Académique Documents
Professionnel Documents
Culture Documents
PPV in Inferior Break RD Archives of Ophthal
Transféré par
bijujcDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
PPV in Inferior Break RD Archives of Ophthal
Transféré par
bijujcDroits d'auteur :
Formats disponibles
CLINICAL SCIENCES
Management of Inferior Breaks in Pseudophakic Rhegmatogenous Retinal Detachment With Pars Plana Vitrectomy and Air
Vicente Martnez-Castillo, MD; Alicia Verdugo, MD; Anna Boixadera, MD; Jos Garca-Arum, MD; Borja Corcstegui, MD
Objective: To determine the role of pars plana vitrec-
tomy without scleral buckling and air as a tamponade with 24 hours of prone positioning in the management of inferior breaks in primary pseudophakic rhegmatogenous retinal detachment.
Methods: Prospective, noncomparative, interventional case series. Fifteen consecutive eyes (15 patients) with primary pseudophakic rhegmatogenous retinal detachment with causative breaks located between the 4-oclock and 8-oclock positions underwent pars plana vitrectomy with air tamponade. The prone position was maintained for 24 hours. Anatomic and functional results are presented. Results: The anatomic reattachment rate was 93.3% after 1 procedure and 100% at the 6-month visit. Mean
preoperative best-corrected visual acuity was 20/60 (range, 20/400 to 20/25) and mean postoperative bestcorrected visual acuity was 20/30 (range, 20/100 to 20/20). In 1 case the retina redetached at the second week because of an undetected break. Postoperative epiretinal membrane was observed in 1 case.
Conclusion: Pars plana vitrectomy and air tamponade with only 24 hours of prone positioning postoperatively is effective in the management of primary pseudophakic rhegmatogenous retinal detachment with causative breaks between the 4-oclock and 8-oclock positions.
Arch Ophthalmol. 2005;123:1078-1081 report on the use of PPV for inferior breaks with 24 hours of prone positioning.
METHODS We included 15 consecutive patients (15 eyes) of 24 consecutive patients with primary pseudophakic RRD and causative inferior breaks between the 4-oclock and 8-oclock positions over a 1-year period. Inferior RRD with subretinal fibrosis or demarcation lines and RRD with proliferative vitreoretinopathy B or greater were excluded. All patients had acute symptoms. Extensive lattice degeneration was not an exclusion criterion. Patients were fully informed of all aspects of the procedure, and all provided written informed consent. We obtained local ethics committee approval for this study. Preoperative evaluation included slitlamp biomicroscopy fundus examination and peripheral retinal evaluation with the binocular indirect ophthalmoscope. The number, type (opercule or horseshoe tear), position (anterior to the equator, equatorial, and posterior to the equator), and size of breaks were determined preoperatively. During postoperative follow-up, the relationship between the air bubble and retinal breaks was established by slitlamp examination.
Author Affiliations: Vall dHebrn Hospital, Universidad Autnoma de Barcelona (Drs Martnez-Castillo, Verdugo, Boixadera, and Garca-Arum); Instituto Oftalmolgico de Barcelona (Drs Martnez-Castillo, Verdugo, and Boixadera); and Instituto de Microciruga Ocular (Drs Garca-Arum and Corcstegui), Barcelona, Spain. Financial Disclosure: None.
detachment (RRD) remains a major problem after cataract surgery because it occurs in approximately 1% of eyes.1 The use of pars plana vitrectomy (PPV) in pseudophakic RRD has gained increasing popularity over the last decade.2 It can be used alone or in combination with scleral explants.2-13 Pars plana vitrectomy improves the visualization of peripheral retina and identification of retinal breaks and enables the removal of vitreous traction.7 Few works have specifically studied the management of inferior breaks during PPV without scleral buckle procedures. In such cases, it is recognized that strict postoperative prone positioning is essential for tamponade inferior breaks when gas or silicone oil is used. This positioning is difficult and uncomfortable for many patients. Posturing periods in the literature vary from 8 to 12 days.14 The current study was conducted to determine the efficacy and safety of PPV and air in pseudophakic RRD with inferior breaks. To our knowledge, this is the first
HEGMATOGENOUS RETINAL
(REPRINTED) ARCH OPHTHALMOL / VOL 123, AUG 2005 1078
WWW.ARCHOPHTHALMOL.COM
Downloaded from www.archophthalmol.com on December 5, 2011 2005 American Medical Association. All rights reserved.
Table 1. Clinical Characteristics of 15 Eyes With Rhegmatogenous Retinal Detachment
Best-Corrected Visual Acuity Patient No./ Age, y/Sex/Eye 1/56/M/OS 2/70/M/OS 3/74/F/OD 4/54/M/OS 5/46/F/OS 6/72/M/OS 7/65/M/OD 8/69/F/OS 9/29/F/OD 10/66/M/OD 11/61/F/OS 12/79/M/OS 13/46/F/OS 14/56/F/OD 15/32/F/OS Pseudophakia Phaco Phaco Phaco Phaco Phaco Phaco Phaco Phaco sulcus Phaco Phaco Phaco Phaco Phaco Phaco Phaco Posterior Capsule Status Normal Normal Nd-YAG Normal Normal Normal Broken Broken Normal Broken Normal Normal Normal Normal Normal Time From Phaco to RRD, mo 6 14 48 4 10 81 12 72 20 11 16 60 54 44 38 Preoperative 20/400 20/400 20/30 20/25 20/30 20/25 20/400 20/400 20/125 20/30 20/200 20/400 20/400 20/400 20/40 Postoperative 20/25 20/30 20/30 20/25 20/50 20/25 20/40 20/40 20/30 20/30 20/30 20/50 20/40 20/25 20/40 Complications 0 0 Punctate superficial keratopathy 0 Macular pucker 0 0 0 0 0 0 0 0 Redetachment 0
Abbreviations: Phaco, phacoemulsification; RRD, rhegmatogenous retinal detachment.
All procedures were performed under retrobulbar anesthesia by the same surgeon (V.M.-C.). Three-port PPV was performed using a wide-angle viewing system. After central and peripheral vitreous removal, all eyes underwent intraoperative scleral depression for 360 for trimming of the vitreous base and removal of all vitreous traction on retinal tears. Vitreous was removed over the pars plana. Perfluoro-n-octane (C8F18; Adato-octa, Adatomed, Mnchen, Germany) was injected over the posterior pole through a 20-gauge blunt cannula in all cases. Once it reached the posterior border of the break, a fluid-air exchange was performed to drain the subretinal fluid through the causative break. Sclerotomies were carefully reviewed before the fluid-air exchange. Two rows of diode laser retinopexy (IRIS Medical Inc, Mountain View, Calif ) were applied to treat causative breaks after the fluid-air exchange; 360 prophylactic laser was not used. No drainage retinotomy was performed. At the end of the procedure, fluid was aspirated with a flute needle to ensure complete air-fill of the cavity. Air was used as an internal tamponade in all cases. Sclerotomies were carefully closed to avoid air loss during the first postoperative hours. No complications developed during the surgical procedure. Patients were instructed to maintain the prone position for 24 hours. Patients were followed up at 24 hours, 48 hours, 72 hours, 1 week, 2 weeks, 1 month, 3 months, and 6 months postoperatively. Visual acuity, the anatomic reattachment, and the proliferative vitreoretinopathy rate were examined at 1 month, 3 months, and 6 months postoperatively. RESULTS
2 (range, 1-5). Thirty breaks were treated: 25 anterior to the equator, 4 equatorial, and 1 posterior to the equator. Twenty-one breaks were less than 1 clock hour and 9 were 1 clock hour or larger. Nine breaks were opercules and 21 horseshoe tears. The average size of the air bubble on postoperative day 1 was 75%, and the range was 60% to 90%. Five breaks located at the 6-oclock position were not covered by air at 24 hours postsurgery without prone positioning. No break had tamponade for more than 3 days. Patient demographic data and RRD characteristics are listed in Table 1 and Table 2. All patients maintained the prone position for 24 hours postsurgery. Preoperative visual acuity for the entire population ranged from 20/400 to 20/25 (mean, 20/60). Postoperative visual acuity ranged from 20/100 to 20/20 (mean, 20/30) at the final follow-up visit. In 1 patient (case 14) the retina redetached at the second week because of an undetected opercule at the 6-oclock position anterior to the primary break and was treated with PPV and 25% sulfur hexafluoride. Another patient developed an epiretinal membrane that required PPV. We observed an inferior break in 1 patient (Figure). No major postoperative complications occurred.
COMMENT
Seven eyes of 7 men (46.66%) and 8 eyes of 8 women (53.33%) composed our study population. Mean follow-up was 8 months (range, 7-10 months). Mean patient age was 58.33 years (range, 29-79 years). On preoperative examination, all eyes had a posterior chamber intraocular lens. The posterior lens capsule was intact in 11 (73.33%) of 15 eyes and broken at the time of cataract surgery or postoperatively with a Nd-YAG laser capsulotomy in 4 eyes (26.66%). The mean number of quadrants affected was 2 (range, 1-3). The macula was found to be detached in 9 (60%) of 15 eyes. The average number of breaks was
(REPRINTED) ARCH OPHTHALMOL / VOL 123, AUG 2005 1079
Pars plana vitrectomy for pseudophakic RRD has gained popularity over the last decade.2-13 The advantages of PPV are the removal of all vitreous traction on retinal tears and improved microscope visualization of peripheral retina. This advantage is very important in patients with pseudophakia because preoperative examination is more difficult than in phakic patients. Other advantages are the removal of posterior capsular lens opacities for better visualization of the peripheral retinal tears and minimal changes induced in refractive error.7 Two potential disadvantages of repairing pseudophakic retinal detachments with primary PPV are the need
WWW.ARCHOPHTHALMOL.COM
Downloaded from www.archophthalmol.com on December 5, 2011 2005 American Medical Association. All rights reserved.
Table 2. Characteristics of Rhegmatogenous Retinal Detachments
Break Size in Disc Diameter , , , 1.5, , , , 2 1, 1 , 1 1 1, , , , 1 1 1, , Break Position in Clock Hour 4, 4:30, 5, 6, 7 7 6, 8 4, 4:30, 5-7 4, 5:30 6 4, 7 5 5 4, 5 4, 5 4:30, 5, 6 5 6:30, 7 4:30, 5 Break Position in Relation to Equator Anterior Anterior Anterior Anterior At equator Anterior Anterior, at equator Anterior Anterior Anterior Anterior, posterior Anterior-anterior Anterior Anterior, at equator Anterior, at equator
Patient No. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15
Quadrants 2 1 2 2 2 3 2 2 2 3 1 2 2 2 2
Macula Off Off On On On On Off Off Off On Off Off Off Off On
Breaks, No. (Types) 5 (H, O, O, H, H) 1 (H) 2 (O, O) 3 (H, H, H) 2 (H, H) 1 (H) 2 (H, H) 1 (O) 1 (O) 2 (H, H) 2 (H, H) 3 (H, O, H) 1 (H) 2 (H, O) 2 (H ,O)
Abbreviations: H, horseshoe tear; O, opercule.
for postoperative positioning and the restriction from air travel.14 When causative breaks are located inferiorly (between the 4-oclock and 8-oclock positions), 1 inherent problem in the use of PPV is the difficulty in maintaining a direct tamponade on inferior breaks for at least 8 days using different currently available gases.14 Indeed, perfluorocarbon liquids and different types of silicone oil have been used to tamponade these breaks in RRD.15,16 However, the minimum number of days in the prone position required to ensure tamponade of inferior breaks remains to be determined. Different authors have reported on the management of inferior breaks with PPV alone.2-8 Tanner et al2 reported an 89% anatomic success rate in a pilot study with 3 different tamponade agents (30% sulfur hexafluoride, 12%14% perfluoropropane, and silicone oil). All patients were instructed to maintain the prone position for 10 days. Escoffery et al3 identified 2 cases; however, no information is given on the results in these 2 cases. Heimann et al6 treated 6 patients with primary RRD and inferior breaks with PPV and sulfur hexafluoride. They reported a 50% retinal redetachment rate. All these series included both inferior and superior causative breaks. There is no consensus on the type of tamponade agent and the duration of prone posture. In cases with gas, a minimum of 8 to 10 days prone posture has been recommended.14 In this series, it proved possible to manage inferior breaks in pseudophakic RRD with PPV alone and 24 hours of prone positioning. The present study included only inferior RRD with causative breaks located between the 4-oclock and 8-oclock positions to determine the minimum time of tamponade required for the retinopexy to be effective. Our overall success rate of reattachment with 1 procedure was 93.3%. Mean postoperative best-corrected visual acuity was 20/30 (range, 20/100 to 20/20). No major complications developed during postoperative follow-up. These results compare favorably with those of previous series.2-10 However, careful case selection and the limited number of eyes may have influenced these results.
(REPRINTED) ARCH OPHTHALMOL / VOL 123, AUG 2005 1080
Yoon and Marmor17 provided direct experimental evidence that fresh laser burns produced a greater-thannormal adhesive bond between the retina and retinal pigment epithelium at 24 hours posttreatment. They also stated that the adhesive force of the photocoagulated areas continued to increase for 2 weeks.17 Folk et al18 reported similar results in a different experimental model and 1 human eye. Kita et al19 measured the retinal adhesive force after laser photocoagulation in living eyes and observed rapid enhancement at 24 hours. This is the reason for maintaining postoperative prone positioning for 24 hours. The concept of performing PPV with air and 24 hours of prone posturing arose from clinical observations made in the first 24 hours post-PPV without scleral buckling in pseudophakic RRD with perfluoropropane tamponade. We observed that breaks in 2 patients located between the 5-oclock and 7-oclock positions were not covered by the gas at 24 hours postsurgery. These patients maintained only 1 day of prone posturing and the retina reattached without complications. On the basis of these observations, we decided to use air to reduce morbidity and enable rapid visual recovery. In our series, 5 of the 30 breaks were located at the 6-oclock position. In all these cases, air was effective for retinal reattachment. In these cases, the process of chorioretinal adhesion was not influenced by the position of the breaks and retinal reattachment was achieved. The efficacy of a tamponade agent lies in its ability to make contact with the retina.20,21 We believe that the size of the air bubble during the first hours is most important for tamponade of inferior retinal breaks. Peripheral vitreous removal and pseudophakia are the main factors influencing the bubble size because they both permit complete filling of the vitreous cavity. In this series, the final reattachment rate of 100% was not affected by break size or type. Tamponade of inferior breaks for the first 24 hours postsurgery suffices for chorioretinal adhesion. In summary, the implications of this study are that 24 hours of prone positioning is effective for the manWWW.ARCHOPHTHALMOL.COM
Downloaded from www.archophthalmol.com on December 5, 2011 2005 American Medical Association. All rights reserved.
Submitted for Publication: March 8, 2004; final revision received September 21, 2004; accepted November 5, 2004. Correspondence: Vicente Martnez-Castillo, MD, Calle Londres No. 54, 41B, Barcelona 08036, Spain (31756vmc @comb.es).
REFERENCES
1. Javitt JC, Vitale S, Canner JK, Krakauer H, McBean AM, Sommer A. National outcomes of cataract extraction, I. retinal detachment after inpatient surgery. Ophthalmology. 1991;98:895-902. 2. Tanner V, Minihan M, Williamson TH. Management of inferior retinal breaks during pars plana vitrectomy for retinal detachment. Br J Ophthalmol. 2001;85: 480-482. 3. Escoffery RF, Olk RJ, Grand MG, Boniuk I. Vitrectomy without scleral buckling for primary rhegmatogenous retinal detachment. Am J Ophthalmol. 1985;99: 275-281. 4. Hakin KN, Lavin MJ, Leaver PK. Primary vitrectomy for rhegmatogenous retinal detachment. Graefes Arch Clin Exp Ophthalmol. 1993;231:344-346. 5. Gartry DS, Chignell AH, Franks WA, Wong D. Pars plana vitrectomy for the treatment of rhegmatogenous retinal detachment uncomplicated by advanced proliferative vitreoretinopathy. Br J Ophthalmol. 1993;77:199-203. 6. Heimann H, Bornfeld N, Friedrichs W, et al. Primary vitrectomy without scleral buckling for rhegmatogenous retinal detachment. Graefes Arch Clin Exp Ophthalmol. 1996;234:561-568. 7. Campo RV, Sipperley JO, Sneed SR, et al. Pars plana vitrectomy without scleral buckle for pseudophakic retinal detachments. Ophthalmology. 1999;106:18111815. 8. Bartz-Schmidt KU, Kirchhof B, Heimann K. Primary vitrectomy for pseudophakic retinal detachment. Br J Ophthalmol. 1996;80:346-349. 9. Brazitikos PD, DAmico DJ, Tsinopoulos IT, Stangos NT. Primary vitrectomy with perfluoro-n-octane use in the treatment of pseudophakic retinal detachment with undetected retinal breaks. Retina. 1999;19:103-109. 10. Speicher M, Fu A, Martin J, Von Fricken M. Primary vitrectomy alone for repair of retinal detachments following cataract surgery. Retina. 2000;20:459464. 11. SPR Study Group. View 2: the case for primary vitrectomy. Br J Ophthalmol. 2003; 87:784-787. 12. Sharma T, Gopal L, Badrinath SS. Primary vitrectomy for rhegmatogenous retinal detachment associated with choroidal detachment. Ophthalmology. 1998; 105:2282-2285. 13. Oshima Y, Yamanishi S, Sawa M, Motokura M, Harino S, Emi K. Two-year follow-up study comparing primary vitrectomy with scleral buckling for macula-off rhegmatogenous retinal detachment. Jpn J Ophthalmol. 2000;44: 538-549. 14. Thompson J. Intraocular gases and techniques for air-fluid exchange. In: Vitreoretinal Surgical Techniques. London, England: Dunitz; 2001:157-172. 15. Bottoni F, Sborgia M, Arpa P, et al. Perfluorocarbon liquids as postoperative shortterm vitreous substitutes in complicated retinal detachment. Graefes Arch Clin Exp Ophthalmol. 1993;231:619-628. 16. Wolf S, Schn V, Meier P, Wiedemann P. Silicone oil-RMN3 mixture (heavy silicone oil) as internal tamponade for complicated retinal detachment. Retina. 2003; 23:335-342. 17. Yoon YH, Marmor MF. Rapid enhancement of retinal adhesion by laser photocoagulation. Ophthalmology. 1988;95:1385-1388. 18. Folk JC, Sneed SR, Folberg R, Coonan P, Pulido JS. Early retinal adhesion from laser photocoagulation. Ophthalmology. 1989;96:1523-1525. 19. Kita M, Negi A, Kawano S, Honda Y. Photothermal, cryogenic, and diathermic effects of retinal adhesive force in vivo. Retina. 1991;11:441-444. 20. Fawcett IM, Williams RL, Wong D. Contact angles of substances used for internal tamponade in retinal detachment surgery. Graefes Arch Clin Exp Ophthalmol. 1994;232:438-444. 21. Williams R, Wong D. The influence of explants on the physical efficiency of tamponade agents. Graefes Arch Clin Exp Ophthalmol. 1999;237:870-874.
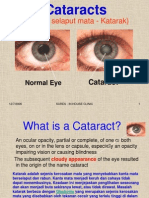
Figure. A, Case 5: fundus photography showing a primary break before surgery. Horseshoe tear from the 5-oclock to 7-oclock positions. B, Postoperative day 7: fundus photography showing the same break photocoagulated. C, Postoperative 1 month: fundus photography showing the primary break pigmented.
agement of inferior retinal breaks in pseudophakic RRD treated by PPV. The combination of excellent patient selection, meticulous peripheral vitrectomy, and laser retinopexy account for the anatomic results in this series. The results are encouraging and, if reproducible in a larger series, might persuade surgeons to reduce postoperative posturing time in these patients.
(REPRINTED) ARCH OPHTHALMOL / VOL 123, AUG 2005 1081
WWW.ARCHOPHTHALMOL.COM
Downloaded from www.archophthalmol.com on December 5, 2011 2005 American Medical Association. All rights reserved.
Vous aimerez peut-être aussi
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- History Lessons What Business and Management Can Learn From The Great Leaders of HistoryDocument274 pagesHistory Lessons What Business and Management Can Learn From The Great Leaders of HistorybijujcPas encore d'évaluation
- KeratoconusDocument10 pagesKeratoconusbijujcPas encore d'évaluation
- Fluorescein Wall ChartDocument1 pageFluorescein Wall ChartbijujcPas encore d'évaluation
- Indirect OphthalmosDocument3 pagesIndirect Ophthalmosbijujc100% (1)
- Disability Evaluation GuidelinesDocument50 pagesDisability Evaluation Guidelinesbijujc100% (4)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- 14.kuliah-Histologi MataDocument35 pages14.kuliah-Histologi MataRahmat NugrohoPas encore d'évaluation
- Cataract Cataracts CataractDocument6 pagesCataract Cataracts Cataractta CPas encore d'évaluation
- Perfect Vision MethodDocument66 pagesPerfect Vision MethodSameh Kahlool100% (1)
- Medical RetinaDocument193 pagesMedical RetinaHanda YaniPas encore d'évaluation
- Entoptic Phenomena, Photopsias, Phosphenes Entoptic Phenomena, Photopsias, Phosphenes Entoptični Pojavi, Fotopsije in FosfeniDocument11 pagesEntoptic Phenomena, Photopsias, Phosphenes Entoptic Phenomena, Photopsias, Phosphenes Entoptični Pojavi, Fotopsije in FosfeniYahya YuusufPas encore d'évaluation
- Gonioscopic AnatomyDocument30 pagesGonioscopic AnatomymanognaaaaPas encore d'évaluation
- Daftar Harga BHP Alkes Mata 2021Document2 pagesDaftar Harga BHP Alkes Mata 2021nadyaPas encore d'évaluation
- DR Tahir Eye mcqs1Document10 pagesDR Tahir Eye mcqs1YUAN LIPas encore d'évaluation
- Opd - Scan Ii PDFDocument6 pagesOpd - Scan Ii PDFDfhos Oftalmo ServicePas encore d'évaluation
- Congenital Cranial Dysinnervation Disorders (CCDDS) - Duane Syndrome Brown SyndromeDocument62 pagesCongenital Cranial Dysinnervation Disorders (CCDDS) - Duane Syndrome Brown SyndromeGaurav shuklaPas encore d'évaluation
- Cataracts PACESDocument2 pagesCataracts PACESDheeshana SayakkaragePas encore d'évaluation
- Use of Dyes in OphthalmologyDocument4 pagesUse of Dyes in OphthalmologyMaulana MalikPas encore d'évaluation
- Cataract and Eye Care DCaDocument26 pagesCataract and Eye Care DCaSamuil SumpalPas encore d'évaluation
- Red Reflex Test: ProcedureDocument6 pagesRed Reflex Test: ProcedureFitri Amelia RizkiPas encore d'évaluation
- Statistical Eye Model For Normal EyesDocument9 pagesStatistical Eye Model For Normal EyesIts EithanPas encore d'évaluation
- Ocular TraumaDocument44 pagesOcular TraumaKing DonPas encore d'évaluation
- Diagnosis MataDocument168 pagesDiagnosis Mata19. Moh Hidayatullah AL AhyaPas encore d'évaluation
- Differences Between Ophthalmologist, and OpticianDocument2 pagesDifferences Between Ophthalmologist, and OpticianLay EcanPas encore d'évaluation
- Proliferative Diabetic RetinopathyDocument9 pagesProliferative Diabetic RetinopathyValerie Anne BebitaPas encore d'évaluation
- Instant Download Test Bank For Macroeconomics For Life Smart Choices For All2nd Edition Avi J Cohen PDF EbookDocument32 pagesInstant Download Test Bank For Macroeconomics For Life Smart Choices For All2nd Edition Avi J Cohen PDF Ebookjordangonzaleswqigpzmcst100% (13)
- Cranial Nerves: DR - Ahmed Gaber Ass. Prof of Neurology Ain Shams UniversityDocument45 pagesCranial Nerves: DR - Ahmed Gaber Ass. Prof of Neurology Ain Shams UniversityKhaled OssamaPas encore d'évaluation
- Structure and Function of The EyesDocument5 pagesStructure and Function of The EyesPreeti ShuklaPas encore d'évaluation
- Real-Life Outcomes of Subthreshold LaserDocument8 pagesReal-Life Outcomes of Subthreshold LaserPutri kartiniPas encore d'évaluation
- Pentacam: Instruction ManualDocument67 pagesPentacam: Instruction ManualWang JYPas encore d'évaluation
- Optics Made EasyDocument52 pagesOptics Made EasyKwaku Afriyie KyeiPas encore d'évaluation
- Extirpation of Eye - DoxcDocument2 pagesExtirpation of Eye - Doxckushal NeupanePas encore d'évaluation
- 34Document2 pages34Walisson BarbosaPas encore d'évaluation
- Vitreous FloatersDocument35 pagesVitreous FloatersnadiasalimaPas encore d'évaluation
- Ophthalmology Set 1Document6 pagesOphthalmology Set 1ajay khadePas encore d'évaluation
- Presentation 2Document57 pagesPresentation 2medhanit anjuloPas encore d'évaluation