Académique Documents
Professionnel Documents
Culture Documents
Airways and Ion Doctor Patient UK
Transféré par
Muntasir BashirDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Airways and Ion Doctor Patient UK
Transféré par
Muntasir BashirDroits d'auteur :
Formats disponibles
Airways and Intubation Doctor Patient UKClick here to return to the home page You are here: Home
PatientPlus Airways and Intubation HomeInformation for Patients Information LeafletsDiagrams of Body PartsMedicines & DrugsWebsite DirectoryVideo DirectoryFind A ...Choices When ReferredPoems & StoriesCare & Support Support GroupsFor CarersBenefits & FinanceProfessional Reference PatientPlusUK GuidelinesEvidence Based MedicineTextbooks & JournalsImages, Pictures & AtlasesMedline InformationPharmacy & Medical Equipment Pharmacy ProductsMedical EquipmentRecommended BooksSpecial OffersHelpArticle See also In more detail Your experience News Click here to open a printer-friendly version of this document, in a new window, together with the print dialogue boxClick here to open this document in PDF format This will offer you the usual PDF options i.e. document navigation, search, zoom and formatted print Note: this is the best way to print the documentClick here to listen to the MP3 audio recording of this documentClick here to download the audio recording of this document as a podcast, for listening to at your leisureClick here to open our Dictionaries and Glossaries pageClick here to see related products in our Online Pharmacy Note: this will open in a new windowClick here to add this page to a social bookmarking site of your choiceClick here if you want to find out more about social bookmarking. This link will take you to the Wikipedia explanation Note: this will open in a new windowPrint options Bookmarks Other options
This is a PatientPlus article. PatientPlus articles are written for doctors and so the language can be technical, however some people find that they add depth to the patient information leaflets. You may find the abbreviations record helpful. Airways and Intubation Endotracheal intubation is the placement of a tube into the trachea to maintain a patent airway in those who are unconscious or unable to breathe independently. Compared to the use of pharyngeal airways (oropharyngeal or nasopharyngeal), benefits of an endotracheal airway include: Protection against aspiration and gastric insufflation More effective ventilation and oxygenation Facilitation of suctioning Delivery of anaesthetic and other drugs via the endotracheal tube (ETT) Previously restricted to the anaesthetic and operating rooms, advances such as rapid sequence induction (RSI) have meant that intubation is often performed in emergency or pre-hospital settings.1 These situations are by their nature high-risk and there is some evidence that pre-hospital endotracheal intubation in adult major trauma patients with head injury actually increases mortality.2 Many confounding variables exist - experience levels, lack of monitoring equipment, difficulties pre-oxygenating patients etc - and the studies are retrospective but benefit should not be assumed. Intubation is a technique that requires training, experience and regular updating to maintain competence. Anyone attempting it should also be capable of managing any complications that arise. GPs will vary in their ability: some will
have developed a special interest during hospital training, gained postgraduate qualifications and may even perform regular anaesthetic lists; others will have an interest in pre-hospital and emergency care and may be involved in BASICS or ATLS to maintain relevant skills. The key principle is not to act beyond your personal level of competence. Alternatives to intubation Laryngeal mask airway (LMA): Widely used in UK in more than 50% of surgical patients. Consists of an inflatable silicone ring attached diagonally to a flexible cushion filling the space around and behind the larynx, creating a low pressure seal between the tube and trachea without insertion into the larynx. It can be used in an emergency setting by providers not trained in tracheal intubation and is an option in the management of a difficult airway where intubation has been unsuccessful. It is not a definitive airway and provides limited protection only from gastric aspiration. Oesophageal Tracheal Combitube (ETC): The ETC is a double lumen tube combining an oesophageal tube with closed distal end linked by a short connection to a conventional tracheal tube. It is designed for blind insertion and placement is determined by examination and auscultation and cuffs can be adjusted according to whether the trachea or oesophagus has been intubated. It has been used amongst first responders in North America successfully3 but its use in the pre-hospital setting can also be associated with serious complications such as aspiration pneumonitis, pneumothorax and oesophageal rupture.4 Tracheostomy Indications5 Inability to oxygenate patient (SO2<90%, PaO2<55). Inability to ventilate patient (rising PaCO2, respiratory acidosis, mental status change). Patient unable to protect airway. Anticipated clinical deterioration. Contraindications5 Neck immobility or increased risk of neck trauma (for example, rheumatoid arthritis or suspected cervical spine injury) - consider fibreoptic intubation if available. Inability to open mouth (for example, scleroderma or surgical wiring) consider nasal intubation or surgical airway. Procedure5,6,7Ensure all equipment is in working order: Monitoring equipmentPulse oximeter BP gauge Cardiac monitor Oxygenation equipmentOxygen source and tubing Face mask Anaesthesia bag or ambu-bag Suction equipment Premedication and induction equipmentIV access Review possible contraindications to drugs
Draw up and label all premedication, induction and paralytic agents Intubation equipmentLaryngoscopes with handles and blades of different sizes and shapes (curved/straight) - to estimate laryngoscope blade size, holding the blade held next to the patient's face, the blade should reach between lips and larynx Check light source working and tighten light bulb. Endotracheal tubes of different sizes Inflate ET cuff to check for leakage Means of securing tube in place Equipment for checking tube positionStethoscope CO2 detector or end-tidal CO2 monitor CXR Preparation Preoxygenate with 100% oxygen via well-fitting mask Consider premedications to counteract side-effects of intubation. If conscious, consider RSI Basic RSI Protocol: Preparation and pre-oxygenation - 100% oxygen for 3 minutes time-allowing, if limited 8 deep breaths approximating vital capacity. Rapid acting induction agent to induce loss of consciousness, e.g. midazolam 0.1 mg/kg IV, injected as a push into a fast-running infusion. Use of an induction agent avoids reflex tachycardia, hypertension and rising ICP triggered by intubation with muscle relaxant alone. Other commonly used agents include etomidate, thiopental, propofol.8 Can also add small dose of opioid, e.g. alfentanil.9 Assistant applies cricoid pressure to prevent gastric content regurgitation from the onset of unconsciousness. Neuromuscular blocking agent immediately following the induction agent to achieve paralysis. Succinylcholine is the most commonly used muscle relaxant, favoured for its fast onset and short duration.10 Intubate. Preventing gastric aspiration Always assume in an emergency setting that a patient has a full stomach carrying the risk of regurgitation and inhalation of gastric contents. If possible, liquid contents of the stomach are removed with a nasogastric or orogastric tube. Cricoid pressure is applied from the time of loss of consciousness until a secure airway is in place. Pressure is applied directly in mid-line on the cricoid cartilage using tips of thumb and index finger while possibly applying counter-pressure from back of neck. This occludes the oesophagus again with the aim of reducing gastric aspiration although the evidence for this is disputed.11 Patient position Patient aligned without lateral deviation of head or neck Head extended on neck with pillow under occiput. If cervical spine trauma is suspected, have assistant provide in-line immobilisation.
Neck flexed to approximately 15 degrees on chest. In infants under 2, the occiput naturally extends the head and the chin alone needs lifting into the 'sniffing' position. Inspect mouth for loose teeth or dentures and remove. Suction any secretions or vomitus. Intubation Intubation attempts should not last longer than 30 seconds. Hold laryngoscope in left hand and ETT in right and introduce laryngoscope over right side of tongue, sweeping the tongue to the midline. Position the tip of the blade in the valecula (between the epiglottis and base of tongue) and lift upwards and away from yourself until the glottis is visualised. Exert traction along the axis of the handle - do not use the teeth or gums as a fulcrum as this will result in damage to teeth and/or gums. Introduce the endotracheal tube into the right corner of the mouth, passing it through the vocal cords with the cuff positioned and inflated just beyond the cords. Ventilate with high concentration oxygen and secure endotracheal tube. To assess tube position: Look for symmetrical chest movement. Listen over apices and base of lungs and stomach for equal breath sounds and no gastric breath sounds. End-tidal carbon dioxide monitor attached to ETT. Trouble shooting6 Consider: Dislodged tube Obstructed tube Pneumothorax Equipment failure Complications5 Failed intubation and hypoxaemia: Can ventilate with mask - seek senior help, defer intubation or consider alternative. Can't ventilate - call for urgent assistance; if bag and mask ventilation maintaining oxygen saturations above 90% and there is adequate time, consider other options such as the use of a bougie to guide ETT placement or alternatives such as the use of LMA or Combitube or fibreoptic induction or if not, cricothryoidotomy. See "failed airway" algorithm.5 Aspiration and post-intubation pneumonia Pneumothorax Trauma from laryngoscope: Teeth & soft tissues - avoidable with good technique. Oedema - usually due to repeated attempts. Right mainstem intubation Oesophageal intubation - fatal if unrecognised Hypotension and arrhythmias Vocal cord avulsion Avoiding problems Potential problems in maintaining airway or performing intubation as suggested by presence of: Physical signs, e.g. short immobile neck, receding jaw, limited mouth opening, protruding or unhealthy teeth, large tongue, facial trauma. Injuries to cervical spine limiting movement. Possible airway obstruction, for example as result of severe facial trauma or
burns to airway. Stridor at rest. Anticipate difficult intubations and seek experienced assistance in advance of the intubation attempt if possible.
Document references Wang HE, Kupas DF, Greenwood MJ, et al; An algorithmic approach to prehospital airway management. Prehosp Emerg Care. 2005 Apr-Jun;9(2):145-55. [abstract] Sen A.; Best Evidence Topics (BETS) review of current evidence - Prehospital endotracheal intubation in adult major trauma patients with head injury; BestBETs May 2005 Rabitsch W, Schellongowski P, Staudinger T, et al; Comparison of a conventional tracheal airway with the Combitube in an urban emergency medical services system run by physicians. Resuscitation. 2003 Apr;57(1):27-32. [abstract] Vezina MC, Trepanier CA, Nicole PC, et al; Complications associated with the Esophageal-Tracheal Combitube in the pre-hospital setting. Can J Anaesth. 2007 Feb;54(2):124-8. [abstract] Ashton RW & Burke CM; ATS Endotracheal Intubation by Direct Laryngoscopy (2004) American Thoracic Society Family Practice Notebook; Endotracheal Intubation Lafferty KA, Kulkarni R; Rapid Sequence Intubation. eMedicine, October 2008. Morris J, Cook TM; Rapid sequence induction: a national survey of practice. Anaesthesia. 2001 Nov;56(11):1090-7. [abstract] Lavazais S, Debaene B; Choice of the hypnotic and the opioid for rapid-sequence induction. Eur J Anaesthesiol Suppl. 2001;23:66-70. [abstract] Perry JJ, Lee JS, Sillberg VA, et al; Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. 2008 Apr 16;(2):CD002788. [abstract] Butler J, Sen A; Best evidence topic report. Cricoid pressure in emergency rapid sequence induction. Emerg Med J. 2005 Nov;22(11):815-6. [abstract] Internet and further reading Virtual anaesthesia textbook; (American website) with links and educational resources for airways management. BASICS; British Association for Immediate Care (website); A source of training for those interested in providing pre-hospital care. ATLS; (Advanced Trauma Life Support) - UK contacts for courses and training. Combitube tutorial Henderson JJ, Popat MT, Latto IP, et al; Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004 Jul;59(7):675-94. [abstract] Acknowledgements EMIS is grateful to Dr Chloe Borton for writing this article. The final copy has passed scrutiny by the independent Mentor GP reviewing team. EMIS 2010. Document ID: 1366 Document Version: 23 Document Reference: bgp24465 Last Updated: 2 Nov 2008 Planned Review: 2 Nov 2011 The authors and editors of this article are employed to create accurate and up to date content reflecting reliable research evidence, guidance and best
clinical practice. They are free from any commercial conflicts of interest. Find out more about updating.Let us know what you think Your experience If you'd like to tell us your experience on this subject, please click here Your comments on this document If you're a health professional and the guidance given here is at variance with your clinical practice, then please let us know (0 comments posted) If you're a patient (or a patient group representative) and you think the article can be improved, then please let us know (0 comments posted)Click here to open a printer-friendly version of this document, in a new window, together with the print dialogue boxClick here to open this document in PDF format This will offer you the usual PDF options i.e. document navigation, search, zoom and formatted print Note: this is the best way to print the documentClick here to listen to the MP3 audio recording of this documentClick here to download the audio recording of this document as a podcast, for listening to at your leisureClick here to open our Dictionaries and Glossaries pageClick here to see related products in our Online Pharmacy Note: this will open in a new windowClick here to add this page to a social bookmarking site of your choiceClick here if you want to find out more about social bookmarking. This link will take you to the Wikipedia explanation Note: this will open in a new windowPrint options Bookmarks Other options Article See also In more detail Your experience News Advertisement Want to search some more? Use the Google Search box below to search our site. Advertisements
Disclaimer: Patient UK has no control over the content of any external links above. Inclusion does not imply endorsement by Patient UK. Want to advertise on this site? Find out how >>Disclaimer/Terms About Us Contact/Feedback Advertise with us Quality Control Licence Data Searchbox Careers Awards Site Map Copyright 2011 EMIS Advertisement
Vous aimerez peut-être aussi
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
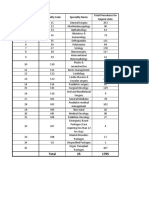
- All PackageRates (ABPMJAY) PDFDocument300 pagesAll PackageRates (ABPMJAY) PDFSumit Soni0% (1)
- Alcoholic Liver DiseaseDocument70 pagesAlcoholic Liver Diseaseaannaass nPas encore d'évaluation
- CHN Study GuideDocument5 pagesCHN Study GuideAshPas encore d'évaluation
- Sample ExamDocument13 pagesSample ExamJenny Mendoza VillagonzaPas encore d'évaluation
- Tumoret e VeshkaveDocument118 pagesTumoret e VeshkavealpePas encore d'évaluation
- Cerebral Blood Flow & StrokeDocument35 pagesCerebral Blood Flow & Stroke-'Henri Djhevon Kaary'-Pas encore d'évaluation
- Actalyke Mini Op Man D6500091JDocument29 pagesActalyke Mini Op Man D6500091Jjyoti ranjanPas encore d'évaluation
- RNI For Malaysians-SummaryDocument2 pagesRNI For Malaysians-SummaryAimi Hannani100% (1)
- E B I W: Safemedicate Rounding Rules GuidelinesDocument9 pagesE B I W: Safemedicate Rounding Rules Guidelineslesky17Pas encore d'évaluation
- 2018 Article 242 PDFDocument57 pages2018 Article 242 PDFOscar NgPas encore d'évaluation
- Bruxism-An Unsolved Problem in Dental MedicineDocument4 pagesBruxism-An Unsolved Problem in Dental Medicinedentace1Pas encore d'évaluation
- A Social Worker's Guide To Narrative Therapy - Daniel-StewartDocument3 pagesA Social Worker's Guide To Narrative Therapy - Daniel-StewartangelaPas encore d'évaluation
- Site-Specific and Stoichiometric Modification of Antibodies by Bacterial TransglutaminaseDocument3 pagesSite-Specific and Stoichiometric Modification of Antibodies by Bacterial Transglutaminasespamemail00Pas encore d'évaluation
- ATARAXIE S7 Cours Par CoursDocument251 pagesATARAXIE S7 Cours Par CoursOussama Hamadi100% (1)
- Developmental DisordersDocument36 pagesDevelopmental DisordersANJIPas encore d'évaluation
- Astm E446 ReqDocument3 pagesAstm E446 ReqwerwewmnlljlajkdPas encore d'évaluation
- Author 'S Accepted ManuscriptDocument24 pagesAuthor 'S Accepted ManuscriptAgal BimaPas encore d'évaluation
- Locomotor SyllabusDocument5 pagesLocomotor SyllabusAyeshaKhalidPas encore d'évaluation
- New Drug Application - WikipediaDocument26 pagesNew Drug Application - Wikipediakabirsahu0019Pas encore d'évaluation
- Sri Lanka NMRA GazetteDocument9 pagesSri Lanka NMRA GazetteSanjeev JayaratnaPas encore d'évaluation
- Demographics: Discharge DocumentationDocument8 pagesDemographics: Discharge Documentationjenny100% (1)
- Interaksi DadahDocument36 pagesInteraksi Dadahnorish7100% (2)
- Operative Hand InstrumentsDocument22 pagesOperative Hand InstrumentsSharad Banker50% (2)
- LipomaDocument51 pagesLipomaAgnes NiyPas encore d'évaluation
- Procedure For Penicillin Skin TestingDocument4 pagesProcedure For Penicillin Skin TestingHarshan Isuru KumaraPas encore d'évaluation
- ARI Company Catalogue PDFDocument29 pagesARI Company Catalogue PDFEd Gar YundaPas encore d'évaluation
- RetailerPriceList OHDocument1 pageRetailerPriceList OHMuhammad Samiur RahmanPas encore d'évaluation
- ENT Summery TABLEDocument19 pagesENT Summery TABLEtaliya. shvetzPas encore d'évaluation
- Fracture of Shoulder and Upper Arm S42Document9 pagesFracture of Shoulder and Upper Arm S42yunitaPas encore d'évaluation
- 9000 One Liner GK PDF in Hindi (For More Book - WWW - Gktrickhindi.com)Document25 pages9000 One Liner GK PDF in Hindi (For More Book - WWW - Gktrickhindi.com)Ashish gautam100% (1)