Académique Documents
Professionnel Documents
Culture Documents
The Natural History of Asthma and Early Intervention 2002
Transféré par
Olga CirsteaDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
The Natural History of Asthma and Early Intervention 2002
Transféré par
Olga CirsteaDroits d'auteur :
Formats disponibles
The natural history of asthma and early intervention
Stanley J. Szefler, MD Denver, Colo
The understanding of the natural history of asthma has changed significantly during the last 4 decades, with the view that asthma is a disease of chronic inflammation and varying degrees of severity replacing that of it being a disease of reversible airway obstruction. Treatment has progressed in accordance with the growing knowledge about the pathophysiologic mechanisms of asthma. Nevertheless, much remains unknown, especially about how to treat asthma effectively. Pharmacogenetics, an emerging field in which the knowledge of the genetic basis of a disease is applied to its treatment, may ultimately lead investigators to define many unanswered questions about asthma therapy. Asthma occurs early in childhood, but the ideal time for intervention and the most effective treatment strategy are yet unknown for young patients. The lack of response to a therapy may indicate the course of the disease as much as a lack of treatment efficacy. It may be that including such variables as airway hyperresponsiveness in treatment goals will not only become routine but will result in improved long-term asthma treatment as well. The progress in defining asthma and targeting treatment toward specific pathophysiologic mechanisms should lead to better-defined optimal strategies for treating asthma in children. (J Allergy Clin Immunol 2002;109:S549-53.) Key words: Asthma, natural history, inflammation, early intervention
Abbreviations used BHR: Bronchial hyperresponsiveness ECP: Eosinophilic cationic protein ICS: Inhaled corticosteroid(s) LT: Leukotriene LTRA: Leukotriene receptor antagonist
The understanding of the pathophysiology of asthma has evolved significantly during the last 4 decades, and treatments have progressed in accordance with the growing knowledge about the natural history of the disease. In the 1960s, asthma was perceived to be an episodic disease, and the therapeutic objectives were to relieve symptoms, primarily bronchospasm. Epinephrine partly achieved this goal, and efforts ensued to develop an oral formulation of this drug and to prolong its duration of action.
From the Department of Pediatrics, National Jewish Medical and Research Center, Denver, Colo, and the Department of Pediatrics and Pharmacology, University of Colorado Health Sciences Center, Denver, Colo. Dr Szefler is the Helen Wohlberg and Helman Lambert Chair in Pharmacokinetics/Divisions of Clinical Pharmacology and Allergy and Immunology. Supported in part by National Institutes of Health grants HL-36577 and HD37237 and General Clinical Research Center Grant 5M01-RR00051 from the Division of Research Resources. Dr Szefler serves on pedatric advisory panels for childhood asthma for Merck, AstraZeneca, and GlaxoSmithKline. Reprint requests: Stanley J. Szefler, MD, Division of Clinical Pharmacology, National Jewish Medical and Research Center, 1400 Jackson St, Room J209, Denver, CO 80206. 2002 Mosby, Inc. All rights reserved. 0091-6749/2002 $35.00 + 0 1/0/124569 doi.10.1067/mai.2002.124569
During the next 2 decades, concerns shifted toward the progression of the disease and how its evolution could be managed. In the 1970s, when medications such as albuterol and theophylline were in use, the emphasis of asthma treatment was bronchospasm prevention rather than simply the relief of symptoms. The introduction of theophylline resulted in improved control of nocturnal asthma, and in the 1980s, cromolyn sodium was used to control allergen-induced bronchospasm during the early and late phases of asthma. Then, in the 1990s, bronchoscopy and endobronchial biopsy specimens revealed inflammation in the airways of asthmatics. The definition of asthma changed from being a reversible disease of airway obstruction to that of a chronic inflammatory disease with varying degrees of severity. Researchers focused attention on the cellular and molecular mechanisms of the disease (such as cytokines, chemokines, and leukotrienes, immune response, remodeling, and inflammation) and how these factors may predict the severity or progression of the disease. Figure 1 summarizes the evolution of asthma as it has been viewed since the late 1990s. The development, refinement, and increased use of assessment tools including bronchoscopy, endobronchial biopsy, bronchoalveolar lavage, and induced sputum were instrumental in quantifying and qualifying inflammation in asthmatic patients. Inhaled glucocorticoids became the agents of choice to prevent and resolve airway inflammation in adults and older children.1 Although steroids were used extensively, a new class of drugs, the leukotriene (LT) modifiers, was being developed. The LT modifiers targeted the cysteinyl LT mediators present in asthma inflammation that are not necessarily or consistently controlled by corticosteroids. Leukotrienes are associated with airway edema, smooth muscle contraction, and altered cellular activity in the inflammatory process. The LT modifiers were designed either to inhibit LT synthesis (5-lipoxygenase inhibitor) or to prevent the LTs from binding to their specific receptors on airways and inflammatory cells. In 1995, two medications of this new class of drugs, zileuton (Zyflo; Abbott Laboratories, North Chicago, Ill), an LT synthesis inhibitor, and zafirlukast (Accolate;
S549
S550 Szefler
J ALLERGY CLIN IMMUNOL JUNE 2002
FIG 1. Natural history of asthma. Schematic of the natural history of asthma demonstrates several possible features of the disease that may be amenable to preventive or therapeutic intervention. (From Holgate ST. The cellular and mediator basis of asthma in relation to natural history. Lancet 1997;350(Suppl 2):5-9. by The Lancet Ltd, 1997.)
AstraZeneca Pharmaceuticals, Wilmington, Del), a leukotriene receptor antagonist (LTRA), were approved for the treatment of asthma in the United States. Another LTRA, montelukast sodium (Singulair; Merck & Company, Inc, West Point, Pa), subsequently received FDA approval in 1998. Approved for adults, only two of these medications are approved for young children: zafirlukast, for children as young as 5 years of age, and montelukast, for children as young as 2 years of age. Although first met with skepticism, the LT modifiers have been incorporated rapidly into the physicians armamentarium for asthma treatment.
DISCERNING THE STATUS OF THE DISEASE
An understanding of the natural history of asthma can contribute substantially to optimal, early treatment. With chronic inflammation, there is an element of progression, but asthma progression has not been defined clearly. The only indication in the literature regarding progression is a decline in FEV1. Other factors, such as intensifying frequency or severity of symptoms, increasing the need for medication to control symptoms and hyperexpansion, may also be important indicators of disease progression. In the past, clinicians used pulmonary function testing primarily to gauge the severity of a patients asthma and to monitor response to therapy. Several questions remain, however, regarding how best to use the pulmonary function tests. Among these questions are: Does spirometry provide information that peak flow does not? Which patients might benefit from the measuring of lung volume and hyperexpansion (with body plethysmography)? The answers may not always be complete enough to provide a full appreciation of the disease for a particular patient. It may also be important, therefore, to evaluate patients
using exercise-induced asthma or methacholine challenge, particularly in those who participate in sports or for whom regular participation in exercise is important. In recent years, measurements for markers of inflammation have become more accessible. These new tools include induced sputum cytology to assess the presence of inflammatory cells in the lungs (eosinophils, neutrophils, and others), and blood tests to determine levels and activation states of inflammatory cells (mainly eosinophils), along with the presence of inflammatory markers such as the eosinophilic cationic protein (ECP). Other measurements are used only in research settings, such as the level of exhaled nitric oxide as a marker of inflammation. New techniques are being developed to measure other mediators. There are, however, no parameters that relate findings of such measurements to a risk profile. Defining the clinical relevance of measurements would allow them to be incorporated into routine practice. Similarly, the best methods for measuring the response to asthma treatment remain unclear. It is not known which indicators are best: the control of symptoms, FEV1, airway hyperresponsiveness, the level of exhaled mediators such as nitric oxide, or a combination of these markers. Regulatory agencies need to address questions raised regarding the application of surrogate markers in terms of which are suitable as short-term markers and which indicate long-term response.
DEFINING A GENETIC BASIS FOR ASTHMA AND APPLYING IT TO TREATMENT
Atopy is the single most important risk factor for asthma2 and, in genetically predisposed patients, environmental stimuli produce inflammation and ultimately can affect airway structure. Pharmacogenetics is an emerging
J ALLERGY CLIN IMMUNOL VOLUME 109, NUMBER 6
Szefler S551
field that may help to incorporate several different treatment aspects (for old therapies and new therapies in development) into a schematic such as drug response (at a cellular receptor level), drug metabolism, and risk for adverse effects of medications. Research has focused on identifying the genes associated with asthma, which would allow for the recognition of patients at risk and for more proactive management, prevention, and selection of therapeutic options. Distinguishing genetic markers for asthma from those for allergy is a challenging task; however, several candidate genes and their functions have been identified.2
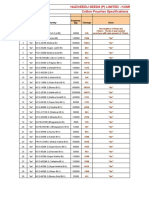
TABLE I. Differences based on patterns of symptoms 1. NAEPP guidelines: mild intermittent, mild persistent, moderate persistent and severe persistent 2. Persistent asthma, obstructed asthma, episodic asthma, asthma in remission, potential asthma, trivial asthma* 3. Cough-variant asthma 4. Asthmatic bronchitis 5. Brittle asthma: chaotic or sudden-onset 6. Potentially fatal asthma
*Adapted from data in Barnes and Woolcock.4
RECOGNIZING INDIVIDUAL DIFFERENCES IN ASTHMA
Asthma is heterogeneous. Elucidation and examination of the variables in asthma could add valuable diagnostic and treatment information. The National Asthma Education and Prevention Program (NAEPP) guidelines provide a limited classification of asthma as mild intermittent, mild persistent, moderate persistent, and severe persistent. By adding other categories, more epidemiologic information could be retrieved (Table I).3,4 The differences among patients with asthma also present other important implications. For example, specific and distinguishing differences occurring during the course of the disease may alter the initial prognosis, and additional information regarding these variables might better define risk features. Patients responses to therapy vary, however, and the impact of such variance is unknown. A key question, then, is do these distinctions reflect varying modifications of a common pathophysiologic process or varying processes?
CHILDHOOD ASTHMA: CURRENT KNOWLEDGE AND ISSUES
Asthma often occurs in early childhood. Because the incidence of asthma in children younger than 5 years of age is the highest compared with that of older children and adults, it is important to identify the disease in these very young patients.5 Owing to the growing understanding of the natural history of asthma, treatment can be targeted toward specific pathophysiologic mechanisms that can lead to better defined optimal strategies for treating asthma in children. Current asthma therapy is based on the concept that chronic inflammation is a key feature of the disease; however, there is neither enough information about the time of onset of inflammation nor precise mechanisms for asthma initiation, progression, and persistence, especially in children. Although asthma often starts early in life, wheezing resolves by 6 years of age in many children. Among 277 children with wheezing before the age of 3 years, 164 (59.2%) had not wheezed during the previous year when examined at 6 years of age. Children with persistent wheezing were twice as likely to have wheezed often or very often (P = .001) or to have wheezed without colds during infancy (P = .05), compared with children who
have transient early wheezing. Although children with persistent wheezing at 6 years of age had significantly reduced pulmonary function, compared with nonwheezers at 6 years (1069.7 vs 1262.1 mL/s, respectively, P < .01). When younger than 1 year of age, they had a pulmonary function similar to the children who never wheezed at age 6 (104.6 vs 123.3 mL/s, respectively). These data suggest that in these children, the persistent wheezing is not caused by poor initial pulmonary function but instead may be the result of the chronic disease process in the bronchi.6 Furthermore, certain patients with bronchial hyperresponsiveness (BHR) were more predisposed to a decline in pulmonary function over time.7 This has led to speculation that if BHR occurs early in children, their lung development may be compromised and could be at risk for more rapid decline and chronic obstructive pulmonary disease. If so, one would expect patients with severe asthma to have a decline in pulmonary function continuously over time, but data from long-term studies do not support that hypothesis.8 Certainly, patients with severe asthma have diminished pulmonary function and airway hyperresponsiveness. What is not clear is whether such deficits in pulmonary function occur suddenly and then continue or whether there is a window of opportunity for intervention. Including the reduction of airway hyperresponsiveness in treatment goals might result in more effective control of asthma, fewer exacerbations, less variable airflow obstruction, and a more effective decrease of airway inflammation and remodeling compared with the use of conventional measures. Data showing the degree of BHR in asthma have provided relevant information on the exacerbation rate, which appeared to be highest in patients with relatively severe BHR.9 These data also suggested that a step-up of doses of inhaled corticosteroid (ICS) therapy could be tailored more easily to the needs of each individual according to the severity of BHR. Including the BHR reduction in the therapeutic goals allowed for a reduced exacerbation rate, an increased FEV1 (bronchodilation) and a decreased thickness of the subepithelial reticular layer (decrease in collagen, a surrogate marker for airway remodeling) in the bronchial wall, indicating a reversal of airway remodeling. The drawback to including BHR reduction in the treatment goal results, however, is an approximate dou-
S552 Szefler
J ALLERGY CLIN IMMUNOL JUNE 2002
FIG 2. Daily doses of inhaled steroids. Actual daily doses of ICS (g: mean SEM) according to the AHR strategy and the reference strategy. AHR strategy necessitated the use of higher mean doses than did the reference strategy throughout the 2-year study. Median difference in treatment and ICS was 400 g during the 2-year follow-up. Treatment requirement decreased with both strategies; however, the decrease with the AHR strategy was somewhat greater than with the reference strategy. (From Sont JK, Willems LN, Bell EH, et al. Clinical control and histopathologic outcome of asthma when using airway hyperresponsiveness as an additional guide to long-term treatment in the AMPUL Study Group. Am J Respir Crit Care Med 1999;159:1043-51. With permission.)
Image available in print only
FIG 3. Variability of response to asthma therapy. The response distribution according to FEV1 shows a bellshaped curve for both montelukast and beclomethasone and indicates that there may be a spectrum of response, at least as measured by FEV1 to drug therapy for asthma. In this study, all patients benefited from mandatory use of spacers, enforced compliance, and the rigorous monitoring of patients. Black bars, Patients receiving 10 mg/d montelukast; white bars, patients receiving inhaled 200 g beclomethasone twice daily. (From Malmstrom K, Rodriguez-Gomez G, Guerra J, et al. Oral montelukast, inhaled beclomethasone and placebo for Montelukast/Beclomethasone Study Group. Ann Intern Med 1999;130:487-95. With permission.)
bling of the ICS dose9 (Fig 2) and the consequent risk of adverse effects. Further study may define better the clinical use of this approach, particularly in children. It may be that earlier intervention negates the need for increased doses of ICS.
The suggestion that the measurement of BHR be included in the long-term treatment of asthma highlights the fact that an adequate response to therapy has not been defined clearly. Studies tend to focus on the average response, often neglecting important aspects, including
J ALLERGY CLIN IMMUNOL VOLUME 109, NUMBER 6
Szefler S553
the variability of each patients response to treatment. Response to montelukast, similar to that for beclomethasone, demonstrated a bell-shaped curve relative to change in FEV1 from baseline10 (Fig 3). Indeed, one population of patients appears to respond very favorably (change of FEV1 20%), whereas another population does not appear to respond at all (change of FEV1 10%). Such variability calls into question whether there are responders and nonresponders to therapy. Poor response to therapy may reflect changes in the course of the disease rather than a lack of treatment efficacy, however. Another important aspect of these responses is the treatment failure rate between various agents. Montelukast and beclomethasone did not differ significantly in reducing asthma attacks (failure rate = 86.7% and 90%, respectively, after 12 weeks)10; these results were different, however, from the Asthma Clinical Research Network study, in which triamcinolone was significantly more effective than salmeterol (treatment failure = 6% and 24%, respectively, after 18 weeks).11
asthma control but also that inhaled steroids had a very limited effect on pulmonary function. Similar studies are needed for other long-term control therapy options.12
CONCLUSIONS
At the threshold of being able to define treatment strategies for childhood asthma, several unique opportunities exist. Significant challenges accompany these opportunities, however. The importance of surrogate markers raises questions that regulatory agencies need to answer in terms of which are suitable as short-term markers and which will be indicators of long-term response. Pharmacogenetics is an emerging field that may help to incorporate several different treatment aspects as well as develop new therapies; however, one downside to using genetic information for preventing asthma or to implement early intervention strategies is its expense. The goals of recognition and intervention, as well as the ability to monitor the progress of asthma, are well within sight. The foundation for such progress must be to focus on improving asthma treatment.
REFERENCES 1. Global Initiatives for Asthma (GINA). (Revised 1998.) Pocket guide for asthma management and prevention. Bethesda, Md: US Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute; November 1998. NIH Publication No. 96-3659B. 2. Holgate ST. The cellular and mediator basis of asthma in relation to natural history. Lancet 1997;350(Suppl 2):5-9. 3. NAEPP. National Asthma Education and Prevention Program. Expert Panel Report 2: Clinical practice guidelines. Guidelines for the diagnosis and management of asthma. Rockville, Md: US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Heart, Lung, and Blood Institute; 1997. NIH Publication No. 98-4051. 4. Barnes PJ, Woolcock AJ. Difficult asthma. Eur Respir J 1998;12:1209-18. 5. Yunginger JW, Reed CE, OConnell EJ, Melton LJ III, OFallon WM, Silverstein MD. A community-based study of the epidemiology of asthma. Incidence rates, 1964-1983. Am Rev Respir Dis 1992;146:888-94. 6. Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. Asthma and wheezing in the first six years of life: The Group Health Medical Associates. N Engl J Med 1995;332:133-8. 7. Weiss ST. Early life predictors of adult chronic obstructive lung disease. Eur Respir Rev 1995;31:303-9. 8. Oswald H, Phelan PD, Lanigan A, Hibbert M, Carlin JB, Bowers G, et al. Childhood asthma and lung function in mid-adult life. Pediatr Pulmonol 1997;23:14-20. 9. Sont JK, Willems LN, Bell EH, van Krieken JH, Vanderbroucke JP, Sterk PJ. Clinical control and histopathologic outcome of asthma when using airway hyperresponsiveness as an additional guide to long-term treatment: The AMPUL Study Group. Am J Respir Crit Care Med 1999;159:1043-51. 10. Malmstrom K, Rodriquez-Gomez G, Guerra J, Villaran C, Pineiro A, Wei LX, et al. Oral montelukast, inhaled beclomethasone and placebo for Montelukast/Beclomethasone Study Group. Ann Intern Med 1999;130:487-95. 11. Lazarus SC, Boushey HA, Fahy JV, Chinchilli VM, Lemanske RF Jr, Sorkness CA, et al. Asthma Clinical Research Network for the National Heart, Lung, and Blood Institute: long-acting beta2-agonist monotherapy vs continued therapy with inhaled corticosteroids in patients with persistent asthma: a randomized controlled trial. JAMA 2001;285:2583-93. 12. The Childhood Asthma Management Program Research Group. Longterm effects of budesonide or nedocromil in children with asthma. N Engl J Med 2000;343:1054-63.
KEY QUESTIONS
Despite the progress in understanding the evolution of asthma, several key questions remain to be answered concerning its pathophysiologic mechanisms. When does inflammation begin? What is the most appropriate early intervention for children? When does wheezing become asthma? These questions engender many more important decision-making discussions, such as those concerning when a diagnosis of asthma is made and when and to whom a referral is made. The benefits and risks of all long-term medications should be evaluated. Much remains poorly defined in this area. The minimally effective and maximally safe doses of ICS need to be determined, as well as measurements of response, whether they be BHR or markers of inflammation. If the most efficacious dose is higher than the one being used, adverse effects must be addressed. Ultimately, patients who do not respond to a therapy may provide important information about resistance to ICS or about the severity of the disease. It is also necessary to rethink delivery devices. The criteria used for initiating and continuing treatment needs to be defined, as do the benefits and risks of early treatment. Patients at risk for adverse effects of medications should be identified. Integral to pharmacotherapy is patient adherence, for which measurement tools and methods for improvement are needed. Data from the recently completed Childhood Asthma Management Program (CAMP) illustrate a profile of performance for 2 different treatments. Interpretation of CAMP data, as well as information from other ongoing studies, will help define a preferred medication for early intervention in children. The results of this study provided an excellent profile for 3 treatment strategies. The study clearly demonstrated that inhaled steroids could markedly reduce the rate of significant asthma episodes and overall
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Batman Animated (1998) (Scan) (Stacalkas)Document169 pagesBatman Animated (1998) (Scan) (Stacalkas)João Gabriel Zó100% (11)
- Test Bank For Cognitive Psychology Connecting Mind Research and Everyday Experience 3rd Edition e Bruce GoldsteinDocument24 pagesTest Bank For Cognitive Psychology Connecting Mind Research and Everyday Experience 3rd Edition e Bruce GoldsteinMichaelThomasyqdi100% (49)
- Boylestad Circan 3ce Ch02Document18 pagesBoylestad Circan 3ce Ch02sherry mughalPas encore d'évaluation
- Odisha Block Summary - NUAGAONDocument8 pagesOdisha Block Summary - NUAGAONRohith B.NPas encore d'évaluation
- Bimetallic ZN and HF On Silica Catalysts For The Conversion of Ethanol To 1,3-ButadieneDocument10 pagesBimetallic ZN and HF On Silica Catalysts For The Conversion of Ethanol To 1,3-ButadieneTalitha AdhyaksantiPas encore d'évaluation
- Civil and Environmental EngineeringDocument510 pagesCivil and Environmental EngineeringAhmed KaleemuddinPas encore d'évaluation
- Syllabus For Final Examination, Class 9Document5 pagesSyllabus For Final Examination, Class 9shubham guptaPas encore d'évaluation
- Peptic UlcerDocument48 pagesPeptic Ulcerscribd225Pas encore d'évaluation
- Cotton Pouches SpecificationsDocument2 pagesCotton Pouches SpecificationspunnareddytPas encore d'évaluation
- 12-Zoomlion 70t Crawler Crane Specs - v2.4Document2 pages12-Zoomlion 70t Crawler Crane Specs - v2.4Athul BabuPas encore d'évaluation
- Horgolás Minta - PulcsiDocument5 pagesHorgolás Minta - PulcsiCagey Ice-RoyPas encore d'évaluation
- A Comparison of Practitioner and Student WritingDocument28 pagesA Comparison of Practitioner and Student WritingMichael Sniper WuPas encore d'évaluation
- Grammar: English - Form 3Document39 pagesGrammar: English - Form 3bellbeh1988Pas encore d'évaluation
- Lyndhurst OPRA Request FormDocument4 pagesLyndhurst OPRA Request FormThe Citizens CampaignPas encore d'évaluation
- Especificação - PneusDocument10 pagesEspecificação - Pneusmarcos eduPas encore d'évaluation
- Solution Document For Link LoadBalancerDocument10 pagesSolution Document For Link LoadBalanceraralPas encore d'évaluation
- Bio Lab Report GerminationDocument10 pagesBio Lab Report GerminationOli Damaskova100% (4)
- Vocabulary Inglés.Document14 pagesVocabulary Inglés.Psicoguía LatacungaPas encore d'évaluation
- Thick Teak PVT LTD Aoa and MoaDocument17 pagesThick Teak PVT LTD Aoa and MoaVj EnthiranPas encore d'évaluation
- Accountancy Service Requirements of Micro, Small, and Medium Enterprises in The PhilippinesDocument10 pagesAccountancy Service Requirements of Micro, Small, and Medium Enterprises in The PhilippinesJEROME ORILLOSAPas encore d'évaluation
- E-Governance Horizon Report 2007 PDFDocument240 pagesE-Governance Horizon Report 2007 PDFtouhedurPas encore d'évaluation
- Garden Club of Virginia RestorationsDocument1 pageGarden Club of Virginia RestorationsGarden Club of VirginiaPas encore d'évaluation
- Title: Daily Visit Report: SDL Mini - Project Academic Year 2020-21 Group ID:GB6Document2 pagesTitle: Daily Visit Report: SDL Mini - Project Academic Year 2020-21 Group ID:GB6Arjuna JppPas encore d'évaluation
- Techniques of Demand ForecastingDocument6 pagesTechniques of Demand Forecastingrealguy789Pas encore d'évaluation
- Detailed Award Sheet Government College University, FaisalabadDocument1 pageDetailed Award Sheet Government College University, FaisalabadAnayat KhetranPas encore d'évaluation
- Laws and Policies of Fertilizers SectorDocument12 pagesLaws and Policies of Fertilizers Sectorqry01327Pas encore d'évaluation
- ZultaniteDocument4 pagesZultaniteAcharya BalwantPas encore d'évaluation
- Comparing Effect of Adding LDPE, PP, PMMA On The Mechanical Properties of Polystyrene (PS)Document12 pagesComparing Effect of Adding LDPE, PP, PMMA On The Mechanical Properties of Polystyrene (PS)Jawad K. OleiwiPas encore d'évaluation
- ViTrox 20230728 HLIBDocument4 pagesViTrox 20230728 HLIBkim heePas encore d'évaluation
- X-Roc Latex: Product DescriptionDocument2 pagesX-Roc Latex: Product DescriptionAmr RagabPas encore d'évaluation