Académique Documents
Professionnel Documents
Culture Documents
Quality and Patient Safety in Malaysian Healthcare
Transféré par
Eric HexumDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Quality and Patient Safety in Malaysian Healthcare
Transféré par
Eric HexumDroits d'auteur :
Formats disponibles
GOALS OF PRESENTATION
HEALTHCARE QUALITY AND PATIENT SAFETY: THE MALAYSIAN EXPERIENCE
1.To Know Malaysia and the healthcare System. 2.Why Quality and Safety 3.Approaches 3 Approaches to improve Quality and Patient Safety
BY Assoc.Prof.Dr.Kadar Marikar CEO,MSQH 5 Feb.2009
4.Foster comparative discussions of strategies for quality of care & safety
Malaysia
The country is made up of two regions, Peninsula Malaysia and East Malaysia (Borneo) across the South China Sea. The Peninsula Malaysia is divided into the 'east coast' and the 'west coast' by the Main Range in the middle. East Malaysia is geographically rugged, with a series of mountain ranges running through the interiors of both Sabah and Sarawak. The Crocker Range in Sabah is the site of Mt Kinabalu, the highest peak in South East Asia.
Peninsula Malaysia
East Malaysia (Borneo)
Population of over 26 million people. Multi-cultural and multi-racial population consists of Malays, Chinese, Indians and numerous natives. Ethnic Groups: 59% Malay and other indigenous indigenous, 32% Chinese and 9% Indian.
Malay is the official language but English is widely spoken, especially in business. Official religion is Islam, but its people are free to observe any religion of their choice. It is common to see temples, mosques and churches located in close proximity. Languages: Malay, English, Chinese, Tamil and other tribal languages. Religion: Muslim (primarily Malays), Buddhism (Chinese), Hindu (Indian), Christianity. (Indian) Christianity
Malaysia is generally warm throughout the year with temperatures ranging from 21 to 32 C in the lowlands. This can however be as low as 16 C in the hills and highlands. Annual rainfall is heavy at 2,500mm (100 inches). On a rainy day, thunder and lightning often accompany the heavy downpour which normally lasts for less than two hours. The humidity level is high at 80% throughout the year. Generally, Malaysia has two seasons. The dry season is from May to September and the rainy season is from November to March.
Malaysia has 12 states and 3 Federal Territories. The Capital City is Kuala Lumpur
MALAYSIAN HEALTH SECTOR:
MINISTRY OF HEALTH Inpatient care services -Total 138 hospitals -Primary -Secondary -Tertiary -Specialized services (Range of beds 40-2000)
Public Health Services Out-patient services: -Health Centre (10,000 centre) -Community Clinics (2,000 Clinics)
(Estimated every 5 kilometers radius -> 1CC)
Private Sectors -Private Hospitals: 328 (Range of beds 2-350 beds)
- Private Medical clinics: 6000 - Maternity Centres : - Hemodialysis centers : - Day care centers : - Nursing Homes:
-In remote areas: Flying Doctors Services.
(Especially for Sabah & Sarawak)
Preventive and Health Promotion services Medical Training Institutions-University Hospitals: 3 Ministry Of Defence: 3 + 1
Corporatised Hospital : National Heart Institute (IJN) 262 beds
VISION FOR HEALTH
Malaysia is to be a nation of healthy individuals, families and communities, through the health system that is equitable, affordable, efficient, technologically appropriate, environmentally adaptable and pp p , y p consumer friendly, with emphasis on quality, innovation, health promotion and respect for human dignity and which promote individual responsibility and community participation towards an enhanced quality of life.
Reasons for Supporting Quality of Care Agenda
REDUCE COSTS OF WASTES & ERRORS THROUGH CLINICAL QUALITY
Purchasers:
1) Control costs + assess quality = VALUE (cost-effectiveness for money spent) 2) Ensure access to care (government)
Suppliers / hospitals / doctors: S li h it l d t
1) Demonstrate quality and value to purchasers 2) Improve safety and reduce medical errors 3) Attract patients to maintain revenue
Patients / consumers:
1) Get high-quality, affordable care when needed 2) Maintain choice of doctors and hospitals
Stakeholders for Quality of Care
Purchasers: National & state governments Private health insurers Suppliers: Health Industry Drug and device companies Providers: Doctors and professional societies Hospitals, Clinics etc..
Why Measure Quality of Care?
Quality & effectiveness of health care essential to: Improve health Improve abnormal risk factors & prognosis (high blood pressure or high glucose) Lower morbidity Lower mortality
US National Library of Medicine
Patients / consumers
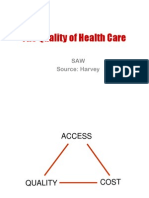
QUALITY FRAMEWORK
LEADERSHIP ORGANISATIONAL CULTURE & VALUES MEDICAL STAFF FOCUS ON PATIENT FOCUS ON PROCESS
OPERATIONAL MODEL
ACCESSIBILITY EFFICIENCY EFFECTIVENESS
SAFETY COMPETENCY COMPETENCY
STRUCTURE
(What are the things that you have)
PROCESS
(What do you do With these things)
OUTCOME
(What is the result of what you do with these things that you have)
QUALITY
PEOPLE FOCUS
APPROPRIATENESS
CONTINUOUS QUALITY IMPROVEMENT ENHANCED QUALITY OF LIFE
MSQH
ORGANISATIONAL STRUCTURE
QUALITY ASSURANCE PROGRAMME IN MINISTRY OF HEALTH
Launched in 1985 (with implementation of Patient Care Services QA Programme) QAP expanded to Public Health Services (1990) Pharmaceutical Services (1990) Dental Services (1992) Engineering Services (1992) Laboratory Services (1992) Training & Manpower Services (1996) Planning Division (1997)
1. National level 2. Programme level 3. State level 4. Hospital/Institutional level
Quality Improvement Activities
ACTS AND REGULATIONS
Hospital based
PRIVATE HEALTHCARE FACILITIES AND SERVICES ACT 1998 REGULATIONS 2006
QUALITY IMPROVEMENT ACTIVITIES IN THE MOH MALAYSIA
NATIONAL INDICATOR APPROACH (NIA) HOSPITAL SPECIFIC APPROACH (HSA)/ DISTRICT SPECIFIC APPROACH (DSA) MATERNAL MORTALITY REVIEW/ PERINATAL MORTALITY REVIEW PERIOPERATIVE MORTALITY REVIEW (POMR) MEDICAL AUDIT TOTAL QUALITY MANAGEMENT QUALITY CONTROL CIRLCE QUALITY CONTROL INFECTION CONTROL CLINICAL PRACTICE GUIDELINES (CPG) INCIDENT REPORTING CORPORATE CULTURE CLIENTS CHARTER INNOVATIONS RENAL REGISTRY Credentialing and Privileging Accreditation of Healthcare Facilities and Services
Strategic Plan For Quality
Late 1996 & 1997: Evaluation of 17 Quality Initiatives in MOH was carried out at National Level. Outcome of the evaluation was deliberated in the 1998 National Conference on Quality in Health Care held in March 1998.
Strategic Plan for Quality in Health
Implementation Plan of the Strategic Plan for Quality in Health 14 Manuals: Corporate Culture PKPA NIA MMR Incident Reporting CPG POMR Renal Registry Nosocomial Infection Innovations Quality Control Client Charter Quality Control Circle MS ISO 9000
The National Indicator Approach
Use of common indicators to assess the quality of care For each indicator a standard is set, against which the performance is compared If do not meet standards carry out investigations standards, to identify contributing factors or reason for shortfalls in quality Remedial measures are identified so as to overcome these shortfalls The cycle is then repeated
Report on a decade of NIA Performance by Programmes
These document have also been distributed for use by the Private Health Care providers - to assist them towards compliance of the Private Healthcare Facilities and Services Act 1998.
NATIONAL INDICATOR APPROACH
Patient Care Services Public Health Services Oral Health Pharmacy Laboratory y Engineering Services Human Resource & Training Planning & Development Division - 51 indicators - 13 indicators - 14 indicators - 6 indicators - 8 indicators - 2 indicators - 5 indicators - 3 indicators
THE HOSPITAL SPECIFIC APPROACH (HSA)/ DISTRICT SPECIFIC APPROACH (DSA) Concept: Local staff identify and solve local problems
Hospitals/Districts identify areas of shortfalls specific to each individual hospital/district Study the process of provision of care to detect weakness Identify remedial measures Implement solution to overcome weaknesses Impact evaluation by reassessing quality
Incident/Event Reporting
- is a system of reporting any unintended occurrences of certain processes or outcomes (quality related) which could have or did harm to the patient p ( ) - Concept (HSA) * local problems * local solutions - Principles * simple process * highlight good ideas * non punitive * immediate remedy * feedback
Incident/Event Reporting
INDICATORS - examples
Nosocomial infection
Adverse drug reactions Falls and accidents Greater than 24 hours waiting time for emergency surgery
HOSPITAL INFECTION CONTROL (HIC)
HOSPITAL INFECTION CONTROL (HIC)
* MOH focus on HIC in late 1980s * Factors contributing to HIC include: -b l below satisfactory standards of nursing care ti f t t d d f i - inadequate facilities (equipment & overcrowding) - misuse and abuse of Antibiotics - improper use of sterilization and disinfection procedures
* Outcome of Research Projects on HIC - Institutionalization of Nosocomial Infection Control Programme in all hospitals - An Antibiotic Policy - Disinfection & Sterilization policies
HOSPITAL INFECTION CONTROL (HIC)
* Publications produced:
- Principles & Practices in Hospital Sterilization and Disinfection ( (Slides on Infection Control in Malaysian Hospitals) y p ) -Disinfection and Sterilization Policy & Practice - Guidelines On The Use Of Antibiotics
PeriPeri-operative Mortality Review (POMR)
*Started in 1990 Aim: Aim: To systematically assess the quality of Anesthetic and Surgical services and quality of supporting services,with the ultimate aim of identifying Shortfalls and taking remedial measures. measures. All cases of peri-operative death during the periwhole hospital stay is being investigated * For the 6th cycle (from 1/1/98 onwards) the POMR committee will review periperi-operative deaths that occur in 5 targeted areas. areas.
PeriPeri-operative Mortality Review (POMR)
5 targeted areas Neurotrauma Obstetrics Colorectal surgery Polytrauma Pediatric Surgery
ACHIEVEMENTS
1. 2 yearly reports have been produced. The 3rd report has been published. 2. Developments of policies and guidelines. 3. Improvement in OT, ICU and HDU services. 4. Improvement in Training and Supervision. 5. Computerised OT Documentation System. 6. Provide inputs for future development of Surgical, Anesthetic and Trauma Services, facility development and human Resource planning for the 8th Malaysian plan.
* Anaesthetic management in these 5 areas will also be reviewed. The parallel reporting system will continue to monitor all peri-operative deaths perias a baseline review.
CLINICAL PRACTICE GUIDELINES (CPG)
* Since 1993, MOH has initiated the Medical Consensus Development Programme with the Academy of Medicine * In October 1996, both MOH & , Academy of Medicine Malaysia took another step forward in developing evidence-based evidenceClinical Practice Guidelines * Since November 1997: MOH, Academy of Medicine and UKM conducted yearly Systemic Review Workshop (Evidence Based)
CLINICAL PRACTICE GUIDELINES (CPG)
Clinical Practice Guidelines Systematically developed statements to assist practitioner and patients decision about appropriate health care for specific clinical circumstances
CLINICAL PRACTICE GUIDELINES (CPG) Why Clinical Practice Guidelines?
- as a tool to address the issue of unjustifiable variations in clinical practice for a clinical condition p - assists practitioner to make the right decision, one which is appropriate, effective & reasonably cost effective - attempt to make the best use of available resources to achieve the best possible outcome - as standard of Clinical Practice
Examples of Consensus & Clinical Practice Guidelines available Prophylaxis of Venous Thrombo-embolism Management of Chronic Obstructive Airway Disease Management of Dengue and Dengue Hemorrhagic Fever in the Pediatric Population Management of Idiopathic Nephrotic Syndrome in Childhood Screening for Hepatocellular Carcinoma
MEDICAL STAFF CREDENTIALLING
HEALTH TECHNOLOGY ASSESSMENTS (HTA)
Unit set up in 1995 Is the systematic evaluation of the properties & the effects of Health Technology gy Focus is on * safety * efficacy/effectiveness * feasibility
Process of ensuring those who provide health care services are fully competent to do so * Right person for the right job * If providers not skilled enough ability to achieve Quality Outcomes will be questionable * Life time qualifications may no longer be valid
HEALTH TECHNOLOGY ASSESSMENTS (HTA)
WORLD ALLIANCE FOR PATIENT SAFETY Launched by WHO in October 2004 in response to World Health Assembly Resolution 2002 urging WHO and member states to pay the closest possible attention to Patient Safety.
Among topics studied: Stereo tactic Radio-Surgery Radio Spinal Cord Stimulation Electromagnetic Prostatectomy Routine Pre-operative Investigation Pre Electronic Fetal Monitoring
PATIENT SAFETY COUNCIL MALAYSIA (PSCoM)
Formed in Feb.2003 Committed to WHO World Alliance for Patient Safety strategies and action plans. MSQH i a member of th PSC M . is b f the PSCoM Strategies and action plans developed by PSCoM is adopted and given emphasis in the MSQH Hospital Accreditation Standards and Compliance assessment .
Goals of Patient Safety Programs
Create the safest possible environment for patients: Reinforce patient safety as top priority & p y pp y
create culture of safety
Measure & evaluate patient safety Change processes identified as unsafe Adopt technology that enhances safety
Patient safety
Patient safety is an outcome of safe health care process. While patient safety is the ultimate goal, it is a safer health care environment in the course of the process of patient care which ultimately determines safety. Safety is one dimension of the broader construct of culture culture, which includes aspects of organisational and clinical culture e,g related to specialities and professions. Communication is vital to patient safety in many ways: thus supporting mutual understanding across cultures is essential in the general development of patient safety.
HOSPITAL ACCREDITATION PROGRAMME
- started in late 1995 with the 1st National Workshop on Accreditation of hospitals - Assistance - WHO Consultant - is a process in which quality of health care services in a particular hospital is compared against established professionally accepted standards - voluntary programme conducted by a nonnongovernmental organisation
Memorandum of Understanding
1st October 1999
MOH MMA
HOSPITAL ACCREDITATION PROGRAMME Objectives
establishes standards of services among health care providers ensure quality of healthcare throughout the country enhance organization and management of healthcare institutions achieve optimum results from available resources increase accountability to customers and stakeholders
PARTNERSHIP & CONSENSUS
MSQH
The Malaysian M l i Healthcare Accreditation Program
COLLABORATION & SUPPORT
APHM
Active Participation of the Public, Private Sectors & Professional Organisations
HOW DO SYSTEMS OF CARE IMPEDE QUALITY & SAFETY?
Systems fragmented and often designed to serve needs of providers, not patients System deficits affect all providers and patients Patients fall through the cracks in complex systems of care Several small problems in multi-step processes can trigger severe adverse events Problems arise even when providers well intentioned
Key Challenge
The biggest challenge is to get people in hospitals- physicians, pharmacists, nurses, and administrators administrators- to recognize that errors are systems problems and not people problems.
Lucian Leape, MD Harvard School of Public Health
CULTURE OF SAFETY
Unreported errors cannot be investigated First, need to create a culture of safety, similar to the aviation industry
Even highly trained people make mistakes Reduce fear of reporting Move beyond blaming & punishing, toward improving the system
CONCLUSIONS & IMPLICATIONS
Many quality & safety tools now available to health policy-makers & health-care leaders:
Information technology Evidence-based quality standards Performance reports Financial incentives Focus on leadership, teamwork & coordination of care
Shift focus from blaming people to improving system
DO IT RIGHT FIRST TIME, ANYTIME
INCREASING PRODUCTIVITY
THANK YOU FOR YOUR ATTENTION
www.msqh.com.my msqh@msqh.com.my
REDUCE COSTS OF WASTES, ERRORS & REWORK THROUGH ENHANCING CLINICAL QUALITY
Vous aimerez peut-être aussi
- Indian Healthcare SectorDocument15 pagesIndian Healthcare SectorabhayPas encore d'évaluation
- 05 International Disc Models TaiwanDocument60 pages05 International Disc Models TaiwanFitra MuhammadPas encore d'évaluation
- Malaysian Healthcare Quality Improvement: Global Standards with Local FocusDocument25 pagesMalaysian Healthcare Quality Improvement: Global Standards with Local FocusAbdul Ghaffar Mohd NoorPas encore d'évaluation
- Services MKTGDocument14 pagesServices MKTGAnusha SatyanarayanPas encore d'évaluation
- Service Sector Management Health Care SectorDocument85 pagesService Sector Management Health Care SectorshuwePas encore d'évaluation
- Woundcare Just StartedDocument40 pagesWoundcare Just StartedMaizatul Akmar IbrahimPas encore d'évaluation
- CLASS 1 - Image - Roles Revised June 260Document48 pagesCLASS 1 - Image - Roles Revised June 260Marie-Lynne L'orPas encore d'évaluation
- Christine Cook CNC Performance Indicators and Role of the ICPDocument37 pagesChristine Cook CNC Performance Indicators and Role of the ICPdyah ayu shinta lesmanawatiPas encore d'évaluation
- MOH CDC Draft Advert July 2023 2Document7 pagesMOH CDC Draft Advert July 2023 2KevinPas encore d'évaluation
- Health Programs in India - RNTCPDocument28 pagesHealth Programs in India - RNTCPAkash Mittal100% (1)
- Role of Diagnostic Centres in Achieving Universal Healthcare Coverage (UHC) - (Hony) Brig. Dr. Arvind LalDocument38 pagesRole of Diagnostic Centres in Achieving Universal Healthcare Coverage (UHC) - (Hony) Brig. Dr. Arvind LalIndia Health ProgressPas encore d'évaluation
- NHP 2Document42 pagesNHP 2A J FathimaPas encore d'évaluation
- Service Sector Management Health Care SectorDocument52 pagesService Sector Management Health Care SectorshuwePas encore d'évaluation
- The Quality of Health Care: SAW Source: HarveyDocument43 pagesThe Quality of Health Care: SAW Source: HarveyMardatillah WiranataPas encore d'évaluation
- Department of Health: History, Policy, Budget, Programs For HealthDocument57 pagesDepartment of Health: History, Policy, Budget, Programs For HealthAngelica Cassandra VillenaPas encore d'évaluation
- Malaria Situation in PakistanDocument31 pagesMalaria Situation in PakistanSalman ArifPas encore d'évaluation
- Virtualeli Phcelements 111103214304 Phpapp01Document70 pagesVirtualeli Phcelements 111103214304 Phpapp01JL CalvinPas encore d'évaluation
- I. General Primary Health Care Facility Design Information: Research RequirementsDocument24 pagesI. General Primary Health Care Facility Design Information: Research RequirementsJoyce LapuzPas encore d'évaluation
- HealthDocument24 pagesHealthqwerty123Pas encore d'évaluation
- A Case Study On Emerging Services of Trauma Centre of KGMUDocument6 pagesA Case Study On Emerging Services of Trauma Centre of KGMUanashussainPas encore d'évaluation
- TPH Quality PolicyDocument8 pagesTPH Quality PolicyAl Sah HimPas encore d'évaluation
- IPHS Dist Hosp 201 To 300 Bed StandardsDocument158 pagesIPHS Dist Hosp 201 To 300 Bed StandardsHarshit YadavPas encore d'évaluation
- Nursing Informatics: Ms. Ma. Joya Jimenea Genzola, RNDocument39 pagesNursing Informatics: Ms. Ma. Joya Jimenea Genzola, RNJoyaGenzolaPas encore d'évaluation
- Health Care in NepalDocument24 pagesHealth Care in Nepalthcp8yf4btPas encore d'évaluation
- International Patient Safety GoalsDocument27 pagesInternational Patient Safety GoalsForhadPas encore d'évaluation
- Patient Safety Friendly Hospital InitiativeDocument46 pagesPatient Safety Friendly Hospital Initiativehum JavedPas encore d'évaluation
- Revised National Tuberculosis Control Programme in IndiaDocument25 pagesRevised National Tuberculosis Control Programme in IndiaSrilekha MaruthaiyanPas encore d'évaluation
- The Heath Care Delivery SystemDocument17 pagesThe Heath Care Delivery SystemAngelou RosalesPas encore d'évaluation
- Iphs PHC CHCDocument22 pagesIphs PHC CHCsurabhisprPas encore d'évaluation
- Transferring Pharmaceutical Services to Improve AccessDocument75 pagesTransferring Pharmaceutical Services to Improve Accesssunny1964Pas encore d'évaluation
- Infusion Therapy TrainingDocument19 pagesInfusion Therapy Trainingjeremie cruz100% (1)
- Clinical Governance in The UK NHSDocument4 pagesClinical Governance in The UK NHSchiefsanjivPas encore d'évaluation
- Nursing care process in patients with chronic obstructive pulmonary diseaseD'EverandNursing care process in patients with chronic obstructive pulmonary diseasePas encore d'évaluation
- Introduction To Medical TechnologyDocument141 pagesIntroduction To Medical TechnologyNilo Golosino IIIPas encore d'évaluation
- Manajemen-Performa Family Practice: Yudhi Wibowo, MDDocument80 pagesManajemen-Performa Family Practice: Yudhi Wibowo, MDfitraniaputriPas encore d'évaluation
- MODULE 3 STUDENT National Patient Safety Goals 2013Document15 pagesMODULE 3 STUDENT National Patient Safety Goals 2013Dewi Ratna Sari100% (1)
- NSW Health (1) - Infection Control PolicyDocument56 pagesNSW Health (1) - Infection Control Policyhanumana_dasaPas encore d'évaluation
- 2 From Volume To ValueDocument20 pages2 From Volume To ValueAR J LopezPas encore d'évaluation
- Unit 5.5 - JCIDocument38 pagesUnit 5.5 - JCILakshmi Sowjanya AkurathiPas encore d'évaluation
- IDSPDocument56 pagesIDSPitsdheeraj2002Pas encore d'évaluation
- Lecture 2 Hospital Supply Chain MnagementDocument50 pagesLecture 2 Hospital Supply Chain MnagementSnehasish GhoshPas encore d'évaluation
- Using ISO 9001 in Healthcare: Applications for Quality Systems, Performance Improvement, Clinical Integration, and AccreditationD'EverandUsing ISO 9001 in Healthcare: Applications for Quality Systems, Performance Improvement, Clinical Integration, and AccreditationPas encore d'évaluation
- CommunityOrgnzng SlidesDocument85 pagesCommunityOrgnzng SlidesKhatlen BagaresPas encore d'évaluation
- The National Unified Health Research Agenda (NUHRA) and The Regional Unified Health Research Agenda (Ruhra)Document35 pagesThe National Unified Health Research Agenda (NUHRA) and The Regional Unified Health Research Agenda (Ruhra)Ella B. CollantesPas encore d'évaluation
- Indian Public Health Standards For PHC: SimranDocument32 pagesIndian Public Health Standards For PHC: Simrankours1072Pas encore d'évaluation
- Problems in Health Care Delivery - Shimla.18.5.2010Document72 pagesProblems in Health Care Delivery - Shimla.18.5.2010National Child Health Resource Centre (NCHRC)Pas encore d'évaluation
- Healthcare SystemDocument25 pagesHealthcare SystemNurul AzminahPas encore d'évaluation
- K.A.P Study On Frontline Health WorkersDocument42 pagesK.A.P Study On Frontline Health WorkersAmit KankarwalPas encore d'évaluation
- KizerDocument68 pagesKizeramroel acehPas encore d'évaluation
- Role & Importance of Medical Records: Mahboob Ali Khan MHA, CPHQ Consultant HealthcareDocument60 pagesRole & Importance of Medical Records: Mahboob Ali Khan MHA, CPHQ Consultant HealthcareDr. Asma QureshiPas encore d'évaluation
- Ethiopian Hospital Services Trasformation Guidelines (Ehstg)Document112 pagesEthiopian Hospital Services Trasformation Guidelines (Ehstg)EzanaPas encore d'évaluation
- Clinical Process ImprovementDocument104 pagesClinical Process Improvementamarneh1969100% (1)
- Kausar-Pres 2 Begum CMDocument51 pagesKausar-Pres 2 Begum CMuzair05mehranPas encore d'évaluation
- Indonesia:: Country Status Mercury-Free Health CareDocument14 pagesIndonesia:: Country Status Mercury-Free Health CareHealth Care Without Harm - AsiaPas encore d'évaluation
- JointcommissionDocument27 pagesJointcommissionapi-245672784Pas encore d'évaluation
- Hospital and Organisation of HospitalDocument39 pagesHospital and Organisation of Hospitalpranal patil (Pranal)Pas encore d'évaluation
- CDS Clinical Decision Support SystemsDocument94 pagesCDS Clinical Decision Support SystemsgopiPas encore d'évaluation
- Combine Majpr TopicsDocument86 pagesCombine Majpr TopicsDr. Pooja DubeyPas encore d'évaluation
- Normes Ethique OoasDocument117 pagesNormes Ethique OoasakowemagnificatPas encore d'évaluation
- Therapy Outcome Measures for Rehabilitation Professionals: Speech and Language Therapy, Physiotherapy, Occupational TherapyD'EverandTherapy Outcome Measures for Rehabilitation Professionals: Speech and Language Therapy, Physiotherapy, Occupational TherapyPas encore d'évaluation
- 1624 - Corporate Transfer PolicyDocument16 pages1624 - Corporate Transfer PolicySyamsul ArifinPas encore d'évaluation
- Healthcare Supply Chain Research AgendaDocument6 pagesHealthcare Supply Chain Research AgendaAbdul WahabPas encore d'évaluation
- Alien TechnologyDocument11 pagesAlien TechnologySharvari TaklikarPas encore d'évaluation
- Using Data for Continuous Quality ImprovementDocument52 pagesUsing Data for Continuous Quality ImprovementasperijonPas encore d'évaluation
- Is Modified Brief Assertiveness Training For Nurses Effective? A Single-Group Study With Long - Term Follow - UpDocument7 pagesIs Modified Brief Assertiveness Training For Nurses Effective? A Single-Group Study With Long - Term Follow - UpWalled لي المعلوماتPas encore d'évaluation
- Employee Engagement and Its Relation To Hospital Performance in A Tertiary Care Teaching HospitalDocument9 pagesEmployee Engagement and Its Relation To Hospital Performance in A Tertiary Care Teaching Hospitalkanthi056Pas encore d'évaluation
- Bridging The Digital Divide in Health Care The Role of HIT in Addressing Racial and Ethnic DisparitiesDocument9 pagesBridging The Digital Divide in Health Care The Role of HIT in Addressing Racial and Ethnic DisparitiesArjun YadavPas encore d'évaluation
- Champion Patient SafetyDocument27 pagesChampion Patient Safetydesna100% (1)
- Baxter Q3 2017 Earnings Presentation (Final)Document21 pagesBaxter Q3 2017 Earnings Presentation (Final)medtechyPas encore d'évaluation
- Gazette July 2011Document16 pagesGazette July 2011St George's Healthcare NHS TrustPas encore d'évaluation
- Medical prescription components and typesDocument8 pagesMedical prescription components and typesAdelia Desti Endah SariPas encore d'évaluation
- Medical Malpractice Thesis StatementDocument6 pagesMedical Malpractice Thesis Statementcrystalwilliamscleveland100% (2)
- HCA/HealthONE's North Suburban Medical Center Achieves Healthgrades 2020 Patient Safety Excellence Award (TM)Document3 pagesHCA/HealthONE's North Suburban Medical Center Achieves Healthgrades 2020 Patient Safety Excellence Award (TM)PR.comPas encore d'évaluation
- RoilsDocument3 pagesRoilsapi-530935128Pas encore d'évaluation
- The Checklist - A Tool For Error Management and Performance ImprovementDocument5 pagesThe Checklist - A Tool For Error Management and Performance ImprovementGustavo Catalan RuzaPas encore d'évaluation
- Experienced Healthcare AssistantDocument2 pagesExperienced Healthcare Assistantbroken bunny 191Pas encore d'évaluation
- Ethical Leadership Fostering An Ethical Environment and Culture 20070808Document60 pagesEthical Leadership Fostering An Ethical Environment and Culture 20070808Maureen O'BrienPas encore d'évaluation
- EngDocument64 pagesEngmellysawitri9Pas encore d'évaluation
- Dermatology - St3: Entry CriteriaDocument7 pagesDermatology - St3: Entry CriteriaAndrea Menares0% (1)
- 122 1271 2 PBDocument122 pages122 1271 2 PBwendy vega100% (1)
- Enhancing Patient Safety by Preventing Medication ErrorsDocument7 pagesEnhancing Patient Safety by Preventing Medication ErrorsEsteban García EcheverryPas encore d'évaluation
- AORN Retained ItemsDocument15 pagesAORN Retained ItemsBingDelaCruzPas encore d'évaluation
- Knowledge of Blood Transfusion Practice Among NursesDocument37 pagesKnowledge of Blood Transfusion Practice Among NursesCallumPas encore d'évaluation
- Beacon HandbookDocument30 pagesBeacon HandbookPaolo VegaPas encore d'évaluation
- Didier PittetDocument67 pagesDidier PittetĐurđica IkićPas encore d'évaluation
- PrometricsDocument440 pagesPrometricsRomuel Villanueva Almeyda100% (3)
- 1 Acendio2013 OkeDocument417 pages1 Acendio2013 OkeridhoganPas encore d'évaluation
- 07 NadderDocument6 pages07 NaddervioletirisesPas encore d'évaluation
- Improving Patient SafetyDocument183 pagesImproving Patient SafetyakkalnurPas encore d'évaluation
- CarlosVillar MSC ThesisDocument120 pagesCarlosVillar MSC ThesisDivyaDeepthi18Pas encore d'évaluation