Académique Documents
Professionnel Documents
Culture Documents
Prom
Transféré par
Mariquita Buenafe0 évaluation0% ont trouvé ce document utile (0 vote)
32 vues14 pagesPremature RUPTURE OF MEMBRANES (PROM) occurs when the sacs containing the developing baby (fetus) and the amniotic fluid bursts or develops a hole prior to the start of labor. A normal pregnancy lasts an average of 40 weeks. At the end of 40 weeks, labor usually begins.
Description originale:
Titre original
Prom (1)
Copyright
© Attribution Non-Commercial (BY-NC)
Formats disponibles
DOCX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentPremature RUPTURE OF MEMBRANES (PROM) occurs when the sacs containing the developing baby (fetus) and the amniotic fluid bursts or develops a hole prior to the start of labor. A normal pregnancy lasts an average of 40 weeks. At the end of 40 weeks, labor usually begins.
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
32 vues14 pagesProm
Transféré par
Mariquita BuenafePremature RUPTURE OF MEMBRANES (PROM) occurs when the sacs containing the developing baby (fetus) and the amniotic fluid bursts or develops a hole prior to the start of labor. A normal pregnancy lasts an average of 40 weeks. At the end of 40 weeks, labor usually begins.
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 14
Systems Plus College Foundation
Balibago, Angeles City
CoIIege of Nursing
In PartiaI FuIfiIIment of the Requirement in NCM 102
ReIated Learning Experience
CASE REPORT
PREMATURE RUPTURE OF
MEMBRANES
Submitted To:
Ms. Junefaith EIese Cordero Neo, RM, RN, MSN
Submitted By Group 1:
Buenafe, Ma.Cresencia S.
Layag, Mark Olie B.
Mendoza, Lyka Marie
Raton, Russel James V.
PREMATURE RUPTURE OF MEMBRANES (PROM)
DEFINITION
Premature rupture of membranes (PROM) is an
event that occurs during pregnancy when the
sacs containing the developing baby (fetus) and
the amniotic fluid bursts or develops a hole prior
to the start of labor.
During pregnancy, the unborn baby (fetus) is surrounded and cushioned by a liquid
called amniotic fluid. This fluid, along with the fetus and the placenta, is enclosed within
a sac called the amniotic membrane. The amniotic fluid is important for several reasons.
t cushions and protects the fetus, allowing the fetus to move freely. The amniotic fluid
also allows the umbilical cord to float, preventing it from being compressed and cutting
off the fetus's supply of oxygen and nutrients. The amniotic membrane contains the
amniotic fluid and protects the fetal environment from the outside world. This barrier
protects the fetus from organisms (like bacteria or viruses) that could travel up the
vagina and potentially cause infection.
Although the fetus is almost always mature at between 36-40 weeks and can be born
without complication, a normal pregnancy lasts an average of 40 weeks. At the end of
40 weeks, the pregnancy is referred to as being "term. At term, labor usually begins.
During labor, the muscles of the uterus contract repeatedly. This allows the cervix to
begin to grow thinner (called effacement) and more open (dilatation). Eventually, the
cervix will become completely effaced and dilated. n the most common sequence of
events (about 90% of all deliveries), the amniotic membrane breaks (ruptures) around
this time. The baby then leaves the uterus and enters the birth canal. Ultimately, the
baby will be delivered out of the mother's vagina. n the 30 minutes after the birth of the
baby, the placenta should separate from the wall of the uterus and be delivered out of
the vagina.
Sometimes the membranes burst before the start of labor, and this is called premature
rupture of membranes (PROM). There are two types of PROM. One occurs at a point in
pregnancy before normal labor and delivery should take place. This is called preterm
PROM. The other type of PROM occurs at 36-40 weeks of pregnancy.
PROM occurs in about 10% of all pregnancies. Only about 20% of these cases are
preterm PROM. Preterm PROM is responsible for about 34% of all premature births.
CAUSES
The causes of PROM have not been clearly identified. Some risk factors include
smoking, multiple pregnancies (twins, triplets, etc.), and excess amniotic fluid
(polyhydramnios). Certain procedures carry an increased risk of PROM, including
amniocentesis (a diagnostic test involving extraction and examination of amniotic fluid)
and cervical cerclage (a procedure in which the uterus is sewn shut to avoid premature
labor). A condition called placental abruption is also associated with PROM, although it
is not known which condition occurs first. n some cases of preterm PROM, it is believed
that bacterial infection of the amniotic membrane causes it to weaken and then break.
However, most cases of PROM and infection occur in the opposite order, with PROM
occurring first followed by an infection.
PATHOPHYSIOLOGY
Numerous risk factors are associated with preterm PROM. Black patients are at
increased risk of preterm PROM compared with white patients. Other patients at higher
risk include those who have lower socioeconomic status, are smokers, have a history of
sexually transmitted infections, have had a previous preterm delivery, have vaginal
bleeding, or have uterine distension (e.g., polyhydramnios, multifetal pregnancy).
Procedures that may result in preterm PROM include cerclage and amniocentesis.
There appears to be no single etiology of preterm PROM. Choriodecidual infection or
inflammation may cause preterm PROM. A decrease in the collagen content of the
membranes has been suggested to predispose patients to preterm PROM. t is likely
that multiple factors predispose certain patients to preterm PROM.
CLINICAL MANIFESTATION (Signs and Symptoms)
The main symptom of PROM is fluid leaking from the vagina. t may be a sudden, large
gush of fluid, or it may be a slow, constant trickle of fluid. The complications that may
follow PROM include premature labor and delivery of the fetus, infections of the mother
and/or the fetus, and compression of the umbilical cord (leading to oxygen deprivation in
the fetus).
Labor almost always follows PROM, although the delay between PROM and the onset
of labor varies. When PROM occurs at term, labor almost always begins within 24
hours. Earlier in pregnancy, labor can be delayed up to a week or more after PROM.
The chance of infection increases as the time between PROM and labor increases.
While this may cause doctors to encourage labor in the patient who has reached term,
the risk of complications in a premature infant may cause doctors to try delaying labor
and delivery in the case of preterm PROM.
The types of infections that can complicate PROM include amnionitis and endometritis.
Amnionitis is an infection of the amniotic membrane. Endometritis is an infection of the
innermost lining of the uterus. Amnionitis occurs in 0.5-1% of all pregnancies. n the
case of PROM at term, amnionitis complicates about 3-15% of pregnancies. About 15-
23% of all cases of preterm PROM will be complicated by amnionitis. The presence of
amnionitis puts the fetus at great risk of developing an overwhelming infection (sepsis)
circulating throughout its bloodstream. Preterm babies are the most susceptible to this
life-threatening infection. One type of bacteria responsible for overwhelming infections
in newborn babies is called group B streptococci.
DIAGNOSTIC TEST
Depending on the amount of amniotic fluid leaking from the vagina, diagnosing PROM
may be easy. Some doctors note that amniotic fluid has a very characteristic musty
smell. A pelvic exam using a sterile medical instrument (speculum) may reveal a trickle
of amniotic fluid leaving the cervix, or a pool of amniotic fluid collected behind the cervix.
One of two easy tests can be performed to confirm that the liquid is amniotic fluid. A
drop of the fluid can be placed on nitrazine paper. Nitrazine paper is made so that it
turns from yellowish green to dark blue when it comes in contact with amniotic fluid.
Another test involves smearing a little of the fluid on a slide, allowing it to dry, and then
viewing it under a microscope. When viewed under the microscope, dried amniotic fluid
will be easy to identify because it will look "feathery like a fern.
Once PROM has been diagnosed, efforts are made to accurately determine the age of
the fetus and the maturity of its lungs. Premature babies are at great risk if they have
immature lungs. These evaluations can be made using amniocentesis and ultrasound
measurements of the fetus' size. Amniocentesis also allows the practitioner to check for
infection. Other indications of infection include a fever in the mother, increased heart
rate of the mother and/or the fetus, high white blood cell count in the mother, foul
smelling or pus-filled discharge from the vagina, and a tender uterus.
MEDICAL MANAGEMENT
Treatment of PROM depends on the stage of the patient's pregnancy. n PROM
occurring at term, the mother and baby will be watched closely for the first 24 hours to
see if labor will begin naturally. f no labor begins after 24 hours, most doctors will use
medications to start labor. This is called inducing labor. Labor is induced to avoid a
prolonged gap between PROM and delivery because of the increased risk of infection.
Preterm PROM presents more difficult treatment decisions. The younger the fetus, the
more likely it may die or suffer serious permanent damage if delivered prematurely. Yet
the risk of infection to the mother and/or the fetus increases as the length of time from
PROM to delivery increases. Depending on the age of the fetus and signs of infection,
the doctor must decide either to try to prevent labor and delivery until the fetus is more
mature, or to induce labor and prepare to treat the complications of prematurity.
However, the baby will need to be delivered to avoid serious risks to both it and the
mother if infection is present, regardless of the risks of prematurity.
MEDICATIONS
Corticosteroids
Corticosteroids decrease perinatal morbidity and mortality after preterm PROM. A
recent meta-analysis found that corticosteroid administration after preterm PROM,
versus no administration, reduced the risk of respiratory distress syndrome (20 versus
35.4 percent), intraventricular hemorrhage (7.5 versus 15.9 percent), and necrotizing
enterocolitis (0.8 versus 4.6 percent) without an increase in the risk of maternal or
neonatal infection. Because corticosteroids are effective at decreasing perinatal
morbidity and mortality, all physicians caring for pregnant women should understand the
dosing and indications for corticosteroid administration during pregnancy. The most
widely used and recommended regimens include intramuscular betamethasone
(Celestone) 12 mg every 24 hours for two days, or intramuscular dexamethasone
(Decadron) 6 mg every 12 hours for two days. The National nstitutes of Health
recommends administration of corticosteroids before 30 to 32 weeks' gestation,
assuming fetal viability and no evidence of intra-amniotic infection. Use of
corticosteroids between 32 and 34 weeks is controversial. Administration of
corticosteroids after 34 weeks' gestation is not recommended unless there is evidence
of fetal lung immaturity by amniocentesis. Multiple courses are not recommended
because studies have shown that two or more courses can result in decreased infant
birth weight, head circumference, and body length.
ntibiotics
Giving antibiotics to patients with preterm PROM can reduce neonatal infections and
prolong the latent period. A meta-analysis showed that patients receiving antibiotics
after preterm PROM, compared with those not receiving antibiotics experienced
reduced postpartum endometritis, chorioamnionitis, neonatal sepsis, neonatal
pneumonia, and intraventricular hemorrhage. Another meta-analysis found a decrease
in neonatal intraventricular hemorrhage and sepsis. A number of antibiotic regimens are
advocated for use after preterm PROM. The regimen studied by the National nstitute of
Child Health and Human Development trial uses an intravenous combination of 2 grams
of ampicillin and 250 mg of erythromycin every six hours for 48 hours, followed by 250
mg of amoxicillin and 333 mg of erythromycin every eight hours for five days. Women
given this combination were more likely to stay pregnant for three weeks despite
discontinuation of the antibiotics after seven days. t is advisable to administer
appropriate antibiotics for intrapartum group B streptococcus prophylaxis to women who
are carriers, even if these patients have previously received a course of antibiotics after
preterm PROM.
%ocolytic %erapy
Limited data are available to help determine whether tocolytic therapy is indicated after
preterm PROM. As described above, corticosteroids and antibiotics are beneficial when
administered to patients with preterm PROM, but no studies of these therapies
combined with tocolysis are available. Tocolytic therapy may prolong the latent period
for a short time but do not appear to improve neonatal outcomes. n the absence of
data, it is not unreasonable to administer a short course of tocolysis after preterm
PROM to allow initiation of antibiotics, corticosteroid administration, and maternal
transport, although this is controversial. Long-term tocolytic therapy in patients with
PROM is not recommended; consideration of this should await further research.
MANAGEMENT BASED ON GESTATIONAL AGE
O TO WEEKS
When preterm PROM occurs at 34 to 36 weeks' gestation, physicians should avoid the
urge to prolong pregnancy. Studies have shown that labor induction clearly is beneficial
at or after 34 weeks' gestation. One study showed that conservative management
between 34 and 36 weeks' gestational age resulted in an increased risk of
chorioamnionitis and a lower average umbilical cord pH. Another study of 430 women
with preterm PROM revealed that there was no improvement in major or minor neonatal
morbidity after 34 weeks' gestation. Although corticosteroids are not indicated after 34
weeks' gestation, physicians should prescribe appropriate antibiotics for group B
streptococcus prophylaxis and should consider maternal transport to a facility skilled in
caring for premature neonates, if possible. Preterm PROM is not a contraindication to
vaginal delivery.
O 2 TO WEEKS
For patients with preterm PROM at 32 or 33 weeks' gestation with documented
pulmonary maturity, induction of labor and transportation to a facility that can perform
amniocentesis and care for premature neonates should be considered. Prolonging
pregnancy after documentation of pulmonary maturity unnecessarily increases the
likelihood of maternal amnionitis, umbilical cord compression, prolonged hospitalization,
and neonatal infection.
There are few data to guide the care of patients without documented pulmonary
maturity. No studies are available comparing delivery with expectant management when
patients receive evidence-based therapies such as corticosteroids and antibiotics.
Physicians must balance the risk of respiratory distress syndrome and other sequelae of
premature delivery with the risks of pregnancy prolongation, such as neonatal sepsis
and cord accidents. Physicians should administer a course of corticosteroids and
antibiotics to patients without documented fetal lung maturity and consider delivery 48
hours later or perform a careful assessment of fetal well-being, observe for intra-
amniotic infection, and deliver at 34 weeks, as described above. Consultation with a
neonatologist and physician experienced in the management of preterm PROM may be
beneficial. Patients with amnionitis require broad-spectrum antibiotic therapy, and all
patients should receive appropriate intrapartum group B streptococcus prophylaxis, if
indicated.
O 2 TO 1 WEEKS
Delivery before 32 weeks' gestation may lead to severe neonatal morbidity and
mortality. n the absence of intra-amniotic infection, the physician should attempt to
prolong the pregnancy until 34 weeks' gestation. Physicians should advise patients and
family members that, despite these efforts, many patients deliver within one week of
preterm PROM. Contraindications to conservative therapy include chorioamnionitis,
abruptio placentae, and nonreassuring fetal testing. Physicians should administer a
course of corticosteroids and antibiotics and perform an assessment of fetal well-being
by fetal monitoring or ultrasonography. After transport to a facility able to care for
patients with preterm PROM before 32 weeks' gestation, patients should receive daily
(or continuous, if indicated) fetal monitoring for contractions and fetal well-being.
Umbilical cord compression is common (32 to 76 percent) 7 with preterm PROM before
32 weeks' gestation; therefore, at least daily fetal monitoring is indicated. n addition, the
physician should observe closely for fetal or maternal tachycardia, oral temperature
exceeding 100.4F (38C), regular contractions, uterine tenderness, or leukocytosis,
which are possible indicators of amnionitis. Corticosteroid administration may lead to an
elevated leukocyte count if given within five to seven days of PROM.
Evidence suggests that prolonged latency may increase the risk of intra-amniotic
infection. A retrospective analysis of 134 women with preterm PROM at 24 to
32 weeks' gestation who received steroids and antibiotics found a non-significant trend
toward intrauterine inflammation in patients with a latency period longer than one week.
Delivery is necessary for patients with evidence of amnionitis. f the diagnosis of an
intrauterine infection is suspected but not established, amniocentesis can be performed
to check for a decreased glucose level or a positive Gram stain and differential count
can be performed. For patients who reach 32 to 33 weeks' gestation, amniocentesis for
fetal lung maturity and delivery after documentation of pulmonary maturity, evidence of
intra-amniotic infection, or at 34 weeks' gestation should be considered.
O BEFORE 2 WEEKS
The majority of patients will deliver within one week when preterm PROM occurs before
24 weeks' gestation, with an average latency period of six days. Many infants who are
delivered after previable rupture of the fetal membranes suffer from numerous long-term
problems including chronic lung disease, developmental and neurologic abnormalities,
hydrocephalus, and cerebral palsy. Previable rupture of membranes also can lead to
Potter's syndrome, which results in pressure deformities of the limbs and face and
pulmonary hypoplasia. The incidence of this syndrome is related to the gestational age
at which rupture occurs and to the level of oligohydramnios. Fifty percent of infants with
rupture at 19 weeks' gestation or earlier are affected by Potter's syndrome, whereas 25
percent born at 22 weeks' and 10 percent after 26 weeks' gestation are affected.
Patients should be counseled about the outcomes and benefits and risks of expectant
management, which may not continue long enough to deliver a baby that will survive
normally.
Physicians caring for patients with preterm PROM before viability may wish to obtain
consultation with a perinatologist or neonatologist. Such patients, if they are stable, may
benefit from transport to a tertiary facility. Home management of patients with preterm
PROM is controversial. A study of patients with preterm PROM randomized to home
versus hospital management revealed that only 18 percent of patients met criteria for
safe home management. Bed rest at home before viability (i.e., approximately 24
weeks' gestation) may be acceptable for patients without evidence of infection or active
labor, although they must receive precise education about symptoms of infection and
preterm labor, and physicians should consider consultation with experts familiar with
home management of preterm PROM. Consider readmission to the hospital for these
patients after 24 weeks' gestation to allow for close fetal and maternal monitoring.
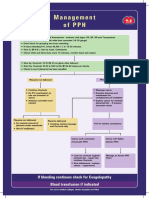
MANAGEMENT OF PROM (DIAGRAM)
Figure 1.
Algorithm for the management of patients with preterm PROM.
COMPLICATIONS
One of the most common complications of preterm PROM is early delivery. The latent
period, which is the time from membrane rupture until delivery, generally is inversely
proportional to the gestational age at which PROM occurs. For example, one large
study3 of patients at term revealed that 95 percent of patients delivered within
approximately one day of PROM, whereas an analysis of studies4 evaluating patients
with preterm PROM between 16 and 26 weeks' gestation determined that 57 percent of
patients delivered within one week, and 22 percent had a latent period of four weeks.
When PROM occurs too early, surviving neonates may develop sequelae such as
malpresentation, cord compression, oligohydramnios, necrotizing enterocolitis,
neurologic impairment, intraventricular hemorrhage, and respiratory distress syndrome.
Complications of PROM
Complications ncidence (%)
Delivery within one week 50 to 75
Respiratory distress syndrome 35
Cord compression 32 to 76
Chorioamnionitis 13 to 60
Abruptio placentae 4 to 12
Antepartum fetal death 1 to 2
PROGNOSIS
The prognosis in PROM varies. t depends in large part on the maturity of the fetus and
the development of infection.
PREVENTION
The only controllable factor associated with PROM is smoking. Cigarette smoking
should always be discontinued during a pregnancy.
HEALTH TEACHING FOR WOMEN WITH PROM
O Take temperature Q4h when awake, Report if more than 38
0
C
O Remain on modified bed rest
O nsert nothing in the vagina
O No sexual activity, No tub baths
O Assess for uterine contraction & fetal movement
O Watch for foul-smelling vaginal discharge
O Wipe front to back after urinating or having a bowel movement
O Take antibiotics if prescribed
CORTICOSTEROIDS Anti inflammatory
ydrocortisone, prednisone, dobutamine ydrocloride, tramadol ydrocloride, nifedifine
TOCOLYTICS
(also called anti-contraction medications or Iabour repressants) are medications used to
suppress premature labor (from the Greek tokos, childbirth, and lytic, capable of dissolving). They are
given when delivery would result in premature birth. The therapy also buys time for the administration
of betamethasone, a glucocorticoid drug which greatly accelerates fetal lung maturity, but takes one to
two days to work.
The suppression of contractions is often only partial and tocolytics can only be relied on to delay birth for
several days. Depending on the tocolytic used the mother or fetus may require monitoring, as for instance
blood pressure monitoring when nifedipine is used as it reduces blood pressure. n any case the risk of
preterm labor alone justifies hospitalization.
%erbutaline sulfate, magnesium sulfate
Necrotizing enterocoIitis (NEC) is a medical condition primarily seen in premature infants,
where
portions of the bowel undergo necrosis (tissue death).
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Nutrition Imbalance Care PlanDocument7 pagesNutrition Imbalance Care PlanMariquita BuenafePas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Journal in PediatricsDocument7 pagesJournal in PediatricsMariquita BuenafePas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Acute PancreatitisDocument20 pagesAcute PancreatitisMariquita BuenafePas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Hemolytic Disease of The Fetus and Newborn JournalDocument10 pagesHemolytic Disease of The Fetus and Newborn JournalMariquita BuenafePas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Effects of Aging in The Cardiovascular SystemDocument6 pagesEffects of Aging in The Cardiovascular SystemMariquita BuenafePas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- DR DrugsDocument2 pagesDR DrugsMariquita BuenafePas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- UrinalysisDocument5 pagesUrinalysisMariquita BuenafePas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Pedia Drugs ImagesDocument1 pagePedia Drugs ImagesMariquita BuenafePas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- CHN - Drug StudyDocument1 pageCHN - Drug StudyMariquita BuenafePas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- RitodrineDocument4 pagesRitodrineMariquita BuenafePas encore d'évaluation
- Pathophysiology of Erythroblastosis Fetalis - RH IsoimmunizationDocument1 pagePathophysiology of Erythroblastosis Fetalis - RH IsoimmunizationRalph Delos SantosPas encore d'évaluation
- Risk for Infection Nursing Care PlanDocument3 pagesRisk for Infection Nursing Care PlanMariquita Buenafe57% (7)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Systems Plus College Foundation Balibago, Angeles City College Of Nursing Drug Study Student Nurse: Buenafe, Ma. Cresencia S. Yr. /Level: BSN III Date: September 25, 2012Document4 pagesSystems Plus College Foundation Balibago, Angeles City College Of Nursing Drug Study Student Nurse: Buenafe, Ma. Cresencia S. Yr. /Level: BSN III Date: September 25, 2012Mariquita BuenafePas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Journal in Anemia and BTDocument19 pagesJournal in Anemia and BTMariquita BuenafePas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- DR DrugsDocument2 pagesDR DrugsMariquita BuenafePas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Focus ChartingDocument3 pagesFocus ChartingMan GatuankoPas encore d'évaluation
- CardiomegalyDocument91 pagesCardiomegalyMariquita Buenafe100% (1)
- NCP CvaDocument4 pagesNCP CvaMariquita BuenafePas encore d'évaluation
- Cardio Drug StudyDocument8 pagesCardio Drug StudyMariquita BuenafePas encore d'évaluation
- Cardio Drug StudyDocument8 pagesCardio Drug StudyMariquita BuenafePas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- NCP Cholecystectomy RevisedDocument7 pagesNCP Cholecystectomy RevisedMariquita Buenafe100% (4)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Cardio Drug StudyDocument8 pagesCardio Drug StudyMariquita BuenafePas encore d'évaluation
- Coronary Artery DiseaseDocument38 pagesCoronary Artery DiseaseMariquita BuenafePas encore d'évaluation
- DengueDocument5 pagesDengueMariquita BuenafePas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Pediatric Nursing FinalDocument35 pagesPediatric Nursing FinalMariquita BuenafePas encore d'évaluation
- Coronary Artery DiseaseDocument9 pagesCoronary Artery DiseaseMariquita Buenafe100% (1)
- Hypertension in PregnancyDocument20 pagesHypertension in PregnancyFAMED RESIDENTS CESMED100% (1)
- Is Sex During Pregnancy Safe?Document3 pagesIs Sex During Pregnancy Safe?mirrawahabPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- FPDocument4 pagesFPHearty ArriolaPas encore d'évaluation
- Pregnancy Among TeenagersDocument5 pagesPregnancy Among TeenagersfarazamPas encore d'évaluation
- 2022 March of Dimes Report Card-Oklahoma SupplementalDocument5 pages2022 March of Dimes Report Card-Oklahoma SupplementalCurtisPas encore d'évaluation
- Thesis SumaryDocument7 pagesThesis SumaryAnonymous hnIkb5Pas encore d'évaluation
- Placenta Abruptio - Topic OverviewDocument8 pagesPlacenta Abruptio - Topic OverviewLei AbellarPas encore d'évaluation
- Skills Checklist - Ob GyneDocument3 pagesSkills Checklist - Ob GyneAnnette Aquino GuevarraPas encore d'évaluation
- OBGYN Nuggets on Diabetes in PregnancyDocument20 pagesOBGYN Nuggets on Diabetes in Pregnancydrusmansaleem100% (1)
- Management of PPHDocument1 pageManagement of PPH098 U.KARTHIK SARAVANA KANTHPas encore d'évaluation
- The Pathology of Placenta Accreta, A Worldwide EpidemicDocument6 pagesThe Pathology of Placenta Accreta, A Worldwide EpidemicYoga ParipurnaPas encore d'évaluation
- Research Article: Bacterial Vaginosis, Educational Level of Pregnant Women, and Preterm Birth: A Case-Control StudyDocument5 pagesResearch Article: Bacterial Vaginosis, Educational Level of Pregnant Women, and Preterm Birth: A Case-Control Studynurul maghfirahPas encore d'évaluation
- UroginDocument13 pagesUroginShandy Suwanto PutraPas encore d'évaluation
- A Century of Labor Induction MethodsDocument4 pagesA Century of Labor Induction MethodsSimon ReichPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Nursing Care of The Client With High-Risk Labor & DeliveryDocument10 pagesNursing Care of The Client With High-Risk Labor & DeliveryWilbert CabanbanPas encore d'évaluation
- Spontaneous MiscarriageDocument14 pagesSpontaneous MiscarriageGomez VanessaPas encore d'évaluation
- Obstetrics V10 Common Obstetric Conditions Chapter Pathology of The Placenta 1663285373Document11 pagesObstetrics V10 Common Obstetric Conditions Chapter Pathology of The Placenta 1663285373Nurliana NingsihPas encore d'évaluation
- Pro Choice SpeechDocument2 pagesPro Choice Speechme_el_st100% (1)
- StratOG Vaginal BreechDocument17 pagesStratOG Vaginal BreechNalin AbeysinghePas encore d'évaluation
- 3 - Intrapartum CareDocument97 pages3 - Intrapartum CareRem AlfelorPas encore d'évaluation
- OB M01 Ch1.1 Normal First TrimesterDocument29 pagesOB M01 Ch1.1 Normal First TrimesterDeshi SportsPas encore d'évaluation
- Poster SurrogacyDocument1 pagePoster Surrogacyapi-372898116Pas encore d'évaluation
- Maternal and Child NursingDocument11 pagesMaternal and Child NursingKSY JanedoePas encore d'évaluation
- Post Partum HemorrhageDocument18 pagesPost Partum Hemorrhageeric100% (1)
- O&G CompendiumDocument676 pagesO&G Compendiumwalefamous100% (1)
- Obstetric and Gynaecological Nursing IInd YearDocument8 pagesObstetric and Gynaecological Nursing IInd YearsanthiyasandyPas encore d'évaluation
- Legacy Birth Services Intake FormDocument7 pagesLegacy Birth Services Intake Formapi-464717431Pas encore d'évaluation
- Preeclampsia Prevalence, Risk Factors, and Pregnancy OutcomesDocument14 pagesPreeclampsia Prevalence, Risk Factors, and Pregnancy OutcomesHaris FadillaPas encore d'évaluation
- Ojsadmin, 993Document6 pagesOjsadmin, 993pondyPas encore d'évaluation
- AbortionDocument41 pagesAbortionp12_miller7777Pas encore d'évaluation
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityD'EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisD'EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisÉvaluation : 4 sur 5 étoiles4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 5 sur 5 étoiles5/5 (78)