Académique Documents
Professionnel Documents
Culture Documents
TF 0692815164 Pai Assessment
Transféré par
racopDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
TF 0692815164 Pai Assessment
Transféré par
racopDroits d'auteur :
Formats disponibles
PAIN ASSESSMENT
G STRUCTURE AND FUNCTION
DEFINITION
The International Association for the Study of Pain (IASP) denes pain as an unpleasant sensory and emotional experience, which we primarily associate with tissue damage or describe in terms of such damage, or both. Recent literature has emphasized the importance of pain and recommended it being the fth vital sign. Some states in the United States have passed laws necessitating the adoption of an assessment tool and documenting pain assessment in patient charts along with temperature, pulse, heart rate and blood pressure (see Chapter 7).
PATHOPHYSIOLOGY
Several theories attempt to explain the concept of pain. Melzack and Wall in 1965 proposed the gate control model emphasizing the importance of the central nervous system mechanisms of pain; this model has inuenced pain research and treatment. Pain is explained as a combination of physiologic phenomena in addition to a psychosocial aspect that inuences the perception of pain. The pathophysiologic phenomenon of pain is summarized by the processes of transduction, transmission, modulation, and perception. Transduction of pain begins when a mechanical, thermal or chemical stimulus results in tissue injury or damage stimulating the nociceptors, which are the primary afferent nerves for receiving painful stimuli. Nociceptors are distributed in the body in the skin, subcutaneous tissue, skeletal muscles, and joints. Pain receptors are also located in the peritoneal surfaces, pleural membranes, dura mater, and blood vessel walls rather than in the parenchyma of
visceral organs. Noxious stimuli initiate a painful stimulus resulting in an inammatory process, which leads to the release of cytokines and neuropeptides from circulating leukocytes, platelets, vascular endothelial cells, immune cells, and cells from within the peripheral nervous system. This results in the activation of the primary afferent nociceptors (A-delta and C-bers). Furthermore, the nociceptors themselves release a substance P that enhances nociception, causing vasodilatation, increased blood ow, and edema with further release of bradykinin, serotonin from platelets, and histamine from mast cells. A-delta primary afferent bers (small-diameter, lightly myelinated bers) and C-bers (unmyelinated, primary afferent bers) are classied as nociceptors because they are stimulated by noxious stimuli. A-delta primary afferent bers transmit fast pain to the spinal cord within 0.1 second, which is felt as pricking, sharp, or electric quality sensation and usually caused by mechanical or thermal stimuli. C-fibers transmit slow pain within 1 second, which is felt as burning, throbbing or aching and is caused by mechanical, thermal or chemical stimuli usually resulting in tissue damage. By the direct excitation of the primary afferent fibers, the stimulus leads to the activation of the fiber terminals. The transmission process is initiated by this inammatory process, resulting in the conduction of an impulse in the primary afferent neurons to the dorsal horn of the spinal cord. There, neurotransmitters are released and concentrated in the substantia gelatinosa (which is thought to host the gating mechanism described in the gate control theory) and bind to specic receptors. The output neurons from the dorsal horn cross the anterior white commissure and ascend the spinal cord in the anterolateral quadrant in two ascending pathways (Fig. 8-1): 1. Spinothalamic tract (STT): ascends through the lateral edge of the medulla, lateral pons, and midbrain to the thalamus then to the somatosensory cortex. It
107
108
U N I T III
NURSING ASSESSMENT OF THE ADULT Postcentral gyrus
Chronic non-malignant pain: usually associated with a specic cause or injury and is described as a constant pain that persists more than 6 months Cancer pain: often due to the compression of peripheral nerves or meninges or from the damage to these structures following surgery, chemotherapy, radiation, or tumor growth and infiltration Pain is also described as transient pain, tissue injury pain (surgical pain, trauma-related pain, burn pain, iatrogenic pain as a result of an intervention), and chronic neuropathic pain. Also pain is viewed in terms of its intensity and location.
Ascending pathways
Thalamus
PHYSIOLOGIC RESPONSES TO PAIN
A-delta C Spinal cord
Pain elicits a stress response in the human body triggering the sympathetic nervous system, resulting in physiologic responses such as the following: Anxiety, fear, hopelessness, sleeplessness, thoughts of suicide Focus on pain, reports of pain, cries and moans, frowns and facial grimaces Decrease in cognitive function, mental confusion, altered temperament, high somatization, and dilated pupils Increased heart rate, peripheral, systemic, and coronary vascular resistance, blood pressure Increased respiratory rate and sputum retention resulting in infection and atelactasis Decreased gastric and intestinal motility Decreased urinary output resulting in urinary retention, uid overload, depression of all immune responses Increased antidiuretic hormone, epinephrine, norepinephrine, aldosterone, glucagons, decreased insulin, testosterone Hyperglycemia, glucose intolerance, insulin resistance, protein catabolism Muscle spasm resulting in impaired muscle function and immobility, perspiration
Figure 8-1 Pathways for transmitting pain.
transmits location, quality, and intensity of acute pain and threatening events. 2. Spinoreticular tract (SRT): ascends to the reticular formation, the pontine, medullary areas, and medial thalamic nuclei. It transmits pain information from the brainstem to the limbic area through noradrenergic bundles. Modulation of pain is a difcult phenomenon. Modulation inhibits the pain message and involves the bodys own endogenous neurotransmitters (endorphins, enkephalins, and serotonin) in the course of processing the pain stimuli. The process of pain perception is still poorly understood. Studies have shown that the emotional status (depression and anxiety) affects directly the level of pain perceived and thus reported by patients. The hypothalamus and limbic system are responsible for the emotional aspect of the pain perception while the frontal cortex is responsible for the rational interpretation and response to pain.
G HEALTH ASSESSMENT
COLLECTING SUBJECTIVE DATA: THE NURSING HEALTH HISTORY
There are few objective findings on which the assessment of pain can rely. Pain is a subjective phenomenon and thus the main assessment lies in the clients reporting. The clients description of pain is quoted. The exact words used to describe the experienced of pain are used
CLASSIFICATION
Pain has many different classifications. Common categories of pain include acute, chronic non-malignant, and cancer pain. Acute pain: usually associated with an injury with a recent onset and duration of less than 6 months and usually less than a month
CHAPTER 8
PAIN ASSESSMENT
109
to help in the diagnosis and management. Pain, its onset, duration, causes, alleviating and aggravating factors are assessed. Then the quality, intensity and the effects of
pain on the physical, psychosocial, and spiritual aspects are questioned. Past experience with pain in addition to past and current therapies are explored.
GG HISTORY OF PRESENT HEALTH CONCERN
Review JCAHO standards (Display 8-1) and tips for collecting subjective data (Display 8-2) before assessing the clients subjective experience of pain. Use the COLDSPA mnemonic as a guideline for information to collect. In addition, the following questions help elicit important information. Following JCAHO standards and tips for collecting subjective data will enhance evaluation of the clients personal experience of pain.
C O L D S P A
C H A R A C T E R : Describe the sign or symptom. How
does it feel, look, sound, smell, and so forth?
O N S E T : When did it begin? L O C A T I O N : Where is it? Does it radiate? D U R A T I O N : How long does it last? Does it recur? S E V E R I T Y : How bad is it? P A T T E R N : What makes it better? What makes
it worse?
A S S O C I A T E D F A C T O R S : What other symptoms
occur with it?
DISPLAY 8-1
JCAHO STANDARDS FOR PAIN MANAGEMENT
Recognize patients rights to appropriate assessment and management of pain. Screen for pain and assess the nature and intensity of pain in all patients. Record assessment results in a way that allows regular reassessment and follow-up. Determine and ensure that staff is competent in assessing and managing pain. Address pain assessment and management when orienting new clinical staff. Establish policies and procedures that support appropriate prescribing of pain medications. Ensure that pain doesnt interfere with a patients participation in rehabilitation. Educate patients and their families about effective pain management. Address patient needs for symptom management in the discharge planning process. Establish a way to collect facility-wide data to monitor the appropriateness and effectiveness of the pain management plan.
Joint Commission on Accreditation of Healthcare Organizations. [Retrieved from: http/www.jcaho.com]
DISPLAY 8-2
TIPS FOR COLLECTING SUBJECTIVE DATA
Maintain a quiet and calm environment that is comfortable for the patient being interviewed. Maintain the clients privacy and ensure condentiality. Ask the questions in an open-ended format. Listen carefully to the clients verbal descriptions and quote the terms used. Watch for the clients facial expressions and grimaces during the interview. DO NOT put words in the clients mouth.
110
U N I T III
NURSING ASSESSMENT OF THE ADULT
QUESTION Continued Are you experiencing pain now or have you in the past 24 hours? Where is the pain located?
RATIONALE Continued To establish the presence or absence of perceived pain.
The location of pain helps to identify the underlying cause. Radiating or spreading pain helps to identify the source. For example, chest pain radiating to the left arm is most probably of cardiac origin while the pain that is pricking and spreading in the chest muscle area is probably musculoskeletal in origin. Accompanying symptoms also help to identify the possible source. For example, right lower quadrant pain associated with nausea, vomiting, and the inability to stand up straight is possibly associated with appendicitis. The onset of pain is an essential indicator for the severity of the situation and suggests a source. This helps to identify the precipitating factors and what might have exacerbated the pain. This is also to help identify the nature of the pain. Understanding the course of the pain provides a pattern that may help to determine the source. Clients are quoted so that terms used to describe their pain may indicate the type and source. The most common terms used are: throbbing, shooting, stabbing, sharp, cramping, gnawing, hot-burning, aching, heavy, tender, splitting, tiring-exhausting, sickening, fearful, punishing. Relieving factors help to determine the source and the plan of care. Identifying factors that increase pain helps to determine the source and helps in planning to avoid aggravating factors. This question establishes any current treatment modalities and their effect on the pain. This helps in planning the future plan of care. An open-ended question allows the client to mention anything that has been missed or the issues that were not fully addressed by the above questions.
Does it radiate or spread?
Are there any other concurrent symptoms accompanying the pain?
When did the pain start?
What were you doing when the pain rst started?
Is the pain continuous or intermittent? If intermittent pain, how often do the episodes occur and for how long do they last? Describe the pain in your own words.
What factors relieve your pain?
What factors increase your pain?
Are you on any therapy to manage your pain?
Is there anything you would like to add?
CHAPTER 8
PAIN ASSESSMENT
111
GG PAST HEALTH HISTORY
QUESTION Have you had any previous experience with pain? RATIONALE Past experiences of pain may shed light on the previous history of the client in addition to possible positive or negative expectations of pain therapies.
GG FAMILY HISTORY
QUESTION Does any one in your family experience pain? RATIONALE To assess possible family-related perceptions or any past experiences with persons in pain. To assess how much the pain is interfering with the clients family relations.
How does pain affect your family?
GG LIFESTYLE AND HEALTH PRACTICES
QUESTION What are your concerns about pain? RATIONALE Identifying the clients fears and worries helps in prioritizing the plan of care and providing adequate psychological support. These are the main lifestyle factors that pain interferes with. The more that pain interferes with the clients ability to function in his/her daily activities, the more it will reect on the clients psychological status and thus the quality of life.
How does your pain interfere with the following? General activity Mood/Emotions Concentration Physical ability Work Relations with other people Sleep Appetite Enjoyment of life
112
U N I T III
NURSING ASSESSMENT OF THE ADULT
COLLECTING OBJECTIVE DATA: PHYSICAL EXAMINATION
Objective data are collected by using one of the pain assessment tools. There are many assessment tools, some of which are specic to special types of pain. The main issues in choosing the tool are its reliability and its validity. Moreover, the tool must be clear and, therefore, easily understood by the client, and require little effort from the client and the nurse.
Verbal Descriptor Scale (VDS)
Ranges pain on a scale between mild, moderate and severe (Fig. 8-2).
Wong-Baker Faces Scale (FACES)
Shows different facial expression where the client is asked to choose the face that best describes the intensity or level of pain being experienced; this works well with pediatric clients (see Chapter 29, Fig. 29-3).
Preparing the Client
In preparation for the interview, clients are seated in a quiet, comfortable and calm environment with minimal interruption. Explain to the client that the interview will entail questions to clarify the picture of the pain experienced in order to develop the plan of care.
Numeric Rating Scale (NRS)
Rates pain on a scale from 0 to 10 where 0 reects no pain and 10 reects pain at its worst (Fig. 8-3).
Visual Analog Scale (VAS)
Rates pain on a 10 cm continuum numbered from 0 to 10 where 0 reflects no pain and 10 reflects pain at its worst (Fig. 8-4).
Equipment/Tools
The main tools used are the Verbal Descriptor Scale (VDS), Wong-Baker Faces scale (FACES), Numeric Rating Scale (NRS) and Visual Analog Scale (VAS).
Physical Assessment
During examination of the client, remember these key points:
Simple Descriptive Pain Intensity Scale
No pain
Mild pain
Moderate pain
Severe pain
Very severe pain
Worst possible pain
Figure 8-2 Verbal Descriptor Scale (VDS).
010 Numeric Pain Intensity Scale
0 No pain
5 Moderate pain
10 Worst possible pain
Figure 8-3 Numeric Rating Scale (NRS).
Visual Analog Scale (VAS)*
No pain * A 10-cm baseline is recommended for VAS scales.
Pain as bad as it could possibly be
Figure 8-4 Visual Analog Scale (VAS).
CHAPTER 8
PAIN ASSESSMENT
113
Choose an assessment tool reliable and valid to your culture. Explain to the client the purpose of rating the intensity of pain. Ensure the clients privacy and condentiality.
Respect the clients behavior towards pain and the terms used to express it. Understand that different cultures express pain differently and maintain different pain thresholds and expectations.
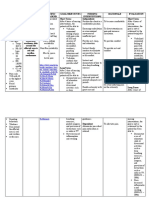
P H Y S I CA L AS S ES S M ENT
Assessment Procedure Normal Findings Abnormal Findings
General Observation
Inspection
Observe posture. Posture is upright when the client appears to be comfortable, attentive, and without excessive changes in position and posture. Client appears to be slumped with the shoulders not straight (indicates being disturbed/uncomfortable). Client is inattentive and agitated. Client might be guarding affected area and have breathing patterns reecting distress. Clients facial expressions indicate distress and discomfort, including frowning, moans, cries, and grimacing. Eye contact is not maintained, indicating discomfort. Edema of a joint may indicate injury. Pain may result in muscle tension. Bruising, wounds, or edema may be the result of injuries or infections, which may cause pain.
Observe facial expression.
Client smiles with appropriate facial expressions and maintains adequate eye contact.
Inspect joints and muscles.
Joints appear normal (no edema); muscles appear relaxed. No inconsistency, wounds, or bruising is noted.
Observe skin for scars, lesions, rashes, changes or discoloration.
Vital Signs
Inspection
Measure heart rate. Heart rate ranges from 60 to 100 beats per minute. Respiratory rate ranges from 12 to 20 breaths per minute. Blood pressure ranges from: Systolic: 100 to 130 mmHg Diastolic: 60 to 80 mmHg. Increased heart rate may indicate discomfort or pain. Respiratory rate may be increased, and breathing may be irregular and shallow. Increased blood pressure often occurs in severe pain.
Measure respiratory rate.
Measure blood pressure.
Note: Refer to physical assessment chapter appropriate to affected body area. Body system assessment will include techniques for assessing for pain, e.g., palpating the abdomen for tenderness and performing range of motion test on the joints.
114
U N I T III
NURSING ASSESSMENT OF THE ADULT
VALIDATING AND DOCUMENTING FINDINGS
Validate the pain assessment data you have collected. This is necessary to verify that the data are reliable and accurate. Document the assessment data following the health care facility or agency policy.
Selected Nursing Diagnoses
Following is a listing of selected nursing diagnoses (wellness, risk, or actual) that you may identify when analyzing the cue clusters.
Wellness Diagnoses
Readiness for enhanced spiritual well-being related to coping with prolonged physical pain Readiness for enhanced comfort level
Sample Documentation of Subjective Data
Ms. S.B. is a 68-year-old female patient known previously as having osteoporosis. This visit she presents with low back pain, burning in nature, radiating to the left lower extremity associated with tingling and numbness sensation of the lower extremity. The pain is continuous and exacerbates mostly in the morning and after any movement. Pain is moderately relieved by pain medications and rest. Pain is intervening with my activities of daily life. I am not able to bathe, dress, and perform the daily household chores. Also, I am not able to concentrate on my work anymore. I cannot sleep at night and I seem not to enjoy anything lately. Using the Visual Analog Scale (VAS), Ms. S.B. rates her pain to be 8/10.
Risk Diagnoses
Risk for activity intolerance related to chronic pain and immobility Risk for constipation related to nonsteroidal antiinammatory agents or opiates intake or poor eating habits Risk for spiritual distress related to anxiety, pain, life change, and chronic illness Risk for powerlessness related to chronic pain, healthcare environment, pain treatment-related regimen
Actual Diagnoses
Acute pain related to injury agents (biological, chemical, physical, or psychological) Chronic pain related to chronic inammatory process of rheumatoid arthritis Ineffective breathing pattern related to abdominal pain and anxiety Disturbed energy eld related to pain and anxiety Fatigue related to stress of handling chronic pain Impaired physical mobility related to chronic pain Bathing/hygiene self-care decit related to severe pain (specify)
Sample Documentation of Objective Data
Client comes in leaning on her daughter and has difculty sitting down on the chair. Her posture is not upright and she seems to be irritated. She is frowning and grimacing most of the time. Focusing on her pain, she is unable to concentrate and continue an idea. Her HR = 108 beats/min, RR = 22 breaths/min, BP = 135/80 mmHg.
Selected Collaborative Problems
After grouping the data, certain collaborative problems may become apparent. Remember that collaborative problems differ from nursing diagnoses in that they cannot be prevented by nursing intervention. However, these physiologic complications of medical conditions can be detected and monitored by the nurse. In addition, the nurse can use physician- and nurse-prescribed interventions to minimize the complications of these problems. The nurse may also have to refer the client in such situations for further treatment of the problem. Following is a list of collaborative problems that may be identied when obtaining a general impression. These problems are worded as Potential Complications (or PC), followed by the problem. PC: Angina PC: Decreased cardiac output PC: Endocarditis PC: Peripheral vascular insufciency PC: Paralytic ileus/small bowel obstruction
G ANALYSIS OF DATA
DIAGNOSTIC REASONING: POSSIBLE CONCLUSIONS
After collecting subjective and objective data pertaining to the pain assessment, identify abnormal ndings and client strengths. Then, cluster the data to reveal any signicant patterns or abnormalities. These data may then be used to make clinical judgments about the status of the clients pain.
CHAPTER 8
PAIN ASSESSMENT
115
PC: Sickling crisis PC: Peripheral nerve compression PC: Corneal ulceration PC: Osteoarthritis PC: Joint dislocation PC: Pathologic fractures PC: Renal calculi
Medical Problems
After grouping the data, the clients signs and symptoms may clearly require medical diagnosis and treatment. Referral to a primary care provider is necessary.
C A S E
S T U DY
The case study demonstrates how to analyze pain assessment data for a specific client. The critical thinking exercises included in the study guide/lab manual and interactive product that complement this text also offer opportunities to analyze assessment data.
L.B. is a 55-year-old male divorced with two children who works as a nancial manager at a company. Two years ago, he experienced difculty urinating and burning upon urination. Tests revealed prostate cancer. Mr. L.B. underwent prostatectomy followed by cycles of chemotherapy 1 year ago. For the past 8 to 10 months, he has complained of continuous low back pain and leg pain that exacerbates at night and while walking. I sometimes feel that I will fall down while walking and at night I am awakened by stabbing deep dull pain in my legs. I am not able to sleep at night and during the day I feel tired and unable to proceed with my work, especially meeting my clients. Mr. L.B. also reports decreased appetite and weight loss of around 6 kg in the past 3 months. During the physical exam, Mr. L.B. entered the room limping and sat on the chair with his shoulders slumped. He changes his position every 2 to 3 minutes looking anxious and uncomfortable with frowns and grimaces as facial expressions. He rates his pain on average on the Visual Analog Scale (VAS) to be 7/10. Vital signs: HR =110 beats/min, RR =22 breaths/min, BP =135/85 mmHg. The following concept map illustrates the diagnostic reasoning process.
116
U N I T III
NURSING ASSESSMENT OF THE ADULT
Diagnosed with prostate cancer; treated with surgery and chemotherapy 1 year ago Low back and leg pain while walking and at night Pain is stabbing, deep and dull Not able to sleep at night I feel tired and unable to proceed with my work Decreased appetite and weight loss Rates pain on the Visual Analog Scale (VAS) to be 7/10 on average I am awakened by stabbing pain
Entered the room limping Sat on the chair with his shoulders slumped Changes his position every 23 minutes Appears anxious and uncomfortable Frowns and grimaces Vital signs: HR = 110 beats/min, RR = 22 breaths/min, BP = 135/85 mmHg ROM tests of legs: Standing: lifts knees only 20 degrees from straight position when asked to march in place. Lying: able to lift each leg with knee unbent 15 degrees before pain starts; lying prone, able to lift each leg only 10 degrees before pain.
Diagnosed with prostate cancer treated with surgery/chemotherapy 1 year ago Pain is stabbing, deep and dull; increasing for the past 810 months Pain on average 7/10 on the VAS Continuous low back pain and leg pain that exacerbates at night and while walking
I sometimes feel that I will fall down while walking and at night I am awakened by stabbing deep dull pain in my legs Limited ROM or legs w/pain Ability to lift knees in standing position for marching/walking decreased
Not able to sleep at night Pain exacerbates at night
Increased respirations and pulse Frowns and grimaces as facial expressions Sat on the chair with his shoulders slumped Changes his position every 23 minutes I feel tired and unable to proceed with my work Unable to sleep because of pain
Client has an onset of pain which is worrying him. Refer for medical investigation and diagnosis
Client has difficulty in mobility affecting his work
Client is awakened by his pain and his inability to sleep is affecting his performance during the day time
Client is uncomfortable and shows facial expressions relating to being distressed and his posture is not straight; vital signs increased in line with discomfort or anxiety
Chronic pain increasing r/t unknown cause
Impaired Physical Mobility r/t the pain
Sleep Deprivation r/t prolonged physical discomfort
Anxiety r/t prolonged pain affecting daily activities
Major: 7/10 continuous and increasing deep stabbing and dull pain for the past 810 months
Major: Limited ROM limited ability to perform gross motor activities
Major: Daytime drowsiness, decreased ability to function, tiredness, anxious, inability to concentrate
Major: Restlessness, concern over effect of pain on lifestyle, anxious, increased respiration, increased pulse, sleep disturbance, increased blood pressure, awareness of physiologic symptoms
Confirm the diagnosis because it meets the defining characteristics and is confirmed by the client
Confirm the diagnosis because it meets the defining characteristics and is confirmed by the client
Confirm the diagnosis because it meets the defining characteristics and is confirmed by the client
Confirm the diagnosis because it meets the defining characteristics and is confirmed by the client
Chronic Pain (increasing) r/t unknown cause Impaired Physical mobility r/t the pain Sleep Deprivation r/t prolonged physical discomfort Anxiety r/t prolonged pain affecting daily activities
PC: Prostate cancer metastasis
CHAPTER 8
PAIN ASSESSMENT
117
References and Selected Readings
Carrier-Kohlman V., Lindsey, A. M., & West, C. M. (2003). Pathophysiologic phenomena in nursing: Human response to illness (3rd ed., pp. 235254). St. Louis: Saunders. NANDA International. (2005). Nursing diagnoses: Denition & classication 20052006. Philadelphia: NANDA International. Price, S. A., & Wilson, L. M. (1997). Pathophysiology, clinical concepts of disease process (5th ed., pp. 819848). St. Louis: Mosby-Year Book Inc.
Rankin, E. A., & Mitchel, M. L. (2000). Creating a pain management educational module for hospice nurses: Integrating the New JCAHO Standards and the AHCPR pain management guidelines. Journal of Hospice and Palliative Nursing, 2(3), 91100. Regan, J. M., & Peng, P. (2000). Neurophysiology of cancer pain. Cancer Control, 7(2), 111119. Wall, P. D., & Melzack R. (1994). Textbook of pain (3rd ed., pp. 523540). London, England: Longman Group U.K. Limited.
Vous aimerez peut-être aussi
- Fast Facts: Perioperative Pain: Effective management has numerous benefitsD'EverandFast Facts: Perioperative Pain: Effective management has numerous benefitsPas encore d'évaluation
- نسخة Lecture - PAIN Assessment & ManagementDocument52 pagesنسخة Lecture - PAIN Assessment & Managementjsoal100% (1)
- Pain Management for Clinicians: A Guide to Assessment and TreatmentD'EverandPain Management for Clinicians: A Guide to Assessment and TreatmentCarl Edward NoePas encore d'évaluation
- Veterinary Pain ManagementDocument8 pagesVeterinary Pain ManagementMenaPas encore d'évaluation
- Assessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsD'EverandAssessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsPas encore d'évaluation
- The PainDocument19 pagesThe PainKevin Torres PontePas encore d'évaluation
- Pain Management PalliativeDocument25 pagesPain Management PalliativeAnnisaaShofiyullah ShofiyunnisaaPas encore d'évaluation
- Unit-3 - Pain ManagementDocument100 pagesUnit-3 - Pain ManagementyaraPas encore d'évaluation
- Journal On PainDocument5 pagesJournal On PainGeevine CansinoPas encore d'évaluation
- Individual rehabilitation program using traditional medicine methods for medical rehabilitation of patients with chronic pain syndromeDocument22 pagesIndividual rehabilitation program using traditional medicine methods for medical rehabilitation of patients with chronic pain syndromedevika FmgePas encore d'évaluation
- PAINDocument41 pagesPAINPrasenjit ChakrabortyPas encore d'évaluation
- Acute Pain Service Handbook: Pain Pathways, Transmission and ModulationDocument116 pagesAcute Pain Service Handbook: Pain Pathways, Transmission and ModulationdennyramdhanPas encore d'évaluation
- 3 +Pain+2018+PDF+1ppDocument33 pages3 +Pain+2018+PDF+1pphorace_linPas encore d'évaluation
- Pain Management For NursesDocument42 pagesPain Management For Nursesblacknurse100% (1)
- Competency Appraisal 2: Pain ManagementDocument96 pagesCompetency Appraisal 2: Pain ManagementLane Mae Magpatoc NoerrotPas encore d'évaluation
- Supplementary Material 7a Analgesia, Sedation and Neuromuscular BlockadeDocument10 pagesSupplementary Material 7a Analgesia, Sedation and Neuromuscular BlockadeJeremiah Andre Poissonier AyupanPas encore d'évaluation
- By Dr. Cuong Ngo-Minh Back To Basics April 14th 2010Document15 pagesBy Dr. Cuong Ngo-Minh Back To Basics April 14th 2010Wael WilsonPas encore d'évaluation
- Pain Management - 03-07 VersionDocument51 pagesPain Management - 03-07 VersionanreilegardePas encore d'évaluation
- Theroleofpain Classificationsystemsin Painmanagement: Patty Montgomery Orr,, Bettina Cobb Shank,, Amy Conner BlackDocument12 pagesTheroleofpain Classificationsystemsin Painmanagement: Patty Montgomery Orr,, Bettina Cobb Shank,, Amy Conner Blackneurologi standart4Pas encore d'évaluation
- Pain ManagementDocument20 pagesPain ManagementProsanjit MajumderPas encore d'évaluation
- Pain Management CHNDocument38 pagesPain Management CHNVaibhavi ShastriPas encore d'évaluation
- Manajemen Nyeri Pada Perawatan PaliatifDocument15 pagesManajemen Nyeri Pada Perawatan PaliatifYosi oktarinaPas encore d'évaluation
- Acute Pain Assessment and TreatmentDocument14 pagesAcute Pain Assessment and TreatmentEygenia PapadpoulouPas encore d'évaluation
- The Fifth Vital SignDocument7 pagesThe Fifth Vital SignMaribee Tagayun EspirituPas encore d'évaluation
- Lecture - 12 2013Document28 pagesLecture - 12 2013LucjaPas encore d'évaluation
- Assessment of Chronic PainDocument7 pagesAssessment of Chronic PainFranciscoGarciaPas encore d'évaluation
- CONCEPT OF PAIN: DEFINITIONS, THEORIES, AND RESPONSESDocument90 pagesCONCEPT OF PAIN: DEFINITIONS, THEORIES, AND RESPONSESQueenClerk VillartePas encore d'évaluation
- PAINDocument11 pagesPAINvavafo7699Pas encore d'évaluation
- Assessing and Managing Pain: A Guide for NursesDocument58 pagesAssessing and Managing Pain: A Guide for NursesErica GyeolsilPas encore d'évaluation
- 9.pain ManagementDocument24 pages9.pain ManagementhebaPas encore d'évaluation
- Pain (Assesment & Modulatin) : Presented By: Sakshi Nerle Guide: Dr. Sanket Mungikar Moderator: Dr. KapilDocument24 pagesPain (Assesment & Modulatin) : Presented By: Sakshi Nerle Guide: Dr. Sanket Mungikar Moderator: Dr. KapilTARVEEN DuraiPas encore d'évaluation
- Bio-Psycho-Social Aspects of PainDocument29 pagesBio-Psycho-Social Aspects of Painnugraha sultanPas encore d'évaluation
- Pain Management F05Document19 pagesPain Management F05Aneka DeanPas encore d'évaluation
- Chronic Pain: Structural and Functional Changes in Brain Structures and Associated Negative ADocument17 pagesChronic Pain: Structural and Functional Changes in Brain Structures and Associated Negative Avicente gaticaPas encore d'évaluation
- Physiology of Pain: 1. TransductionDocument16 pagesPhysiology of Pain: 1. Transductioncopy world100% (2)
- Effective Pain Management GuideDocument100 pagesEffective Pain Management GuideMatthew Lee Hon LamPas encore d'évaluation
- Chronic PainDocument12 pagesChronic PainlizPas encore d'évaluation
- Acupuncture and Pain: A Review of The Literature: Ladan Eshkevari, CRNA, MS, Dipl. AcDocument10 pagesAcupuncture and Pain: A Review of The Literature: Ladan Eshkevari, CRNA, MS, Dipl. AcRatrika SariPas encore d'évaluation
- Physiology of Pain: Guide To Pain Management in Low-Resource SettingsDocument6 pagesPhysiology of Pain: Guide To Pain Management in Low-Resource SettingsomboPas encore d'évaluation
- PainDocument20 pagesPainvinnu kalyanPas encore d'évaluation
- Pain Physiology Pathways Mechanisms ClassificationDocument71 pagesPain Physiology Pathways Mechanisms Classificationkeerthi_keshapagaPas encore d'évaluation
- Final - Pain ManagementDocument18 pagesFinal - Pain ManagementFatma Shnewra100% (1)
- AliliDocument3 pagesAliliSaf Tanggo DiampuanPas encore d'évaluation
- Pain AssessmentDocument12 pagesPain AssessmentFadhilah Asyifa DewantiPas encore d'évaluation
- PainDocument23 pagesPainAbo De7kaPas encore d'évaluation
- Pain ManagementDocument11 pagesPain ManagementLokeshwari KatrePas encore d'évaluation
- Nursing Pharmacology Inflammation Study GuideDocument11 pagesNursing Pharmacology Inflammation Study GuideChelsea Smith100% (1)
- Pain ManagementDocument49 pagesPain ManagementQasim ChacharPas encore d'évaluation
- Physiology & Pathophysiology of PainDocument31 pagesPhysiology & Pathophysiology of Painkuncupcupu1368Pas encore d'évaluation
- Acute Service Pain Handbook 2011Document116 pagesAcute Service Pain Handbook 2011Iskandar414Pas encore d'évaluation
- Understanding Pain Concepts and TreatmentDocument46 pagesUnderstanding Pain Concepts and TreatmentwokorowPas encore d'évaluation
- Pain AssessmentDocument11 pagesPain AssessmentJenjen Cortey100% (1)
- Clasificación Dolor OrofacialDocument8 pagesClasificación Dolor OrofacialCindy Bernal MPas encore d'évaluation
- Understanding PainDocument23 pagesUnderstanding Painnisha justinPas encore d'évaluation
- Chapter 9: Stress and Stress ManagementDocument6 pagesChapter 9: Stress and Stress ManagementjefrocPas encore d'évaluation
- Chronic pain assessment written assignmentDocument11 pagesChronic pain assessment written assignmentMonika SimpsonPas encore d'évaluation
- Pain ManuscriptDocument5 pagesPain ManuscriptGPaolo FauniPas encore d'évaluation
- POST-OP PAIN MGMTDocument7 pagesPOST-OP PAIN MGMTEstefaniSabrinaSandovalPas encore d'évaluation
- Mechanisms of Pain MUIRDocument11 pagesMechanisms of Pain MUIRLorena B-iPas encore d'évaluation
- Pain Physiology Chapter Explains Nociception and HyperalgesiaDocument20 pagesPain Physiology Chapter Explains Nociception and HyperalgesiaDiana TiganucPas encore d'évaluation
- Choice of SpouseDocument14 pagesChoice of SpouseracopPas encore d'évaluation
- SGD 4 Pad 2016Document1 pageSGD 4 Pad 2016racopPas encore d'évaluation
- Philippines Declaration of Principles and State Policies SummaryDocument29 pagesPhilippines Declaration of Principles and State Policies SummaryracopPas encore d'évaluation
- May Day EveDocument3 pagesMay Day EvemapletheanxiousPas encore d'évaluation
- Vol 371 Topic 03Document13 pagesVol 371 Topic 03racopPas encore d'évaluation
- BCGDocument2 pagesBCGracopPas encore d'évaluation
- Reye SyndromeDocument2 pagesReye SyndromeracopPas encore d'évaluation
- 9916748Document11 pages9916748racopPas encore d'évaluation
- Thrombosis PDFDocument5 pagesThrombosis PDFracopPas encore d'évaluation
- About Jure and The AEQ MethodDocument3 pagesAbout Jure and The AEQ MethodJure KoščakPas encore d'évaluation
- FK Conox Product Brochure 4ppa4 v6Document4 pagesFK Conox Product Brochure 4ppa4 v6Lucas ShotsPas encore d'évaluation
- Analgesia For Labor and Vaginal DeliveryDocument21 pagesAnalgesia For Labor and Vaginal DeliveryLouije MombzPas encore d'évaluation
- Acute Pain NCPDocument2 pagesAcute Pain NCPkrz05Pas encore d'évaluation
- 10 Reyna SallyDocument4 pages10 Reyna SallyRaja WahidPas encore d'évaluation
- Predicting Migraine Patient Response to Botox TreatmentDocument26 pagesPredicting Migraine Patient Response to Botox TreatmentfparralePas encore d'évaluation
- Blood Letting Therapy (Siravyadhana) in Acute Sciatica Pain (Gridhrasi)Document5 pagesBlood Letting Therapy (Siravyadhana) in Acute Sciatica Pain (Gridhrasi)YADU GOPANPas encore d'évaluation
- (Undefined Series For Scimag) - Libgen - LiDocument7 pages(Undefined Series For Scimag) - Libgen - LiNicholas LimPas encore d'évaluation
- Palliative Pain Management in The Er: UBC EM Palliative Medicine Day Lindsay Cohen July 27, 2016Document31 pagesPalliative Pain Management in The Er: UBC EM Palliative Medicine Day Lindsay Cohen July 27, 2016b BPas encore d'évaluation
- Alexanders Care of The Patient in Surgery 16th Edition Rothrock Test BankDocument11 pagesAlexanders Care of The Patient in Surgery 16th Edition Rothrock Test Banklilykeva56r100% (31)
- AbdomenDocument7 pagesAbdomenAbhishek DussaPas encore d'évaluation
- Giles Set CDocument45 pagesGiles Set CPrinting CoPas encore d'évaluation
- Acute Pain Nursing Care PlanDocument3 pagesAcute Pain Nursing Care PlanTipey Segismundo100% (1)
- Alien Transfusion Conditioning Into The Aether Copycat: ElixirDocument2 pagesAlien Transfusion Conditioning Into The Aether Copycat: ElixirLuis F PayanPas encore d'évaluation
- Care Plan #1 - June 2012Document4 pagesCare Plan #1 - June 2012Meghan Equality ShalvoyPas encore d'évaluation
- TSU Nursing Performance Evaluation ChecklistDocument7 pagesTSU Nursing Performance Evaluation ChecklistKatKat Bognot100% (2)
- Case Reflection 25321902Document8 pagesCase Reflection 25321902Santhi Swetha PudhotaPas encore d'évaluation
- Is There A Role For Transversus Abdominis in Lumbo-Pelvic Stability?Document13 pagesIs There A Role For Transversus Abdominis in Lumbo-Pelvic Stability?mientwegPas encore d'évaluation
- Critical thinking exercises for therapeutic communicationDocument2 pagesCritical thinking exercises for therapeutic communicationLuisz PalmaPas encore d'évaluation
- Pain Management and Unani MedicineDocument1 pagePain Management and Unani MedicineMSKCPas encore d'évaluation
- Chronic Fatigue Syndrome From Vagus Nerve InfectionDocument10 pagesChronic Fatigue Syndrome From Vagus Nerve InfectionLevente BalázsPas encore d'évaluation
- MPS Therapy Flyer April 10 2018Document8 pagesMPS Therapy Flyer April 10 2018Neptune ShellPas encore d'évaluation
- The Argument Essay 1Document7 pagesThe Argument Essay 1api-495880377Pas encore d'évaluation
- 300307814sherlin SapthicaDocument100 pages300307814sherlin SapthicaTitin PrihartiniPas encore d'évaluation
- Roh 4Document52 pagesRoh 4gajucoolkarni50% (6)
- Arthritis ReversedDocument132 pagesArthritis Reversedciprian72Pas encore d'évaluation
- Key English collocations documentDocument4 pagesKey English collocations documentNguyễn Ngọc Mỹ AnhPas encore d'évaluation
- Oet Writing Exercise AnswersDocument10 pagesOet Writing Exercise AnswersLia Angulo-Estrada95% (22)
- Defining A Bobath ClinicalDocument2 pagesDefining A Bobath ClinicalAlicia HernandezPas encore d'évaluation
- Virginia Workers' Compensation Claim Surgery Approval DisputeDocument10 pagesVirginia Workers' Compensation Claim Surgery Approval Disputedbircs777Pas encore d'évaluation
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (13)
- The Comfort of Crows: A Backyard YearD'EverandThe Comfort of Crows: A Backyard YearÉvaluation : 4.5 sur 5 étoiles4.5/5 (23)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsD'EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsÉvaluation : 3.5 sur 5 étoiles3.5/5 (3)
- Why We Die: The New Science of Aging and the Quest for ImmortalityD'EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 5 sur 5 étoiles5/5 (78)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeD'EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BePas encore d'évaluation
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsD'EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsÉvaluation : 5 sur 5 étoiles5/5 (1)
- Techniques Exercises And Tricks For Memory ImprovementD'EverandTechniques Exercises And Tricks For Memory ImprovementÉvaluation : 4.5 sur 5 étoiles4.5/5 (40)
- The Obesity Code: Unlocking the Secrets of Weight LossD'EverandThe Obesity Code: Unlocking the Secrets of Weight LossÉvaluation : 5 sur 5 étoiles5/5 (4)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisD'EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisÉvaluation : 4 sur 5 étoiles4/5 (1)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisD'EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisÉvaluation : 5 sur 5 étoiles5/5 (8)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsD'EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsÉvaluation : 4.5 sur 5 étoiles4.5/5 (169)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingD'EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (33)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsD'EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsPas encore d'évaluation
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingD'EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingÉvaluation : 5 sur 5 étoiles5/5 (5)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.D'EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Évaluation : 4.5 sur 5 étoiles4.5/5 (110)
- The Ultimate Guide To Memory Improvement TechniquesD'EverandThe Ultimate Guide To Memory Improvement TechniquesÉvaluation : 5 sur 5 étoiles5/5 (34)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaD'EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeD'EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeÉvaluation : 4.5 sur 5 étoiles4.5/5 (253)
- The Happiness Trap: How to Stop Struggling and Start LivingD'EverandThe Happiness Trap: How to Stop Struggling and Start LivingÉvaluation : 4 sur 5 étoiles4/5 (1)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsD'EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsPas encore d'évaluation
- Recovering from Emotionally Immature Parents: Practical Tools to Establish Boundaries and Reclaim Your Emotional AutonomyD'EverandRecovering from Emotionally Immature Parents: Practical Tools to Establish Boundaries and Reclaim Your Emotional AutonomyÉvaluation : 4.5 sur 5 étoiles4.5/5 (201)
- The Tennis Partner: A Doctor's Story of Friendship and LossD'EverandThe Tennis Partner: A Doctor's Story of Friendship and LossÉvaluation : 4.5 sur 5 étoiles4.5/5 (4)