Académique Documents
Professionnel Documents
Culture Documents
EPI Nursing Considerations
Transféré par
Bel AllenDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
EPI Nursing Considerations
Transféré par
Bel AllenDroits d'auteur :
Formats disponibles
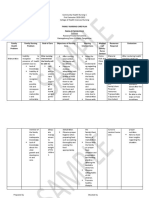
Nursing Considerations for Common Pediatric Immunizations
IMMUNIZATION TYPE Diphtheria and pertussis vaccines and tetanus toxiod (DTaP) Route: Intramuscular Dosage: 0.5 mL May give at same time as all other vaccines in a separate site. SIDE EFFECTS Common: Redness,pain,swelling, nodule at injection site; temperature up to 101F (38.3C); drowsiness,irritability,fussiness; anorexia within 2 days of injection.Increase in frequency and magnitude of local reactions with doses 4 and 5 (e.g.,entire limb swelling). Serious: Allergic reaction, anaphylaxis; shock, fever above 102F (38.8C); febrile seizure; persistent inconsolable crying; coma or permanent brain damage. Common: Swelling and tenderness, irritability, tiredness. Serious: Allergic reaction or anaphylaxis. NURSING CONSIDERATIONS Use same brand for all doses where feasible. Prior to immunization, ask about previous reaction to immunization. DTaP may coincide with or hasten the recognition of a seizure disorder. In children with a history of seizures with or without fever, give acetaminophen at the time of vaccine and then every 4 hours for 24 hours. Shake vaccine before withdrawing. Solution will be cloudy. If it contains clumps that cannot be resuspended, do not use. Inform parents of the chance of increased reaction to doses 4 and 5. Defer the vaccine if the child has a progressive neurologic problem until the child is stable. The series does not need to be restarted, regardless of when the previous dose was given. Prior to immunization, ask if child has an allergy to neomycin, streptomycin, or polymyxin B (whichever of these antibiotics the specific vaccine to be used contains). Clear, colorless suspension. Do not use if it contains particulate matter, becomes cloudy, or changes color. All doses must be separated by at least 4 weeks. The series does not need to be restarted, regardless of when the previous dose was given. Prior to immunization, ask if child has an allergy to neomycin or gelatin. Observe the child with an egg allergy for 90 minutes after injection. Inquire about immunosuppression. Instruct adolescent girls of childbearing age to avoid pregnancy for 3 months after immunization. Give tuberculosis test at same time as MMR or 46 weeks later. If MMR and Varivax are not given on the same day, space them at least 28 days apart. Reconstituted vaccine is a clear, yellow solution. Give entire contents of reconstituted vial even if more than 0.5 mL. As college students are at greater risk due to decreasing immunity, make sure they have received a second MMR dose. Prior to immunization, check status of mothers hepatitis B test and presence of other liver disease.Note: If mother has HbsAg+, vaccine must be given to infant within 12 hours of birth along with hepatitis B immune globulin at the same time in another site with a new needle and syringe. Shake vaccine before withdrawing. Solution will appear cloudy. Minimum spacing for children and teens is 4 weeks between doses 1 and 2, and 8 weeks between doses 2 and 3. The last dose in an infant series should not be given before 6 months of age. Vaccine brands can be interchanged for 3-dose series. The series does not need to be restarted, regardless of when the previous dose was given. (continued)
Poliovirus vaccine (IPV) Route: Subcutaneous or intramuscular, depending on vaccine used Dosage: 0.5 mL May give at same time as all other vaccines in a separate site. Measles, mumps, rubella (MMR) vaccine Route: Subcutaneous Dosage: 0.5 mL May give at same time as all other vaccines in a separate site.
Common: Elevated temperature 12 weeks after immunization; redness or pain at injection site; noncontagious rash; joint pain. Serious: Allergic reaction, febrile seizure; meningitis (usually mild); encephalopathy; thrombocytopenia purpura; rare cases of coma and permanent brain damage.
Hepatitis B (HB) vaccine Route: Intramuscular Dosage: Engerix-B: 10 mcg or Recombivax HB: 5 mcg May give at same time as all other vaccines in a separate site.
Common: Pain or redness at injection site; headache; photophobia; altered liver enzymes. Serious: Allergic reaction or anaphylaxis; fever.
Nursing Considerations for Common Pediatric Immunizations (continued)
IMMUNIZATION TYPE Haemophilus influenza type B (Hib) Route: Intramuscular Dosage: 0.5 mL May give at same time as all other vaccines in a separate site. SIDE EFFECTS Common: Pain, redness, or swelling at site. Serious: Allergic reaction of anaphylaxis (extremely rare); fever. NURSING CONSIDERATIONS Prior to immunizations, ask if child is immunosuppressed. Solution is clear and colorless. If the first dose is given between 7 and 11 months of age, 3 doses are needed. If the first dose is given at 1214 months of age, give a booster dose in 8 weeks. If the first dose is given when the child is older than 15 months or younger than 5 years, only one dose is needed. Second and third doses can be given 48 weeks after the first. Use the same vaccine preparation for all doses of the primary series if possible. The series does not need to be restarted, regardless of when the previous dose was given. Clear, colorless, or slightly opalescent liquid. In addition to infants, this vaccine is a priority for children ages 25 with sickle cell disease, asplenia, or HIV infection, or in those who are immunocompromised. The vaccine is also a priority for Native American and Native Alaskan children ages 25 because of their increased risk for pneumococcal disease. The series does not need to be restarted, regardless of when the previous dose was given. Prior to immunization, ask if child is immunodeficient, on immunosuppression treatment, or has an allergy to neomycin or gelatin. Determine if a family member is immunocompromised. Clear, colorless to pale yellow liquid when reconstituted. Give the entire contents of the vial even if more than 0.5 mL. Instruct adolescent girls of childbearing age to avoid pregnancy for 3 months after immunization.
Heptavalent pneumococcal conjugate vaccine (PCV) Route: Intramuscular Dosage: 0.5 mL
Common: Soreness, swelling, redness at injection site; mild to moderate fever; irritability, drowsiness, restless sleep, decreased appetite, vomiting and diarrhea, rash or hives. Severe: Allergic reaction or anaphylaxis. Common: Pain or redness at injection site; fever up to 102F (38.8C) in children. Less commonly, a mild vaccinerelated rash may occur during first month after the injection. Severe: Allergic reaction or anaphylaxis; thrombocytopenia; febrile seizure; central nervous system manifestations. Rare reports of anaphylaxis reaction.
Varicella virus vaccine Route: Subcutaneous Dosage: 0.5 mL
Hepatitis A Route: Intramuscular Dosage: 0.5 mL, 1 mL over 17 years for Vaqta, 1 mL over 18 years for Havrix May give at same time as all other vaccines in a separate site. Influenza Route: Intramuscular (all ages), intranasal (5 years and older) Dosage: 0.25 mL in infants 635 months, 0.5 mL beginning at 3 years May give at same time as all other vaccines in a separate site.
Shake well, slightly opaque white suspension. Can be given for postexposure prophylaxis against hepatitis A. Immune globulin and vaccine can be given at same time in different sites. Vaccine brands can be interchanged.
Common after injection: May have soreness or swelling at injection site, fever, aches. Life-threatening allergic reactions are rare. Common after intranasal vaccine: Runny nose or nasal congestion, fever, headache or muscle aches, abdominal pain, and occasional vomiting.
Thawed intranasal vaccine is pale yellow, clear to slightly cloudy. Administered annually in autumn. Children with no history of influenza illness or vaccine need 2 doses 1 month apart. lntranasal dose is split (0.25 mL) with a dose divider clip. Administer in each nostril while child is sitting in an upright position.Insert the tip of the sprayer inside the nose and depress the plunger to spray. Children 8 years of age or younger who are receiving the influenza vaccine for the first time should get 2 doses separated by at least 4 weeks (injectable) and 6 weeks (intranasal). Must be reimmunized each year as immunity wanes.
Data from American Academy of Pediatrics. (2003). Red Book: Report of the Committee on Infectious Disease (26th ed.). Elk Grove Village, IL: Author; Immunization Action Coalition. (2004). Mosbys drug consult 2004. St. Louis: Mosby; Bindler, R.M., & L.B., Howry. (2005). Pediatric drug with nursing implications. Upper Saddle River, NJ: Prentice Hall.
Vous aimerez peut-être aussi
- Nursing Care Plan - HyperDocument4 pagesNursing Care Plan - HyperJennalyn Casapao100% (1)
- Drug Study: Pharmacology: Pharmacodynamics: TheDocument2 pagesDrug Study: Pharmacology: Pharmacodynamics: Theliza sianPas encore d'évaluation
- NCP For Caesarian Delivery (Breech Presentation)Document2 pagesNCP For Caesarian Delivery (Breech Presentation)Raymond BasiloniaPas encore d'évaluation
- Dengue Fever Discharge PlanDocument9 pagesDengue Fever Discharge PlanTrisha Faye OrtegaPas encore d'évaluation
- Nursing Care Plan: Cues Objectives Interventions Rationale EvaluationDocument1 pageNursing Care Plan: Cues Objectives Interventions Rationale EvaluationlaehaaaPas encore d'évaluation
- FNCPDocument4 pagesFNCPsenyorakathPas encore d'évaluation
- Book-Based: Pathophysiology of Allergic RhinitisDocument2 pagesBook-Based: Pathophysiology of Allergic RhinitisJeraldine Corpuz PascualPas encore d'évaluation
- Discharge PlanningDocument3 pagesDischarge PlanningAlex Marie100% (2)
- Hep B Vaccine Drug StudyDocument2 pagesHep B Vaccine Drug StudyFrian MariñasPas encore d'évaluation
- Pathophysiology of Erythroblastosis Fetalis - RH IsoimmunizationDocument1 pagePathophysiology of Erythroblastosis Fetalis - RH IsoimmunizationRalph Delos SantosPas encore d'évaluation
- Absence of Responsible Member and Financial ConstraintsDocument2 pagesAbsence of Responsible Member and Financial ConstraintsFavor ColaPas encore d'évaluation
- Drug StudyDocument2 pagesDrug StudyCarlo AniagPas encore d'évaluation
- HydroxyzineDocument3 pagesHydroxyzineapi-3797941100% (2)
- Peach and Green Organic Shapes Meditation Workshop Webinar Keynote PresentationDocument7 pagesPeach and Green Organic Shapes Meditation Workshop Webinar Keynote PresentationNicole Ivy GorimoPas encore d'évaluation
- Chief ComplaintDocument3 pagesChief ComplaintAngela TuantePas encore d'évaluation
- Nursery Drug Study 2 1Document22 pagesNursery Drug Study 2 1Wenalyn Grace Abella LlavanPas encore d'évaluation
- Cefaclor, Salbutamol, Paracetamol and NCPDocument13 pagesCefaclor, Salbutamol, Paracetamol and NCPAriane Rose Saria CedronPas encore d'évaluation
- Family Nursing Care Plan1Document2 pagesFamily Nursing Care Plan1Karlo ReyesPas encore d'évaluation
- MOriamin ForteDocument1 pageMOriamin Forteianecunar100% (3)
- A. Not My Job!: Ncmp109 Bioethics: Case StudyDocument2 pagesA. Not My Job!: Ncmp109 Bioethics: Case StudyAudrey Ann Acob100% (1)
- Macronutrients-Carbohydrates: NCM 105A Nutrition and Diet Therapy Laborator YDocument3 pagesMacronutrients-Carbohydrates: NCM 105A Nutrition and Diet Therapy Laborator YArriane Desepeda100% (1)
- Family Nursing Care Plan-MalnutritionDocument2 pagesFamily Nursing Care Plan-MalnutritionNovelyn PuaPas encore d'évaluation
- OB Nursing Care Plan Patient Tahbso CS RodriguezDocument2 pagesOB Nursing Care Plan Patient Tahbso CS RodriguezKaren ValdezPas encore d'évaluation
- Nursing Care Plan Assessment Diagnosis Planning Implementation Rationale EvaluationDocument1 pageNursing Care Plan Assessment Diagnosis Planning Implementation Rationale EvaluationMyrien BanaagPas encore d'évaluation
- FNCP Proper RevisedDocument2 pagesFNCP Proper RevisedKevinPas encore d'évaluation
- Drug Study SARAHDocument2 pagesDrug Study SARAHirene Joy DigaoPas encore d'évaluation
- Drug Study DemerolDocument2 pagesDrug Study DemerolKayelyn-Rose CombatePas encore d'évaluation
- Drug Study of Oral Polio VaccineDocument2 pagesDrug Study of Oral Polio VaccineDeanne Stephanie Hordista100% (1)
- Ob Case Study - BCG Drug StudyDocument1 pageOb Case Study - BCG Drug StudyAngelica Rose Villegas0% (1)
- NCP TEACHING PLAN (Postpartum)Document2 pagesNCP TEACHING PLAN (Postpartum)teuuuuPas encore d'évaluation
- Chapter 24: Nursing Care of A Family During A Surgical Intervention For BirthDocument22 pagesChapter 24: Nursing Care of A Family During A Surgical Intervention For BirthAlyssaGrandeMontimorPas encore d'évaluation
- Pathophysiology AGEDocument2 pagesPathophysiology AGEMareeze Hatta100% (1)
- NCPDocument2 pagesNCPKasandra Dawn Moquia BerisoPas encore d'évaluation
- Cognitive Perception Pattern of Nursing CareDocument9 pagesCognitive Perception Pattern of Nursing CareGloria Khan100% (4)
- NCPDocument3 pagesNCPChrisTine M. MoralesPas encore d'évaluation
- Pcap Pathophysiology PDFDocument3 pagesPcap Pathophysiology PDFMikaela RamosPas encore d'évaluation
- VIII. Discharge PlanDocument2 pagesVIII. Discharge PlanPia Therese CabaticPas encore d'évaluation
- DRUG STUDY RabiesDocument1 pageDRUG STUDY RabiesFranz RolfPas encore d'évaluation
- Nursing Care Plan: Cues Objectives Interventions Rationale EvaluationDocument2 pagesNursing Care Plan: Cues Objectives Interventions Rationale EvaluationAkiraMamoPas encore d'évaluation
- Drug StudyDocument8 pagesDrug StudyYaniiee DeFiestaPas encore d'évaluation
- Co AmoxiclavDocument2 pagesCo AmoxiclavkaijeiPas encore d'évaluation
- GI: Diarrhea/loose: Stools, Fulminant Hepatitis, Hepatic Dysfunction, JaundiceDocument3 pagesGI: Diarrhea/loose: Stools, Fulminant Hepatitis, Hepatic Dysfunction, JaundiceDaniela Claire FranciscoPas encore d'évaluation
- Careplan Sexual Dysfuntion DyspareuniaDocument12 pagesCareplan Sexual Dysfuntion DyspareuniaAxus War0% (1)
- Terramycin - Drug StudyDocument2 pagesTerramycin - Drug StudyBolasoc, HazelPas encore d'évaluation
- Case Analysis CHN2Document3 pagesCase Analysis CHN2Nicxx GamingPas encore d'évaluation
- XtendaDocument2 pagesXtendaAlexis CoronadoPas encore d'évaluation
- Chicken Pox N C P BY BHERU LALDocument2 pagesChicken Pox N C P BY BHERU LALBheru Lal100% (1)
- GENERIC NAME: Co-Amoxiclav (Amoxicillin & Clavulanic Acid) BRAND NAMES: Natravox, AddexDocument4 pagesGENERIC NAME: Co-Amoxiclav (Amoxicillin & Clavulanic Acid) BRAND NAMES: Natravox, AddexDRAPas encore d'évaluation
- Sheryl Ann B. Pedines Bsn-IvDocument2 pagesSheryl Ann B. Pedines Bsn-IvSheryl Ann Barit PedinesPas encore d'évaluation
- Family Nursing Care PlanDocument2 pagesFamily Nursing Care PlanWilliam Oz CiferPas encore d'évaluation
- NCP Acute Pain FURUNCOLOSISDocument2 pagesNCP Acute Pain FURUNCOLOSISMaria Imogen MilambilingPas encore d'évaluation
- OxacillinDocument2 pagesOxacillinSatinderSinghPas encore d'évaluation
- Introduction: Hepatitis A Maurice HillemanDocument19 pagesIntroduction: Hepatitis A Maurice Hillemanahmed solimanPas encore d'évaluation
- Expanded Program On Immunization and Reproductive Health DOH ProgramsDocument24 pagesExpanded Program On Immunization and Reproductive Health DOH ProgramsPrince Jhessie L. AbellaPas encore d'évaluation
- Vaccines NisDocument12 pagesVaccines NisHimanshu MehtaPas encore d'évaluation
- Expanded Immunization Report 1Document54 pagesExpanded Immunization Report 1RIK HAROLD GATPANDAN100% (1)
- Immunization Part 3Document12 pagesImmunization Part 3Marleen ShehadaPas encore d'évaluation
- Vaccination: Passive ImmunityDocument12 pagesVaccination: Passive ImmunityuouoPas encore d'évaluation
- Expanded Program On ImmunizationDocument12 pagesExpanded Program On ImmunizationRosechelle Baggao Siupan-Elarco100% (1)
- ImmunizationDocument60 pagesImmunizationleekabrams11Pas encore d'évaluation
- Vaccination Policy Letter of IntentDocument2 pagesVaccination Policy Letter of IntentTravis MealingPas encore d'évaluation
- Turtles Book English - Chapter 1Document83 pagesTurtles Book English - Chapter 1Britt WarePas encore d'évaluation
- Aspek Hukum Kekarantinaan Kesehatan Dan Perlindungan Konsumen Dalam Penanggulangan Pandemi Covid-19Document22 pagesAspek Hukum Kekarantinaan Kesehatan Dan Perlindungan Konsumen Dalam Penanggulangan Pandemi Covid-19Nikeu KusnantiniPas encore d'évaluation
- What's in A Vaccine and What Does It Do To Your Body?Document4 pagesWhat's in A Vaccine and What Does It Do To Your Body?Oscar Ciutat OróPas encore d'évaluation
- No Lie Can Live Forever - Mitchell AguilarDocument265 pagesNo Lie Can Live Forever - Mitchell AguilarNoliecanLiveforever100% (1)
- Ontario Immunization Schedule ENDocument1 pageOntario Immunization Schedule ENMing XiePas encore d'évaluation
- Regulasies 11 Junie 2020Document20 pagesRegulasies 11 Junie 2020Elvira WoodPas encore d'évaluation
- Childhood Immunization & Catch Up Immunization-2Document53 pagesChildhood Immunization & Catch Up Immunization-2Haters ExterminatorPas encore d'évaluation
- Final Requirement - Sustainable Development GoalsDocument3 pagesFinal Requirement - Sustainable Development GoalsLeyang SpeaksPas encore d'évaluation
- Manual of Antimicrobial Stewardship (1st Edition)Document49 pagesManual of Antimicrobial Stewardship (1st Edition)Socrates AbroadPas encore d'évaluation
- Submitted To DR Ritu Jindal Professor and Head of Dept Dept of Pedodontics and Preventive DentistryDocument43 pagesSubmitted To DR Ritu Jindal Professor and Head of Dept Dept of Pedodontics and Preventive Dentistrydr parveen bathlaPas encore d'évaluation
- A Special Interview With Dr. Natasha Campbell-Mcbride by Dr. MercolaDocument25 pagesA Special Interview With Dr. Natasha Campbell-Mcbride by Dr. Mercolaruth19774Pas encore d'évaluation
- Elimination of Measles From Bangladesh ProgressionDocument4 pagesElimination of Measles From Bangladesh ProgressionmamunpalashPas encore d'évaluation
- Annotated Bibliography On VaccinationsDocument4 pagesAnnotated Bibliography On VaccinationsRyan MarshPas encore d'évaluation
- Government of Pakistan Planning Commission Pc-1 Form Name of The Project Livestock and Access To Markets Project (LAMP)Document34 pagesGovernment of Pakistan Planning Commission Pc-1 Form Name of The Project Livestock and Access To Markets Project (LAMP)RizwanRashidPas encore d'évaluation
- Due For Submission On 5th of Following Month: Numbers Reported During The MonthDocument3 pagesDue For Submission On 5th of Following Month: Numbers Reported During The MonthPanthangi SrinivasPas encore d'évaluation
- Insert Hep B Engerix-BDocument16 pagesInsert Hep B Engerix-BshifanahmedPas encore d'évaluation
- 23943CROATIA UN FinalDocument109 pages23943CROATIA UN FinalrenkovikiPas encore d'évaluation
- Table 44-8 Nursing Assessment: Hepatitis Subjective Data Important Health InformationDocument7 pagesTable 44-8 Nursing Assessment: Hepatitis Subjective Data Important Health InformationAnggela kian puspaPas encore d'évaluation
- Final 2014Document414 pagesFinal 2014Bhavesh Bhakodiya0% (1)
- Dirty Vaccines: New Study Reveals Prevalence of ContaminantsDocument5 pagesDirty Vaccines: New Study Reveals Prevalence of Contaminantsrblais100% (1)
- Studi Kasus Bioetika Semester Gasal 2015-2016 PDFDocument8 pagesStudi Kasus Bioetika Semester Gasal 2015-2016 PDFShokhikhun NatiqPas encore d'évaluation
- Mock Examination For Erasmus Series Learners (EslDocument54 pagesMock Examination For Erasmus Series Learners (EslKumah Wisdom100% (5)
- News ItemDocument3 pagesNews ItemNovia 'opy' RakhmawatiPas encore d'évaluation
- MLS 422 Diagnostic MicrobiologyDocument50 pagesMLS 422 Diagnostic MicrobiologyMayowa OgunmolaPas encore d'évaluation
- Coronavirus - Oxford University To Resume Vaccine Trial After Pause - BBC NewsDocument7 pagesCoronavirus - Oxford University To Resume Vaccine Trial After Pause - BBC Newslockleong93Pas encore d'évaluation
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary DetailsNikhil shindePas encore d'évaluation
- Community Health Nursing Review NotesDocument12 pagesCommunity Health Nursing Review NotesISICLE GTPas encore d'évaluation
- Fiitjee: Talent Reward Exam - 2020Document46 pagesFiitjee: Talent Reward Exam - 2020abhinav100% (1)
- Iir 2013 14Document347 pagesIir 2013 14SHESH RAJPRABHAKARPas encore d'évaluation