Académique Documents
Professionnel Documents
Culture Documents
F.M. Smith - Extrinsic Inputs To Intrinsic Neurons in The Porcine Heart in Vitro
Transféré par
GretymjDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
F.M. Smith - Extrinsic Inputs To Intrinsic Neurons in The Porcine Heart in Vitro
Transféré par
GretymjDroits d'auteur :
Formats disponibles
Extrinsic inputs to intrinsic neurons in the porcine heart in vitro
F. M. Smith
Am J Physiol Regul Integr Comp Physiol 276:R455-R467, 1999. You might find this additional info useful... This article cites 48 articles, 25 of which can be accessed free at: http://ajpregu.physiology.org/content/276/2/R455.full.html#ref-list-1 This article has been cited by 1 other HighWire hosted articles Effects of chronic cardiac decentralization on functional properties of canine intracardiac neurons in vitro F. M. Smith, A. S. McGuirt, J. Leger, J. A. Armour and J. L. Ardell Am J Physiol Regul Integr Comp Physiol, November 1, 2001; 281 (5): R1474-R1482. [Abstract] [Full Text] [PDF] Updated information and services including high resolution figures, can be found at: http://ajpregu.physiology.org/content/276/2/R455.full.html Additional material and information about American Journal of Physiology - Regulatory, Integrative and Comparative Physiology can be found at: http://www.the-aps.org/publications/ajpregu
Downloaded from ajpregu.physiology.org on January 2, 2012
This infomation is current as of January 2, 2012.
American Journal of Physiology - Regulatory, Integrative and Comparative Physiology publishes original investigations that illuminate normal or abnormal regulation and integration of physiological mechanisms at all levels of biological organization, ranging from molecules to humans, including clinical investigations. It is published 12 times a year (monthly) by the American Physiological Society, 9650 Rockville Pike, Bethesda MD 20814-3991. Copyright 1999 by the American Physiological Society. ISSN: 0363-6119, ESSN: 1522-1490. Visit our website at http://www.the-aps.org/.
Extrinsic inputs to intrinsic neurons in the porcine heart in vitro
F. M. SMITH Department of Anatomy and Neurobiology, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada B3H 4H7
Smith, F. M. Extrinsic inputs to intrinsic neurons in the porcine heart in vitro. Am. J. Physiol. 276 (Regulatory Integrative Comp. Physiol. 45): R455R467, 1999.Convergence of inputs from extrinsic cardiac nerves [vagus and cardiopulmonary (CPN)] on intrinsic cardiac neurons was investigated in the pig (Sus scrofa). A segment of the right atrial wall containing epicardial neurons along with attached stumps of the right vagus nerve and CPN was maintained in vitro; intracellular recordings were made from 57 neurons. Three types of neuron were identied by their responses to long intracellular depolarizing current pulses: phasic [discharged 1 action potential (AP); 40%]; accommodating (discharged multiple APs decrementing in frequency during pulse; 33%); and tonic (discharged multiple APs at a high frequency; 27%). Sixty-six percent of the neurons responded with excitatory postsynaptic potentials (EPSP) to vagal nerve stimulation; two-thirds of these cells red APs when EPSP amplitude exceeded threshold level. Postsynaptic responses to vagal nerve stimulation were mediated by nicotinic ion channels; responses were eliminated by hexamethonium. CPN stimulation produced EPSPs but no APs in 17% of the neurons. All neurons responding with postsynaptic depolarizations to CPN stimulation also received vagal inputs. Combined stimulation of the vagus nerve and CPN produced APs in all but one of these neurons. Timolol eliminated postsynaptic responses from CPN stimulation, indicating that these responses involved -adrenergic receptors and likely resulted from activation of sympathetic postganglionic terminals. These results show that some intrinsic cardiac neurons receive convergent inputs from the CPN and vagus nerve. It is suggested that such neurons represent intraganglionic sites for sympathetic-parasympathetic interactions in neural control of the heart. intrinsic cardiac ganglia; sympathetic innervation; vagus nerve; cardiopulmonary nerve; intracellular recording
THE MAMMALIAN HEART is dually innervated by the sympathetic and parasympathetic limbs of the autonomic nervous system. The cardiac branches of the vagus nerves convey parasympathetic efferent preganglionic axons to the heart (29, 30) where some of these terminate on postganglionic neurons in the intrinsic cardiac ganglia. The majority of sympathetic postganglionic axons innervating the heart course in cardiopulmonary nerves originating from the middle cervical, stellate, and, in some species, upper thoracic ganglia of the paravertebral ganglion chain (30, 31, 40). The anatomic separation of these autonomic pathways has informed analyses of their functions in cardiac regulation, and the sympathetic and parasympathetic limbs are traditionally considered to control the heart in a reciprocal fashion. That is, when vagal cardiodepressant activity is low, sympathetic cardioaugmentatory activity is high, and vice versa (14). However, studies in which activity
of vagal and sympathetic cardiac nerves was recorded simultaneously have shown that these inputs to the heart are coactivated under a wide range of physiological conditions, for example during periods of increased atrial lling (36). When parasympathetic and sympathetic inputs to the heart are activated together, signicant interactions between these inputs occur, and the primary sites for these interactions are considered to be the autonomic neuroeffector junctions at the myocardium (24, 38, 39, 46, 47, 53). At these sites, interactions occur through sympathetic modulation of vagal function or vagal modication of sympathetic function, depending on the prevailing physiological circumstances (58). These interactions are believed to be mediated by the combined inuences of transmitter and modulator substances released by sympathetic and parasympathetic terminals on the myocardium (39), as well as by prejunctional modulatory mechanisms on neuroeffector terminals (38, 47). However, another potential site for sympathetic-parasympathetic interactions is within the intracardiac ganglia at the level of single neurons. These neurons are organized into ganglionated plexuses, which are connected into a network by interganglionic nerves (5, 9, 10, 12, 13, 22, 51). Classically, intracardiac neurons have been viewed as simple relays between parasympathetic preganglionic axons and the myocardium. However, recent anatomic reports indicate that sympathetic terminals exist within intracardiac ganglia (22, 43, 44), and it is therefore possible that sympathetic and parasympathetic inputs may converge on single intracardiac neurons. The main objective of this study was to investigate the intracellular responses of single intrinsic cardiac neurons of the pig right atrium in vitro to stimulation of attached cardiac vagal and cardiopulmonary nerve stumps to identify neurons potentially capable of integrating information from both efferent limbs of the autonomic nervous system. Recordings made from intracardiac neurons in this study show that some of these neurons receive both parasympathetic and sympathetic inputs and that interactions between these dual inputs can modify neuronal ring properties.
METHODS
Downloaded from ajpregu.physiology.org on January 2, 2012
Experiments were done on 22 pigs of both sexes, 2026 days old and with a mean body mass of 8.5 0.3 kg (mean SE). Pilot studies were conducted on a range of species (dog, pig, and guinea pig) to determine the best preparation for recording intracellularly from intracardiac neurons with extrinsic inputs. The pig heart was chosen because, in this species, a population of intracardiac neurons with responses to extrinsic nerve stimulation was located in the right atrial
R455
0363-6119/99 $5.00 Copyright
1999 the American Physiological Society
R456
EXTRINSIC INPUTS TO INTRACARDIAC NEURONS
wall close to the entry point of the extrinsic nerves. The overall size of this segment of atrial wall and attached nerve stumps was small enough to be maintained in vitro, and intracardiac ganglia receiving extrinsic inputs could be accessed easily for recording. Animals were obtained from a local livestock supplier and were maintained in the University Animal Care Facility for up to 3 days at 20C under a 12:12-h light-dark cycle before the experiments. Animals were treated in conformance with the guidelines of the Canadian Council on Animal Care; the protocol for these experiments was approved by the Dalhousie University Committee on Animal Care. Animals were killed by an overdose of pentobarbital sodium (1,000 mg) administered intraperitoneally. The sternum was opened in the midline, and the heart with attached stumps of right vagal and cardiopulmonary nerves was quickly removed and further dissected in a dish containing owing oxygenated Tyrode solution at room temperature. This solution contained (in mM) 120 NaCl, 4 KCl, 1.2 KH2PO4, 1.2 MgSO4, 11 glucose, 10 HEPES, and 1.9 CaCl2; pH was adjusted to 7.4 before use. All chemicals were obtained from Sigma (St. Louis, MO). The solution was saturated with 100% O2 using a gas disperser. A block of tissue including the intercaval right atrial wall along with attached nerves was dissected free of the heart for in vitro recording from intracardiac neurons. To ensure inclusion of all right cardiac vagal branches, segments of this nerve extending cranially from the heart to the level of the middle cervical ganglion near the thoracic inlet and caudally from the heart to the diaphragm were included. The attached sympathetic cardiac nerves included all cardiopulmonary branches running to the heart from the right stellate and middle cervical ganglia and ansae subclavia. The tissue block was pinned to the silicone rubber-covered bottom of a 30-ml recording chamber and perfused with oxygenated Tyrode solution maintained at 36C by a thermostatically controlled heater. The stumps of the vagal and cardiopulmonary nerves were gathered into bipolar suction electrodes lled with perfusate for stimulation with rectangular current pulses (0.5-ms duration). These electrodes were driven by a stimulator (S88, Grass Instrument, Quincy, MA) through constant-current stimulus isolation units. Epicardial ganglia were exposed by blunt dissection with the aid of a dissecting microscope. In this area of the atrium, ganglia were embedded in epicardial fat and were connected together by small nerves in a ganglionated plexus. A ganglion selected for recording was lightly supported on a metal platform (0.2 mm wide, 0.6 mm long) attached to a micropositioner. With this platform the ganglion was held slightly away from the underlying tissue to provide mechanical stabilization, thus facilitating penetration of the tough ganglion sheath by the recording electrode (50). Ganglion cells and connecting nerves were not damaged by this procedure. Ganglia were explored with a glass micropipette electrode lled with 3 M KCl (electrode resistance 50120 M ), mounted on a three-axis mechanical micromanipulator. The electrode was connected to an intracellular amplier equipped with current injection and bridge-balancing circuitry (model 1600, A-M Systems, Everett, WA) for nulling the electrode resistance. Before neurons were impaled, electrode potential was nulled with reference to the bath potential, and this null was conrmed after withdrawing the electrode from the neuron at the end of a recording session. The difference between intracellular and bath potentials was taken as the transmembrane potential. The bath reference electrode consisted of a silver wire, coated with silver chloride, inserted into a capillary tube lled with 1% agar dissolved in the same solution used to ll the recording
electrode, with the tip of the capillary tube immersed in the bath. To determine threshold and maximal responses to nerve stimulation, stimulus current was increased by increments until the rst response appeared (threshold response), then further increased until the response reached peak amplitude (maximal response). Transmembrane potential, intracellular stimulus waveforms, and responses to nerve stimulation were monitored on an oscilloscope during the experiments and stored on videotape through a digital data converter (model PCM4, Medical Systems, Greenvale, NY) connected to a videocassette recorder for later analysis. Selected responses were played back from the tape into a data-acquisition board attached to a personal computer and analyzed with pCLAMP software (Axon Instruments, Foster City, CA). Data Analysis Whole cell input resistance was estimated from the slope of a line plotting membrane potential displacements from resting potential against the amplitudes of a series of hyperpolarizing current pulses (200- to 400-ms duration) delivered through the recording electrode to clamp membrane current at preset levels. Some neurons displayed time-dependent voltage changes at the start of hyperpolarizing pulses, so only the last 50 ms of responses, when potentials had reached steady-state values, were sampled. Plots of current-voltage relationships were linear over a range of voltages up to 3540 mV more negative than the resting potential. All neurons displayed marked nonlinearity in the current-voltage relationship when depolarizing pulses subthreshold for action potential (AP) generation were injected, so these responses were not included in estimates of input resistance. Membrane time constant was estimated from the time course of responses to small (0.1 nA) hyperpolarizing currents. A curve-tting program (CLAMPAN in the suite of pCLAMP programs) indicated that these responses followed a single-exponential time course, as reported for other autonomic neurons (28), so time constant for each cell was calculated as the time for membrane potential to change by 1 1/e of the nal steady-state value during hyperpolarization. The amplitude of depolarization to threshold for AP generation was taken as the difference between resting membrane potential and the voltage at which regenerative changes were initiated. AP duration was measured at one-half peak amplitude. Afterhyperpolarization (AHP) amplitude was taken as the difference between resting membrane potential and peak amplitude of the hyperpolarization following the AP. For estimating AHP duration, the time was measured from the point at which the repolarizing waveform crossed the level of the resting membrane potential, to the point at which the potential had returned to one-half the peak amplitude of the AHP. Differences among mean values of intracellular variables were analyzed by ANOVA (P 0.05). Where f values were signicant, comparisons between means were done using Scheffes multiple means comparison test (57). Experimental design and statistical analysis of the data were carried out in accordance with guidelines suggested by Wallenstein et al. (52), Glantz (25), and Denenberg (20).
RESULTS
Downloaded from ajpregu.physiology.org on January 2, 2012
Membrane and Firing Properties of Intracardiac Neurons Neurons with resting membrane potentials that did not settle to values more negative than 40 mV within 5 min of impalement were excluded from this study. Mean values of resting membrane potential, whole cell
EXTRINSIC INPUTS TO INTRACARDIAC NEURONS
R457
Table 1. Membrane properties and characteristics of action potentials for neurons grouped by ring pattern
Neuron Type Phasic (40%) (n 23) Accommodating (33%) (n 19) Tonic (27%) (n 15)
Resting membrane potential, mV Whole cell input resistance, M Whole cell time constant, ms Action potential characteristics Threshold depolarization, mV Total amplitude, mV Overshoot, mV Duration, ms After hyperpolarization characteristics Amplitude, mV Duration, ms
lus continued, Fig. 2B); and 3) 27% were tonic (discharged multiple APs with little or no frequency decrement throughout the stimulus pulse, Fig. 2C). There were no statistically signicant differences in mean resting membrane potential or mean whole cell time constant among the three types of neuron, but whole cell input resistance was signicantly higher in phasic than in accommodating or tonic neurons. Phasic neu-
49 72 5.8
4 (23) 8* (23) 0.7 (8)
47 33 7.2
5 (19) 7 (19) 1.1 (9)
49 39 6.1
5 (15) 7 (15) 1.2 (11)
19 73 24 1.5
4 (23) 5 (23) 4 (23) 0.4 (23)
27 75 27 1.9
2 (14) 4 (19) 4 (19) 0.3 (18)
25 72 24 1.6
2 (15) 5 (15) 2 (15) 0.2 (15)
Downloaded from ajpregu.physiology.org on January 2, 2012
8 48
3 (22) 4 (22)
13 39
3 (19) 5 (19)
10 130
2 (15) 11 (15)
Values are expressed as means SE. No. of measurements contributing to each mean is shown in parentheses beside each value. Characteristics of action potentials were evoked by intracellular depolarizing currents delivered through the recording electrode. Signicantly different from: * accommodating neurons and tonic neurons; accommodating neurons but not tonic neurons; phasic neurons and accommodating neurons.
input resistance, and whole cell time constant, along with neuronal responses to depolarization, are summarized in Table 1. All neurons sampled in this study responded with depolarizations to inward current pulses of 50- to 60-ms duration delivered through the recording electrode, and generated APs when stimulus current reached threshold (Fig. 1). Three types of response to prolonged (400- to 600-ms duration) depolarizing current pulses permitted classication of intracardiac neurons into three groups: 1) 40% were phasic (discharged 1 AP at the start of the stimulus pulse, Fig. 2A); 2) 33% were accommodating (discharged multiple APs that decreased in frequency as the stimuFig. 2. Examples of responses of 3 types of intracardiac neurons to long intracellular depolarizing current pulses. AC: top main trace represents transmembrane potential (0 V indicated at left), and bottom main trace represents stimulus current. Smaller traces (insets) above main voltage traces show AP and afterhyperpolarization (AHP) in response to a brief intracellular depolarizing pulse (5-ms duration; current artifact precedes AP). A: phasic neuron; 1.2-nA, 520-ms duration current pulse evoked 1 AP. A, inset: AHP duration was 35 ms. Resting membrane potential before stimulation was 67 mV. B: accommodating neuron; 0.7-nA, 540-ms-duration current pulse elicited multiple APs, which decreased in frequency during the depolarization pulse. B, inset: AHP duration was 29 ms. Resting membrane potential was 42 mV. C: tonic neuron; 0.6-nA, 440-ms-duration current pulse produced multiple APs that did not decrement in frequency over duration of pulse. C, inset: AHP duration was 118 ms. Resting membrane potential was 57 mV. Tonic neuron (C) had longest-duration AHP despite displaying highest ring frequency. Vertical calibration bar: 30 mV for inset traces; 20 mV, 1 nA for main traces. Horizontal calibration bar: 150 ms for inset traces, 60 ms for main traces.
Fig. 1. Response of membrane potential (top trace) of an intracardiac neuron to a depolarizing current pulse (0.2 nA, 60-ms duration; bottom trace) delivered through the intracellular recording electrode. Stimulus current intensity was at threshold for evoking an action potential (AP) in this cell. Resting membrane potential before current injection was 48 mV; peak of AP overshoots 0 V (indicated at left). Vertical calibration bar: 20 mV, 1 nA. Horizontal calibration bar: 20 ms.
R458
EXTRINSIC INPUTS TO INTRACARDIAC NEURONS
Table 2. Patterns of extrinsic input to physiologically identied intracardiac neurons
Response to Extrinsic Nerve Stimulation Neuron Type Phasic Accommodating Tonic Totals
No extrinsic input n % of total Vagal input only n % of total Vagal and CPN input n % of total
1 2 22 38 9 15
4 7 15 26 1 2
14 24 1 2 0 0
19 33 38 66 10 17
CPN, cardiopulmonary nerve; n, no. of neurons of each type within each category of response to extrinsic nerve stimulation.
rons also had a signicantly lower depolarization threshold for ring APs than did the other two cell types. The APs of all neurons in this study overshot 0 V, and AP duration was not signicantly different among the groups. AHPs were of similar amplitude in all cell types, but the duration of AHP in tonic neurons was signicantly longer than in phasic or accommodating neurons (Table 1; examples shown in Fig. 2, insets). Responses to Extrinsic Nerve Stimulation All intracardiac neurons in this study were tested for the presence of inputs from extrinsic cardiac nerves. Intracellular responses evoked by single-pulse stimulation of vagus and cardiopulmonary nerves in the three classes of neurons are summarized by neuron type in Table 2. All phasic neurons except one received input from the vagus nerve, and a subset of these neurons also responded to cardiopulmonary nerve stimulation. Many accommodating neurons also received vagal inputs, and one of these cells responded to cardiopulmonary nerve stimulation as well. Only one tonic neuron responded to vagal nerve stimulation, and no tonic cells received inputs from cardiopulmonary nerves. All intracellular responses to nerve stimulation were conrmed as orthodromic by their elimination in a modied perfusate containing 0 Ca2 and high Mg2 (10 mM) (see Figs. 3B, 4B, and 5B). No antidromic responses to extrinsic nerve stimulation were recorded in this study. All postsynaptic responses were depolarizing; no hyperpolarizing responses were observed. Responses to vagus and cardiopulmonary nerve stimulation are described in more detail in the following sections. Vagus nerve stimulation. In this study, 66% of neurons sampled responded to vagus nerve stimulation (Table 2; Figs. 3 and 4). Threshold neuronal responses were without exception marked by the appearance of small excitatory postsynaptic potentials (EPSP) at latencies of up to 40 ms (Figs. 3 and 4); as stimulus current intensity was increased, multiple EPSPs were evoked (Figs. 3 and 4). Graded increases in stimulation produced corresponding increases in the amplitude of the EPSPs (Figs. 3 and 4). In some neurons additional EPSPs frequently occurred at latencies of 70 to 100 ms after the stimulus pulse (e.g., Fig. 4A, 2.1-mA trace
from top). One-third of the neurons responding to vagal stimulation generated EPSPs that did not reach threshold for AP initiation (Fig. 3) even when the intensity of nerve stimulation was maximal. Some of these EPSPs were followed by small AHPs (e.g., Fig. 4A, 2.5-mA trace). The duration of EPSPs evoked by vagal nerve stimulation was similar in all three cell types, so data from all groups have been combined; the mean value of EPSP duration was 15 2 ms. In eight phasic cells and ve accommodating cells responsive to vagal nerve stimulation, EPSPs reached threshold for AP generation. The mean amplitude of EPSPs reaching threshold for AP generation was 17 3 mV in phasic and 23 4 mV in accommodating neurons; these values are consistent with threshold values for intracellularly evoked APs in these two groups (Table 1). All orthodromically mediated APs overshot 0 V, and, for phasic and accommodating neurons, peak AP amplitude was within a few millivolts of the values shown in Table 1 for directly
Downloaded from ajpregu.physiology.org on January 2, 2012
Fig. 3. Excitatory response of an intracardiac neuron to single-pulse stimulation (0.5-ms duration) of cardiac branches of right vagus nerve (stimulus indicated by artifacts at start of traces). Resting membrane potential of cell was 49 mV. A: responses to intensitygraded stimulation (current increasing from top to bottom traces; intensity indicated at left of each trace). Note multiple excitatory postsynaptic potentials (EPSP) and a reduction of latency to onset of response at greatest current intensity. No AP could be evoked by nerve stimulation in this neuron. B: response to nerve stimulation was eliminated by 5-min exposure to modied, Ca2 -free perfusate containing 10 mM Mg2 . C: exposure to hexamethonium (HEX; 100 M for 6 min in perfusate) also eliminated response to nerve stimulation, demonstrating that this response was mediated by nicotinic channels in postsynaptic membrane. Stimulus intensity in B and C was 5 mA. All stimulus artifacts have been truncated for clarity. Vertical calibration bar: 10 mV. Horizontal calibration bar: 10 ms.
EXTRINSIC INPUTS TO INTRACARDIAC NEURONS
R459
Fig. 4. Intracardiac neuron generating EPSPs and AP in response to vagus nerve stimulation (experimental protocol similar to that in Fig. 3). Resting membrane potential was 51 mV. A: intensity-graded single-pulse nerve stimulation evoked multiple EPSPs that summed to exceed threshold for AP generation at the highest intensity (bottom trace; 0-V level indicated at left). B and C: at same stimulus intensity as in bottom trace of A, neuronal responses to nerve stimulation were blocked in 0-Ca2 , high-Mg2 (lo Ca2 , hi Mg2 ) perfusate and in 100 M bath-applied hexamethonium, respectively (both 5-min exposure). As in Fig. 3, neuronal responses to nerve stimulation were mediated by nicotinic postsynaptic receptors. D: timolol (TIM; 10 M, 5 min in perfusate) had no effect on membrane potential or responses to vagus nerve stimulation. AP was truncated for clarity. Vertical calibration bar: 10 mV. Horizontal calibration bar: 20 ms.
Downloaded from ajpregu.physiology.org on January 2, 2012
evoked APs. Within the group of neurons responding to vagus nerve stimulation, mean AHP amplitude and duration were, respectively, 9 2 mV and 54 6 ms for phasic and 15 4 mV and 47 11 ms for accommodating neurons. In the only tonic neuron responding to vagal nerve stimulation, the EPSP did not reach threshold for AP generation. Cardiopulmonary nerve stimulation. Graded cardiopulmonary nerve stimulation evoked EPSPs with correspondingly graded amplitudes in 17% of the neurons in this study, at latencies up to 15 ms after the stimulus pulse (Fig. 5). Nine of these cells were phasic and one was accommodating (Table 2). These neurons constituted a subset of those responsive to vagal stimulation;
no neurons impaled in this study responded only to cardiopulmonary nerve stimulation. As shown in the example in Fig. 5, maximal cardiopulmonary nerve stimulation was not, in itself, sufficient to evoke an AP in any of these neurons. EPSPs evoked in accommodating and phasic neurons by cardiopulmonary nerve stimulation had similar amplitudes and durations, so EPSP data from all neurons were combined for comparison with the properties of EPSPs evoked in these cells by vagus nerve stimulation, as shown in Table 3. EPSPs evoked by cardiopulmonary nerve stimulation were signicantly smaller in amplitude and signicantly shorter in duration than those evoked by vagal nerve stimulation in the same neurons. In none of these
R460
EXTRINSIC INPUTS TO INTRACARDIAC NEURONS
Table 3. Comparison of properties of excitatory postsynaptic potentials evoked in same neurons by stimulation of vagus and cardiopulmonary nerves
Vagus Nerve Stimulation Cardipulmonary Nerve Stimulation
Amplitude, mV Duration, ms
19 17
3 2
7 11
1* 2*
Values are expressed as means SE; n 10 neurons. * Signicant difference from value for vagus nerve stimulation (P 0.05; t-test).
and of longer duration (Fig. 6C) compared with the AP and AHP generated by vagal nerve stimulation alone. These differences are readily apparent in Fig. 6C, where the AP resulting from vagus nerve stimulation has been juxtaposed with the response to combined
Downloaded from ajpregu.physiology.org on January 2, 2012
Fig. 5. Effects of cardiopulmonary nerve stimulation on an intracardiac neuron. Protocol was similar to that of Figs. 3 and 4. Resting membrane potential was 46 mV. A: intensity-graded nerve stimulation evoked an EPSP but no AP in this neuron; this was true for all neurons receiving inputs from the cardiopulmonary nerve. B and C: blockade of postsynaptic responses by lo Ca2 , hi Mg2 perfusate and by timolol (10 M in bath) showed that these responses were orthodromic and involved -adrenergic receptors. D: postsynaptic responses were unaffected by 100 M hexamethonium in the bath. Vertical calibration bar: 10 mV. Horizontal calibration bar: 10 ms.
dually innervated neurons did vagal nerve stimulation alone evoke EPSPs above threshold for AP generation. Costimulation of vagus and cardiopulmonary nerves. There were two types of response to combined vagal and sympathetic nerve stimulation. Two cells, both phasic, displayed responses of the type designated type 1, illustrated in Fig. 6. These neurons produced EPSPs and APs in response to maximal vagal nerve stimulation alone (Fig. 6A) but did not show any postsynaptic responses to cardiopulmonary nerve stimulation alone (Fig. 6B). However, simultaneous stimulation of vagal and cardiopulmonary nerves produced an AP of longer duration and an AHP with a slightly greater amplitude
Fig. 6. Example of type 1 response of an intracardiac neuron to vagus nerve and cardiopulmonary nerve (CPN) stimulation. Resting membrane potential was 43 mV. A: AP produced by maximal (5.0 mA) single-pulse stimulation of vagus nerve (0-V level indicated at left of trace). B: CPN stimulation produced no direct postsynaptic response, even at highest intensity available (10 mA shown). C: costimulation of vagus nerve and CPN with same stimulus parameters as in A and B produced prolonged AP and AHP duration. In C, a portion of trace A has been inset at right of main trace for comparison. In both, dashed lines indicate level of resting membrane potential, and arrows indicate half-amplitude of each AP (for duration comparison). Vertical calibration bar: 10 mV. Horizontal calibration bar: 20 ms.
EXTRINSIC INPUTS TO INTRACARDIAC NEURONS
R461
(Fig. 4A; Fig. 8A, top) were also eliminated by hexamethonium (Fig. 4C; Fig.8B, top). The responses to cardiopulmonary nerve stimulation were unchanged after hexamethonium application (Fig. 5D; Fig. 8B, middle), and combined stimulation of the vagus and cardiopul-
Downloaded from ajpregu.physiology.org on January 2, 2012
Fig. 7. Example of type 2 response of an intracardiac neuron to vagus nerve and CPN stimulation. A: maximal vagus nerve stimulation (6.8 mA) elicited an EPSP but no AP. B: maximal stimulation of CPN (9.0 mA) also generated an EPSP but no AP. C: costimulation of vagus nerve and CPN, using the same stimulus parameters as in A and B, produced EPSPs that summed to exceed ring threshold. Resting membrane potential in this cell was 41 mV before stimulation. Vertical calibration bar: 10 mV. Horizontal calibration bar: 10 ms.
nerve stimulation. As only two neurons displaying a type 1 response were found, no statistical analysis of the effects of combined nerve stimulation was possible. The second type of response, designated type 2, was observed in nine neurons: eight phasic and one accommodating. In these cells, independent vagal and cardiopulmonary nerve stimulation evoked EPSPs (Fig. 7, A and B, respectively; Fig. 8A), but neither input alone was strong enough at maximal stimulus intensity to generate an AP. When both nerves were costimulated at their respective maximal stimulus intensities, the resulting EPSPs summed and reached threshold for AP generation (Fig. 7C; Fig. 8A, bottom). One phasic neuron in which separate stimulation of the cardiopulmonary and vagus nerves evoked smallamplitude EPSPs showed no augmentation of postsynaptic effects in response to combined nerve stimulation, so t neither of the above categories and was not included in the analysis. Effects of cholinergic and -adrenergic blockade. Of the 38 neurons having vagal but no cardiopulmonary inputs, a group of six neurons was tested to determine whether nicotinic neurotransmission was involved. In this group of cells, the nicotinic channel blocker hexamethonium [100 M in the perfusate for at least 5 min; this dose was found to be effective in pig heart in a previous study (50)] eliminated all postsynaptic depolarizing potentials evoked by nerve stimulation (Fig. 3C). In another group of six neurons that were dually innervated by the vagus and cardiopulmonary nerves, the postsynaptic responses to vagus nerve stimulation
Fig. 8. Nicotinic and -adrenergic receptors are involved in type 2 responses of intracardiac neuron to vagus nerve and CPN stimulation. A: control responses to separate stimulation of vagus nerve (7.0 mA) and CPN (9.0 mA) and AP generated by combined nerve stimulation (vagus CPN). Stimulus parameters were unchanged throughout this experiment. B: hexamethonium (100 M for 5 min in perfusate) eliminated the vagally generated EPSP. EPSP resulting from CPN stimulation was unaffected by hexamethonium but neuron did not re an AP in response to costimulation. C: timolol (100 M in perfusate) administered for 5 min in the continued presence of hexamethonium eliminated the EPSP due to CPN stimulation. In this condition, combined nerve stimulation had no postsynaptic effect. Resting membrane potential was 57 mV. Vertical calibration bar: 20 mV. Horizontal calibration bar: 10 ms.
R462
EXTRINSIC INPUTS TO INTRACARDIAC NEURONS
monary nerves then produced the same effect (Fig. 8B, bottom) as did cardiopulmonary nerve stimulation alone. To address the possibility that this concentration of hexamethonium was insufficient to block potential nicotinic neurotransmission through cardiopulmonary inputs, the antagonist dose was increased in two trials to 200 M, but this did not alter the response to cardiopulmonary nerve stimulation (data not shown). To determine the involvement of -adrenergic receptors in responses to nerve stimulation, the -adrenergic antagonist timolol (10 M) was applied in the perfusate. This agent was used because it is a nonselective -antagonist and does not have membrane-stabilizing effects (6). The dose used in this study was within the range found effective in previous studies (6) and was chosen for the present study on the basis of a series of preliminary experiments to determine optimum concentration in atrial tissue. Two protocols were followed in these experiments. In the rst, timolol was applied during vagus nerve stimulation in four experiments to determine if -adrenergic receptors were involved in these responses. -Blockade had no effect on the postsynaptic response to vagal nerve stimulation in these trials, an example of which is shown in Fig. 4D. In the second protocol (6 experiments), timolol was administered during vagus and cardiopulmonary nerve stimulation in the continued presence of hexamethonium. As shown in Fig. 8C, this protocol eliminated the EPSP due to cardiopulmonary nerve stimulation (Fig. 8C, middle); combined cardiopulmonary and vagus nerve stimulation then had no effect (Fig. 8C, bottom).
DISCUSSION
Three patterns of innervation of right atrial neurons by axons in extrinsic cardiac nerves have been revealed in this study. One-third of the neurons sampled received no synaptic inputs of extracardiac origin, whereas the remaining two-thirds were innervated by axons running in the vagus nerve. None of the neurons sampled in this study received inputs solely from cardiopulmonary nerves; instead, inputs from cardiopulmonary axons converged on a subset of vagally innervated neurons. Intracardiac neurons could be classied into three physiological types based on their responses to depolarizing test current pulses, and there appeared to be a relationship between the physiological class of a neuron and the probability of that neuron receiving extrinsic inputs. The properties of extrinsic inputs to intracardiac neurons, the relationships between neuron type and specicity of input, the integrative capabilities conferred by these input patterns and by intrinsic membrane and active properties, and the functional implications of the results are discussed in the following sections. Extrinsic Innervation of Atrial Neurons Sixty-six percent of the cells sampled in this study responded with depolarizing postsynaptic potentials to right vagus nerve stimulation, but in some neurons these depolarizations did not reach threshold for AP
generation. None of the neurons capable of generating APs in response to vagus nerve stimulation exhibited strong postsynaptic activation (i.e., a unitary EPSP large enough to exceed threshold for AP generation). Instead, multiple EPSPs were summed to generate an AP. Neurons generating vagally mediated EPSPs therefore must integrate synaptic inputs from multiple preganglionic axons to produce a regenerative output, a result that concords with the observations of Seabrook et al. (49) on vagal innervation of neurons in the neonatal rat heart. Those neurons responding with APs to vagal stimulation in the present study may in fact represent classical efferent parasympathetic neurons innervating the myocardium. If this is the case, it is interesting to note that these neurons did not represent the majority of intracardiac neurons sampled. Perfusion with a modied Tyrode solution containing reduced calcium and high magnesium levels (blocking release of neurotransmitter at nerve terminals) or exposure to the nicotinic channel blocker hexamethonium eliminated the postsynaptic effects of vagal nerve stimulation. These results demonstrate that the effects of nerve stimulation were mediated synaptically and imply that such stimulus-elicited depolarizations were produced by acetylcholine released from vagal preganglionic terminals and acting at nicotinic postsynaptic receptors. The latter nding agrees with that of Edwards et al. (21), who reported that the nicotinic receptor antagonist D-tubocurarine blocked vagal transmission to intracardiac neurons in the guinea pig atrium. Interestingly, Seabrook et al. (49), using the nicotinic receptor antagonist mecamylamine to block cholinergic neurotransmission, found that some intracardiac neurons had a residual postsynaptic response to vagal nerve stimulation and suggested that a noncholinergic neurotransmitter was coreleased from vagal preganglionic terminals in intracardiac ganglia. However, no evidence for this effect was found in the present study. Seventeen percent of intracardiac neurons in this study were dually innervated by axons in the right vagus and cardiopulmonary nerves; none of the neurons sampled received inputs exclusively from cardiopulmonary nerves. Two types of responses were recorded in these neurons. In type 1 responses, illustrated in Fig. 6, vagus nerve stimulation alone evoked EPSPs and an AP whereas cardiopulmonary nerve stimulation alone had no postsynaptic effect. Stimulation of cardiopulmonary and vagal nerves together broadened the duration of both the AP and the AHP compared with that produced by vagal stimulation alone. Because there was no direct postsynaptic effect of cardiopulmonary nerve stimulation, one possible explanation for this augmentation is that a neuroactive agent released from intraganglionic sympathetic terminals (possibly norepinephrine or a substance coreleased with this transmitter) could have acted presynaptically on vagal terminals to potentiate the release of acetylcholine. Higher acetylcholine concentrations within the synaptic cleft could then have been responsible for prolonging postsynaptic channel-opening times, thus leading to
Downloaded from ajpregu.physiology.org on January 2, 2012
EXTRINSIC INPUTS TO INTRACARDIAC NEURONS
R463
increased AP and AHP durations. The receptor types involved in this response remain unknown. In this study, type 1 responses were in the minority and were found in only two neurons. The majority of neurons inuenced by axons in cardiopulmonary nerves displayed type 2 responses: concomitant stimulation of cardiopulmonary nerves enabled ring of APs during vagal stimulation (Figs. 7 and 8). In these neurons, vagus nerve stimulation alone evoked depolarizations that were orthodromically mediated (eliminated by low-calcium, high-magnesium perfusate), were blocked by hexamethonium, and had electrophysiological properties (mean EPSP amplitude and duration, Table 3) similar to those produced by nerve stimulation in neurons innervated only by the vagus. EPSPs produced by cardiopulmonary nerve stimulation in dually innervated neurons with type 2 responses were signicantly smaller in amplitude and shorter in duration than those produced in the same neurons by vagal inputs, as summarized in Table 3. Nicotinic receptors were not involved in responses to cardiopulmonary nerve stimulation, as determined by stimulating these nerves during exposure to hexamethonium; this antagonist had no effect on the response to cardiopulmonary nerve stimulation either at a concentration that blocked all vagally mediated responses (100 M; Fig. 8) or at double this dose. However, the -antagonist timolol blocked postsynaptic responses to stimulation of cardiopulmonary nerves (Fig. 5), and exposure to hexamethonium and timolol together completely eliminated postsynaptic responses of these neurons to combined nerve stimulation (Fig. 8). Given the differences in the properties of EPSPs and the differential effects of cholinergic and adrenergic antagonists on the postsynaptic responses to vagus and cardiopulmonary nerve stimulation, it is clear that different synaptic mechanisms were activated by these inputs. Acetylcholine, released from vagal preganglionic terminals and acting at nicotinic postsynaptic receptors, likely mediated the effects produced by vagus nerve stimulation, whereas the adrenergic neurotransmitter norepinephrine, most likely released from postganglionic sympathetic terminals and acting at -adrenergic receptors, was involved in the effects of cardiopulmonary nerve stimulation. There have been several anatomic reports demonstrating the presence of sympathetic postganglionic nerve terminals in mammalian intracardiac ganglia (22, 43, 44), and the results of the present study constitute functional evidence that these terminals may be capable of modulating ganglionic neurotransmission when activated. Endogenously released or exogenously applied norepinephrine has been shown to affect ion conductances and thus membrane and ring properties of peripheral autonomic neurons, either facilitating or inhibiting ganglionic neurotransmission (1, 3, 17, 18, 45, 50). In the pig heart, Smith et al. (50) found that exogenously applied norepinephrine facilitated orthodromically mediated responses of some neurons to stimulation of intracardiac plexus nerves. In that study, it was proposed that facilitation could have
resulted either from direct postsynaptic effects of norepinephrine or through action at a presynaptic site. The observation of type 1 and 2 responses in the present study provides evidence that both of these mechanisms may be operative in intrinsic cardiac ganglia in the pig heart. Results of the present in vitro study also support the ndings of a previous study of the beating canine heart in vivo showing that adrenergic agonists applied locally to intracardiac ganglia enhanced the frequency of neuronal AP discharge (33). Clearly the facilitatory effects of exogenously applied adrenergic agents in the heart in vivo could have been operating by the same mechanism responsible for the excitatory effects of activating sympathetic inputs to intracardiac neurons seen in the present in vitro study. The results of the present experiments showing that the inuences of axons in vagus and cardiopulmonary nerves are mediated by cholinergic and adrenergic receptors, respectively, provide an insight into the issue of possible mixing of sympathetic and parasympathetic bers within individual extrinsic cardiac nerves. Some parasympathetic preganglionic bers innervating the mammalian heart have been reported to diverge from the vagus nerve in the neck to course with sympathetic nerves, joining the cervical sympathetic trunk, the middle cervical or stellate ganglia, or the ansae subclavia (29, 31). It is therefore possible that intracardiac neurons activated by stimulation of vagal and cardiopulmonary nerves in the present study may have been responding to parasympathetic preganglionic inputs running to the heart in both nerves. If this were the case, then the postsynaptic effect of activating parasympathetic axons in the cardiopulmonary nerves should have been eliminated by nicotinic blockade. However, because hexamethonium did not eliminate responses to cardiopulmonary nerve stimulation, these responses were likely not mediated by displaced vagal axons. There is also anatomic and functional evidence that sympathetic bers, originating from postganglionic neurons in the sympathetic chain, may reach the heart via the cardiac vagus (11, 35, 48) as well as the cardiopulmonary nerves. It is thus possible that stimulation of the vagus nerve in the present study could have activated some sympathetic postganglionic as well as parasympathetic preganglionic bers innervating intracardiac neurons. This also does not appear to be the case, since -adrenergic blockade had no effect on the postsynaptic responses of intracardiac neurons to vagus nerve stimulation. Although the number of neurons sampled in this study was limited, the data indicate that stimulation of the vagus nerve activated only parasympathetic inputs and cardiopulmonary nerve stimulation activated only sympathetic inputs to these neurons. This may not, however, be true for all intracardiac neurons. Intrinsic Neuron Properties and Correlation with Extrinsic Input Pattern Properties. There were no signicant differences between mean resting membrane potentials of the three neuron types (Table 1). Values reported in this study were consistent with the mean value of resting poten-
Downloaded from ajpregu.physiology.org on January 2, 2012
R464
EXTRINSIC INPUTS TO INTRACARDIAC NEURONS
tial reported in an earlier in vitro study of intracardiac neurons in the pig heart (50), with the value for R-type canine intracardiac neurons (55), and with mean values reported for guinea pig atrial neurons (21, 32). However, mean values of resting potential in the present study were smaller than those reported for neonatal rat intracardiac neurons (49), canine S-type intracardiac neurons (55), and phasic neurons in the guinea pig left atrium (27). The mean values for resting potential in these studies ranged roughly from 50 to 60 mV, and this variation is likely to be due at least partly to interspecies differences and possibly to differences in recording conditions (see Ref. 2 for discussion). Mean whole cell input resistance of phasic neurons in the present study was double that of accommodating and tonic neurons (Table 1), but resistance values for all neurons in this study were within the range of those reported for intracardiac neurons in a previous study of pig atrial neurons (50) and for atrial neurons of other species (21, 27, 49, 55, 56). The higher resistance (or lower membrane conductance) of phasic neurons in the present study implies that a smaller current would be required to depolarize the voltage-gated channels responsible for AP generation to threshold for ring in these neurons, compared with currents needed to depolarize lower-resistance neurons to ring threshold. This characteristic of phasic neurons, coupled with a threshold depolarization voltage for AP generation that was signicantly less than threshold voltages for accommodating and tonic neurons (Table 1), means that phasic neurons may be more excitable than the other types of intracardiac neuron. Mean time constants for the three cell types in the present study were statistically similar (Table 1) and were also similar to those reported for atrial neurons in other species (21, 27, 49, 50, 55, 56). Properties of the APs induced by intracellular stimulation in the three classes of neuron (with the exception of the signicantly lower threshold voltage for AP generation in phasic cells mentioned above) were not signicantly different. These properties were, moreover, similar to those reported for neurons in porcine (50), rat (49), and dog (55, 56) hearts. All neurons in the present study displayed prominent AHPs following single APs (Figs. 4 and 6). When mean amplitudes and durations of AHPs in the three groups of neurons were compared, the only signicant difference found was that mean AHP duration in tonic cells was more than twice the duration of AHPs in the other two groups of neurons (Table 1; Fig. 2). A similar difference was reported for AHP duration between S-type (phasically discharging, AHP 50-ms duration) and SAH and P-type (repetitively ring, AHP 200 ms) intracardiac neurons in the guinea pig heart (21). Correlations. In the present study there appears to be a correlation between neuron class (based on electrophysiological criteria) and pattern of innervation by extracardiac inputs. Data compiled by neuron class in Table 2 show that extrinsic vagal inputs appear to be routed to phasic and to some accommodating intracardiac neurons, whereas extrinsic sympathetic input
primarily targeted phasic neurons; most tonic neurons appeared to receive no extrinsic inputs. Several schemes have recently been proposed to classify peripheral autonomic neurons by functional criteria (summarized in Ref. 2), based either on the time course of the AHP following single intracellularly evoked APs (4, 15, 23, 56), ring behavior in response to long depolarizing currents injected through the recording electrode (26, 54), or a combination of both. In the present study, neurons have been divided into three classes based on their ring behavior in response to depolarization, as shown in Fig. 2. This scheme was adopted because of the implications of this intrinsic property for the potential roles of the different neuron types in controlling intracardiac neurotransmission. The existence of correlations between ring properties and patterns of extrinsic innervation of the three classes of neuron found in this study provides some insight into the potential roles of these neuron types in regulating the heart. Implicit in the use of this classication scheme is the concept that neurons with different ring behaviors are involved in different intracardiac functional pathways. In this respect, autonomic neurons with different types of ring behavior have been shown to participate in anatomically and functionally distinct pathways involved in visceral control (15, 23, 41, 42). Firing behavior is an important physiological characteristic that can at least partly determine the responses of neurons to ongoing high-frequency synaptic input sufficient to depolarize the cell membrane to ring threshold. Thus phasic and accommodating neurons would act as low-pass lters in the presence of sustained high-frequency synaptic input. Because the majority of intracardiac neurons receiving vagal preganglionic inputs in this study were phasic or accommodating, high levels of vagal preganglionic activity would result in the generation of only one or two APs or a brief decrementing burst of APs at the start of depolarization, depending on the neuron type. The output pathways of these neurons are as yet unknown, but if they mediate parasympathetic control of the myocardium, the rate of transganglionic transmission of impulses of extracardiac origin to effector sites would thus be subject to a low cut-off frequency even in the presence of strong, high-frequency preganglionic activity. This correlation is strengthened further when the pattern of innervation by axons in cardiopulmonary nerves is considered: neurons displaying type 2 responses were almost exclusively phasic, so parasympathetic neurotransmission to these neurons would be modulated by sympathetic inputs. The nding that none of the neurons expressing type 2 responses could be induced to re an AP through vagal drive alone suggests that these neurons were not in the pathway for direct efferent parasympathetic control of the myocardium. Indeed, inasmuch as these neurons only generated an output in response to the activation of both sympathetic and parasympathetic inputs, they may represent a special category of neuron concerned with intracardiac integration of information from both efferent limbs of the autonomic nervous
Downloaded from ajpregu.physiology.org on January 2, 2012
EXTRINSIC INPUTS TO INTRACARDIAC NEURONS
R465
system. On the other hand, some of the accommodating and all but one of the tonically discharging neurons in this study lacked extrinsic inputs, so presumably these cells would be activated primarily by inputs from sources intrinsic to the heart and may therefore be local-circuit neurons or interneurons (7, 8) involved in intracardiac reex loops. If this is the case, the highfrequency repetitive ring properties of these cells may help promote strong activation of such reex loops by feedback from intracardiac events. In the guinea pig heart, an alternate, sensory role for intracardiac neurons receiving no extrinsic inputs has been proposed (27). The existence of intracardiac sensory neurons has also been postulated in the hearts of other mammalian species (see Ref. 8 for review). In the present study, one-third of the neurons sampled were devoid of extrinsic inputs, raising the possibility that these neurons may be sensory in function. However, solid electrophysiological criteria for identifying intracardiac sensory neurons have not yet been established at the cellular level. Efferent axons of potential sensory neurons in the heart that might communicate with the central nervous system or intrathoracic ganglia would be expected to run in the extrinsic cardiac nerves and should have been antidromically activated by nerve stimulation, but no antidromically activated neurons were detected in the present study. As a side issue, data on AHP properties of intracardiac neurons may provide some insight into the relationship of AHP characteristics to neuronal ring behavior. It has been proposed that AHP duration may have a causal relationship with repetitive ring behavior in peripheral autonomic neurons (reviewed in Ref. 2). In cells with long-duration AHPs, it would be expected that repetitive ring in response to prolonged depolarization would be limited to a low frequency because of the time needed for membrane potential to recover to a value near the resting level. Phasically ring cells would therefore be expected to have longer AHPs than repetitively ring cells. However, this was not the case for phasic neurons either in the present study (Fig. 2, insets) or for phasic (S-type) cells in the guinea pig heart (21). It is thus possible that AHP duration per se may not be directly related to repetitive ring behavior. In response to intracellular depolarizing current in the tonic neuron illustrated in Fig. 2C, the initial interspike interval was 25 ms, yet the AHP duration of this neuron was close to the mean value of 130 ms for tonic cells (Table 1). In contrast, phasically discharging neurons in this study had a signicantly shorter mean AHP duration of 48 ms. The characteristics of the AHP and the capability for repetitive ring of a particular neuron type are set by the complement of ionic conductances present in the cell membrane (2, 4), but the results of the present study and those of Edwards et al. (21) indicate that in atrial neurons AHP characteristics and ring behavior may not be closely related. The membrane currents underlying these physiological properties in neurons in the pig heart have not been established.
In conclusion, this study shows that there exists a neuronal substrate within intracardiac ganglia for the convergence of inputs from vagal and cardiopulmonary cardiac nerves onto single intracardiac neurons. Vagal inputs to these neurons appear to be mediated by nicotinic postsynaptic receptors, whereas inputs from cardiopulmonary nerves appear to involve -adrenergic receptors. These convergent inputs can interact to modify the ring properties of intracardiac neurons. Evidence is presented to indicate that there may also be presynaptic modulation of vagal neurotransmission through intracardiac ganglia, mediated by inputs from cardiopulmonary nerves. The results presented here suggest that some interactions between sympathetic and parasympathetic inputs to the heart can occur at a premyocardial site within intracardiac ganglia. Inputs of extracardiac origin targeted phasic and some accommodating neurons, whereas other accommodating and almost all tonically ring neurons lacked extrinsic inputs. Analysis of the correlations between innervation pattern and electrophysiological properties of the three neuron types found in this study suggests that neurons of each type may play a distinct role in neuronal control of cardiac function. Perspectives The major issue addressed in this study was the possibility of vagosympathetic convergence on single intracardiac neurons. The identication of such neurons now raises further questions about the implications of this convergence for neural control of the heart. To evoke orthodromically mediated APs in dually innervated neurons, activation of both inputs was required because neither input was capable on its own of depolarizing these cells to threshold for ring. Neurons in this group must therefore integrate signals from both efferent limbs of the autonomic nervous system to produce an output. It may be that sympathetic inputs function to prime these neurons for ring by increasing their excitability, acting to increase neuronal sensitivity to succeeding vagal inputs. Alternatively, vagal inputs may function to prime sympathetically innervated neurons for ring. In any case, either input pathway may function as a gate, controlling transmission through the other pathway. In this way, these neurons may represent a major site for vagosympathetic interactions, allowing cooperation between these pathways in coordinating the neural regulation of cardiac function. One reex mechanism that could make use of such an integrative process is the cardiac response to increased atrial lling. In this condition sympathetic activity is reexly increased to elevate cardiac output by raising stroke volume and heart rate. However, strong sympathetic drive can elevate heart rate to a level too high for efficient ventricular ejection and it has been proposed that coactivation of vagal preganglionic cardiomotor axons would ensure that sympathetic overdrive does not result in heart rate exceeding the optimal level for maximizing cardiac output during increased atrial lling (36, 37). Intracardiac neurons that respond to inputs from both limbs of the autonomic nervous sys-
Downloaded from ajpregu.physiology.org on January 2, 2012
R466
EXTRINSIC INPUTS TO INTRACARDIAC NEURONS 12. Bojsen-Moller, F., and J. Tranum-Jensen. Whole-mount demonstration of cholinesterase-containing nerves in the right atrial wall, nodal tissue, and atrioventricular bundle of the pig heart. J. Anat. 108: 375386, 1971. 13. Calaresu, R. F., and A. J. St. Louis. Topography and numerical distribution of intracardiac ganglion cells in the cat. J. Comp. Neurol. 131: 5566, 1967. 14. Cannon, W. B. The Wisdom of the Body. New York: Norton, 1939. 15. Cassell, J. F., A. L. Clark, and E. M. McLachlan. Characteristics of phasic and tonic sympathetic ganglion cells of the guineapig. J. Physiol. (Lond.) 372: 457483, 1986. 16. Crowcroft, P. J., and J. H. Szurszewski. A study of the inferior mesenteric and pelvic ganglia of guinea-pigs with intracellular electrodes. J. Physiol. (Lond.) 219: 421441, 1971. 17. De Groat, W. C., and A. M. Booth. Inhibition and facilitation in parasympathetic ganglia of the urinary bladder. Federation Proc. 39: 29902996, 1980. 18. De Groat, W. C., and A. M. Booth. Synaptic transmission in pelvic ganglia. In: Nervous Control of the Urogenital System, edited by C. A. Maggi. Philadelphia, PA: Harwood, 1993, p. 291347. 19. De Groat, W. C., and W. R. Saum. Sympathetic inhibition of the urinary bladder and of pelvic ganglionic transmission in the cat. J. Physiol. (Lond.) 220: 297314, 1972. 20. Denenberg, V. H. Some statistical and experimental considerations in the use of the analysis-of-variance procedure. Am. J. Physiol. 246 (Regulatory Integrative Comp. Physiol. 15): R403 R408, 1984. 21. Edwards, F. R., G. D. S. Hirst, M. F. Klemm, and P. A. Steele. Different types of ganglion cell in the cardiac plexus of guineapigs. J. Physiol. (Lond.) 486: 453471, 1995. 22. Ellison, J. P., and R. G. Hibbs. An ultrastructural study of mammalian cardiac ganglia. J. Mol. Cell. Cardiol. 8: 89101, 1976. 23. Frieling, T., H. J. Cooke, and J. D. Wood. Electrophysiological properties of neurons in submucosal ganglia of guinea pig distal colon. Am. J. Physiol. 260 (Gastrointest. Liver Physiol. 23): G835G841, 1991. 24. Furukawa, Y., P. Martin, and M. N. Levy. AV junctional rhythm induced by sympathetic-parasympathetic imbalance in dog hearts. Am. J. Physiol. 259 (Heart Circ. Physiol. 28): H839 H842, 1990. 25. Glantz, S. A. Biostatistics: how to detect, correct and prevent errors in the medical literature. Circulation 61: 17, 1980. 26. Griffith, W. H., J. P. Gallagher, and P. Shinnick-Gallagher. An intracellular investigation of cat vesical pelvic ganglia. J. Neurophysiol. 43: 343354, 1980. 27. Hardwick, J. C., G. M. Mawe, and R. L. Parsons. Evidence for afferent ber innervation of parasympathetic neurons of the guinea-pig cardiac ganglion. J. Auton. Nerv. Syst. 53: 166174, 1995. 28. Hodgkiss, J. P., and G. M. Lees. Morphological studies of electrophysiologically-identied myenteric plexus neurons of the guinea pig ileum. Neuroscience 8: 593608, 1983. 29. Hopkins, D. A., and J. A. Armour. Medullary cells of origin of physiologically identied cardiac nerves in the dog. Brain Res. Bull. 8: 359362, 1982. 30. Hopkins, D. A., and J. A. Armour. Localization of sympathetic postganglionic and parasympathetic preganglionic neurons which innervate different regions of the dog heart. J. Comp. Neurol. 229: 186198, 1984. 31. Hopkins, D. A., P. M. Gootman, N. Gootman, S. M. Di Russo, and M. E. Zeballos. Brainstem cells of origin of the cervical vagus and cardiopulmonary nerves in the neonatal pig (Sus scrofa). Brain Res. 306: 6372, 1984. 32. Horackova, M., M. H. Huang, J. A. Armour, D. A. Hopkins, and C. Mapplebeck. Cocultures of adult ventricular myocytes with stellate ganglia or intrinsic cardiac neurons from guinea pigs: spontaneous activity and pharmacological properties. Cardiovasc. Res. 27: 11011108, 1993. 33. Huang, M. H., F. M. Smith, and J. A. Armour. Modulation of in situ canine intrinsic cardiac neuronal activity by nicotinic,
tem may thus act as dual-input gates capable of balancing sympathetic and parasympathetic drive in control of the heart. A parallel to this type of dual-input integration has been described in prevertebral ganglia that innervate pelvic organs (16, 19, 34), in which parasympathetic and sympathetic inputs interact at the level of postganglionic neurons to control their ring. In this system parasympathetic preganglionic inputs synapse directly on postganglionic neurons innervating pelvic end organs, while sympathetic inputs reach the same postganglionic neurons either directly (16) or indirectly via interneurons (18). Sympathetic and parasympathetic convergence within the pelvic ganglia appears to be a key factor in regulating pelvic organ function during changes in relative activity of the two limbs of the autonomic nervous system. Evidence in the present study for a similar type of convergence on intracardiac neurons suggests that sympathetic-parasympathetic interactions within cardiac ganglia, occurring at intracardiac neurons, may help balance the cardiac inuences of extrinsic autonomic inputs.
This research was supported by an operating grant from the Medical Research Council of Canada. The author is grateful to the Heart and Stroke Foundation of Canada for a Research Scholarship. Address for reprint requests: F. M. Smith, Dept. of Anatomy and Neurobiology, Faculty of Medicine, Dalhousie Univ., Halifax, Nova Scotia, Canada B3H 4H7. Received 7 July 1997; accepted in nal form 16 October 1998. REFERENCES 1. Adams, D. J., and Z. Xu. Norepinephrine and GTP S inhibit a calcium conductance and activate a nonselective cation conductance in rat parasympathetic cardiac neurons (Abstract). J. Gen. Physiol. 94: 1a2a, 1989. 2. Adams, J. A., and A. A. Harper. Electrophysiological properties of autonomic ganglion neurons. In: The Autonomic Nervous System. Autonomic Ganglia, edited by E. M. McLachlan. Reading, UK: Harwood, 1995, vol. 6, p. 153212. 3. Akasu, T., J. P. Gallagher, T. Nakamura, P. ShinnickGallagher, and M. Yoshimura. Noradrenaline hyperpolarization and depolarization in cat vesical parasympathetic neurones. J. Physiol. (Lond.) 361: 165184, 1985. 4. Allen, T. G., and G. Burnstock. Intracellular studies of the electrophysiological properties of cultured intracardiac neurones of the guinea-pig. J. Physiol. (Lond.) 388: 349366, 1987. 5. Anderson, R. H. The disposition, morphology and innervation of cardiac specialized tissue in the guinea-pig. J. Anat. 111: 453 468, 1972. 6. Anderson, R., G. Rama, and A. J. Theron. Membrane stabilizing, anti-oxidative interactions of propranolol and dexpropranolol with neutrophils. Biochem. Pharmacol. 52: 341349, 1996. 7. Ardell, J. L. Structure and function of mammalian intrinsic cardiac neurons. In: Neurocardiology, edited by J. A. Armour and J. L. Ardell. New York: Oxford University Press, 1994, p. 95114. 8. Armour, J. A. Peripheral autonomic neuronal interactions in cardiac regulation. In: Neurocardiology, edited by J. A. Armour and J. L. Ardell. New York: Oxford University Press, 1994, p. 219244. 9. Armour, J. A., and D. A. Hopkins. Activity of in vivo canine ventricular neurons. Am. J. Physiol. 258 (Heart Circ. Physiol. 27): H326H336, 1990. 10. Armour, J. A., and D. A. Hopkins. Activity of canine in situ left atrial ganglion neurons. Am. J. Physiol. 259 (Heart Circ. Physiol. 28): H1207H1215, 1990. 11. Balkowiec, A., and P. Szulczyk. Properties of postganglionic sympathetic neurons with axons in the right thoracic vagus. Neuroscience 48: 159167, 1992.
Downloaded from ajpregu.physiology.org on January 2, 2012
EXTRINSIC INPUTS TO INTRACARDIAC NEURONS muscarinic and -adrenergic agonists. Am. J. Physiol. 265 (Regulatory Integrative Comp. Physiol. 34): R659R669, 1993. Janig, W., and E. M. McLachlan. Organization of lumbar spinal outow to distal colon and pelvic organs. Physiol. Rev. 67: 13321404, 1987. Kamosinska, B., D. Nowicki, A. Szulczyk, and P. Szulczyk. Spinal segmental sympathetic outow to cervical sympathetic trunk, vertebral nerve, inferior cardiac nerve and sympathetic bres in the thoracic vagus. J. Auton. Nerv. Syst. 32: 199204, 1991. Koizumi, K., and M. Kollai. Multiple modes of operation of cardiac autonomic control: development of the ideas from Cannon and Brooks to the present. J. Auton. Nerv. Syst. 41: 1930, 1992. Koizumi, K., N. Terui, M. Kollai, and C. M. Brooks. Functional signicance of coactivation of vagal and sympathetic cardiac nerves. Proc. Natl. Acad. Sci. USA 79: 21162120, 1982. Levy, M. N. Autonomic interactions in cardiac control. Ann. NY Acad. Sci. 601: 209221, 1990. Loffelholz, K., and A. J. Pappano. The parasympathetic neuroeffector junction of the heart. Pharmacol. Rev. 37: 124, 1985. McKibben, J., and R. Getty. Innervation of heart of domesticated animals: pig. Am. J. Vet. Res. 30: 779789, 1969. McLachlan, E. M., and R. L. Meckler. Characteristics of synaptic input to three classes of sympathetic neurone in the coeliac ganglion of the guinea-pig. J. Physiol. (Lond.) 415: 109129, 1989. Meckler, R. L., and E. M. McLachlan. Axons of peripheral origin preferentially synapse with tonic neurones in the guinea pig coeliac ganglion. Neurosci. Lett. 86: 189194, 1988. Moravec, J., and M. Moravec. Intrinsic nerve plexus of mammalian heart: morphological basis of cardiac rhythmical activity? Int. Rev. Cytol. 106: 89148, 1987. Moravec, M., J. Moravec, and S. Forsgren. Catecholaminergic and peptidergic nerve components of intramural ganglia in the rat heart. An immunohistochemical study. Cell Tissue Res. 262: 315327, 1990. Nishi, S. Electrophysiological properties of sympathetic neurons. In: Autonomic and Enteric Ganglia, edited by A. G. Karczmar, K. Koketsu, and S. Nishi. New York: Plenum, 1986, p. 79106.
R467
34. 35.
36.
37. 38. 39. 40. 41.
42. 43. 44.
45.
46. Pirola, F. T., and E. K. Potter. Vagal action on atrioventricular conduction and its inhibition by sympathetic stimulation and neuropeptide Y in anaesthetized dogs. J. Auton. Nerv. Syst. 31: 112, 1990. 47. Potter, E. K., and L. G. Ulman. Neuropeptides in sympathetic nerves affect vagal regulation of the heart. News Physiol. Sci. 9: 174177, 1994. 48. Randall, W. C., D. V. Priola, J. B. Pace, and J. S. Wechsler. Ventricular augmentor bres in the cervical vagosympathetic trunk. Proc. Soc. Exp. Biol. Med. 124: 12541258, 1967. 49. Seabrook, G. R., L. A. Fieber, and D. J. Adams. Neurotransmission in neonatal rat cardiac ganglion in situ. Am. J. Physiol. 259 (Heart Circ. Physiol. 28): H997H1005, 1990. 50. Smith, F. M., D. A. Hopkins, and J. A. Armour. Electrophysiological properties of in vitro intrinsic cardiac neurons in the pig (Sus scrofa). Brain Res. Bull. 28: 715725, 1992. 51. Tay, S. S., W. C. Wong, and E. A. Ling. An ultrastructural study of the neuronal changes in the cardiac ganglia of the monkey (Macaca fascicularis) following unilateral vagotomy. J. Anat. 138: 6780, 1984. 52. Wallenstein, S., C. L. Zucker, and J. L. Fleiss. Some statistical methods useful in circulation research. Circ. Res. 47: 19, 1980. 53. Wallick, D. W., and P. J. Martin. Separate parasympathetic control of heart rate and atrioventricular conduction of dogs. Am. J. Physiol. 259 (Heart Circ. Physiol. 28): H536H542, 1990. 54. Weems, W. A., and J. H. Szurszewski. An intracellular analysis of some intrinsic factors controlling neural output from inferior mesenteric ganglion of guinea pigs. J. Neurophysiol. 41: 305321, 1978. 55. Xi, X., W. C. Randall, and R. D. Wurster. Electrophysiological properties of canine cardiac ganglion cell types. J. Auton. Nerv. Syst. 47: 6974, 1994. 56. Xi, X., J. X. Thomas, Jr., W. C. Randall, and R. D. Wurster. Intracellular recordings from canine intracardiac ganglion cells. J. Auton. Nerv. Syst. 32: 177182, 1991. 57. Zar, J. H. Biostatistical Analysis. Englewood Cliffs, NJ: PrenticeHall, 1984, p. 186191. 58. Zipes, D. P., M. N. Levy, L. A. Cobb, S. Julius, P. G. Kaufman, N. E. Miller, and R. L. Verrier. Sudden cardiac death. Neuralcardiac interactions. Circulation 76: I202I207, 1987.
Downloaded from ajpregu.physiology.org on January 2, 2012
Vous aimerez peut-être aussi
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- James Kent - Toward A Unified Theory of Psychedelic Action Or: "Hallucinogens and Recurrent Excitation in Cortical Circuitry"Document1 pageJames Kent - Toward A Unified Theory of Psychedelic Action Or: "Hallucinogens and Recurrent Excitation in Cortical Circuitry"GretymjPas encore d'évaluation
- Yuan Xiao-Ping Et Al - Spiral Wave Generation in A Vortex Electric FieldDocument4 pagesYuan Xiao-Ping Et Al - Spiral Wave Generation in A Vortex Electric FieldGretymjPas encore d'évaluation
- Georg Gottwald, Alain Pumir and Valentin Krinsky - Spiral Wave Drift Induced by Stimulating Wave TrainsDocument8 pagesGeorg Gottwald, Alain Pumir and Valentin Krinsky - Spiral Wave Drift Induced by Stimulating Wave TrainsGretymjPas encore d'évaluation
- Gang Hu Et Al - Controlling Spiral Waves in A Model of Two-Dimensional Arrays of Chua's CircuitsDocument4 pagesGang Hu Et Al - Controlling Spiral Waves in A Model of Two-Dimensional Arrays of Chua's CircuitsGretymjPas encore d'évaluation
- Ma Jun Et Al - Breakup of Spiral Waves in Coupled Hindmarsh-Rose NeuronsDocument4 pagesMa Jun Et Al - Breakup of Spiral Waves in Coupled Hindmarsh-Rose NeuronsGretymjPas encore d'évaluation
- Jun Ma Et Al - The Instability of The Spiral Wave Induced by The Deformation of Elastic Excitable MediaDocument11 pagesJun Ma Et Al - The Instability of The Spiral Wave Induced by The Deformation of Elastic Excitable MediaGretymjPas encore d'évaluation
- Removal of A Pinned Spiral by Generating Target Waves With A Localized StimulusDocument5 pagesRemoval of A Pinned Spiral by Generating Target Waves With A Localized StimulusGretymjPas encore d'évaluation
- Michael Jachan Et Al - Inferring Direct Directed-Information Flow From Multivariate Nonlinear Time SeriesDocument5 pagesMichael Jachan Et Al - Inferring Direct Directed-Information Flow From Multivariate Nonlinear Time SeriesGretymjPas encore d'évaluation
- Complex-Periodic Spiral Waves in Confluent Cardiac Cell Cultures Induced by Localized InhomogeneitiesDocument7 pagesComplex-Periodic Spiral Waves in Confluent Cardiac Cell Cultures Induced by Localized InhomogeneitiesGretymjPas encore d'évaluation
- KURENAI: Kyoto University Research Information RepositoryDocument5 pagesKURENAI: Kyoto University Research Information RepositoryGretymjPas encore d'évaluation
- Zhoujian Cao Et Al - Turbulence Control With Local Pacing and Its Implication in Cardiac DefibrillationDocument9 pagesZhoujian Cao Et Al - Turbulence Control With Local Pacing and Its Implication in Cardiac DefibrillationGretymjPas encore d'évaluation
- Hong Zhang Et Al - Control of Spiral Breakup by An Alternating Advective FieldDocument5 pagesHong Zhang Et Al - Control of Spiral Breakup by An Alternating Advective FieldGretymjPas encore d'évaluation
- Marcel Hörning Et Al - Wave Emission On Interacting Heterogeneities in Cardiac TissueDocument8 pagesMarcel Hörning Et Al - Wave Emission On Interacting Heterogeneities in Cardiac TissueGretymjPas encore d'évaluation
- Sitabhra Sinha Et Al - Critical Role of Inhomogeneities in Pacing Termination of Cardiac ReentryDocument10 pagesSitabhra Sinha Et Al - Critical Role of Inhomogeneities in Pacing Termination of Cardiac ReentryGretymjPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
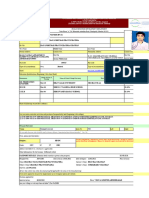
- HR 2 FormDocument8 pagesHR 2 Formrkpatel40Pas encore d'évaluation
- Varicose Vein and Its Homeopathic Cure - DR Bashir Mahmud ElliasDocument8 pagesVaricose Vein and Its Homeopathic Cure - DR Bashir Mahmud ElliasBashir Mahmud Ellias100% (2)
- Arterial Line Analysis PresentationDocument35 pagesArterial Line Analysis PresentationLisa GilbertPas encore d'évaluation
- San Marcelino Campus San Marcelino, Zambales: Ramon Magsaysay Technological UniversityDocument33 pagesSan Marcelino Campus San Marcelino, Zambales: Ramon Magsaysay Technological UniversityKristine Grace CachoPas encore d'évaluation
- Clinical Study: The Effects of Uncomplicated Cataract Surgery On Retinal Layer ThicknessDocument7 pagesClinical Study: The Effects of Uncomplicated Cataract Surgery On Retinal Layer ThicknessJohn ElfranPas encore d'évaluation
- Splice PDFDocument5 pagesSplice PDFpedroPas encore d'évaluation
- Science 6 Endocrine SystemDocument39 pagesScience 6 Endocrine Systemcharmaine_olivia_1100% (1)
- Mediclaim Policy - Buy Group Health Insurance Online - Future GeneraliDocument39 pagesMediclaim Policy - Buy Group Health Insurance Online - Future GeneraliRizwan KhanPas encore d'évaluation
- Garcia. Act 1 and 2 NUR103Document4 pagesGarcia. Act 1 and 2 NUR103Frances Katherine GarciaPas encore d'évaluation
- Agc332 Lecture 10-Wheat DiseasesDocument33 pagesAgc332 Lecture 10-Wheat DiseasesSolomon MbewePas encore d'évaluation
- ABSITE Killer PlusDocument16 pagesABSITE Killer PlusMark Soliman100% (1)
- Diazepam Drug StudyDocument1 pageDiazepam Drug StudyAndee Salegon100% (3)
- Multiple Pulp Polyps Associated With Deciduous TeethDocument4 pagesMultiple Pulp Polyps Associated With Deciduous TeethJea Ayu YogatamaPas encore d'évaluation
- Contact Lens Complications and ManagementDocument10 pagesContact Lens Complications and Managementstrawberry8832850% (2)
- Mental Disorder Due To AlcoholDocument18 pagesMental Disorder Due To AlcoholAnonymous Oj5JCpO5xPas encore d'évaluation
- Heart Disease and Cancer: CirculationDocument4 pagesHeart Disease and Cancer: CirculationDewi AyuPas encore d'évaluation
- CystsDocument5 pagesCystsranindita maulyaPas encore d'évaluation
- Aromatherapy For Professionals ENGDocument593 pagesAromatherapy For Professionals ENGcamelia100% (3)
- Latin Root Words ListDocument4 pagesLatin Root Words ListrbalakrPas encore d'évaluation
- Theory ApplicationDocument38 pagesTheory ApplicationAnusha VerghesePas encore d'évaluation
- Introduction of The Topic: Nano-BiotechnologyDocument7 pagesIntroduction of The Topic: Nano-BiotechnologyAbhishek YadavPas encore d'évaluation
- English Composition II 1Document11 pagesEnglish Composition II 1api-548473407Pas encore d'évaluation
- Pathomorphology MCQSDocument191 pagesPathomorphology MCQSNana BentilPas encore d'évaluation
- Ultimate Guide To Surviving in The WildDocument175 pagesUltimate Guide To Surviving in The WildSal Ot100% (1)
- CHN RLE Module 1M 3M With Self Assessment 1.2.3 of Rle Module 1mDocument62 pagesCHN RLE Module 1M 3M With Self Assessment 1.2.3 of Rle Module 1mPhilip Anthony Fernandez100% (1)
- How To Implement Health Technology Assessment - 230715 - 093605Document10 pagesHow To Implement Health Technology Assessment - 230715 - 093605Nour ElsabahPas encore d'évaluation
- Tof Care PlanDocument4 pagesTof Care Plankayal67% (12)
- Access To Primary Health Care Services For Indigenous PeopleDocument9 pagesAccess To Primary Health Care Services For Indigenous PeopleLawrence Ryan DaugPas encore d'évaluation
- Group Assignment Population EconomicsDocument7 pagesGroup Assignment Population EconomicsSayed Abdullah Shah SadaatPas encore d'évaluation
- HWC (SC) Nqas ChecklistDocument79 pagesHWC (SC) Nqas Checklistqa100% (1)