Académique Documents
Professionnel Documents
Culture Documents
Ectopic New1
Transféré par
Vincent TuazonDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Ectopic New1
Transféré par
Vincent TuazonDroits d'auteur :
Formats disponibles
Ectopic Pregnancy (EP)cavity.
When an implantation occurs outside the uterine
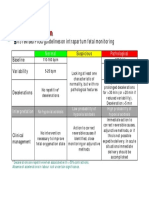
-Implantation may occur in the ovary, fallopian tube, or cervix. 95% are in the fallopian tubes, most of them in the ampullar portion(distal third), but can also occur in the isthmus or fimbrial portions of the fallopian tubes. Causes: An obstruction is present like an adhesion in the fallopian tube from a previous infection ( chronic salpingitis or pelvic inflammatory disease), congenital malformations, scars from tubal surgery, or uterine tumor pressing on the proximal end of the tube. Passage is blocked, thus the zygote cant travel, so it implants in a strictured site along the tube and continues to grow. -2% of pregnancies are ectopic -2nd most frequent cause for early bleeding in pregnancy -EP increases with use of intrauterine devices (slows transport) -Increases following in vitro -Increases 10%-20% if they had a previous EP -Oral contraceptives can reduce EP Assessment: -Vomiting and nausea -+ hCG test -Can be detected early with ultrasound -6-12 weeks of gestation, zygote is large enough to rupture fallopian tube -Rupture causes bleeding especially when near the interstitial portion* -Sharp stabbing pains at lower abdomen quadrants -Products of conception may expel into pelvic cavity -Placenta is dislodged and causes additional bleeding -If internal bleeding progresses to acute hemorrhage, may lead to shock -Transvaginal ultrasound detects the rupture -Falling hCG or serum progesterone level suggests end of pregnancy -Laparoscopy or ultrasonography to visualize fallopian tube. Therapeutic Management: -Some EPs spontaneously end before rupture and no treatment is needed -When early EP is revealed, unruptured EP can be treated medically with oral administration -Methotrexate- a folic acid antigonist chemotherapeutic agent that attacks fast growing cells -Mifepristone- causes sloughing of the tubal implantation site (Tube is left intact) -If there is a rupture, laparoscopy is done to ligate bleeding vessels and repair the damaged fallopian tubes. The tube is either removed or a microsurgical technique is done to suture the tube. Placenta Previa - A condition of pregnancy in which the placenta is implanted
abnormally in the uterus. - the most common cause of painless bleeding in the third trimester. There are four degrees. 1) low-lying placenta 2) Marginal implantation 3) partial placenta previa 4) total placenta previa - coverage of cervix opening is done in percentages 100%, 75%, 30 % etc. - Placenta previa is increase with advanced maternal age, past CS, past D&C, and multiple gestation. Incidence is 5 per 1000 pregnancies and happens when the placenta is forced to spread and find adequate exchange surface. Assessment: -Most placenta previa is diagnosed early -Women are told to avoid coitus and get adequate rest -Bleeding begins when the lower uterine segment starts to differentiate from the upper segment at around 30 weeks into gestation and the cervix begins to dilate -Bleeding is caused by placentas inability to stretch to accommodate the lower uterine segment. Bleeding is usually abrupt, painless and bright red. -Therapeutic Managemnt: -The site of bleeding, open vessels of the uterine decidua (maternal blood) places the mother at risk for hemorrhage. -Fetal oxygen supply is compromised when placenta is loosened and there is a threat for preterm birth. -Place woman in a side-lying position to ensure adequate blood supply to fetus. Assess: Duration of pregnancy, time of bleeding, amount of blood, pain, color of blood, prior bleeding, prior cervical surgery -Weigh perinea pads to determine blood loss -Kleihauer- Betke test to determine if blood is fetal or maternal -NEVER attempt pelvic or rectal examination, may initiate massive hemorrhage. -Obtain VS every 5-15 mins -If previa is under 30%, fetus may be born -If over 30%, then cesarean
Abruptio Placentae: - Premature separation of the placenta, results in bleeding. - Premature separation of the placenta occurs in 10% of pregnancies, and is the most frequent cause of perinatal death. Separation usually occurs late in pregnancy but can occur in the first or second stage of labor. The primary cause
is unknown but some predisposing factors may be advanced maternal age, short umbilical cord, chronic hypertensive disease, PIH, direct trauma, vasoconstrictions, or chrioamnionitis. Following a premature placenta separation is a rapid decrease in uterine volume and sudden release of amniotic fluid. - Partial separation (concealed hemorrhage) - Partial separation ( apparent hemorrhage) - Complete separation ( concealed hemorrhage) Assessment: - Woman experiences sharp stabbing pain high in the uterine fundus as separation occurs - during labor each contraction will be accompanied with so much more pain over the contractions itself. - Heavy bleeding after separation * - whether blood is evident or not, signs of shock will follow due to blood loss. - Uterus becomes tense and rigid to touch - Couvelaire uterus ( hard boardlike uterus) - Blood fibrinogen may be used up and disseminated intravascular coagulation can occur (DIC) - Blood work should be done - test for DIC , draw 5 ml of blood, into dry test tube, let stand for 5 minutes, and a clot should form. No clot indicates abnormality Therapeutic Management: - woman needs large- gauge catheter to replace fluids - monitor fetal heart sounds - record VS every 5- 15 mins - keep woman in lateral position to prevent pressure to vena cava - do not perform vaginal, abdominal, pelvic examinations - Placental separation grade* 0,1,2,3 - if higher than 1, pregnancy must be terminated = CS - If DIC has developed, CS may pose a risk for hemorrhage. - Worst case, a hysterectomy to prevent exsanguination - A woman who has had bleeding before birth is more prone to infection after birth than the average woman. Needs close attention in postpartum period.
Vous aimerez peut-être aussi
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Computational BioengineeringDocument480 pagesComputational Bioengineeringscribd990Pas encore d'évaluation
- Endocrine 50 Questions & AnswersDocument28 pagesEndocrine 50 Questions & AnswersBrooke Susac100% (1)
- Medical Management of in Children: A Delphi Consensus: BlepharokeratoconjunctivitisDocument8 pagesMedical Management of in Children: A Delphi Consensus: Blepharokeratoconjunctivitisriskab123Pas encore d'évaluation
- CTG Classification PDFDocument1 pageCTG Classification PDFganotPas encore d'évaluation
- Dorn Method Certification CourseDocument10 pagesDorn Method Certification Coursejpepe100% (1)
- Adv For CounselorDocument2 pagesAdv For CounselorRashmi RanjanPas encore d'évaluation
- Para Instwise Adm Af Reporting Cancel r1Document639 pagesPara Instwise Adm Af Reporting Cancel r1Rutvik DhoriyaPas encore d'évaluation
- Portfolio ResumeDocument2 pagesPortfolio Resumeapi-658308760Pas encore d'évaluation
- FeverDocument45 pagesFeverAsish Geiorge100% (1)
- Welcome Letter For FamiliesDocument3 pagesWelcome Letter For FamiliesChild and Family InstitutePas encore d'évaluation
- AAA Mixed Pain SMGDocument37 pagesAAA Mixed Pain SMGandhita96Pas encore d'évaluation
- Management of Diabetes: DR Rukman Mecca M I 51 ST Batch Calicut Med CollegeDocument47 pagesManagement of Diabetes: DR Rukman Mecca M I 51 ST Batch Calicut Med CollegeRukman MeccaPas encore d'évaluation
- Ilase UM PDFDocument31 pagesIlase UM PDFVijay Prabu GPas encore d'évaluation
- Opioid AnalgesicDocument43 pagesOpioid AnalgesicAnanta MiaPas encore d'évaluation
- BandurasTheory PDFDocument23 pagesBandurasTheory PDFJohncarlo DungogPas encore d'évaluation
- Psychology - Article 38Document1 pagePsychology - Article 38piping stressPas encore d'évaluation
- Abg Case StudiesDocument22 pagesAbg Case StudiesMaria DalalPas encore d'évaluation
- Diagnosis of Iron-Deficiency Anemia in The ElderlyDocument3 pagesDiagnosis of Iron-Deficiency Anemia in The ElderlyGeranyl LaguardiaPas encore d'évaluation
- Intravenous Fluid Guideline-1Document4 pagesIntravenous Fluid Guideline-1Marco CalvaraPas encore d'évaluation
- Kasus AsmaDocument5 pagesKasus AsmaHananun Zharfa0% (3)
- Grandjean 2000Document13 pagesGrandjean 2000Ivan VeriswanPas encore d'évaluation
- Surgical Drains Catheters and Tubes (M)Document120 pagesSurgical Drains Catheters and Tubes (M)nikprov100% (6)
- Anti AcidsDocument8 pagesAnti AcidsMohammad Ali Abu Ma'ashPas encore d'évaluation
- Malaria ModulDocument18 pagesMalaria ModulcheiwinarnoPas encore d'évaluation
- Data StokDocument26 pagesData StokUlfhey ChupidPas encore d'évaluation
- The Truth About ReikiDocument6 pagesThe Truth About ReikiM RezaPas encore d'évaluation
- Level 1: Healing Touch Certificate ProgramDocument2 pagesLevel 1: Healing Touch Certificate Programapi-25955699Pas encore d'évaluation
- Psychiatric MisadventuresDocument10 pagesPsychiatric MisadventuresRob_212Pas encore d'évaluation
- Trans CounselingDocument71 pagesTrans CounselingMolly GumPas encore d'évaluation
- Health Teaching PlanDocument4 pagesHealth Teaching PlanRene John Francisco80% (5)