Académique Documents
Professionnel Documents
Culture Documents
Journal of The Anatomical Society of India
Transféré par
onlyjust4me0 évaluation0% ont trouvé ce document utile (0 vote)
18 vues11 pagesAn attempt is being made to discuss the anatomical basis Ior various surgical incisions in the human body. A sound, healthy and cosmetically acceptable scar is what patient wishes to see Iirst oI all aIter surgery. Incisions are always designed based upon certain anatomical land marks. Without the proper knowledge oI anatomy oI the part, surgery can not be attempted.
Description originale:
Titre original
Journal of the Anatomical Society of India
Copyright
© Attribution Non-Commercial (BY-NC)
Formats disponibles
DOCX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentAn attempt is being made to discuss the anatomical basis Ior various surgical incisions in the human body. A sound, healthy and cosmetically acceptable scar is what patient wishes to see Iirst oI all aIter surgery. Incisions are always designed based upon certain anatomical land marks. Without the proper knowledge oI anatomy oI the part, surgery can not be attempted.
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
18 vues11 pagesJournal of The Anatomical Society of India
Transféré par
onlyjust4meAn attempt is being made to discuss the anatomical basis Ior various surgical incisions in the human body. A sound, healthy and cosmetically acceptable scar is what patient wishes to see Iirst oI all aIter surgery. Incisions are always designed based upon certain anatomical land marks. Without the proper knowledge oI anatomy oI the part, surgery can not be attempted.
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 11
1ournal of the Anatomical Society of India
All Medical Journals Issues Contents Editorial Board
& InIormation
Surgical Incisions - Their Anatomical Basis: Part 1 - Head
And Neck
Author(s): Patnaik V.V.G.`, Singla R.K.` and Bala Sanjus
Vol. 49, No. 1 (2000-01 - 2000-06)
Department oI Anatomy, *Govt. Medical College, Amritsar (Punjab) and Govt. Dental College,
Amritsar (Pb.) INDIA.
Abstract:
Applied Anatomy i.e. application oI knowledge oI anatomy in clinical and surgical practise is the
most vital branch oI anatomy. There is no Iun oI studying anatomy, iI its knowledge can't be
used in clinics.
Surgical incisions are always designed based upon certain anatomical land marks. Without the
proper knowledge oI anatomy oI the part, surgery can not be attempted. Norman and Bramley
(1990) have given certain general guidelines Ior incisions. An attempt is being made to discuss
the anatomical basis Ior various surgical incisions in the human body oI which this paper is a
part pertaining to the "Head and Neck" region.
Keywords: Surgical Incisions - Head and Neck
ZtroductioZ
In the era oI cosmetic surgery the value oI precise incision on the skin has increased maniIold.
Anywhere in the body a sound, healthy and cosmetically acceptable scar is what patient wishes
to see Iirst oI all aIter surgery. The value oI such scar increases in Iace Ior obvious reasons. The
incisions can't be given anywhere and in any direction. In this context, anatomy should be
considered 'mother oI surgery' as without a proper knowledge oI it, one can't attempt surgery and
every surgical incision has a sound anatomical basis.
Norman and Bramley (1990) give certain guidelines Ior incisions in general i.e. incisions :
1 should be based on sound anaLomlcal prlnclples
2 should have clear anaLomlcal landmarks
3 should be deslgned Lo glve proLecLlon Lo Lhe lmporLanL nerves ln Lhe vlclnlLy eg aurlculo
Lemporal and faclal nerves ln paroLld reglon
should provlde relaLlvely blood less fleld
3 should provlde excellenL vlslblllLy of Lhe leslonal slLe wlLhouL Lenslon
6 should be rapldly and confldenLly execuLed
7 should be uncompllcaLed ln lLs repalr
8 should glve a good cosmeLlc resulL wlLh mlnlmal funcLlonal sequalae
9 should be readlly Leachable
ruger (1989) Iurther added that while giving an incision, skin should be stretched in a way that
marked line oI incision rests on a solid bone thereby providing a Iirm base Ior clean incision in
one deIt incising move. Also the incision should be perpendicular to the skin and completely
through it. Cutting on the bias may result in an edge with decreased vascular supply and possible
widening oI the resultant scar.
Dupuytren (1834) was 1st to note the skin tension when he conIronted with the corpse oI a man
who had stabbed himselI with an awl and wounds on his body were elliptical instead oI round.
Other researchers such as Filhos (1833), Eschricht (1837), Malgaigne (1938) and Voight (1857)
also studied the same phenomenon. Langer (1861) studied incisions and puncture wounds in
cadavers and his results were published as a schematic representation oI the lines oI greatest
normal skin tension Ior all regions oI the body. ocher (1907) set Iorth the principle that surgical
incisions should be made along these Langer lines oI normal skin tension; in this manner the skin
would be closed under the least amount oI tension and resulting scar would be minimum. Rubin
(1948), raissl (1951) and Bulacio Nunez (1974) have challenged Langer's original concepts and
have provided new maps oI skin tension. Langer's lines tend to run parallel with skin creases,
which generally are perpendicular to the action oI underlying muscles. The action oI these
muscles would tend to pull an incision apart. In these newer studies many oI the lines are
perpendicular to Langer's lines particularly in the head and neck region. Despite this skin
incisions are still generally placed within skin creases to hide the scar.
urgical iZcisioZs iZ bead aZd Neck {Maxillofacial area]
(A) Maxillofacial incisions
1 or mandlble
1 Submandlbular lnclslon
2 8lsdons lnclslon
3 8eLromandlbular lnclslon
SubmenLal lnclslon
2 or Lemporomandlbular [olnL
1 reaurlcular lnclslon wlLh varlaLlons
2 osLaurlcular lnclslon
3 Lndaural lnclslon
lnLraoral lnclslon
3 1emporal lnclslon
6 Submandlbular lnclslon
3 or zygoma
1 Cllles lnclslon
2 Crows fooL lnclslon
3 LaLeral eyebrow lnclslon
or orblL
1 1ranscon[uncLlval
2 lnfraorblLal
3 8lcoronal
3 or nose
1 Medlan verLlcal
2 P shaped
3 8llaLeral Z approach
W shaped approach
3 Coronal approach
(B) Other incisions
1 8lock dlssecLlon of neck
2 Lxposure of sallvary glands
3 1racheosLomy
1hyroldecLomy
{A] Maxillofacial iZcisioZs
(1) For mandible
(a) Submandibular incision: This incision is used Ior approach to ramus oI mandible
extraorally in cases oI severe trismus, limitation oI jaw opening, a small mouth or severe
mandibular prognathism. It is made one Iinger breadth below the lower border oI ramus (Fig 1).
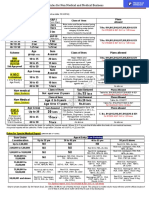
Fig. 1. Commonly used skin incisions. A, Submandibular. B, Risdon. C,
retromandibular D, preauricular, E. Gillies, F. Lateral Eyebrow
Fig.2. The Al ayat and Bramley modiIication oI the preauricular approach
The design must be related to diminish the scar and reduce the risk oI damage to the marginal
mandibular branch oI Iacial nerve. Undoubtedly, the skin crease is best approach as Iar as
scarring is concerned, but in adolescent, a crease is not always Iound and there the incision
should Iollow Langer's lines and should be situated I cm below the lower border with length not
2.5 cm (Moore,) Care should be taken to avoid external jugular vein running Irom the angle oI
mandible downwards and posteriorly towards junction oI middle and lateral third oI clavicle
where it joins subclavian vein.
Dingman and Grabb (1962) in dissections oI 100 marginal mandibular nerves Iound that in 81
oI instances this nerve passed above the inIerior border oI mandible posterior to anteroinIerior
angle oI masseter where Iacial artery enters the Iace and in rest oI 19 cases, it made a
downward arc, the lowest point oI which was I cm below the inIerior border. They Iurther added
that anterior to the point where Iacial artery enters Iace, all the branches oI Iacial nerve which
innervate depressers oI lower lip pass above the inIerior border and the branches which were
present below the mandible were innervating platysma and not depressors oI lower lip. However,
since the anterior Iibres oI platysma Irequently continue with lower Iibres oI depressor labii
inIerioris, these muscles contract as a unit and iI the branches to platysma are cut a Ialse
interpretation oI damage to nerve supply oI depressor labii inIerioris may be made.
In all the cases, the marginal mandibular nerve lay in a plane superIicial to Iacial artery being
situated immediately, anterior, posterior or on it. However, submandibular lymphnode lay
immediately posterior to the artery and is a constant landmark in this region Ior searching
marginal mandibular nerve. The mandibular and buccal branches inosculate only in 5 cases in
which iI Iormer is damaged, muscles supplied by it may escape because oI innervation Irom the
other (Dingman and Grabb, 1962).
The platysma is cut along the incision line again to avoid damage to marginal mandibular nerve.
At the anterior terminus oI incision there lie Iacial vessels and submandibular lymphnodes which
should be leIt intact. Further by blunt dissection, lower border oI mandible, ramus, sigmoid
notch, condylar neck, lower part oI coronoid process and anterior border oI ramus may be
reached.
(b) Risdon's incision: It is a modiIication oI submandibular incision, so ruger (1990) discussed
it under same heading. Here the submandibular incision is extended posteriorly and curved in
best cosmetic conIirmity with angle oI mandible later being the posterior terminus oI incision.
Anterior terminus remains corresponding to point oI entrance oI Iacial artery in Iace (Fig.1)
(Rongetti, 1954). ruger (1990) and Thoma (1963) keep this incision 2 cm below inIerior border
oI mandible Ior the same reasons i.e. marginal mandibular nerve passes maximum 1 cm below
inIerior margin oI mandible.
(c) Retromandibular incision: It is considered best Ior approaching subcondylar Iractures by
Hinds (1967) so named aIter him also. This incision begins approximately I cm below the lobe oI
ear and I cm posterior to ramus oI mandible. (Fig.1) Parotid is retracted anteriorly and Iibres oI
masseter are separated bluntly along their vertical course to reach underlying ramus. The location
oI incision is such that it is aesthetically more pleasing.
(d) Submental incision: This approach is used only iI major re-positioning oI lower border oI
symphysis menti is needed. Usually symphysis menti is approached intraorally. The incision is
given along a skin crease I cm below the lower border oI mandible and parallel to it provided it
lies in the submental skin crease. II later is absent, then it is placed 0.5 cm below and behind
symphysis to produce a scar which is well hidden. There is little risk oI damage to marginal
mandibular branch oI Iacial nerve which has already crossed the lower border oI mandible and
reached the Iace. The blood supply to lower border may be maintained to some extent by
avoiding stripping the genial muscle in midline (Moore).
bmandibular. B, Risdon. C, retromandibular
D, preauricular, E. Gillies, F. Lateral Eyebrow
(II) Incisions for temporomandibular joint :
(a) Pre-auricular incision with its variations: This gives the easiest approach to mandibular
condyle, although iI both condyles need to be exposed Ior extensive condylar ankylosis, the
bicoronal Ilap may be worthwhile. The pre-auricular incision is sited just anterior to pinna or
alternatively around the tragus and at the junction oI the ear and the scalp superiorly. It is then
directed obliquely Iorwards and upwards at an angle oI 45. (Fig.1) Usually posterior branch oI
superIicial temporal artery requires ligation while its anterior branch and auriculotemporal nerve
are retracted anteriorly.
Al Kayat and Bramley (1979) modification - This modiIication is used Ior a wider exposure.
They recommended a question mark shaped skin incision which avoids main vessels and nerves
(See Fig.2) About 2 cm above the malar arch, the temporalis Iascia splits into 2 parts, which can
be easily identiIied by Iat globules between 2 layers which Iorm an important landmark. In this,
temporal Iacia and superIicial temporal artery are reIlected with skin Ilap. Later helps in better
healing oI the Ilap. Under no circumstances should the inIerior end oI the skin incision be
extended below the lobe oI the ear as it increases the risk oI damage to main trunk oI Iacial
nerve. It is particularly important in children where it may be quite superIicial. The length oI the
Iacial nerve which is visible to the surgeon is about 1.3 cm. It divides into temporoIacial and
cervicoIacial divisions at a point vertically below the lowest part oI bony external auditory
meatus at a distance oI 2.3 0.28cm; shortest distance being 1.5 cm. The distance between
lowest point oI posterior glenoid tubercle to biIurcation oI Iacial nerve is 3.0 0.3 cm; shortest
distance being 2.4 cm (Alkayat and Bramley, 1979).
(b) Postauricular incision with variations - This incision as described Iully by Alexander and
James (1975) is placed in the groove between the helix and post auricular skin so that the entire
ear can be reIlected anteriorly aIter completely dividing the cartilagenous external auditory
canal. It gives a wide exposure to joint with cosmetic advantage since the scar is completely
hidden behind the auricle. But there may be partial stenosis oI auditory canal and necrosis oI
auricular cartilage causing deIormity oI pinna.
Circum meatal approach: It is a modiIication oI post auricular approach incorporating
elements oI preauricular and postauricular incisions. The preauricular incision commences at
upper border oI tragus and passed upwards in preauricular crease to reach most superior
attachment oI helix to scalp. From here, incision is carried backwards and downwards around the
outer margin oI Iunnel shaped bony audiotry meatus to terminate just above the commencement
oI mastoid process. The cosmetic results with this approach are excellent with transient weakness
oI upper branches oI Iacial nerve in only 1.6 cases (Moore,).
(c) Endaural approach: It was designed by Davidson (1955) and passes downwards and
backwards in the cleIt between the helix and tragus and proceeds along the rooI oI external
auditory canal Ior approximately I cm. It is then reversed and made at anterior halI oI meatal
circumIerence at the junction oI cartilaginous and bony meati. A surgical cleIt is thus created
along almost an avascular plane leading to posterior aspect oI joint capsule behind and beneath
the glenoid lobe oI parotid gland and its contained arteries and nerves. Since the direction oI
external auditory canal is downwards, Iorwards and medially so dissection should proceed in
same Iashion otherwise tympanic membrane can be injured.
(d) Intraoral approach: It was described by Sear (1972) Ior removal oI hyperplastic condyles.
The incision commences at the level oI upper occlusal plane and passes downwards and Iorwards
between the internal and external oblique ridges oI mandible and then Iorwards as necessary
along mandibular body. Upper end should not be extended beyond the level oI upper molar teeth,
otherwise buccal pad oI Iat is encountered and prolapses in the wound decreasing the visibility.
(e) Temporal approach: It is Alkayat and Bramley (1979) modiIication oI preauricular
approach discussed vide supra.
(I) Submandibular approach: It is the Risdon's modiIication oI submandibular incision
discussed vide supra.
(g) Face lift incision: It comprises a pre-auricular component together with and in continuity
with the postauricular component much oI which may be in the hair line. It has advantages oI
preauricular approach with better aesthetics (Zide and ent, 1983).
{] ZcisioZs for zygoma:
(a) Gille's incision: It is also known as temporal Iossa approach and was 1st introduced by Gilles
et al (1927). The rationale Ior it depends upon the Iact that temporal Iascia is attached to the
outer aspect and superior border oI zygomatic arch and beneath this layer and superIicial to
temporalis muscles, there is a potential tissue plane into which a long Ilat and narrow instrument
can be introduced to liIt the depressed zygomatic bone or arch.
The superIicial temporal artery crosses posterior root oI zygomatic process oI temporal bone and
biIurcates into anterior and posterior branches 5 cm above it. The anterior branch runs towards
Irontal tuberosity (Williams et al, 1999). The incision about 2.5 cm long is made above and
parallel to anterior branch oI superIicial temporal artery and dissection is carried upto temporal
Iascia. It is to be kept in mind that the lateral expansion oI epicranial aponeurosis separates Irom
temporal Iascia about 2 cm above zygomatic arch to Iorm 2 distinct layers with loose areoler
tissue and Iat in between. II incision is placed too low, one may enter this space and get
obstructed at zygomatic arch and unable to go deep to it. II incision is placed too Iar posteriorly,
the extrinsic muscles oI ear arising Irom superIicial layer may be erroneously identiIied as
temporal muscles.
(b) Crow's Foot incision: Is preIerred in older patients in whom there are well deIined skin
creases, so called 'Crow's Ioot' wrinkles around the outer aspect oI eye. An incision through one
oI these lines about I cm above the outer canthus ensures an almost invisible postoperative scar
(Williams, 1994).
(c) Incision at lateral end of eyebrow - This is the ideal approach in young patients where
incision is given through outer end oI eyebrow. Here incision should not be at right angles to
skin surIace but directed downwards at the same angle as the emerging hairs so as to avoid
transecting the Iollicles which would impair their subsequent growth (Converse, 1974). II the
hair are long and thick, they may be lightly trimmed with scissors but should never be shaved oII
since they provide a valuable guide to alignment during skin closure (Williams, 1994).
{] ZcisioZs for Urbital floor:
In some cases, a pre-existing laceration or scar dictates the site oI incision and these are usually
Iound at the junction oI the thinner and more mobile skin oI the lower eyelid and thicker and
more Iixed skin oI cheek.
Although there is a well deIined skin crease at the level oI inIerior orbital margin, which at 1st
sight might appear suitable Ior placement oI an incision, this should be avoided. The junction oI
the palpebral and circumorbital components oI the orbicularis oculi muscle, the presence oI
orbital septum at the level where it arises Irom the periosteum oI the rim and periorbital Iat
combine to increase the risk oI subsequent scar contracture and a depressed scar leading to
ectropion. A guideline principle is a 'stepped' incision where each layer oI tissue is divided at a
diIIerent level. An incision which transacts all layers at same level should be avoided on Iace to
prevent a tethered and depressed scar.
Fig. 3. The Transconjunctival Approach
(a) Transconjunctival approach: (Fig.3) This oIIers the advantage oI an invisible scar but has a
disadvantage oI restricted access and limited extension. For this, lower eyelid is stabilised with
traction sutures and conjunctiva is elevated with Iixation sutures. Then a small incision is made 3
mm below tarsal plate on medial aspect and in line with punctum. This level oI division is
critical; iI placed too low down near the Iornix, it will be below the Iascia passing Irom inIerior
rectus to the tarsal plate thus allowing escape oI periorbital Iat; iI placed too high, there may be
distortion oI lower eyelid. The periosteum is not incised at orbital rim but 5 mm below the rim. II
it is done at rim, the periorbital Iat herniates through, which interIeres with surgery and is
extremely diIIicult to replace when tissues are closed (Williams, 1994).
(b) Infraorbital approach: It gives an excellent exposure oI entire orbital Iloor and lower part
oI lateral and medial walls. The incision Iollows a line parallel to margin oI lower eyelid but not
too close to Iree edge. There is usually a skin crease 2-3 mm away which provides a convenient
line to Iollow. It is extended laterally and inIeriorly at an angle oI 45 placed in one oI skin
creases Iorming lower limit oI crow's Ioot wrinkles (Williams, 1994).
{] ZcisioZs for Zose: {Fig.]
Fig.4. Diagrammatic arepresentation oI the various methods oI surgical approach Ior
nasoethmoid injuries
(a) Median vertical: A 2-3 cm vertical incision (Stranc, 1970) is made Irom the Iorehead down
to the base oI nose. It reveals Iractures oI nasal skeleton and medial canthal ligament.
(b) H shaped incision: It was Iirst described by Converse and Smith (1962) and later modiIied
by Mustarde (1980) to a curved lateral nasal incision made over anterior lacrimal crest to expose
scructures around medial canthus. It gives excellent exposure oI nasal bridge and canthal
ligaments but inadequate exposure oI Irontal bone.
(c) Bilateral Z approach: The use oI bilateral Z incision anterior to medial canthal area on the
lateral aspect oI nose was described by Dingman et al (1969). But Iurther details are not given.
(d) W shaped approach: A curved transverse incision is made across, the base oI nose within a
skin crease with convexity upwards. It is extended on both sides upwards and laterally just below
the eyebrows (Bowerman, 1975). Supraorbital nerves are to be careIully identiIied and
preserved. It gives an excellent visibility and access to various bone Iragments Ior plating.
(e) Bicoronal approach: In this, the preauricular incisions are extended across the scalp within
the hairline. The soIt tissues are divided down to the subaponeurotic areolar tissue just
superIicial to the pericranium. Flap is raised and reIlected down and Iorwards by dissection
along this plane thus virtually degloving the Iorehead. Its major advantage is cosmetic
acceptance and wide exposure so much so that whole oI the Iacial skeleton can be laid bare
(Williams, 1994). This has been conIirmed byJackson (1989) and Wedgewood (1992).
lg3(a) Payes MarLln
lnclslonlg3(b) 1rlradlaLe lnclslonlg3(c) Conley lnclslon
lg3(d) Macfee lnclslon
{B] Utber iZcisioZs:
(1) Block dissection: McGreger and McGreger (1986) described three types oI incisions Ior this.
1 1he Payes MarLln lnclslon
2 1he LrlradlaLe lnclslon or one of lLs modlfled verslons
3 1he Macee lnclslon
The submandibular part oI the incision as generally practised is common to the Hayes Martin
and the tri-radiate incisions and it is thereIore convenient to discuss it Iirst. Beginning anteriorly
a little beyond the mid-line near the lower border oI the mandibular symphysis it ends well back
on the mastoid area. Between these extremities the incision can either be straight or curved.
Straight, it consists oI two lines meeting in the submandibular at which the two lines meet is also
the point at which any vertical incision in the neck meets them and its precise placing is
determined by the siting oI the vertical incision. Curved, it consists oI a continuous curving line
between the two extremities with its lowest point where it meets any vertical neck incision. The
depth oI the curve can vary as can also the line oI the straight incisions.
There is a horizontal vascular watershed approximetely mid-way between the mandible and the
clavicle (Rogers and Freeland, 1976) and the blood supply oI the submandibular Ilap with the
healing properties which depend on it are not likely to be impaired even iI the submandibular
component oI the incision is considerably lowered. The eIIect is to place the suture line well
below the level oI the carotid biIurcation. It is Irom the vicinity oI the biIurcation that carotid
'blow-out' most oIten occurs the less likely is it to be exposed should postoperative breakdown oI
the wound takes place.
The common submandibular element apart, the three incision types vary signiIicantly.
(a) The Hayes Martin incision: The submandibular component is met by a vertical limb which
below becomes continuous with an inverted Y in the supraclavicular region. (Fig.5a) Four Ilaps
are thus created, the base oI each extending to the limit oI the neck dissection on each side. The
posterior Ilap, with no platysma at its base to signpost the plane in which the Ilap is raised, is
liable to have a less adequate blood supply than the others. It is cartainly the one which becomes
slightly cyanosed most oIten.
The Hayes Martin incision provides best exposure but at the expense oI healing. The point at
which any 3 Ilaps meet has an inherent tendency to breakdown and Hayes Martin has 2 such
sites, upper and lower (Mc Greger and Mc Gregor, 1986).
(b) The tri-radiate incision: This incision used the same submandibular component as the
Hayes Martin incision, either straight or curved, and also uses a vertical incision in the same line
as Hayes Martin, i.e., a little behind the line oI the carotid, but it continues this incision down
over the clavicle 3-4 cm. (Fig.5b) This continuation allows better access to the antero and
postero-inIerior angles oI the dissection once the skin Ilaps are elevated.
Variations oI the tri-radiate incision have been described. It has been suggested that the vertical
limb instead oI being straight should be curved posteriorly (Schobinger, 1957), in order to avoid
lying directly over the carotids. A Iurther alternative is an S-shaped incision (Cramer and CulI
1969), suggested Ior the same reason. Much more worthwhile than either oI these is a variant oI
the posteriorly curving incision, illustrated by Conely (1970), (Fig.5c) in which the posterior
curve and the anterior part oI the submandibular incision are both modiIied to run as a single
curve, beginning in the submental region and ending by running downwards along the anterior
border oI trapezius to the level oI the clavicle. The posterior part oI the submandibular incision
then meets it at aright angle approximately below the lobule oI the ear (Mc Gregor and Mc
Gregor, 1986).
This incision provides same exposure as Hayes Martin but chances oI supraclavicular breakdown
are less.
(c) The MacFee incision (Fig 5d): This incision (MacFee, 1960) diIIers Irom virtually all others
in that it avoids using a vertical limb. Instead, two horizontal incisions are made one in the
submandibular region and one in the supraclavicular region. Between these two incisions a
bipedicled Ilap is raised, based anteriorly on the mid-line and posteriorly on the anterior border
oI trapezius. Through this exposure the neck dissection, otherwise standard, is carried out. The
Ilap is retracted upwards to expose the lower part oI the neck until dissection has proceeded Iar
enough upwards to allow the resection specimen to be pulled through into the submandibular
incision.
This incision is said to give better cosmetic results by avoiding a vertical scar in the neck, but it
is not strictly accurate. Cosmesis is related more to loss oI neck symmetry, the result oI tissues
removed and shoulder droop (McGregor and McGregor, 1986).
(2) Exposure of salivary glands:
(a) Parotid gland: For parotidectomy, incision is made anterior to tragus, passing inIeriorly
around the lobule and thereaIter curving posteriorly below the lobule and passing downwards
and anteriorly along the angle oI mandible. The incision can be extended superiorly or inIeriorly,
iI Iurther exposure is needed to the skull base or neck respectively (Myers and Suen, 1996).
(b) Submandibular gland: It may be exposed by submandibular approach discussed vide supra.
(3) Tracheostomy: It is usually an emergency surgery and a low tracheostomy is perIormed i.e.
below the thyroid isthmus. There may be 2 incisions :
(a) Midline vertical incision: It is placed Irom the upper border oI cricoid cartilage downwards
Ior one and a halI to two inches. It gives a better access and can be extended in space oI burns to
ligate jugular venous arch.
(b) Transverse incision: It is made in the lines oI skin Iolding at 2nd-3rd tracheal ring. Isthmus
oI thyroid can be retracted up or ligated and cut in centre to reach the trachea (Sicher and Dubrul,
1996).
(4) Thyroidectomy : A curved incision is made one inch above the medial ends oI 2 clavicles
with convexity downwards and extending Irom lateral border oI one sternocleidomastoid to that
oI the other. This Ialls in natural skin creases oI neck and the scar is hidden. Platysma is divided
at higher level than skin to produce a Iine scar. Anterior jugular veins may need ligation and
division (Das, 1985).
ummary aZd CoZclusioZs
To summarise, in general, the surgical incisions are always based upon anatomical landmarks
and Iacts, to protect certain important structures, keeping in mind the cosmetic eIIects. This is
even more important in Iace region Ior obvious reasons. So a thorough knowledge oI anatomy oI
the region is a must, beIore surgery is attempted. This article is an endeavor to classiIy and
discuss various, incisions in the 'Head and Neck' region along with the anatomical guidlines on
which these are based.
Vous aimerez peut-être aussi
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- New Mcgraw Hill EducationDocument132 pagesNew Mcgraw Hill EducationAlexandru LeșanPas encore d'évaluation
- Poverty Is General Scarcity or The State of One Who Lacks A Certain Amount of Material Possessions or MoneyDocument41 pagesPoverty Is General Scarcity or The State of One Who Lacks A Certain Amount of Material Possessions or MoneyChristian Cañon GenterolaPas encore d'évaluation
- Urethral Trauma: Sub Bagian Urologi Bagian / SMF Bedah FK Uns/Rsud Dr. MoewardiDocument19 pagesUrethral Trauma: Sub Bagian Urologi Bagian / SMF Bedah FK Uns/Rsud Dr. MoewardiAtika SugiartoPas encore d'évaluation
- Nordic Business Forum 2023 ExecutiveSummaryDocument71 pagesNordic Business Forum 2023 ExecutiveSummaryveda.norwayPas encore d'évaluation
- MDWF 1030 Carter Plugged Duct Mastitis Abscess PGDocument5 pagesMDWF 1030 Carter Plugged Duct Mastitis Abscess PGapi-366292665Pas encore d'évaluation
- Flashcards About Medical DefinitionsDocument62 pagesFlashcards About Medical DefinitionsSrikanth PagidiPas encore d'évaluation
- The Tactical Combat Casualty Care Casualty Card - TCCC Guidelines - Proposed Change 1301Document9 pagesThe Tactical Combat Casualty Care Casualty Card - TCCC Guidelines - Proposed Change 1301Paschalis DevranisPas encore d'évaluation
- Tarea Nâ°1.es - en Derecho Civil Legalmente RubiaDocument5 pagesTarea Nâ°1.es - en Derecho Civil Legalmente RubiaMax Alva SolisPas encore d'évaluation
- Chest Drains Al-WPS OfficeDocument16 pagesChest Drains Al-WPS OfficeisnainiviaPas encore d'évaluation
- Tetanus Treatment: Vitria DwiayuDocument12 pagesTetanus Treatment: Vitria DwiayuvitriaPas encore d'évaluation
- 12 Compulsive Activities ChecklistDocument8 pages12 Compulsive Activities ChecklistShrey BadrukaPas encore d'évaluation
- Thesis On Food Security PDFDocument8 pagesThesis On Food Security PDFbsrf4d9d100% (2)
- PI - Standard - Seafood Processing - Issue 5.0 - 1-February-2019Document65 pagesPI - Standard - Seafood Processing - Issue 5.0 - 1-February-2019pebru yuwono0% (1)
- Attending Physicians Statement - Form CDocument1 pageAttending Physicians Statement - Form CPritam sarkarPas encore d'évaluation
- Diabetes: Physical Activity and ExerciseDocument2 pagesDiabetes: Physical Activity and ExerciseZobaida Khatun JuliePas encore d'évaluation
- Hospital Supply Chain ManagementDocument39 pagesHospital Supply Chain ManagementFatima Naz0% (1)
- The X Factor 11Document31 pagesThe X Factor 11writerguy78Pas encore d'évaluation
- Blue Modern Medical Center Z-Fold BrochureDocument2 pagesBlue Modern Medical Center Z-Fold BrochureAngela Shaine CruzPas encore d'évaluation
- Conflict or Consensus - An Investigation of Stakeholder Concerns DuringDocument10 pagesConflict or Consensus - An Investigation of Stakeholder Concerns DuringhohoexePas encore d'évaluation
- Magnetis Polus AmboDocument4 pagesMagnetis Polus Amboadi.mititean1585Pas encore d'évaluation
- Summary of Non Sexist CityDocument2 pagesSummary of Non Sexist CityIMY KARDAS100% (3)
- VtM2nded1 Page PDFDocument1 pageVtM2nded1 Page PDFJoseph CortesPas encore d'évaluation
- Recruit HandbookDocument72 pagesRecruit HandbookJUAN RAMON0% (1)
- American Well - Case StudyDocument13 pagesAmerican Well - Case StudySumitPas encore d'évaluation
- Masha Sardari Nutrition ResumeDocument2 pagesMasha Sardari Nutrition Resumeapi-428097674Pas encore d'évaluation
- Rules For Non Medical BusinessDocument1 pageRules For Non Medical BusinessAbhijit AminpurPas encore d'évaluation
- GP 9.7 Brochure 6 5 20 PDFDocument16 pagesGP 9.7 Brochure 6 5 20 PDFDaisy FloresPas encore d'évaluation
- Republic Act No. 11210 - 105-Day Expanded Maternity Leave LawDocument4 pagesRepublic Act No. 11210 - 105-Day Expanded Maternity Leave LawRaymond CruzinPas encore d'évaluation
- Risk Factors of Internet Addiction Among AdolescentsDocument14 pagesRisk Factors of Internet Addiction Among AdolescentsM. F. MubinPas encore d'évaluation
- Thesis Dental ImplantsDocument4 pagesThesis Dental Implantstmexyhikd100% (2)