Académique Documents
Professionnel Documents
Culture Documents
Pad Pamphlet
Transféré par
Dapie LinganDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Pad Pamphlet
Transféré par
Dapie LinganDroits d'auteur :
Formats disponibles
PERIPHERAL ANGIOGRAM AND INTERVENTION
Your cardiologist has recommended a procedure called a Peripheral Arteriogram. Peripheral refers to those arteries which are located away from the center of the body (heart). One of the most common reasons for a peripheral arteriogram is the need to visualize the arteries which supply blood flow to the legs; however, arteriograms can be performed to obtain information regarding blood flow to the abdomen, kidneys, arms, and brain. At Cardiovascular Consultants, peripheral arteriograms are performed by an Interventional Cardiologist. The procedure is performed in the catheterization lab in the hospital. During the procedure, contrast dye, which appears white on x-ray, is injected into the blood vessel that is being studied. As the artery fills with the contrast, blockages can be seen. The image is digitally recorded and reviewed. With this information, the Interventional Cardiologist can offer you a treatment plan. Often the diagnostic angiogram and the treatment angioplasty can be performed in the same setting. The advisability of performing both procedures will be discussed with you by the Interventional Cardiologist. When peripheral angioplasty (PTA) is the recommended treatment, the blocked artery is opened by placing a thin tube (catheter) with a small balloon on the tip across the narrowed artery. Once positioned, the balloon is inflated and the blockage is compressed against the artery wall. The diameter of the artery is increased and blood flow is improved. A peripheral stent (expandable metal coil) may be inserted in the artery after the balloon inflation. Another approach is to reduce the size of the blockage with an atherectomy device. This can be accomplished with a laser, high speed rotating diamond tip burr, or shaving device that cuts and removes plaque. The development of new techniques and devices used in peripheral angioplasty is a rapidly changing field. The Interventional Team at Cardiovascular Consultants is on the cutting edge of this technology and research and can offer you the most current therapy available anywhere in the world. This might include participation in scientific trials.
COMMON ROUTINES Prior to the procedure When your peripheral arteriogram is scheduled, a nurse will review pre-procedure instructions. Blood tests will need to be obtained which give information concerning blood count, blood coagulation, kidney function, sodium and potassium and lipid status (blood fats). You will be requested to drink 6-8 large glasses of fluid (8 oz.) the day prior to your angiogram in order to maintain hydration and reduce the impact contrast dye may have on your kidneys. IF YOU ARE ALLERGIC TO CONTRAST DYE, you will be given special medication the night prior and the morning of the angiogram. PLEASE NOTIFY US IF YOU HAVE A CONTRAST ALLERGY. You will be NPO (nothing by mouth) except for medications and liquids after midnight. Persons with diabetes will be given special instructions.
You will be admitted to the hospital catheterization laboratory the morning of your procedure and spend a short time in the holding area. Your history, electrocardiogram, and preprocedure blood work will have been reviewed and you will meet members of the Interventional Team. In the holding area, the right and left groin site will be shaved in preparation for arterial access. An intravenous line will be started in your arm to provide a route for medication and fluid. You will be asked to sign a consent for the procedure. Your family will then be directed to the waiting room outside the cath lab. During the Procedure
The skin over the arterial access site will be cleansed with a cool antiseptic solution. The Interventional Cardiologist will inject the area with a local anesthetic. You will experience a momentary stinging sensation followed quickly by numbness. A small tube (sheath) is then inserted into the femoral artery and a smaller tube (catheter) is placed into the sheath and advanced to the artery being studied. Contrast (x-ray dye) which appears white on x-ray, is injected into the artery. As the dye fills the artery, x-ray pictures are recorded digitally. Based on the appearance of the blood vessel being studied, a decision will be made to stop after the pictures of the artery have been obtained or to proceed with the PTA. A peripheral angiogram can take an hour to perform. A peripheral intervention (PTA) can take an additional one to two hours to complete. After the Peripheral Angiogram ONLY You are transferred back to the holding area.
The sheath is removed and hand held pressure is applied to the site to prevent bleeding. A small bandage is placed on the groin site and you remain on bedrest for an additional four (4) hours. If a closure device is used, bedrest is two (2) hours. The decision to use a closure device is made by the Interventional Cardiologist. Clear liquids will be available as soon as the procedure is completed. Solid food will be offered after sheath removal.
If you are uncomfortable, pain medication will be available upon request. The nursing staff will be checking your heart rhythm, blood pressure and general well being closely. The nurse will also be assessing the procedure site for signs of bleeding complications. The Interventional Cardiologist will discuss the results of your peripheral angiogram and develop a treatment plan. If possible, your spouse, a family member, or a friend should be present for this discussion. Your primary care physician will promptly receive a letter describing your angiogram results and the treatment plan. Follow up exams post procedure will be arranged. After The Peripheral Intervention You are transferred to a special recovery unit for overnight observation and care. Several hours after the procedure, a blood test will be done to determine if the effect of the intravenous blood thinner (heparin) given during the procedure is reversed. Once anticoagulation is reversed, the sheath is removed. Hand held pressure is applied to the site to prevent bleeding. A small bandage is then placed on the groin site. You will remain on bedrest for an additional four (4) hours to make sure the site is stable and to prevent bleeding complications. If a closure device is placed at the end of the procedure, bedrest is two (2) hours. The decision to use a closure device (suture or collagen plug) will be made by the Interventional Cardiologist. Clear liquids will be available as soon as you are admitted to recovery. Solid food will be offered after sheath removal and as soon as you are able to tolerate an advanced diet. If you are uncomfortable, pain medication will be available upon request. The nursing staff will be checking your heart rhythm, blood pressure, and general well being closely. The nurse will also be assessing the procedure site for signs of bleeding complications.
DISMISSAL AFTER PTA You will spend the night of the procedure in the cardiovascular recovery unit (CVRU) and will be dismissed by the Interventional Team Advanced Practice Nurse between 10:00 a.m. and 2:00 p.m. on the following day.
The APN will review your procedure, perform a physical assessment, and discuss dismissal guidelines. This will include a discussion of risk factors contributing to peripheral arterial disease. If possible, your spouse, a family member, or friend should be present for this discussion. You will need to make arrangements for transportation home on the day of dismissal. Follow up will be one month post procedure and six months thereafter. At the six month visit, a duplex of the artery may be performed. You will then have regular annual exams to follow your progress. Upon dismissal, a letter will be sent to your primary care physician describing the procedure, hospital stay, and treatment recommendations. Peripheral Interventional Cardiologists Steven B. Laster, MD William C. Daniel, MD Steven P. Marso, MD David M. Safley, MD Dmitri Baklanov, MD Adnan Chhatriwalla, MD Interventional Advanced Practice Nurses Jan Dennis, RN, BC, M-CNS Kristi Calkins, RN, BC, ANP Diane Cunningham, RN, BC, ANP
Vous aimerez peut-être aussi
- MeningitisDocument70 pagesMeningitisDapie LinganPas encore d'évaluation
- CHED Memorandum Order # 5 (2008)Document121 pagesCHED Memorandum Order # 5 (2008)wiredpsyche100% (69)
- DengueDocument12 pagesDengueDapie LinganPas encore d'évaluation
- Clinical Teaching PlanDocument3 pagesClinical Teaching PlanDapie Lingan83% (18)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Eu Clinical TrialDocument4 pagesEu Clinical TrialAquaPas encore d'évaluation
- Cs205-E S3dec18 KtuwebDocument2 pagesCs205-E S3dec18 KtuwebVighnesh MuralyPas encore d'évaluation
- Crown BeverageDocument13 pagesCrown BeverageMoniruzzaman JurorPas encore d'évaluation
- Chemical Classification of HormonesDocument65 pagesChemical Classification of HormonesetPas encore d'évaluation
- Your Bentley Bentayga V8: PresentingDocument9 pagesYour Bentley Bentayga V8: PresentingThomas SeiferthPas encore d'évaluation
- 24 Inch MonitorDocument10 pages24 Inch MonitorMihir SavePas encore d'évaluation
- 30 de Thi Hoc Ky 2 Mon Tieng Anh Lop 9 Co Dap An 2023Document64 pages30 de Thi Hoc Ky 2 Mon Tieng Anh Lop 9 Co Dap An 2023Trần MaiPas encore d'évaluation
- CSR Report On Tata SteelDocument72 pagesCSR Report On Tata SteelJagadish Sahu100% (1)
- Activity Sheet Housekeeping Week - 8 - Grades 9-10Document5 pagesActivity Sheet Housekeeping Week - 8 - Grades 9-10Anne AlejandrinoPas encore d'évaluation
- Capital Structure and Leverage: Multiple Choice: ConceptualDocument53 pagesCapital Structure and Leverage: Multiple Choice: ConceptualArya StarkPas encore d'évaluation
- SLTMobitel AssignmentDocument3 pagesSLTMobitel AssignmentSupun ChandrakanthaPas encore d'évaluation
- UK Tabloids and Broadsheet NewspapersDocument14 pagesUK Tabloids and Broadsheet NewspapersBianca KissPas encore d'évaluation
- HUAWEI PowerCube 500Document41 pagesHUAWEI PowerCube 500soumen95Pas encore d'évaluation
- A Quantitative Method For Evaluation of CAT Tools Based On User Preferences. Anna ZaretskayaDocument5 pagesA Quantitative Method For Evaluation of CAT Tools Based On User Preferences. Anna ZaretskayaplanetalinguaPas encore d'évaluation
- GT I9100g Service SchematicsDocument8 pagesGT I9100g Service SchematicsMassolo RoyPas encore d'évaluation
- DISTRICT CENSUS HANDBOOK North GoaDocument190 pagesDISTRICT CENSUS HANDBOOK North Goants1020Pas encore d'évaluation
- Prediction of Mechanical Properties of Steel Using Artificial Neural NetworkDocument7 pagesPrediction of Mechanical Properties of Steel Using Artificial Neural NetworkInternational Association of Scientific Innovations and Research (IASIR)Pas encore d'évaluation
- Malampaya Case StudyDocument15 pagesMalampaya Case StudyMark Kenneth ValerioPas encore d'évaluation
- Financial Statement AnalysisDocument18 pagesFinancial Statement AnalysisAbdul MajeedPas encore d'évaluation
- Bai Tap Av 12 Thi Diem Unit TwoDocument7 pagesBai Tap Av 12 Thi Diem Unit TwonguyenngocquynhchiPas encore d'évaluation
- POLYTHEOREMSDocument32 pagesPOLYTHEOREMSYen LeePas encore d'évaluation
- Old Highland Park Baptist Church E01Document74 pagesOld Highland Park Baptist Church E01Lawrence Garner100% (2)
- PC's & Laptop Accessories PDFDocument4 pagesPC's & Laptop Accessories PDFsundar chapagainPas encore d'évaluation
- Teacher'S Individual Plan For Professional Development SCHOOL YEAR 2020-2021Document2 pagesTeacher'S Individual Plan For Professional Development SCHOOL YEAR 2020-2021Diether Mercado Padua100% (8)
- Plant Vs Filter by Diana WalstadDocument6 pagesPlant Vs Filter by Diana WalstadaachuPas encore d'évaluation
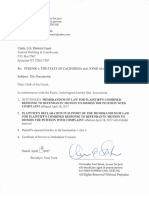
- STRUNK V THE STATE OF CALIFORNIA Etal. NYND 16-cv-1496 (BKS / DJS) OSC WITH TRO Filed 12-15-2016 For 3 Judge Court Electoral College ChallengeDocument1 683 pagesSTRUNK V THE STATE OF CALIFORNIA Etal. NYND 16-cv-1496 (BKS / DJS) OSC WITH TRO Filed 12-15-2016 For 3 Judge Court Electoral College ChallengeChristopher Earl Strunk100% (1)
- Abacus 1 PDFDocument13 pagesAbacus 1 PDFAli ChababPas encore d'évaluation
- Alem Ketema Proposal NewDocument25 pagesAlem Ketema Proposal NewLeulPas encore d'évaluation
- Accounting System (Compatibility Mode) PDFDocument10 pagesAccounting System (Compatibility Mode) PDFAftab AlamPas encore d'évaluation
- NSTP SlabDocument2 pagesNSTP SlabCherine Fates MangulabnanPas encore d'évaluation