Académique Documents
Professionnel Documents
Culture Documents
Stroke Note
Transféré par
api-118818524Description originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Stroke Note
Transféré par
api-118818524Droits d'auteur :
Formats disponibles
Stroke Note
Published online: December 1, 2011
Cerebrovasc Dis 2011;32:614615 DOI: 10.1159/000334578
Fatal Intracerebral Hemorrhage Associated with Administration of Recombinant Tissue Plasminogen Activator in a Stroke Patient on Treatment with Dabigatran
Ignacio Casado Naranjo, Juan Carlos Portilla-Cuenca, Pedro Enrique Jimnez Caballero, Maria Luisa Calle Escobar, Ral Mauricio Romero Sevilla Department of Neurology, Stroke Unit, Hospital San Pedro de Alcntara, Cceres, Spain
Dabigatran is an oral anticoagulant that has been recently approved in Europe for prevention of stroke in patients with nonvalvular atrial fibrillation (NVAF), demonstrated to be equally safe or safer or at least as effective as warfarin [1]. In selected patients, we have the opportunity of thrombolysis treatment within 4.5 h after onset of ischemic stroke (IS) [2, 3] in order to minimize the risk of bleeding complications. Concomitant use of anticoagulants is a contraindication for administration of recombinant tissue plasminogen activator (rtPA) even if the international normalized ratio is !1.7 [4]. There is little information on bleeding risk in patients treated with rtPA while taking dabigatran [5, 6].
We report a 62-year-old diabetic man who underwent electric cardioversion for NVAF detected 2 months previously, who refused to take acenocoumarol and who was pretreated only with enoxaparin for 1 month. After the procedure, he was treated with dabigatran 110 mg twice daily, as an off-label situation. Three hours after taking the third dose, he had an abrupt onset of aphasia and right hemiplegia. The National Institutes of Health Stroke Scale score was 18. A non-contrast head computed tomography (CT) scan was normal. Perfusion CT revealed a deficit of 12/3 of the left middle cerebral artery area (fig.1a). His blood pressure was 142/78 mm Hg and his glycemic level was 233 mg/dl. Coagulation parameters were: platelet count 154 ! 109/l (normal range 150450), prothrombin time 14.6 s (normal range 814), international normalized ratio 1.29 (normal range 0.71.5), activated partial thromboplastin time 37.1 s (normal range 2438) and fibrinogen level 293 mg/dl (normal range 200450). After obtaining informed consent, thrombolysis was initiated at 190 min from stroke onset. The neurological status did not change. Twelve hours later, the patient became drowsy and fell into a coma shortly thereafter. A CT brain scan showed a lobar hemorrhage with mass effect (fig. 1b). Control coagulation parameters were normal. The patient was intubated and transferred to an intensive care unit where he died 2 days later. To the best of our knowledge, this is the first report to describe a fatal bleeding complication in a patient treated with dabigatran who had an IS and was treated with intravenous rtPA.
Fig. 1. a Perfusion CT of the brain. b CT
scan 12 h after rtPA perfusion.
2011 S. Karger AG, Basel 10159770/11/03260614$38.00/0 Fax +41 61 306 12 34 E-Mail karger@karger.ch www.karger.com Accessible online at: www.karger.com/ced
Color version available online
Table 1. Main clinical characteristics of patients reported
Study De Smedt et al. [5] Matute et al. [6] Present study
Age years/sex 46/F 76/F 62/M
Dabigatran dose, mg NA 220 o.i.d. 110 b.i.d.
Last dose PT, s h 7 15 3 NA 11.4 14.6
aPTT, s 34.8 30.6 37.1
INR 1.2 1 1.29
NIHSS 19 4 18
rtPA time onset, min
Outcome
just below 270 improvement (12) 120 asymptomatic (0) 190 death
Figures in parentheses are National Institutes of Health Stroke Scale scores. PT = Prothrombin time; aPTT = activated partial thromboplastin time; INR = international normalized ratio; NA = not available; o.i.d. = one per day; b.i.d. = twice daily.
After regulatory approval, more patients with NVAF will be treated with dabigatran and some of them will developed an IS, forcing the clinician to decide whether to treat these cases with rtPA or not, or use a lower dose of the drug [7]. Including ours, only 3 diverse cases have been reported so that it is difficult to draw any conclusions (table1). It is possible that a shorter time interval between the last dabigatran dose and rtPA administration may be a critical factor in the increased risk of bleeding, considering the pharmacological characteristics of the drug. Secondary intracerebral hemorrhage might have occurred even without rtPA or dabigatran use, due to large perfusion deficit or diabetes [8]. Our case warrants caution when deciding on the administration of rtPA in patients treated with dabigatran who have an IS. Disclosure Statement The authors state that there are no conflicts of interest. References
1 Rother J, Crijns H: Prevention of stroke in patients with atrial fibrillation: the role of new antiarrhythmic and antithrombotic drugs. Cerebrovasc Dis 2010;30:314322. 2 Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, Schneider D, von Kummer R, Wahlgren N, Toni D: Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008; 359:13171329.
3 Wahlgren N, Ahmed N, Davalos A, Hacke W, Millan M, Muir K, O Roine R, Toni D, Lees KR, SITS investigators: Thrombolysis with alteplase 34.5 h after acute ischemic stroke: an observational study. Lancet 2008;372:13031309. 4 Prabhakaran S, Rivolta J, Vieira JR, Rincon F, Stillman J, Marshall RS, Chong JY: Symptomatic intracerebral hemorrhage among eligible warfarin-treated patients receiving intravenous tissue plasminogen activator for acute ischemic stroke. Arch Neurol 2010; 67:559563. 5 De Smedt A, De Raedt S, Nieboer K, De Keyser J, Brouns R: Intravenous thrombolysis with recombinant tissue plasminogen activator in a stroke patient treated with dabigatran. Cerebrovasc Dis 2010; 30: 533 534. 6 Matute MC, Guilln M, Garcia-Caldentey J, Buisan J, Aparicio M, MasJuan J, Alonso de Leciana M: Thrombolysis for acute ischaemic stroke in a patient on treatment with dabigatran. Thromb Haemost 2011;106: 178179. 7 Dempfle CH, Hennerici MG: Dabigatran and stroke thrombolysis. Cerebrovasc Dis 2010;30:203205. 8 Lansberg MG, Albers GW, Wijman CA: Symptomatic intracerebral hemorrhage following thrombolytic therapy for acute ischemic stroke: a review of the risk factors. Cerebrovasc Dis 2007;24:110.
Ignacio Casado Naranjo Department of Neurology Hospital San Pedro de Alcntara ES10001 Cceres (Spain) Tel. +34 927 256 322, E-Mail icasadon @ gmail.com
Stroke Note
Cerebrovasc Dis 2011;32:614615
615
Vous aimerez peut-être aussi
- International Journal of Neurology and Neurotherapy Ijnn 2 030Document2 pagesInternational Journal of Neurology and Neurotherapy Ijnn 2 030Anis Rita PratiwiPas encore d'évaluation
- ASRA GuidelinesDocument26 pagesASRA GuidelinesAzam DanishPas encore d'évaluation
- Beyond The Basics of Stroke EvaluationDocument48 pagesBeyond The Basics of Stroke EvaluationDrGasnasPas encore d'évaluation
- DCV PDFDocument25 pagesDCV PDFLeyDi CamposanoPas encore d'évaluation
- Ischemic Stroke: Laboratory StudiesDocument21 pagesIschemic Stroke: Laboratory Studieskuchaibaru90Pas encore d'évaluation
- Eht 104Document9 pagesEht 104MAX ANTHONY SALAMANCA HILASACAPas encore d'évaluation
- Thrombolytic Therapy For Ischemic StrokeDocument7 pagesThrombolytic Therapy For Ischemic StrokechandradwtrPas encore d'évaluation
- 2016-04-15 Banjarmasin DisolfDocument41 pages2016-04-15 Banjarmasin DisolffaisalsyahrilPas encore d'évaluation
- Treatment: Stroke UnitDocument6 pagesTreatment: Stroke Unitgraze_hinataPas encore d'évaluation
- Cardioprotection by Opening of The K Channel in Unstable AnginaDocument7 pagesCardioprotection by Opening of The K Channel in Unstable Angina111111111111111111132222Pas encore d'évaluation
- Brain Natriuretic Peptide in Acute Ischemic StrokeDocument6 pagesBrain Natriuretic Peptide in Acute Ischemic Strokesalma rachidiPas encore d'évaluation
- Bezold JarischDocument6 pagesBezold Jarischbecky_meloniPas encore d'évaluation
- Profile and Relation To Neurological Impairment Matrix Metalloproteinase Expression After Human Cardioembolic Stroke: TemporalDocument9 pagesProfile and Relation To Neurological Impairment Matrix Metalloproteinase Expression After Human Cardioembolic Stroke: TemporalArif Dwi CahyonoPas encore d'évaluation
- Article 4 NL RatioDocument4 pagesArticle 4 NL RatioPrateek Kumar PandaPas encore d'évaluation
- Antithrombotic and Thrombolytic Therapy For Ischemic StrokeDocument21 pagesAntithrombotic and Thrombolytic Therapy For Ischemic StrokeHabibie TifanPas encore d'évaluation
- Emergent Management of Acute Ischemic Stroke PDF VersionDocument73 pagesEmergent Management of Acute Ischemic Stroke PDF VersionElizar JarPas encore d'évaluation
- StrokeDocument22 pagesStrokeAlex GasnasPas encore d'évaluation
- 89705664Document10 pages89705664justin_sanePas encore d'évaluation
- Imagingofacute Ischemicstroke: Carlos Leiva-Salinas and Max WintermarkDocument14 pagesImagingofacute Ischemicstroke: Carlos Leiva-Salinas and Max Wintermarkpima29Pas encore d'évaluation
- AINES e Clinical OutcomesDocument23 pagesAINES e Clinical Outcomesdiogofc123Pas encore d'évaluation
- Nanda, A, Niranjan NS, Transient Ischemic Attack. Medscape. 2013Document6 pagesNanda, A, Niranjan NS, Transient Ischemic Attack. Medscape. 2013rahmatPas encore d'évaluation
- Thrombolytic Therapy in Emergency MedicineDocument8 pagesThrombolytic Therapy in Emergency MedicinemedeviPas encore d'évaluation
- Nejmoa 010746Document9 pagesNejmoa 010746Mmle BlaséPas encore d'évaluation
- Piis1052305713004734 PDFDocument7 pagesPiis1052305713004734 PDFbellaPas encore d'évaluation
- Spontaneous Subdural Hematoma and Antiplatelet Therapy: Does Efficacy of Ticagrelor Come With Added Risk?Document6 pagesSpontaneous Subdural Hematoma and Antiplatelet Therapy: Does Efficacy of Ticagrelor Come With Added Risk?Indira DeviPas encore d'évaluation
- Neurologic EmergenciesDocument11 pagesNeurologic EmergenciesRoberto López MataPas encore d'évaluation
- Cortez-Neuroradiology 2020Document10 pagesCortez-Neuroradiology 2020Pedro VillamorPas encore d'évaluation
- Mavinkurve Groothuis2012Document8 pagesMavinkurve Groothuis2012rcmvywo jamqalhxilwPas encore d'évaluation
- JurnalDocument9 pagesJurnalRifqi FathendraPas encore d'évaluation
- Myocard InfarctionDocument10 pagesMyocard InfarctionFelicia HoseaPas encore d'évaluation
- Intracerebral Hemorrhage Medical TreatmentDocument3 pagesIntracerebral Hemorrhage Medical TreatmentDarrel Allan MandiasPas encore d'évaluation
- (19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeDocument7 pages(19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeRandy Reina RiveroPas encore d'évaluation
- In Practice: Hypertension After Kidney TransplantDocument11 pagesIn Practice: Hypertension After Kidney TransplantRavan WidiPas encore d'évaluation
- Commander HFDocument11 pagesCommander HFhairos.izhaPas encore d'évaluation
- Version of Record:: ManuscriptDocument23 pagesVersion of Record:: Manuscriptmiko balisiPas encore d'évaluation
- Safety and Efficacy of Intensive Vs Guideline Antiplatelet Thera 2015Document7 pagesSafety and Efficacy of Intensive Vs Guideline Antiplatelet Thera 2015AnDreARPas encore d'évaluation
- HicksCodeStrokeHospitalists PDFDocument57 pagesHicksCodeStrokeHospitalists PDFRizky DimasaputraPas encore d'évaluation
- Impact of Atropine and Aminophylline On TAVB With Inferior Wall MIDocument2 pagesImpact of Atropine and Aminophylline On TAVB With Inferior Wall MIRakhmat RamadhaniPas encore d'évaluation
- Endovascular and Neurosurgical MX of StrokeDocument18 pagesEndovascular and Neurosurgical MX of StrokeAndrei ChirtoacaPas encore d'évaluation
- DynaMed Plus - Stroke (Acute Management)Document126 pagesDynaMed Plus - Stroke (Acute Management)Sarah Shafa MarwadhaniPas encore d'évaluation
- Glyceryl Trinitrate For Acute Intracerebral HemorrhageDocument21 pagesGlyceryl Trinitrate For Acute Intracerebral HemorrhageAhmad Al-atthosPas encore d'évaluation
- Effect of Nocturnal Oxygen Therapy On Electrocardiographic Changes Among Patients With Congestive Heart FailureDocument3 pagesEffect of Nocturnal Oxygen Therapy On Electrocardiographic Changes Among Patients With Congestive Heart FailureNurAfifahPas encore d'évaluation
- Iacta 2011 Janak Mehta Award Winning PresentationDocument56 pagesIacta 2011 Janak Mehta Award Winning PresentationDr.Sandeep Kumar KarPas encore d'évaluation
- Dong 2022Document8 pagesDong 2022Olivia LimPas encore d'évaluation
- Perioperative Anesthesia Anagement OnDocument30 pagesPerioperative Anesthesia Anagement OnryandikaPas encore d'évaluation
- T T A S: Hrombolytic Herapy in Cute TrokeDocument3 pagesT T A S: Hrombolytic Herapy in Cute TrokevivinPas encore d'évaluation
- MNG - D1 - 1. Clinical Guideline of Acute Stroke (WHO)Document42 pagesMNG - D1 - 1. Clinical Guideline of Acute Stroke (WHO)Shelin ClarissaPas encore d'évaluation
- White 2012 Champion PooledDocument13 pagesWhite 2012 Champion PooledRadu CiprianPas encore d'évaluation
- Jaha 119 012932Document29 pagesJaha 119 012932Emily Araujo nonatoPas encore d'évaluation
- Ehac 053Document9 pagesEhac 053Andreea TudurachiPas encore d'évaluation
- Cardiovascular Risk: The Safety of Local Anesthesia, Vasoconstrictors, and Sedation in Heart DiseaseDocument7 pagesCardiovascular Risk: The Safety of Local Anesthesia, Vasoconstrictors, and Sedation in Heart DiseaseMARIA KARINA HERNANDEZ PEREZPas encore d'évaluation
- Fluid Resuscitation in Haemorrhagic ShockDocument9 pagesFluid Resuscitation in Haemorrhagic ShockbashiruaminuPas encore d'évaluation
- 3091 Full PDFDocument7 pages3091 Full PDFgeeheebPas encore d'évaluation
- 2009 8 Focus09158Document5 pages2009 8 Focus09158ninostranoPas encore d'évaluation
- Efficacy and Safety of Thrombolytic Therapy in ProDocument5 pagesEfficacy and Safety of Thrombolytic Therapy in ProgalalPas encore d'évaluation
- EPITHET Failed Chance or New HopeDocument2 pagesEPITHET Failed Chance or New HopeMondo BijainePas encore d'évaluation
- Fifteen-Year Experience: Open Heart Surgery in Patients With End-Stage Renal FailureDocument6 pagesFifteen-Year Experience: Open Heart Surgery in Patients With End-Stage Renal FailureDavid RamirezPas encore d'évaluation
- Use of Heparin in Neurointervention: A Review of The LiteratureDocument6 pagesUse of Heparin in Neurointervention: A Review of The LiteratureStrawberry ShortcakePas encore d'évaluation
- Assessment of bleeding Shock in a Politraumatized PatientD'EverandAssessment of bleeding Shock in a Politraumatized PatientPas encore d'évaluation
- Case-Based Device Therapy for Heart FailureD'EverandCase-Based Device Therapy for Heart FailureUlrika Birgersdotter-GreenPas encore d'évaluation
- Ankle ExerciseDocument2 pagesAnkle Exercisepocholofiesta20048772Pas encore d'évaluation
- Chiari Malformation: An Overview: Rick Labuda, Executive DirectorDocument18 pagesChiari Malformation: An Overview: Rick Labuda, Executive DirectornsurgeonPas encore d'évaluation
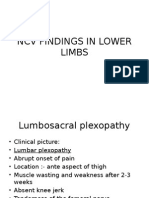
- NCV Findings in Lower LimbsDocument30 pagesNCV Findings in Lower LimbsKarthik BhashyamPas encore d'évaluation
- LMU-DCOM Insights Fall 2019Document36 pagesLMU-DCOM Insights Fall 2019MichellePas encore d'évaluation
- Taquiarritmias Supraventriculares NEJMDocument11 pagesTaquiarritmias Supraventriculares NEJMCamilo VidalPas encore d'évaluation
- Algoritma SVTDocument87 pagesAlgoritma SVTbonne_amePas encore d'évaluation
- Anottated BibDocument5 pagesAnottated Bibapi-207760045Pas encore d'évaluation
- Foot and Ankle TreatmentDocument59 pagesFoot and Ankle TreatmentKonstantinosKontouvalisPas encore d'évaluation
- Organizational AnalysisDocument14 pagesOrganizational AnalysisLizzie JanitoPas encore d'évaluation
- Wilson DiseaseDocument12 pagesWilson DiseasedrakshatbPas encore d'évaluation
- TCM Tongue Diagnosis - Complete Health and HappinessDocument17 pagesTCM Tongue Diagnosis - Complete Health and HappinessmusatiiPas encore d'évaluation
- The Beauty of DentistryDocument5 pagesThe Beauty of DentistryMorosanu Diana GeorgianaPas encore d'évaluation
- Elastic Bandage - ApplyingDocument4 pagesElastic Bandage - ApplyingMargarida CaladoPas encore d'évaluation
- Eff Ects On Hypotension Incidence: Hyperbaric, Isobaric, and Combinations of Bupivacaine For Spinal Anesthesia in Cesarean SectionDocument7 pagesEff Ects On Hypotension Incidence: Hyperbaric, Isobaric, and Combinations of Bupivacaine For Spinal Anesthesia in Cesarean SectionPalwasha MalikPas encore d'évaluation
- Hydrocephalus PresDocument14 pagesHydrocephalus Presapi-610861419Pas encore d'évaluation
- Daftar PustakaDocument2 pagesDaftar PustakajhuvanPas encore d'évaluation
- SOP Hand WashDocument4 pagesSOP Hand Washjajardoank100% (3)
- Kulkarni2018 PDFDocument7 pagesKulkarni2018 PDFtooba uroojPas encore d'évaluation
- Biomechanics NotesDocument21 pagesBiomechanics Notesstarlight9394100% (1)
- Manual Capnografo npb-75mDocument65 pagesManual Capnografo npb-75mLuis Mendoza100% (2)
- Biologic Width Around One - and Two-Piece Titanium ImplantsDocument13 pagesBiologic Width Around One - and Two-Piece Titanium Implantsptrjn_vdc100% (1)
- Family Satisfaction in The Trauma and Surgical Intensive Care Unit: Another Important Quality MeasureDocument5 pagesFamily Satisfaction in The Trauma and Surgical Intensive Care Unit: Another Important Quality MeasureSeptiana ChimuzPas encore d'évaluation
- Vyr GBL 2100296 Seven Ventilators Challenged With Leaks During Neonatal Nasal Cpap - Final - 0Document2 pagesVyr GBL 2100296 Seven Ventilators Challenged With Leaks During Neonatal Nasal Cpap - Final - 0Michael LevitPas encore d'évaluation
- Annual Report 2016-2017 (English Version)Document396 pagesAnnual Report 2016-2017 (English Version)Mishthi MalaniPas encore d'évaluation
- Abg Analysis ReviewerDocument21 pagesAbg Analysis ReviewerAyiessa_AJPas encore d'évaluation
- Rotablation TipsDocument60 pagesRotablation TipsSabyasachi MukhopadhyayPas encore d'évaluation
- Uses of LichensDocument42 pagesUses of LichensbenzzzxPas encore d'évaluation
- RMO Clinical HandbookDocument533 pagesRMO Clinical HandbookRicardo TPas encore d'évaluation
- Sample CCMSADocument8 pagesSample CCMSAVasantha Eswaraka0% (1)
- 4th Lecture On Nerve Physiology by Dr. RoomiDocument8 pages4th Lecture On Nerve Physiology by Dr. RoomiMudassar Roomi100% (1)