Académique Documents
Professionnel Documents
Culture Documents
Surgical Management of Vascular Lesion in H&N
Transféré par
Dipti Patil0 évaluation0% ont trouvé ce document utile (0 vote)
109 vues7 pagesVascular anomalies are amongst the most common congenital abnormalities observed in infants and children. Their occurrence in the head and neck region is a source of functional and aesthetic compromise. A new classification based on the anatomical location and depth of the lesion has been proposed.
Description originale:
Titre original
Surgical Management of Vascular Lesion in h&n
Copyright
© Attribution Non-Commercial (BY-NC)
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentVascular anomalies are amongst the most common congenital abnormalities observed in infants and children. Their occurrence in the head and neck region is a source of functional and aesthetic compromise. A new classification based on the anatomical location and depth of the lesion has been proposed.
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
109 vues7 pagesSurgical Management of Vascular Lesion in H&N
Transféré par
Dipti PatilVascular anomalies are amongst the most common congenital abnormalities observed in infants and children. Their occurrence in the head and neck region is a source of functional and aesthetic compromise. A new classification based on the anatomical location and depth of the lesion has been proposed.
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 7
Clinical Paper
Congenital Craniofacial Anomalies
Surgical management of
vascular lesions of the head and
neck: a review of 115 cases
S. C. Nair, N. J. Spencer, K. P. Nayak, K. Balasubramaniam: Surgical management
of vascular lesions of the head and neck: a review of 115 cases. Int. J. Oral
Maxillofac. Surg. 2011; 40: 577583. #2011 International Association of Oral and
Maxillofacial Surgeons. Published by Elsevier Ltd. All rights reserved.
S. C. Nair
1
, N. J. Spencer
2
,
K. P. Nayak
3
, K. Balasubramaniam
3
1
Maxillofacial Surgery Department,
Bangalore Institute of Dental Sciences,
Bangalore, India;
2
University of Cincinnatti,
USA;
3
B.M. Jain Hospital, India
Abstract. Vascular anomalies are amongst the most common congenital
abnormalities observed in infants and children. Their occurrence in the head and
neck region is a source of functional and aesthetic compromise. This article reviews
the surgical management of 115 cases of vascular anomalies involving the head and
neck area treated by the authors between 1998 and 2009. It discusses the diagnostic
aids, treatment protocol and the results obtained. A new classication based on the
anatomical location and depth of the lesion has been proposed. This allows
guidelines for surgical ablation of the vascular lesions. The complications
encountered are discussed. The use of external carotid artery control as opposed to
pre-surgical embolization has proved effective and the technique is described. The
location and extent of a vascular malformation should dictate the preoperative
investigations, surgical procedure and subsequent outcome.
Keywords: surgery; head; neck; lesions.
Accepted for publication 3 February 2011
Available online 22 March 2011
Vascular anomalies are a group of lesions
derived fromblood vessels and lymphatics
with widely varying histology and clinical
behaviour. They constitute the most com-
mon congenital abnormalities in infants
and children. James Wardrop, a London
surgeon, rst recognized the differences
between true hemangiomas and the less
common vascular malformations in
1818
14
. Despite Dr. Wardrops work,
descriptive identiers such as Strawberry
hemangioma and salmon patch continued
to be used until the 1980s. This terminol-
ogy did not correlate with the biological
behaviour or histology of these lesions. In
1982, Mulliken and Glowacki greatly
advanced the eld by introducing a
biological classication which differen-
tiated vascular lesions into two distinct
entities: hemangiomas and vascular mal-
formations
13,14
. The term hemangioma
now describes a lesion that is neoplastic,
demonstrating endothelial hyperplasia.
Vascular malformations, conversely, do
not demonstrate cellular hyperplasia but
display progressive ectasia of abnormal
vessels lined by at endothelial on a thin
basal lamina. A more practical classica-
tion integrating their biological behaviour
with dynamics of ow was later advanced
(Table 1)
7
.
The diagnosis of this group of lesions
primarily depends on the history of the
lesion and the clinical presentation. Radio-
graphic evaluation may be helpful in
determining the exact extent, location
and ow dynamics of some lesions.
Patients and methods
One hundred and fteen patients treated
by the authors between 1999 and 2009
were reviewed retrospectively. Relevant
data including gender, age, age at presen-
tation of symptoms, anatomical site of
lesion, relevant radiographic investiga-
tions and period of follow up were tabu-
lated. Exclusion criteria included
segmental lesions and those associated
with syndromes such as Sturge-Weber.
Int. J. Oral Maxillofac. Surg. 2011; 40: 577583
doi:10.1016/j.ijom.2011.02.005, available online at http://www.sciencedirect.com
0901-5027/060577 +07 $36.00/0 # 2011 International Association of Oral and Maxillofacial Surgeons. Published by Elsevier Ltd. All rights reserved.
All patients underwent surgery as the
principal modality of treatment. Com-
puted tomography (CT) with contrast,
magnetic resonance imaging (MRI) and
angiography were used based on the ana-
tomical location and ow dynamics of the
lesion. Selective control of the external
carotid artery to reduce blood ow into the
lesion was used effectively by the author
in lieu of routine preoperative emboliza-
tion.
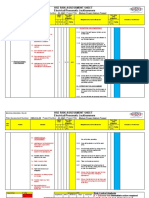
Technique for external carotid control
The external carotid artery (ECA) of the
involved side is exposed through a cervi-
cal incision, which often forms part of the
access for removal of the malformation
(Fig. 1). The sternocleidomastoid muscle
is retracted posteriorly at the level of the
greater cornu of the hyoid bone, exposing
the carotid sheath. The external carotid
distal to the carotid bifurcation is identi-
ed. The vessel is snared with a vascular
sling passed through a red rubber catheter.
Gentle strangulation of the vessel can be
accomplished by advancing the catheter.
This additional compression of the vessel
serves to reduce blood ow to the lesion.
The lesion is exposed with great care taken
not to disturb the vascular network. Feed-
ing arteries and draining vessels are iden-
tied and ligated, permitting total excision
of the lesion. The wound is closed primar-
ily with vacuum drains in situ. The mal-
formations were categorized into ve
types depending on their anatomy and
depth of location in the head and neck
region (Table 2). In type I supercial
lesions requiring excision of skin or
mucosa, local or regional aps have been
used in defect reconstruction (Fig. 2).
Type II submucosal lesions require com-
plete excision after elevation of skin aps
(Fig. 3). Type III lymphovenous malfor-
mations or venous malformations invol-
ving salivary glands are excised along
with the affected gland (Fig. 4). Type
IV intraosseous lesions require excision
with involved bone and reconstruction
when required (Fig. 5). Type V lesions
involving deep visceral spaces, such as the
parapharyngeal or infra-temporal fossa,
require mandibular access osteotomy for
complete exposure and total excision
(Fig. 6). The above classication helped
in determining the surgical approach and
reconstruction necessary for the type of
vascular lesion.
Results
Of the 115 patients evaluated, 63 were
male and 52 female. The youngest patient
was a 2-year-old girl with a lymphatic
malformation in the parotid region (type
III) and the oldest was a 58-year-old male
with a venous malformation involving the
entire tongue and submandibular region
(type II). Table 3 shows the patients cate-
gorized into types with gender distribu-
tion. 38 patients with type I, 44 patients
with type II, 12 patients with type III, 11
patients with type IV and 10 patients with
type V anomalies were treated success-
fully by surgical ablation of their vascular
lesions. Four patients with type I lesions
required reconstruction with local or
regional aps and 2 patients with type
IV lesions required reconstruction of
resected mandible. Only 88 patients could
provide an approximate time of appear-
ance of the lesion. In 27 patients the lesion
had been noticed at birth or soon after. The
remaining 61 patients were clinically
aware of it shortly before their rst surgi-
cal visit. Table 4 highlights the different
imaging techniques used according to the
578 Nair et al.
Table 1. Existing classication of hemangiomas and vascular malformations.
A. Hemangiomas
Supercial (capillary hemangioma)
Deep (cavernous hemangioma)
Compound (capillary cavernous hemangioma)
B. Vascular malformations
Simple lesions
Low-ow lesions
Capillary malformations (capillary hemangioma, port-wine stain)
Venous malformation (cavernous hemangioma)
Lymphatic malformation (lymphangioma, cystic hygroma)
High-ow lesions
Arterial malformation
Combined lesions
Arteriovenous malformations
Lymphovenous malformations
Other combinations
Fig. 1. ECA snared with vascular sling.
Table 2. Categorization of vascular malfor-
mation based on anatomical presentation.
Type I Mucosal/cutaneous (Fig. 2)
Type II Submucosal/subcutaneous (Fig. 3)
Type III Glandular (Fig. 4)
Type IV Intraosseous (Fig. 5)
Type V Deep visceral (Fig. 6)
Table 3. Patients and age according to the
types of the various vascular lesions.
Type Age (years) Female Male
I 744 (24.705)
a
15 23
II 352 (23.27)
a
25 19
III 243 (26.2)
a
7 5
IV 849 (22.8)
a
3 8
V 1856 (32.8)
a
4 6
a
Average age.
type of malformation. At the authors
centre CT scanning with contrast is the
most frequently used imaging modality.
Table 5 demonstrates the method of hae-
morrhage control used for the malforma-
tion. Pre-surgical embolization was
restricted to two patients and external
carotid artery control was required in 52
patients. Complications encountered are
listed in Table 6. One hundred and eleven
patients gained an acceptable aesthetic
outcome with a single procedure. Table
7 summarizes the surgical plan employed
for each type of lesion and the reconstruc-
tion used when required.
Discussion
The rst public demonstration of ether
anaesthesia by William Green Morton in
1846 was for surgical removal of a venous
vascular malformation
14
. Numerous
attempts to understand, classify and treat
these lesions have met with unpredictable
outcomes. The classication proposed by
Mulliken and Glowacki differentiated this
group of lesions into the biologically active
hemangiomas and inactive vascular mal-
formations. Classication led to improved
understanding of the behaviour of these
lesions. Timing of treatment could be based
on a scientic understanding of the lesions
biological behaviour rather than clinical
appearance or the surgeons sense of
gestalt
14
. Subsequently, Mulliken and
Kaban introduced the ow dynamics of
vascular lesions, describing hi-ow and
low-ow vascular malformations
10
. More
recently, a practical classication (Table 1)
has helped to consolidate all previous clas-
sication
7
. The authors have categorized
vascular lesions requiring surgery into ve
types. This simplied categorization pro-
vides input into the investigation and effec-
tive surgical management of various
lesions based on anatomical presentation.
Diagnosis of vascular malformations
depends on precise identication, accurate
history, physical examination and the
proper use of imaging. Advances in ima-
ging have led to the unnecessary exposure
of many lesions. Grey scale ultrasound
and Doppler analysis are useful in dening
whether the lesion is solid or cystic and in
establishing the ow dynamics of a
lesion
17
. In evaluating vascular malforma-
tions, MRI has a major advantage over CT
or angiography in differentiating heman-
giomas from the surrounding structures,
but its cost and limited availability can be
prohibitive to its use. In the authors
experience, imaging is restricted to CT
with contrast for most lesions for cost
reasons. MRI is restricted to 2 patients
Surgery for vascular head and neck lesions 579
Fig. 2. Type I low ow cutaneous venous malformation.
Fig. 3. Type II low ow vascular malformation in the buccal region.
Table 4. Imaging techniques used in the different types of vascular lesion.
Type I
n = 38
Type II
n = 44
Type III
n = 12
Type IV
n = 11
Type V
n = 10
CTC 32 34 7 2 6
MRI 0 1 1 0 0
Angiogram 0 5 4 8 4
No investigation 6 4 0 1 0
and angiography to 18 patients (Table 4).
Angiography, particularly digital subtrac-
tion angiography (Fig. 7), has a specic but
limited role in the diagnosis of vascular
lesions. It is restricted to lesions requiring
therapeutic endovascular intervention
7
.
Selective embolization as a single treat-
ment modality is rarely successful with
high owanomalies because of rapid estab-
lishment of newpathways of ow. Ligation
of main feeder vessels is also forbidden due
to low success rates and its elimination of
access for future embolization
3,5,12,16
.
The use of temporary control (ligation)
of the ECA instead of presurgical embo-
lization has proven effective in reduction
of blood ow to the lesion, allowing effec-
tive excision with minimal blood loss.
Where blood replacement is required,
autologous transfusion is preferred. When
embolization is chosen subsequent to digi-
tal subtraction angiograph (DSA) it should
proceed from distal to proximal thus ablat-
ing both the nidus and its source
18
. Choice
of embolic agents is purely the clinicians
preference. Gelfoam, polyvinyl alcohol,
silicone uid and isobutyl-2 cyanoacrylate
are commonly used agents
7
. When embo-
lization is used, surgery is carried out
within 2448 h to prevent the develop-
ment of collateral blood supply
1,4,6,9,11
.
The use of presurgical embolization was
restricted to two patients with type V
(deep visceral) lesions, both of which
required ECA control intraoperatively
despite embolization. One of these
patients presented for surgical manage-
ment after undergoing an emergent embo-
lization. The second presented with both
ECAs feeding into the lesion; one was
embolized and the other controlled with
temporary intraoperative ligation.
Sclerotherapy has a promising but lim-
ited role in the management of vascular
lesions. Success has been realized in the
treatment of macrocystic lesions. The ther-
apy has been less effective in treating
microcystic vascular malformations
2,8,15
.
The different agents used include sodium
tetradecyl sulphate (3%), sodiumtetradecyl
acetate and more recently OK 432 (lyophi-
lized Streptococcus pyogenes treated with
benzyl penicillin)
7
.
Surgery has been used effectively to
eradicate or minimize the lesion in this
review of 115 cases. Surgery must be
aimed at removal of the entire nidus along
with any structure associated with the
lesion because any remaining vasculature
will probably lead to recurrence. The pro-
posed classication (Table 2) was used to
help plan the approach and extent of
resection. Supercial lesions required
excision of skin or mucosa with recon-
580 Nair et al.
Fig. 4. (a) Type III lymphovenous malformation in left parotid gland. (b) Exposure of lesion
through preauricular incision with cervical extension. (c) Excised specimen showing cystic
spaces. (d) 2-Month postoperative appearance after total excision of lesion with gland.
Fig. 5. Type IV intra bony hi-ow arterial malformation in maxilla.
struction using local or regional aps.
Lesions involving the parotid or subman-
dibular gland require excision of the gland
with preservation of nerves. Deeper
lesions necessitate access osteotomies
for excision. Lesions within bone, under-
went bone resection followed with recon-
struction using autologous grafts. In one
patient with arteriovenous malformation
(AVM) in the mandible, successful repla-
cement of the resected mandible after
enucleation of the pathology was per-
formed. Skeletal deformities secondary
to lymphangiomas were common and
required secondary correction of the ske-
letal deformity. Table 7 demonstrates the
authors surgical approach to vascular
malformations based on anatomical pre-
sentation. The complications were
restricted to morbidity with no mortality.
The most common problem encountered
was incomplete excision requiring another
operation at a later date. Temporary par-
esis of branches of facial nerve and exces-
sive intraoperative haemorrhage were also
seen. Excessive haemorrhage was dened
as blood loss requiring more than auto-
logous transfusion. The overall satisfac-
tion quotient was high.
In conclusion, the use of intraoperative
control of branches of the external carotid
artery has proved a successful, safe and
effective method of intraoperative hae-
morrhage control when removing these
potentially bloody lesions. The approach
is easy to incorporate into the access
necessary to remove the lesion. An
increase in morbidity by this approach
was not seen compared with lesions trea-
ted with preoperative embolization. The
present accepted classication (Table 1)
attempts to correlate the biological classi-
cation by Mulliken and Glowacki with
the ow dynamics of the lesion. Whilst
Surgery for vascular head and neck lesions 581
Fig. 6. Type V MRI showing venous malformation in lateral and post-pharyngeal space.
Table 5. Number of patients who had ECA control as against pre-surgical embolization.
Type I
n = 38
Type II
n = 44
Type III
n = 12
Type IV
n = 11
Type V
n = 10
ECA control 1 32 11 11 10
Non-ECA control 37 12 1 Nil Nil
Embolization Nil Nil Nil 1
a
1
a
a
Had ECA control along with presurgical embolization.
Table 6. Complications encountered in the different types of vascular anomalies with the site and prescribed imaging modality.
SL Classication Age Sex Site Investigation Complication
1 Type IV 8 M Lt maxilla Angio Excessive intraoperative haemorrhage
2 Type II 23 F Rt cheek Angio Incomplete excision
3 Type IV 8 M Lt maxilla Angio with presurgical
embolization
Recurrence in mandible
4 Type I 19 F Lt upper lip CTC Overexcision with hypoplastic apearance
5 Type II 31 F Rt cheek CTC Temporary neuroparesis VII nerve
6 Type I 25 F Tongue CTC Residual lesion cheek
7 Type I 22 F Lower lip CTC Incomplete excision and scarring
8 Type II 21 F Lt lower eyelid CTC Temporary ectropion
9 Type V 18 F Lt infra temporal fossa Angio with presurgical
embolization
VII nerve weakness
10 Type V 23 M Lt temporal fossa CTC Intraoperative haemorrhage from cavernous sinus
Table 7. Surgical treatment advocated for the types of vascular anomalies.
Classication Male Female Treatment
Type I Mucosal/cutaneous lesion arising from
papillary dermis involving skin or mucosa (n = 38)
23 15 Excision with overlying skin or mucosa
Primary closure or regional ap
Type II Submucosal or subcutaneous with no discoloration
of overlying skin (n = 44)
19 25 Surgical access to lesion with total excision and primary
closure
Type III Lesions involving glands ex-parotid/
submandibular (n = 12)
5 7 Surgical access to glandular lesions with excision along
with the involved gland and primary closure (Fig. 4AD)
Type IV Skeletal involving the facial skeleton
ex-maxilla/mandible/zygoma (n = 11)
8 3 Excision of involved skeletal structure with reconstruction
Type V Deep visceral ex-parapharyngeal/
infratemporal (n = 10)
6 4 Mandibulotomy to access the lesion followed by total excision
this is helpful in understanding the lesions
behaviour, a further categorization of
lesions that require operative intervention
based on the technique needed for surgical
treatment would be helpful to the managing
surgeon. The authors describe a simplied
algorithmfor effective management of vas-
cular lesions requiring surgery (Table 7).
For example, hemangiomas are treated
with a wait and watch policy since they
frequently undergo resolution, but vascular
malformations causing functional or aes-
thetic deformity are dealt with at the earliest
opportunity. Proper management depends
not only on the biological behaviour, but
also on site of anatomical presentation.
Presentation of a lesion not only as a venous
malformation, but as a type V venous mal-
formation gives the surgeon the additional
information needed to plan treatment prop-
erly. Adequate imaging techniques are the
key to the successful diagnosis and effec-
tive treatment of all vascular anomalies.
Angiography should be restricted to
anomalies requiringendovascular interven-
tion and lesions that may have feeders from
the internal carotid artery. MRI with fat
suppressed images is most effective. The
use of alternative therapy, such as emboli-
zation and sclerotherapy, has an effective
but limited role in treating vascular lesions.
The use of clinical data with non-invasive
imaging techniques, followed by precise
surgery has been successful in providing
satisfactory treatment in the majority of
patients. Segmental and large composite
lesions require multiple therapies. Eradica-
tion is unlikely with either surgery alone or
combination therapies.
Funding
None.
Competing interests
None declared.
Ethical approval
Retrospective case review ethical clear-
ance not required.
Acknowledgements. Prof. Paul Stoelinga,
Nijmegen, Netherlands and Dr. Deepak
Gopalakrishnan, University of Cincin-
natti, USA are acknowledged for their
support in preparing this manuscript.
References
1. Azzzolini A, Bertani A, Riberti C.
Superselective embolization and immedi-
ate surgical treatment; our present
approach to treatment of vascular heman-
giomas of the face. Ann Plast Surg 1982:
9: 4260.
2. Baneieghlal B, Davis MR. Guidelines
for the successful treatment of lymphna-
gioma with OK-432. Eur J Pediatr Surg
2003: 13: 103107.
3. Biller HF, Krespi YP, Som PM. Com-
bined therapy for vascular lesions of the
head and neck with intra-arterial emboli-
zation and surgical excision. Otolaryngol
Head Neck Surg 1982: 90: 37.
4. Burrows PE, Lasjaunias PL, Ter
Brugge KG, Flodmark O. Urgent and
emergent embolisation of lesions of head
and neck in children: indications and
results. Pediatrics 1987: 80: 386394.
5. Demuth RJ, Milller SH, Kellar F.
Complications of embolization treatment
for problem cavernous hemangiomas.
Ann Plast Surg 1984: 13: 135144 6.
6. Emjolras O, Logeart I, Gelbert F,
Lemarchand-Venencie F, Reizihne
D, Guichard JP, Merland JJ. Arterio
venous malfomations: a study of 200
cases. Ann Dermatol Venerol 2000:
127: 1722.
7. Ethunandan M, Mellor TK. Heman-
giomas and vascular malformations of the
maxillofacial region review. Br J Max-
illofac Surg 2006: 44: 263272.
8. Giguere CM, Bauman NM, Sata Y,
Burke DK, Grienwald JH, Pransky
S, Kelley P, Georgeson K, Smith
RJ. Treatment of lymphangiomas with
OK-432(Picibani) sclerotherapy: a pro-
spective multiinstitutional trial. Arch
Otolaryngol Head Neck Surg 2002:
128: 11371144.
9. Jackson IT, Carreno R, Potparic Z,
Hussain K. Hemangiomas, vascular mal-
formation, and lymphovenous malforma-
tions: classication and methods of
treatment. Plast Recontr Surg 1993: 91:
12161230.
10. Kaban LB, Mulliken JB. Vascular
anomalies of maxillofacial region. J Oral
Maxillofac Surg 1986: 44: 203213.
11. Kahout MP, Hansen M, Pribaz JJ,
Mulliken JB. Arterio venous malforma-
tions of the head and neck: natural history
582 Nair et al.
Fig. 7. Digital subtraction angiography of submandibular hi-ow AVM.
and management. Plast Reconstr Surg
1998: 102: 643654.
12. Merland JJ, Riche MC, Hadjean E.
The use of superselective arteriography,
embolization and surgery in the current
management of cervicocephalic vascular
malformations (350 cases). In: Williams
HB, ed: Symposium on Vascular Malfor-
mation and Melanotic LesionsSt Louis,
Mosby, 1983.
13. Mulliken JB, Glowacki J. Hemangio-
mas and vascular malformations in
infants and children: a classication
based on endothelial characteristrics.
Plast Reconstr Surg 1982: 69: 412422.
14. Mulliken JB, Young AE. Vascular
birthmarks. Hemangiomas and Malfor-
mations. Philadelphia: Saunders 1988.
15. Ogita S, Tsuto T, Nakamura K, Degu-
chi E, Iwai N. OK-432 therapy in 64
patients with lymhangioma. J Pediatr
Surg 1994: 29: 784785.
16. Persky MS. Congenital vascular lesions
of the head and neck. Laryngoscope
1986: 96: 1002.
17. Platiel HJ, Burrows PE, Kozakewich
HPW, Zurakowski D, Mulliken JB.
Soft tissue vascular anomalies: utility of
US for diagnosis. Radiology 2002: 214:
747754.
18. Waner M, Suen JY. Hemangiomas and
Vascular Malformations of the Head and
Neck. New York: Wiley-Liss 1999:.
Address:
Sanjiv C. Nair
Maxillofacial Surgery
Bangalore Institute of Dental Sciences
Wilson Garden
Bangalore 560 029
India
Tel.: +91 98454 33106
E-mail: snmaxfax@gmail.com
Surgery for vascular head and neck lesions 583
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- SHCO Second Edition - NEDocument65 pagesSHCO Second Edition - NESwati Bajpai100% (2)
- Milton Terry Biblical HermeneuticsDocument787 pagesMilton Terry Biblical HermeneuticsFlorian100% (3)
- Business Research Chapter 1Document27 pagesBusiness Research Chapter 1Toto H. Ali100% (2)
- Factoring Problems-SolutionsDocument11 pagesFactoring Problems-SolutionsChinmayee ChoudhuryPas encore d'évaluation
- Brochure of El Cimarron by HenzeDocument2 pagesBrochure of El Cimarron by HenzeLuigi AttademoPas encore d'évaluation
- LEGO Group A Strategic and Valuation AnalysisDocument85 pagesLEGO Group A Strategic and Valuation AnalysisRudmila Ahmed50% (2)
- Small Healthcare Organization: National Accreditation Board For Hospitals & Healthcare Providers (Nabh)Document20 pagesSmall Healthcare Organization: National Accreditation Board For Hospitals & Healthcare Providers (Nabh)Dipti PatilPas encore d'évaluation
- Enhanced Recovery After Surgery (ERAS)Document11 pagesEnhanced Recovery After Surgery (ERAS)Dipti PatilPas encore d'évaluation
- 5th Edition Hospital STD April 2020 PDFDocument148 pages5th Edition Hospital STD April 2020 PDFFeroz Ikbal100% (1)
- Aneurysmal Bone CystDocument5 pagesAneurysmal Bone CystDipti PatilPas encore d'évaluation
- 0PIOIDDocument77 pages0PIOIDDipti PatilPas encore d'évaluation
- ChandraDocument17 pagesChandraDipti PatilPas encore d'évaluation
- Adverse Effect of Chemotherapy.Document3 pagesAdverse Effect of Chemotherapy.Dipti PatilPas encore d'évaluation
- Cerebral Shunts: DR Dipti Patil (1 MDS) Dept of Oral Maxillofacial Surgery KCDS, BangloreDocument25 pagesCerebral Shunts: DR Dipti Patil (1 MDS) Dept of Oral Maxillofacial Surgery KCDS, BangloreDipti PatilPas encore d'évaluation
- Harish: Odontogenic Kerato CystDocument4 pagesHarish: Odontogenic Kerato CystDipti PatilPas encore d'évaluation
- New Findings and Controversies in Odontogenic TumorsDocument4 pagesNew Findings and Controversies in Odontogenic TumorsDipti PatilPas encore d'évaluation
- 1 Additives To Local Anesthetics For PeripheralDocument1 page1 Additives To Local Anesthetics For PeripheralDipti PatilPas encore d'évaluation
- Intravenous Lipid Emulsion As Antidote For Local ADocument1 pageIntravenous Lipid Emulsion As Antidote For Local ADipti PatilPas encore d'évaluation
- Clotting FactorDocument2 pagesClotting FactorDipti Patil100% (1)
- Forehead Flap: DR Dipti Patil (1 MDS) Dept of Oral Maxillofacial Surgery KCDS, BangloreDocument42 pagesForehead Flap: DR Dipti Patil (1 MDS) Dept of Oral Maxillofacial Surgery KCDS, BangloreDipti PatilPas encore d'évaluation
- Medical Secretary: A. Duties and TasksDocument3 pagesMedical Secretary: A. Duties and TasksNoona PlaysPas encore d'évaluation
- Houses WorksheetDocument3 pagesHouses WorksheetYeferzon Clavijo GilPas encore d'évaluation
- Reading 7.1, "Measuring and Managing For Team Performance: Emerging Principles From Complex Environments"Document2 pagesReading 7.1, "Measuring and Managing For Team Performance: Emerging Principles From Complex Environments"Sunny AroraPas encore d'évaluation
- 4TES-9Y 20KW With InverterDocument4 pages4TES-9Y 20KW With InverterPreeti gulatiPas encore d'évaluation
- Omnibus Motion (Motion To Re-Open, Admit Answer and Delist: Republic of The PhilippinesDocument6 pagesOmnibus Motion (Motion To Re-Open, Admit Answer and Delist: Republic of The PhilippinesHIBA INTL. INC.Pas encore d'évaluation
- W1 MusicDocument5 pagesW1 MusicHERSHEY SAMSONPas encore d'évaluation
- Poetry Analysis The HighwaymanDocument7 pagesPoetry Analysis The Highwaymanapi-257262131Pas encore d'évaluation
- Body ImageDocument7 pagesBody ImageCristie MtzPas encore d'évaluation
- Your Song.Document10 pagesYour Song.Nelson MataPas encore d'évaluation
- Four Year Plan DzenitaDocument4 pagesFour Year Plan Dzenitaapi-299201014Pas encore d'évaluation
- Bruce and The Spider: Grade 5 Reading Comprehension WorksheetDocument4 pagesBruce and The Spider: Grade 5 Reading Comprehension WorksheetLenly TasicoPas encore d'évaluation
- SwimmingDocument19 pagesSwimmingCheaPas encore d'évaluation
- 9 Electrical Jack HammerDocument3 pages9 Electrical Jack HammersizwePas encore d'évaluation
- HDFCDocument60 pagesHDFCPukhraj GehlotPas encore d'évaluation
- Electronic Form Only: Part 1. Information About YouDocument7 pagesElectronic Form Only: Part 1. Information About YourileyPas encore d'évaluation
- Gmail - Payment Received From Cnautotool - Com (Order No - Cnautot2020062813795)Document2 pagesGmail - Payment Received From Cnautotool - Com (Order No - Cnautot2020062813795)Luis Gustavo Escobar MachadoPas encore d'évaluation
- Abb PB - Power-En - e PDFDocument16 pagesAbb PB - Power-En - e PDFsontungPas encore d'évaluation
- Connecting Microsoft Teams Direct Routing Using AudioCodes Mediant Virtual Edition (VE) and Avaya Aura v8.0Document173 pagesConnecting Microsoft Teams Direct Routing Using AudioCodes Mediant Virtual Edition (VE) and Avaya Aura v8.0erikaPas encore d'évaluation
- AllisonDocument3 pagesAllisonKenneth RojoPas encore d'évaluation
- 2 - (Accounting For Foreign Currency Transaction)Document25 pages2 - (Accounting For Foreign Currency Transaction)Stephiel SumpPas encore d'évaluation
- COPARDocument21 pagesCOPARLloyd Rafael EstabilloPas encore d'évaluation
- Clasificacion SpicerDocument2 pagesClasificacion SpicerJoseCorreaPas encore d'évaluation
- Meter BaseDocument6 pagesMeter BaseCastor JavierPas encore d'évaluation
- Republic of The Philippines Legal Education BoardDocument25 pagesRepublic of The Philippines Legal Education BoardPam NolascoPas encore d'évaluation
- Coffee in 2018 The New Era of Coffee EverywhereDocument55 pagesCoffee in 2018 The New Era of Coffee Everywherec3memoPas encore d'évaluation