Académique Documents
Professionnel Documents
Culture Documents
NCP
Transféré par
Abegail AbaygarDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
NCP
Transféré par
Abegail AbaygarDroits d'auteur :
Formats disponibles
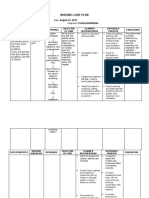
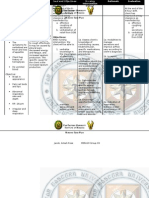
ASSESSMENT
NURSING DIAGNOSIS
PLANNING
INTERVENTIONS
RATIONALE
EVALUATION
Subjective: Nahihirapan huminga si lola dahil sa plema, as verbalized by the patient relative. Objective: productive cough sputum is thick and brownish in color crackles DOB Deep breathing irritability
Ineffective Airway Clearance related to presence of Secretions secondary to Community acquired pneumonia
After 2 hours of nursing interventions, the clients respiration will improve and difficulty of breathing will be Relieved.
Monitor RR, taking note of the depth and rate, BP, PR Auscultate lung fields, noting presence of adventitious breath sounds Elevate head of bed to high fowlers
To establish baseline data and monitor changes To determine possible bronchospasm or obstruction To facilitate breathing and lung expansion To facilitate in the expulsion of mucus
After 2 hours of nursing intervention, goal was not met as evidenced by an increase in the depth and rate of respirations due to an increase in difficulty of breathing.
Provide health teachings regarding coughing and deep breathing exercise. Encourage client to increase fluid intake to about 2000 mL Administer medications such as expectorants as ordered
To liquefy secretions
To reduce bronchospasm and mobilize secretions
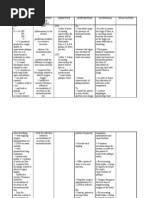
ASSESSMENT
NURSING DIAGNOSIS
PLANNING
INTERVENTIONS
RATIONALE
EVALUATION
Subjective : Nanghihina si lola as verbalized by the patient relative. Objective: Ineffective cough Restlessness Use of accessory muscles when breathing Loss of appetite Poor muscle tone
Imbalanced nutrition: less than body requirements related to inadequate intake of nutritious foods secondary to underlying disease as evidenced by loss of appetite and body weakness.
OBJECTIVE: After 5 hours of nursing intervention, the patient will regain body strength and loss of appetite will be relieved. GOAL: At the end of the nursing rotation, the patient will demonstrate behaviours, to regain or and or maintain appropriate weight.
Determine clients ability to chew, swallow, and taste food. Assess drug interactions, disease effects, allergies. Auscultate bowel sounds. Note characteristics of stool (color, amount, frequency etc.) Evaluate total daily food intake. Obtain diary of calorie intake, patterns and times of eating. Emphasize importance of well-balanced nutritious intake.
To determine factors that can affect ingestion and digestion of nutrients. To determine factors that may affect appetite, food intake or absorption. To evaluate degree of deficit
After 5 hours of nursing intervention, the patient regained body strength and loss of appetite has been relieved.
V/s
BP- 140/80 mm/Hg T -36.6 C P- 102 bpm R -41 cpm
To reveal possible cause of malnutrition/change s that could be made in clients intake. To promote wellness
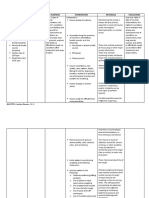
ASSESSMENT
NURSING DIAGNOSIS
PLANNING
INTERVENTIONS
RATIONALE
EVALUATION
Subjective : none Objective: V/S BP: 140/80 mmHg T: 36.6 C P: 100 bpm R: 44 cpm With AB With ET DOB Restlessness Irritability
Impaired gas exchange related to ventilation perfusion imbalance.
After 8 hours of nursing intervention the patient will be able to: 1. Demonstrate improved ventilation and adequate oxygenation of tissues by HBGs within clients normal limits. 2. Participate in treatment regimen (e.g., breathing exercises, effective coughing, and use of oxygen) within level of ability/situation. 3. Verbalize understanding of causative factors and appropriate intervention.
Independent: 1. Elevated head of bed/position client appropriately, provide airway adjuncts and suction as indicated. 2. Encouraged frequent deep breathing/ coughing exercises. 3. Auscultated breath sounds noting crackles, wheezes
Independent: 1. To maintain airway
Goal -Met: After 8 hours of nursing intervention the patient was able to demonstrate improved ventilation and
2. Promotes optimal chest expansion and drainage of secretions.
adequate oxygenation of tissues by HBGs within clients normal limits.
3. Reveals presence of pulmonary congestion/ collection of secretion, indicating need for further intervention.
Collaborative: 1. Assisted with procedures as individually indicated (e.g., transfusion, phlebotomy, bronchoscopy.
Collaborative: 1. To improve respiratory function/ oxygen-carrying capacity.
Vous aimerez peut-être aussi
- NCP - CapDocument4 pagesNCP - CapSherryPas encore d'évaluation
- Assessing and Managing Respiratory DistressDocument3 pagesAssessing and Managing Respiratory DistressGen RodriguezPas encore d'évaluation
- NCP Ineffective Breathing PatternDocument3 pagesNCP Ineffective Breathing PatternNecheal BaayPas encore d'évaluation
- Nursing Care Plan for Ineffective Airway ClearanceDocument1 pageNursing Care Plan for Ineffective Airway ClearanceLhexie CooperPas encore d'évaluation
- NCP Ineffective Airway Clearance Related To Lung Impairment PNEUMOTHORAXDocument5 pagesNCP Ineffective Airway Clearance Related To Lung Impairment PNEUMOTHORAXMa. Elaine Carla Tating0% (2)
- Assessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveDocument2 pagesAssessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveDanica Kate GalleonPas encore d'évaluation
- Promoting Activity Tolerance in a Patient with CoughDocument3 pagesPromoting Activity Tolerance in a Patient with CoughitsmeayaPas encore d'évaluation
- NCP DobDocument2 pagesNCP DobIvy Mary Grace TanguiligPas encore d'évaluation
- Nursing Care Plan For PcapDocument6 pagesNursing Care Plan For PcapMadsPas encore d'évaluation
- Body Weakness NCPDocument1 pageBody Weakness NCPArnold Christian QuilonPas encore d'évaluation
- NCP PneumoniaDocument2 pagesNCP Pneumonia_garonPas encore d'évaluation
- NCP For CTTDocument2 pagesNCP For CTTKay D. BeredoPas encore d'évaluation
- NCPDocument3 pagesNCPWendy EscalantePas encore d'évaluation
- NCP: Acute GastroenteritisDocument3 pagesNCP: Acute GastroenteritishauteanicolePas encore d'évaluation
- Ineffective Airway ClearanceDocument6 pagesIneffective Airway ClearanceBenly Grace Rebuyon MosquedaPas encore d'évaluation
- NCP PediaDocument2 pagesNCP PediaJacinth Rizalino40% (5)
- NCP - Acute Pain Related To EdemaDocument2 pagesNCP - Acute Pain Related To EdemaChenime Añana0% (1)
- Ineffective Airway Clearance (Retained Secretions)Document1 pageIneffective Airway Clearance (Retained Secretions)Danna Tan50% (2)
- NCP For Ineffective Airway ClearanceDocument3 pagesNCP For Ineffective Airway ClearanceJennelyn BaylePas encore d'évaluation
- Cap NCPDocument2 pagesCap NCPkyshb100% (2)
- BSNURSE: NCP - HypertensionDocument3 pagesBSNURSE: NCP - Hypertensionmickey_beePas encore d'évaluation
- Nursing Care Plan: References: Nurse's Pocket Guide Pages 151-155Document1 pageNursing Care Plan: References: Nurse's Pocket Guide Pages 151-155Caroline ChaPas encore d'évaluation
- Disturbed Sleep PatternDocument2 pagesDisturbed Sleep PatternROxanne S. RendonPas encore d'évaluation
- Nursing Care Plan - Ineffective Airway ClearanceDocument1 pageNursing Care Plan - Ineffective Airway ClearanceLei OrtegaPas encore d'évaluation
- NCP Ineffective Airway ClearanceDocument4 pagesNCP Ineffective Airway ClearanceMary Joyce Limoico100% (1)
- NCP DobDocument1 pageNCP DobsarahAcristobalPas encore d'évaluation
- NCPDocument4 pagesNCPAnn AquinoPas encore d'évaluation
- NCP Ineffective Airway Clearance Related To Excessive Mucus Production COPDDocument7 pagesNCP Ineffective Airway Clearance Related To Excessive Mucus Production COPDMa. Elaine Carla Tating67% (3)
- NCP DMDocument6 pagesNCP DMstara123Pas encore d'évaluation
- NCP - Ineffective Airway ClearanceDocument4 pagesNCP - Ineffective Airway ClearanceJet BautistaPas encore d'évaluation
- Risk For Infection - NCPDocument3 pagesRisk For Infection - NCPHamil BanagPas encore d'évaluation
- Ineffective Breathing PatternDocument2 pagesIneffective Breathing PatternEna Katherine CanonoPas encore d'évaluation
- NCPDocument1 pageNCPJ. ishtellePas encore d'évaluation
- FDAR (After Tracheostomy)Document2 pagesFDAR (After Tracheostomy)Maribeth DantesPas encore d'évaluation
- Assessment Subjective: "Nahihirapan Ako Huminga" As VerbalizedDocument2 pagesAssessment Subjective: "Nahihirapan Ako Huminga" As Verbalizedmayla_jordan3666Pas encore d'évaluation
- Goal:: Ineffective Airway Clearance Related To Cumulation of SecretionDocument4 pagesGoal:: Ineffective Airway Clearance Related To Cumulation of SecretionWyen CabatbatPas encore d'évaluation
- Nursing Care Plan ADocument6 pagesNursing Care Plan ACrystal WyattPas encore d'évaluation
- NCP DobDocument2 pagesNCP DobTata Wendz100% (1)
- Nursing Care Plans of Bronchial AsthmaDocument8 pagesNursing Care Plans of Bronchial AsthmaKannanPas encore d'évaluation
- NCP Impaired Gas Exchange STROKEDocument2 pagesNCP Impaired Gas Exchange STROKEMa. Elaine Carla TatingPas encore d'évaluation
- I. Nursing Care Plan Assessment Diagnosis Planning Intervention EvaluationDocument3 pagesI. Nursing Care Plan Assessment Diagnosis Planning Intervention EvaluationCherubim Lei DC FloresPas encore d'évaluation
- NCP - Fluid RetentionDocument3 pagesNCP - Fluid RetentionMichelle Teodoro100% (1)
- NCP Ineffective Breathing ActualDocument3 pagesNCP Ineffective Breathing ActualArian May Marcos100% (1)
- NCP For AsthmaDocument1 pageNCP For AsthmaMelvin Martinez100% (1)
- Nursing Care Plan Impaired ComfortDocument3 pagesNursing Care Plan Impaired ComfortAldwin Louis EstradaPas encore d'évaluation
- Impaired Gas Exchange-Sample NCPDocument1 pageImpaired Gas Exchange-Sample NCPKaycee BinanPas encore d'évaluation
- Respiratory Failure NCPDocument1 pageRespiratory Failure NCPkyaw100% (1)
- Lopez, Maria Sofia B. 10/07/2020 3-BSN-B Prof. Zoleta: Nursing Care Plan: PneumoniaDocument9 pagesLopez, Maria Sofia B. 10/07/2020 3-BSN-B Prof. Zoleta: Nursing Care Plan: PneumoniaSofia Lopez100% (2)
- NCP LatestDocument6 pagesNCP LatestThirdy AquinoPas encore d'évaluation
- Assessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationDocument3 pagesAssessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationAlyssa Moutrie Dulay Arabe100% (1)
- Monitor and regulate body temperature for patient with hyperthermiaDocument2 pagesMonitor and regulate body temperature for patient with hyperthermiaDudong SasakiPas encore d'évaluation
- Health Teaching Plan DyspneaDocument3 pagesHealth Teaching Plan DyspneaMae JavierPas encore d'évaluation
- Ineffective Breathing Pattern Nursing DiagnosisDocument2 pagesIneffective Breathing Pattern Nursing DiagnosisChristianmel JavierPas encore d'évaluation
- Nursing Care Plan Bronchial AsthmaDocument2 pagesNursing Care Plan Bronchial AsthmaSummer Ilu100% (1)
- FEver NCPDocument1 pageFEver NCPSam AlipioPas encore d'évaluation
- Drug Study and NCP!Document8 pagesDrug Study and NCP!Abegail Abaygar100% (1)
- Nursing Care PlanDocument9 pagesNursing Care PlanjmichaelaPas encore d'évaluation
- Revised NCP (Baiae)Document9 pagesRevised NCP (Baiae)Jennifer BactatPas encore d'évaluation
- Ncp'sDocument8 pagesNcp'sDuchess Kleine RafananPas encore d'évaluation
- NCPDocument11 pagesNCPJaziel Remo100% (1)
- Definition of TermsDocument2 pagesDefinition of TermsAbegail AbaygarPas encore d'évaluation
- HemmorhoidectomyDocument3 pagesHemmorhoidectomyAbegail AbaygarPas encore d'évaluation
- Nursing Care Plan !Document2 pagesNursing Care Plan !Abegail AbaygarPas encore d'évaluation
- Concept Map - Abby !Document2 pagesConcept Map - Abby !Abegail AbaygarPas encore d'évaluation
- Drug Study and NCP!Document8 pagesDrug Study and NCP!Abegail Abaygar100% (1)
- INDIRECT QUESTIONS AND REPORTED SPEECHDocument7 pagesINDIRECT QUESTIONS AND REPORTED SPEECHOmar Chavez100% (1)
- Alcoholic BeveragesDocument101 pagesAlcoholic BeveragesAmazing Grace Dela Cruz100% (2)
- Business Environment: Swot Analyasis Report OnDocument24 pagesBusiness Environment: Swot Analyasis Report OnMohammed ArsiwalaPas encore d'évaluation
- Thirst - C.A. JohnsonDocument92 pagesThirst - C.A. JohnsonMaddy MullaheyPas encore d'évaluation
- Fishing For More Than FishDocument3 pagesFishing For More Than FishKaren FuentesPas encore d'évaluation
- Houston Family of West Tennessee Cookbook & MemoirsDocument159 pagesHouston Family of West Tennessee Cookbook & MemoirsMelissa Melsa BrownPas encore d'évaluation
- Integrated Rice and Duck Farming - Takao Furuno CaseDocument2 pagesIntegrated Rice and Duck Farming - Takao Furuno CaseRija Ménagé100% (1)
- Express Review Guides VocabularDocument200 pagesExpress Review Guides VocabularIgor R Souza100% (2)
- Abstinence Journal ReflectionDocument3 pagesAbstinence Journal Reflectionapi-451295416Pas encore d'évaluation
- 1 Introduction To The SubjectDocument41 pages1 Introduction To The SubjectMiera SaidPas encore d'évaluation
- 2 Questions 1-5 3 3: KET Handbook 2004 - Listening Sample Test 2 KET Handbook 2004 - Listening Sample Test 2Document3 pages2 Questions 1-5 3 3: KET Handbook 2004 - Listening Sample Test 2 KET Handbook 2004 - Listening Sample Test 2Mario Abel Vega Perez100% (1)
- In The Earliest CitiesDocument2 pagesIn The Earliest CitiessingenaadamPas encore d'évaluation
- Assess supplier vulnerability matrixDocument10 pagesAssess supplier vulnerability matrixNewhame Dagne100% (1)
- Tariff Rulings MARCH 2022 Final 3 1Document22 pagesTariff Rulings MARCH 2022 Final 3 1milanPas encore d'évaluation
- Processing of Honey A ReviewDocument19 pagesProcessing of Honey A ReviewReniPas encore d'évaluation
- SITHCCC037-Major-assessment-C-V1 0 Docx v1 0Document6 pagesSITHCCC037-Major-assessment-C-V1 0 Docx v1 0cecelee222Pas encore d'évaluation
- Format Đề Thi Không Chuyên Ptnk: Phần Trắc NghiệmDocument13 pagesFormat Đề Thi Không Chuyên Ptnk: Phần Trắc NghiệmQuảng TuyềnPas encore d'évaluation
- 1 LecDocument2 pages1 LecMaricel Sanchez - CostillasPas encore d'évaluation
- Pig - Roald DahlDocument1 pagePig - Roald DahlONE2MIRRORPas encore d'évaluation
- Collective Nouns WorksheetsDocument14 pagesCollective Nouns WorksheetsGina Singh100% (1)
- Wine DrinksDocument2 pagesWine DrinkseatlocalmenusPas encore d'évaluation
- Chapter 1-3Document35 pagesChapter 1-3pontiveros.fc67% (3)
- Chapter IIDocument13 pagesChapter IITaguno ChrisPas encore d'évaluation
- Gastronomy Tourism Events & DestinationsDocument10 pagesGastronomy Tourism Events & DestinationsRita SalibaPas encore d'évaluation
- Unit Fraction Word Problems: AnswersDocument1 pageUnit Fraction Word Problems: AnswersShon EllisonPas encore d'évaluation
- Sorsu Shipboarding 2024 With Cebu Bohol TourDocument3 pagesSorsu Shipboarding 2024 With Cebu Bohol TouriamrezelmPas encore d'évaluation
- Maintain Hospitality Industry KnowledgeDocument234 pagesMaintain Hospitality Industry Knowledgenyoman pastikaPas encore d'évaluation
- YLE Practice Tests Plus Starter SB 2nd EdDocument79 pagesYLE Practice Tests Plus Starter SB 2nd EdAli Raza100% (17)
- Rephrasing C1Document7 pagesRephrasing C1Pablo AlejandroPas encore d'évaluation
- Past Simple and Past Continuous WorksheetDocument3 pagesPast Simple and Past Continuous WorksheetAna MateusPas encore d'évaluation