providing the role of secondary restraints is clear. Defining and comparing knee instability and proprioception experimentally helps interpreting the neuromuscular changes after ACL injury [2325].
Neuromuscular studies on proprioception in the ACL deficient knee have been greatly advanced in the cat's knee as an experimental model, from the original description of articular nerve endings [26] to ligamentomuscular reflexes [27] or muscular reaction [17] and neural pathways [28]. Thus, it has allowed significant insight in knee proprioception currently, with a considerable body of literature to support it. This includes the fact that neural endings within articular structures are stimulated by strain. This proprioceptive potential passes to spinal ganglia and spinal cord, where a muscular reaction is mediated via a gamma loop [29]. This muscular reaction includes muscle tone regulation, which is affected following ACL injury due to a proprioceptive deficit [23]. In this context, the remaining proprioception should be located in the remaining mechanically competent structures, the secondary restraints, such as the MCL. Our study evaluated both the MCL and the patellar ligament as a passive restraint [4]; the latter also served as a control. If the muscular control is inadequate due to poor proprioception then instability and giving way will occur. This leads to the critical role of muscular reaction timing. With the aim of obtaining better time-dependent information about the ACL deficient knee, we planned surface strain detection in secondary restraints to anterior tibial displacement through gauges. Methodological issues include the use and location of strain gauges, the choice of variables providing useful information, and the unavoidable data variability. Regarding the use and location of gauges, we selected devices of small size and avoided implantation among ligament fibres that could distort the ligament function. These two aspects are important dealing with ACL deficient knees, were the use of DVRT [3032] or force probes and Hall effect-based transducers is difficult. Insertion placement skipped tissue disruption at the ligament body, leaving intact the ligament structure [33], and avoiding deformation or hysteresis at the ligament body. Thus, the obtained voltage variations were expected to more precisely reflect the tensional state at the secondary restraints, as signalled by others [4]. These gauges previously used in cadaver knees [20], permit in our study to detect strain on real time by studying a living system. Regarding the study variables, latency has been previously used [8,34] to compare a time-related response. First peak latency (the response delay) has been used to synchronize strain changes with other parameters (such as muscle electrical activity, measured ATT, stresses, etc.) [18,23]. Other authors studied voltage amplitude with time or with load [7,11,19]. However, latency and amplitude may be confounding variables as the starting point for latency may be inaccurate, and the voltage amplitude expresses a different reaction if spread along time. We then calculated the slope, a magnitude obtained from amplitude and time of the first peak in the recorded voltage, to address timedepending changes establishing a relationship between strain changes and time [11,35]. When other factors influencing the gauge output are under control, a higher slope indicates an
44
N. Bonsfills et al. / The Knee 14 (2007) 3945
earlier and more intense deformation under traction. This occurred in our study, especially in the MCL gauge during anterior tibial translation after ACL section. The final methodological problem was data variability, as voltage changes from the gauge can be affected by many factors. Although sensitivity of a single transducer was independent from room temperature, rotation of the knee, and number of cycles [11], other authors [17] found a 100% inter-specimen variation in strain measurements at the patellar tendon, using an IFT sensor. We decreased variability by following a precise protocol that included technique, position, calibration, and same researcher performing the manoeuvres, but a 30% variability coefficient indicated the same trend found by other investigators [17]. To cope with this variability, we normalized the amplitude values per specimen and performed sequential comparisons in the same knee, before and after ACL section. This study allowed us to conclude that gauges located on secondary restraints insertions clearly differentiate the knee before and after ACL section. This difference was not only related to intensity of the response, but also to its time distribution: a 10 to 40-fold increase in the response intensity vs. time (slope) was observed after ACL section. With high sensitivity (over 80%) and specificity (100%) during a Lachman-like maneuver, the MCL gauge was a good detector of anterior knee laxity in the absence of the ACL. The application of this result suggests that the MCL is able to detect a forced anterior tibial translation in the ACL-deficient knee, better than knee flexion or extension. The present experimental work is far from immediate clinical application. However, despite previous clinical experience and biomechanical studies, it was unclear how secondary restrictors respond in the ACL injured knee. Particularly, it was unclear whether if secondary restraints tensioning after ACL injury may stimulate their proprioceptive receptors differently during anterior tibial displacement than during flexionextension. This is important not only to understand real-time detection of anterior instability that occurs in the ACL-deficient knee, but also to understand how proprioceptive information obtained from those preserved structures can elicit a muscular response in the ACLdeficient knee. The same strain gauges have already detected increased tension in human collateral ligaments in knees submitted to anterior tibial traction at different knee angles [20]. We obtained similar patterns with in vivo strain gauges that could be useful to detect instability. An accurate instability detection can be used to feed a microprocessor that could differentiate stable and unstable knees, as showed by our group in preliminary work [36]. This understanding can help to program specific rehabilitation programs oriented to take advantage of preserved proprioception in secondary restraints such as the MCL. In conclusion, this is an experimental study obtaining the evidence that particularly the MCL can differentiate the anterior tibial translation from the knee flexion or extension when the ACL is not present, and this response can be
quantified. This suggests that secondary restraints may offer a substituting proprioceptive system when the proprioception is damaged due to ACL injury, and there are opportunities to better define clinical rehabilitation programs taking advantage of this preserved capability when the ACL is absent. This could include proprioceptive training programs to learn pattern recognition to elicit an early muscular response in the ACL-deficient knee through guided muscular stimulation. Knee proprioceptive remaining elements should be the aim of therapeutic approaches, as its potential to signal abnormal knee displacements has been verified in the ACL deficient knees. Acknowledgments This study was supported by a grant by F.I.S. (Fondo de Investigaciones Sanitarias; 01/0371). Conflict of interest statement. The authors state that there are no financial or personal relationships with other people or organisations that could influence their work. References
[1] McCarty E, Ibarra C, Torzilli P, Warren R. Ligament cutting studies. In: Pedowitz R, O'Connor J, Akeson W, editors. Daniel's knee injuries. Ligament and cartilage structure, function injury, and repair. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2003. p. 8196. [2] Gmez-Barrena E, Nez A, Martnez-Moreno E, Valls J, Munuera L. Neural and muscular electric activity in the cat's knee. Acta Orthop Scand 1997;68(2):14955. [3] Crisco J, Moore D, McGovern R. Strain-rate sensitivity of the rabbit MCL diminishes at traumatic loading rates. J Biomech 2002;35:137985. [4] Herzog W, Hasler E, Leonard T. In-situ calibration of the implantable force transducer. J Biomech 1996;29(12):164952. [5] Daniel D. Reference, Maintenance and User's Guide for the Knee Ligament Arthrometer. California: MEDmetric Corporation; 1993. [6] Hasler E, Herzog W. Quantification of in vivo patellofemoral contact forces before and after ACL transection. J Biomech 1998;31(1):3744. [7] Maitland M, Leonard T, Frank C, Shrive N, Herzog W. Method to assess in vivo knee stability longitudinally in an animal model of ligament injury. J Orthop Res 1998;16:4417. [8] Ageberg E. Consequences of a ligament injury on neuromuscular function and relevance to rehabilitation using the anterior cruciate ligamentinjured knee as model. J Electromyogr Kinesiol 2002;12:20512. [9] Fleming B, Peura G, Beynnon B. Factors influencing the output of an implantable force transducer. J Biomech 2000;33:88993. [10] Hall G, Crandall J, Carmines D, Hale J. Rate-independent characteristics of an arthroscopically implantable force probe in the human Achilles tendon. J Biomech 1999;32:2037. [11] Holden J, Grood E, Cummings J. Factors affecting sensitivity of a transducer for measuring anterior cruciate ligament force. J Biomech 1995;28(1):99102. [12] Korvick D, Cummings J, Grood E, Holden J, Feder S, Butler D. The use of an implantable force transducer to measure patellar tendon forces in goats. J Biomech 1996;29(4):55761. [13] Fleming B, Beynnon B, Tohyama H, Johnson R, Nichols C, Renstrm P, et al. Determination of a zero strain reference for the anteromedial band of the anterior cruciate ligament. J Orthop Res 1994;12:78995. [14] Beynnon B, Johnson R, Fleming B. The science of anterior cruciate ligament rehabilitation. Clin Orthop 2002;402:920.
N. Bonsfills et al. / The Knee 14 (2007) 3945 [15] Cholewicki J, Panjabi M, Nibu K, Macias M. Spinal ligament transducer based on a Hall effect sensor. J Biomech 1997;30(3):2913. [16] Hirokawa S, Yamamoto K, Kawada T. Circumferential measurement and analysis of strain distribution in the human ACL using a photoelastic coating method. J Biomech 2001;34:113543. [17] Herzog W, Archambault J, Leonard T, Nguyen H. Evaluation of the implantable force transducer for chronic tendon-force recordings. J Biomech 1996;29(1):1039. [18] Biewener A, Corning W. Dynamics of mallard (Anas platyrhynchos) gastrocnemius function during swimming versus terrestrial locomotion. J Exp Biol 2001;204:174556. [19] Williamson M, Dial K, Biewener A. Pectoralis muscle performance during ascending and slow level flight in mallards (Anas platyrhynchos). J Exp Biol 2001;204:495507. [20] Hinterwimmer S, Baumgart R, Plitz W. Tension changes in the collateral ligaments of a cruciate ligament-deficient knee joint: an experimental biomechanical study. Arch Orthop Trauma Surg 2002;122(8):4548. [21] Bach J, Hull M, Patterson H. Direct measurement of strain in the posterolateral bundle of the anterior cruciate ligament. J Biomech 1997;30(3):2813. [22] Johnson D, Smith R. Outcome measurement in the ACL deficient knee what's the score? Knee 2001;8:518. [23] Wojtys E, Huston L. Neuromuscular performance in normal and anterior cruciate ligament-deficient lower extremities. Am J Sports Med 1994;22(1):89104. [24] Beard D, Kyberd P, Fergusson C, Dodd C. Proprioception after rupture of the anterior cruciate ligament. An objective indication of the need of surgery? J Bone Jt Surg 1993;75-B(2):3115. [25] Jennings A, Seedhom B. Proprioception in the knee and reflex hamstring contraction latency. J Bone Jt Surg 1994;76-B(3):4914. [26] Freeman MA, Wyke B. The innervation of the knee joint. An anatomical and histological study in the cat. J Anat 1967;101(Pt 3):50532.
45
[27] Solomonow M, Baratta R, Zhou E, Shoji H, Bose W, Beck C, et al. The synergistic action of the anterior cruciate ligament and thigh muscles in maintaining joint stability. Am J Sports Med 1987;15 (3):20713. [28] Gmez-Barrena E, Martnez-Moreno E, Munuera L. Segmental sensory innervation of the anterior cruciate ligament and the patellar tendon of the cat's knee. Acta Orthop Scand 1996;67(6):54552. [29] Johansson H, Sjolander P, Sojka P. A sensory role for the cruciate ligaments. Clin Orthop Relat Res 1991(268):16178. [30] Beynnon B, Fleming B. Anterior cruciate ligament strain in vivo: a review of previous work. J Biomech 1998;31(6):51925. [31] Markolf K, Willems M, Jackson S, Finerman G. In situ calibration of miniature sensors implanted into the anterior cruciate ligament Part I: Strain measurements. J Orthop Res 1998;16:45563. [32] Markolf K, Willems M, Jackson S, Finerman G. In situ calibration of miniature sensors implanted into the anterior cruciate ligament Part II: Force probe measurements. J Orthop Res 1998;16:46471. [33] Hinterwimmer S, Plitz W. Strain measurement at the knee ligament insertion sites. Biomed Tech (Berl) 2003;48(12):114. [34] Fujita I, Nishikawa T, Kambic H, Andrish J, Grabiner M. Characterization of hamstrings reflexes during anterior cruciate ligament disruption: in vivo results from a goat model. J Orthop Res 2000;18:1839. [35] Enoka R. Describing motion. In: Enoka R, editor. Neuromechanics of Human Movement. Illinois: Human Kinetics; 2002. p. 615. [36] Raygoza-Panduro J, Ortega-Cisneros S, Boemo E, Gmez-Barrena E, Nez A, Bonsfills N. FPGAs implementation of digital electronic circuit to pattern clasification of knee instability. XVII Congreso Nacional y III Congreso Internacional de Informtica y Computacin; 2004 Octubre; Mxico; 2004.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Artificial Intelligence Questions&Ans Uninformed SearchDocument5 pagesArtificial Intelligence Questions&Ans Uninformed Searchjaijohnk83% (6)
- Bsee201 B - Fluid MechanicsDocument150 pagesBsee201 B - Fluid MechanicsMarvin GagarinPas encore d'évaluation
- Genetic AlgorithmDocument6 pagesGenetic AlgorithmShashikant ChaurasiaPas encore d'évaluation
- Flabeg Solar enDocument11 pagesFlabeg Solar enZeec NoorPas encore d'évaluation
- SensoNODE Catalog 3864 Feb 2015Document28 pagesSensoNODE Catalog 3864 Feb 2015btsgr parkerPas encore d'évaluation
- Imp For As400Document21 pagesImp For As400Dinesh ChaudhariPas encore d'évaluation
- September 2015Document2 pagesSeptember 2015Patriziah Marie SeldaPas encore d'évaluation
- HHW 35 m6 GBDocument6 pagesHHW 35 m6 GBSuper WhippedPas encore d'évaluation
- Hazard-Identification Dec 2015Document22 pagesHazard-Identification Dec 2015Dumitru EninPas encore d'évaluation
- Scenario of Shale Gas Exploration in IndiaDocument24 pagesScenario of Shale Gas Exploration in IndiaManish TiwariPas encore d'évaluation
- Role of QAQC Eng.Document38 pagesRole of QAQC Eng.arunkumar100% (2)
- A C +Haier+12000+BTUDocument51 pagesA C +Haier+12000+BTUfox7878Pas encore d'évaluation
- Aerospace MaterialsDocument68 pagesAerospace MaterialsAykut Üçtepe100% (1)
- Smart Obj. Kiss and SwotDocument5 pagesSmart Obj. Kiss and SwotjtopuPas encore d'évaluation
- Parts Catalog: F Y 8 - 3 1 F X - 0 0 0Document86 pagesParts Catalog: F Y 8 - 3 1 F X - 0 0 0julian gonzalezPas encore d'évaluation
- ABB LMU 574 - mcd80Document12 pagesABB LMU 574 - mcd80gadware2011bplPas encore d'évaluation
- ThaiREC Checklist-Barge Inspection Questionnaire GasDocument18 pagesThaiREC Checklist-Barge Inspection Questionnaire Gasเปีย วันชัย สวนทอง100% (1)
- ASTM D287-92 (Metodo de Prueba Estandar para Gravedad API de Petroleo Crudo y Productos Del Petroleo Metodo Del Hidrómetro)Document3 pagesASTM D287-92 (Metodo de Prueba Estandar para Gravedad API de Petroleo Crudo y Productos Del Petroleo Metodo Del Hidrómetro)Juan MonjePas encore d'évaluation
- SY-5SSM V1.1 SY-5SSM/5 V1.1 Super 7 Motherboard: User's Guide & Technical ReferenceDocument88 pagesSY-5SSM V1.1 SY-5SSM/5 V1.1 Super 7 Motherboard: User's Guide & Technical Referencealopezcuervo82190% (1)
- CSC 263Document108 pagesCSC 263osecaloPas encore d'évaluation
- Practical Considerations For The Use of A Howland Current SourceDocument4 pagesPractical Considerations For The Use of A Howland Current SourceRamiShaabannnnPas encore d'évaluation
- 02-Engine Mechanical System PDFDocument129 pages02-Engine Mechanical System PDFSigit Indrawan100% (1)
- TDS Tixatrol STDocument2 pagesTDS Tixatrol STJose E BatistaPas encore d'évaluation
- FD100 CatalogoDocument4 pagesFD100 CatalogoKaren VásconezPas encore d'évaluation
- Assignment 1Document4 pagesAssignment 1MikeyPas encore d'évaluation
- Manual PSW 2600Document18 pagesManual PSW 2600Jc C. GomezPas encore d'évaluation
- CT Terminology LexiconDocument12 pagesCT Terminology LexiconjtbushbergPas encore d'évaluation
- Grid Synchronization of Power Converters Using Multiple Second Order Generalized IntegratorsDocument6 pagesGrid Synchronization of Power Converters Using Multiple Second Order Generalized IntegratorsJandfor Tansfg ErrottPas encore d'évaluation
- Pakistani Radio MarketDocument72 pagesPakistani Radio MarketNajeeb Anwar100% (1)
- Project Title: Hotel Management Software Project: PurposeDocument3 pagesProject Title: Hotel Management Software Project: PurposesuryaPas encore d'évaluation