Académique Documents
Professionnel Documents
Culture Documents
Module7 Medicationswordpresentation
Transféré par
Yep YepDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Module7 Medicationswordpresentation
Transféré par
Yep YepDroits d'auteur :
Formats disponibles
*Administering Medications by Nasogastric or Gastrostomy Tube * PARENTERAL MEDICATIONS intradermally (ID) subcutaneously (SC or SQ) intramuscularly (IM) intravenously
(IV Equipment: syringes and needles to withdraw medication from ampules and vials. Syringes hypodermic syringe comes in 2-, 2.5-, and 3- mL sizes insulin syringe is similar to a hypodermic syringe, but the scale is specially design for insulin: a 100-unit calibrated scale intended for use with U-100 insulin - The correct choice of syringe is based on the amount of insulin required. tuberculin syringe - a narrow syringe, calibrated in tenths and hundredths of a milliliter (up to 1 mL) on one scale and sixteenths of a minim (up to 1 minim) on the other scale Syringes are made in other sizes as well (e.g., 5, 10, 20, and 50 mL). prefilled unit-dose systems. These are available as (a) prefilled syringes ready for use of (b) prefilled sterile cartridges and needles that require the attachment of a reusable holder (injection system) before use. Examples Tubex and Carpuject injection system. Needles A dull or damaged needle should never be used. Needles used for injections have three variable characteristics: 1. Slant or length of the bevel. - Longer bevels provide the sharpest needles and cause less discomfort. - commonly used for subcutaneous and intramuscular injections. - Short bevels are used for intradermal and intraveneous injections because a long bevel can become occluded if it rests against the side of the blood vessel. 2. Length of the shaft - 1/3 to 2 inches. the appropriate needle length is chosen according to the clients muscle development, the clients weight, and the type of injection. 3. Gauge (or diameter) of the shaft. - #18 to #28. The larger the gauge number, the smaller the diameter of the shaft. Smaller gauges produce less tissue trauma, but the larger gauges are necessary for viscous medications, such as penicillin. * For an adult requiring a subcutaneous injection, it is appropriate to use a needle of #24 to #26 gauge and 3/8 to 5/8 inch long. * Obese clients may require a 1-inch needle. * For intramuscular injections, a longer needle (e.g., 1 to 1 inches) with a larger gauge (e.g., #20 to # 22 gauge) is used.
*Slender adults and children usually require a shorter needle. The nurse must assess the client to determine the appropriate needle length. Preventing Needlestick Injuries Avoiding Puncture Injuries * Use appropriate puncture-proof disposal containers to dispose of uncapped needles and sharps. These are provided in all client areas. Never throw sharps in wastebaskets. Never bend or break needles before disposal. Never recap used needles except under specified circumstances (e.g., when transporting a syringe to the laboratory for an arterial blood gas or blood culture). When recapping needle: - Use a safety mechanical device that firmly grips the needle cap and holds it in place until it is ready for recap. - Use a one-handed scoop method. This is performed by (a) placing the needle cap and syringe with needle horizontally on a flat surface (b) inserting the needle into the cap, using one hand, and then (c) using your other-hand to pick- up the cap and tighten it to the needle hub. Preparing Injectable Medications Injectable medications can be prepared by withdrawing the medication from an ampule or vial into a sterile syringe, using prefilled syringes, or using needles injection systems. Ampule - a glass container usually designed to hold a single dose of a drug - made of clear glass and has a distinctive shape with a constricted neck - vary in size from 1 to 10 mL or more - Most ampule necks have colored marks around them, indicating where they are prescored for easy opening. Vial - a small glass bottle with a sealed rubber cap. vials come in different sizes, from single to multidose vials. They usually have a metal or plastic caps that protects the rubber seal. The following are two examples of the preparation of powdered drugs: 1. Single-dose vial: instructions for preparing a single-dose vila direct that 1.5 mL of sterile water be added to the sterile dry powder, thus providing a single dose of 2 mL. The volume of the drug powder was 0.5 mL. Therefore, the 1.5 mL of water plus the 0.5 mL of powder results in 2 mL of solution. In other instances, the addition of a solution does not increase the volume. Therefore, it is important to follow the manufacturers directions. 2. Multidose vial: a dose of 750 mg of a certain drug is ordered for a client. On hand is a 10-g multidose vial. The direction for preparation read: Add 8.5 mL of sterile water, and each milliliter will contain 1.0 g or 1,000 mg. To determine the amount to inject, the nurse calculate as follows: 1 mL = 1,000 mg x mL = 750 mg (cross multiply)
x = 750 x 1/ 1,000 x = 0.75 The nurse will give 0.75 mL of the medication. Preparing Medications from Ampules PLANNING Delegation Preparing medications from ampules and vials involves knowledge and use of aseptic technique. Therefore, these techniques are not delegated to UAP. Equipment - MAR or computer printout - Ampule of sterile medication - File (if ampule is not scored) and small gauze square - Antiseptic swabs - Needle and syringe - Filter needle IMPLEMENTATION Preparation 1. Check the medication administration order. - Check the label on the ampule carefully against the MAR to make sure that the correct medication is being prepared. - Follow the three checks for administering medication
(1) when it is taken from the medication cart. (2) before withdrawing the medication, and (3) after withdrawing the medication.
2. Organize the equipment. Performance Preparing Medications from Vials PLANNING Equipment - MAR or computer printout - Vial of sterile medication - Antiseptic swabs - Needle and syringe - Filter needle (check agency policy) - Sterile water or normal saline, if drug is in powdered form. IMPLEMENTATION Preparation - Same preparation as described in previous procedure Performance 1. Wash hands and observe other appropriate infection control procedures.
2. Prepare the medication vial for drug withdrawal. Mix the solution, if necessary, by rotating the vial between the palms of the hands, not by shaking. Some vials contain aqueous suspensions, which settle when they stand. In some instances, shaking is contraindicated because it may cause the mixture to foam. Remove the protective cap, or clean the rubber cap of a previously opened vial with an antiseptic wipe by rubbing in a circular motion. The antiseptic cleans the cap of dust or grease and reduces the number of microorganisms. 3. Withdraw the medication. Attach a filter needle, as agency practice dictates, to draw up premixed liquid medications from multidose vials. Using the filter needle prevents any solid particles from being drawn up through the needle. Ensures that the needle is firmly attached to the syringe. Remove the cap from the needle, then draw up into the syringe the amount of air equal to the volume of the medication to be withdrawn. Carefully insert the needle into the upright vial through the center of the rubber cap, maintaining the sterility of the needle. Inject the air into the vial, keeping the bevel of the needle above the surface of the medication. The air will allow the medication to be drawn out easily because negative pressure will not be created inside the vial. The bevel is kept above the medication to avoid creating bubbles in the medication. Withdraw the prescribed amount of medication using either of the following methods: 1. Hold the vial down (i.e., with the base lower than the top), move the needle tip so that it is below the fluid level, and withdraw the medication . Avoid drawing up the last drops of the vial. Proponents of this method say that keeping the vial in the upright position while withdrawing the medication allows particulate matter to precipitate out of the solution. Leaving the last few drops reduces the chance of withdrawing foreign particles. Or 2. Invert the vial; ensure the needle tip is below the fluid level; and gradually withdraw the medication. Keeping the tip of the needle below the fluid level prevents air from being drawn into the syringe. Hold the syringe and vial at eye level to determine that the correct dosage of drug is drawn into the syringe. Eject air remaining at the top of the syringe into the vial. When the correct volume of medication is obtained, withdraw the needle from the vial, and replace the cap over the needle using the scoop method, thus maintaining its sterility. If necessary, tap the syringe barrel to dislodge any air bubbles present in the syringe. The tapping motion will cause the air bubbles to rise to the top of the syringe where they can be ejected out of the syringe. Replace the filter needle, if used with a regular needle and cover of the correct gauge and length before injecting the client.
VARIATION: PREPARING AND USING MULTIDOSE VIALS Read the manufacturers directions. Withdraw an equivalent amount of air from the vial before adding the diluent, unless otherwise indicated by the directions. Add the amount of sterile water or saline indicated in the directions.
If a multidose vial is reconstituted, label the vial with the date and time it was prepared, the amount of drug contained in each milliliter of solution, and your initials. Time is an important factor to consider in the expiration of these medications. Once the medication is reconstituted, store it in a refrigerator or as recommended by the manufacturer.
MIXING MEDICATIONS USING ONE SYRINGE PLANNING Delegation Mixing medications in one syringe involves knowledge and use of aseptic technique. Therefore, this procedure is not delegated to UAP. Equipment MAR or computer printout Two vials of medication; one vial and one ampule; two ampules; or one vial or ampule and one cartridge Antiseptic swabs Sterile hypodermic or insulin syringe and needle (if insulin is being given, use a small-gauge hypodermic needle, e.g.,#26 gauge) Additional sterile subcutaneous or intramuscular needle (optional) IMPLEMENTATION Preparation 1. Check the MAR. Check the label on the medications carefully against the MAR to make sure that the correct medication is being prepared. Follow the three checks for administering medications. Read the label on the medication (1) when it is taken from the medication cart, (2) before withdrawing the medication, and (3) after withdrawing the medication. Before preparing and combining the medications, ensure that the total volume of the injection is appropriate for the injection site. 2. Organize the equipment. Performance 1.Wash hands and observe other appropriate infection control procedures. 2.Prepare the medication ampule or vial for drug withdrawal. See Procedure 33-2, step 2, for an ampule Inspect the appearance of the medication for clarity. Some medications are always cloudy. Preparations that have changed in appearance should be discarded. If using insulin, thoroughly mix the solution in each vial prior to administration. Rotate the vials between the palms of the hands and invert the vials. Mixing ensures an adequate concentration and thus an accurate dose. Shaking insulin vials can make the medication frothy, making precise measurement difficult. Clean the tops of the vials with antiseptic swabs. 3. Withdraw the medications.
INTRADERMAL INJECTIONS An intradermal (ID) injection is the administration of a drug into the dermal layer of the skin just beneath the epidermis. Usually only a small amount of liquid is used, for example, 0.1 mL. This method of administration is frequently used for allergy testing and tuberculosis (TB) screening. Common sites for intradermal injections are the inner lower arm, the upper chest, and the back beneath the scapulae. The left arm is commonly used for TB screening and the right arm is used for all other tests. ADMINISTERING AN INTRADERMAL INJECTION Purpose To provide a medication that the client requires for allergy testing and TB screening ASSESSMENT Assess Appearance of injection site Specific drug action and expected response Clients knowledge of drug action and response Check agency protocol about sites to use for skin tests. PLANNING Delegation Equipment Vial or ampule of the correct medication Sterile 1-mL syringe calibrated into hundredths of a milliliter (i.e., tuberculin syringe) and a # 25- to #27- gauge needle that is to 5/8 inch long Alcohol swabs 2-in. x 2-in. sterile gauze (optional) clean gloves (according to agency protocol) bandage (optional) epinephrine (a bronchodilator and antihistamine) on hand IMPLEMENTATION Preparation 1. Check the MAR. Check the label on the medication carefully against the MAR to make sure that the correct medication is being prepared Follow the three checks for administering medication 1. When it is taken from the medication cart 2. Before withdrawing the medication 3. After withdrawing the medication 2. Organize the equipment
Performance 1. Wash hands and observe other appropriate infection control procedures (eg clean gloves) 2. Prepare the medication from the vial or ampule for drug withdrawal 3. Prepare the client Check the clients identification band. This ensures that the right client receives the medication 4. Explain to the client that the medication will produce a small wheal, sometimes called a bleb. A wheal is a small raised area, like a blister. The client will feel a slight prick as the needle enters the skin. Some medications are absorbed slowly through the capillaries into the general circulation, and the bleb gradually disappears. Other drugs remain in the area and interact with the body tissues to produce redness and induration (hardening), which will need to be interpreted at a particular time (e.g., in 24 or 48 hours). This reaction will also gradually disappear. Information facilitates acceptance of and compliance with the therapy. 5. Provide for client privacy. 6. Select and clean the site. Select a site (like the forearm about a hands width above the wrist and three or four fingerwidths below the antecubital space). Avoid using sites that are tender, inflamed, or swollen and those that have lesions. Put on gloves as indicated by agency policy. Cleanse the skin at the site using firm circular motion starting at the center and widening the circle outward. Allow the area to dry thoroughly. 7. Prepare the syringe for the injection. Remove the needle cap while waiting for the antiseptic to dry. Expel any air bubbles from the syringe. Small bubbles that adhere to the plunger are of no consequence. A small amount of air will not harm the tissues. Grasp the syringe in your dominant hand, holding it between thumb and forefinger. Hold the needle almost parallel to the skin surface, with the bevel of the needle up. The possibility of the medication entering the subcutaneous tissue increases when using an angle greater than 15 degrees if the bevel is down. 8. Inject the fluid. * With the nondominant hand, pull the skin at the site until it is taut. For example, if using the ventral forearm, grasp the clients dorsal forearm and gently pull it to tighten the ventral skin. Taut skin allows for easier entry of the needle and less discomfort for the client. Insert the tip of the needle far enough to place the bevel through the epidermis into the dermis. The outline of the bevel should be visible under the skin surface. Stabilize the syringe and needle; inject the medication carefully and slowly so that it produces a small wheal on the skin. This verifies that the medication entered the dermis. Withdraw the needle quickly at the same angle at which it was inserted. Apply a bandage if indicated. Do not massage the area. Massage can disperse the medication into the tissue or out through the needle insertion site. Dispose of the syringe and needle safely. Do not recap the needle in order to prevent needlestick injuries. Remove gloves. Circle the injection site with the ink to observe for redness or induration (hardening), per agency policy.
9. Document all relevant information. Record the testing material given, the time, dosage, route, site, and nursing assessments. EVALUATION Evaluate the clients response to the testing substance. Some medications used in the testing may cause allergic reaction. An antidote drug (e.g., epinephrine) may need to be used. Evaluate the condition of the site in 24 or 48 hours, depending on the test. Measure the area of redness in indurations in millimeters at the largest diameter and document findings. SUBCUTANEOUS INJECTIONS Kinds of drugs administered subcutaneously (just beneath the skin) are: vaccines, preoperative medications, narcotics, insulin, and heparin. Common sites for subcutaneous (SC or SQ) injections are the outer aspect of the thighs. - These areas are convenient and normally have good blood circulation. - Other areas that can be used are the abdomen, the scapular areas. Only small doses (0.5 to 1 mL) of medications are usually injected via the subcutaneous route. Check agency policy. The type of syringe used for subcutaneous injections depends on the medication to be given. Generally a 2-mL syringe is used for most SC injections. - if insulin is being administered, an insulin syringe is used - if heparin is being administered, a tuberculin syringe or prefilled cartridge may be used. Needle sizes and lengths are selected based on the clients body mass, the intended angle of insertion, and the planned site. Generally a #25-gauge, 5/8-inch needle is used for adults of normal weight and the needle is inserted at a 45-degree angle; a 3/8-inch needle is used at a 90-degree angle - A child may need a1/2-inch needle inserted at a 45-degree angle. - One method nurses used to determine length of needle is to pinch the tissue at the site and select a needle length that is half the width of the skinfold. To determine the angle of insertion, a general rule to follow relates to the amount of tissue that can be bunched or grasped at the site. A 45-degree angle is used when 1 inch of tissue can be grasped at the site; A 90-degree angle is used when 2-inches of tissue can be grasped. Procedure: Administering a Subcutaneous Injection INTRAMUSCULAR INJECTIONS Injections into muscle tissue, or intramuscular (IM) injections, are absorbed more quickly than subcutaneous injections because of the greater blood supply to the body muscles. Muscles can also take a larger volume of fluid without discomfort than subcutaneous tissues can, although the amount varies among individuals, chiefly muscle size and condition and with the size used. An adult with well-developed muscles can usually safely tolerate up to 4 mL of medication in the gluteus medius and gluteus maximus muscles. A volume of 1 to 2 mL is usually recommended for adults with less developed muscles. In the deltoid muscle, volumes of 0.5 to 1 mL are recommended. Usually a 2- to 5-mL syringe is needed. The size of syringe used depends on the amount of medication being administered. The standard prepackaged intramuscular needle is 1 inches and #21 or #22 gauge. Several factors indicate the size and length of the needle to be used:
The muscle The type of solution The amount of adipose tissue covering the muscle The age of the client. For example, a smaller needle such as a #23- to #25-gauge needle 1 inch long is commonly used for the deltoid muscle. More viscous solutions require a larger gauge (e.g., #20 gauge). Very obese clients may require a needle longer than 1 1/2 inches (e.g., 2 inches) and emaciated clients mat require a shorter needle (e.g., 1 inch). A major consideration in the administration of intramuscular injections is the selection of a safe site located away from large blood vessels, nerves, and bone. Several body sites can be used for intramuscular injections. These sites are discussed in detail next. Contraindications for using a specific site include tissue injury and the presence of nodules, lumps, abscesses, tenderness, or other pathology. Ventrogluteal Site Vastus Lateralis Site Dorsogluteal Site Deltoid Site Rectus Femoris Site IM Injection Technique The Z-track method has been found to be less painful than the traditional injection technique INTRAVENOUS MEDICATIONS - appropriate when a rapid effect is required. - appropriate when medications are too irritating to tissues to be given by other routes. - When an intravenous line is already established, this route is desirable because it avoids the discomfort of other parenteral routes. * Medications are administered intravenously by the following methods: Large-volume infusion of intravenous fluid. Intermittent intravenous infusion (piggyback or tandem setups) Volume-controlled infusion (often used for children) Intravenous push or bolus Intermittent injection ports (device) Large-Volume Infusions Mixing a medication into a large-volume IV container is the safest and easiest way to administer a drug intravenously. The drugs are diluted in volumes of 1,000 mL or 500 mL of compatible fluids. It may be necessary to consult a pharmacist to confirm compatibility. Fluids such as IV normal saline or Rangers lactate are frequently used. Commonly added drugs are potassium chloride and vitamins. It may also be necessary to ensure the compatibility of some drugs with the plastic IV bag and tubing. A glass IV bottle and special tubing may be used in special situations. The main danger of infusing a large volume of fluid is circulatory overload (hypervolemia). The medication can be added to the fluid container that is running or before it is hung and infusing. In some hospitals the pharmacist adds the medication to the container. Adding Medications to Intravenous Fluid Containers Intravenous Push
TOPICAL MEDICATIONS A topical medication is applied locally to the skin or to mucous membranes in areas such as: Eye external ear canal nose vagina rectum A particular type of topical or dermatologic medication delivery system is the transdermal patch. This system administers sustained-action medication (e.g., nitroglycerin, estrogen, and nicotine) via mulitlayered films containing the drug and adhesive layer. - The rate of delivery of the drug is controlled and varies with each product (e.g., from 12 hours to 1 week). - applied to a hairless, clean area of skin that is not subject to excessive movement or wrinkling (i.e., the trunk or lower abdomen) - It may also be applied on the side, lower back, or buttocks. - Patches should not be applied to areas with cuts, burns or abrasions, or on distal parts of extremities (e.g., the forearms). - If hair is likely to interfere with patch adhesion or removal, clipping may be necessary before application. SKIN APPLICATIONS Topical skin or dermatologic preparations include ointments, pastes, creams, lotions, powders, sprays, and patches. Before applying a dermatologic preparation, thoroughly clean the area with soap and water and dry it with a patting motion. APPLYING SKIN PREPARATIONS Powder Make sure the skin surface is dry. Spread apart any skin folds and sprinkle the site until the are is covered with a fine thin layer. Cover the site with a dressing if ordered Suspension-Based Lotion Shake the container before use to distribute suspended particles. Put a little lotion on a small gauze dressing or pad, and apply the lotion to the skin by stroking it evenly in direction of the hair growth. Creams, Ointments, Pastes, and Oil-Based Lotions Warm and soften the preparation in gloved hands to make it easier to apply and to prevent chilling (if a large area is to be treated). Smear it evenly over the skin using long stroke that follow the direction of the hair growth. Explain that the skin may feel somewhat greasy after application. Apply a sterile dressing if ordered by the physician. Aerosol Spray
Shake the container well to mix the contents hold the spray container at the recommended distance from the area (usually about 15-30 cm [6-12 inches] but check the label). Cover the clients face with a towel if the upper chest or neck is to be sprayed. Spray the medication over the specified area. Transdermal Patches Select a clean, dry area that is free of hair and matches the manufacturers recommendations. Remove the patch from its protective covering, holding it without touching the adhesive edges and apply it by pressing firmly with the palm of the hand for about 10 seconds. Advise the client to avoid using a heating pad over the area to prevent an increase in circulation and the rate of absorption. Remove the patch at the appropriate time folding the medicated side to the inside so it is covered. OPTHALMIC MEDICATIONS - Medications may be administered to the eye using irrigations or instillations. - An eye irrigation is administered to wash out the conjunctival sac to remove secretions or foreign bodies or to remove chemicals that may injure the eye. - Medications for the eyes, called ophthalmic medications are instilled in the form of liquids or ointments. - Eye drops are packaged in monodrip plastic containers that are used to administer the preparation - Ointment are usually supplied is small tubes. OTIC MEDICATIONS Instillations or irrigations of the external auditory canal are referred to as otic and generally carried out for cleaning purposes. Sometimes applications of heat and antiseptic solutions are prescribed. Irrigation performed in a hospital require aseptic technique so that microorganisms will not be introduced into the ear. Sterile technique is used if the eardrum is perforated. The position of the external auditory canal varies with age. In the child under 3 years of age, it is directed upward. In the adult, the external auditory canal is an S-shaped structure about 2.5 cm (1 inch) long. The procedure below explains how to administer otic instillations. Variation: Ear Irrigation NASAL MEDICATIONS Nasal instillations (nose drops and sprays) usually are instilled for their astringent effect (to shrink swollen mucous membranes), to loosen secretions and facilitate drainage, or to treat infections of the nasal cavity or sinuses. Nasal decongestants are the most common nasal instillation. Many of theses products are available without a prescription. Clients need to be taught to use these agents with caution. Chronic use of nasal decongestants may lead to a rebound effect, that is, an increase in nasal congestion. If excess decongestant solution is swallowed, serious systemic effects may also develop, especially in children. Nasal drops are used to treat sinus infections. Clients need to learn ways to position themselves to effectively treat an affected sinus: To treat the ethmoid and sphenoid sinuses, instruct the client to lie back with the head over the edge of the bed or a pillow under the shoulder so that the head is tipped backward. To treat the maxillary and frontal sinuses, instruct the client to assume the same back-lying position, with the head turned toward the side to be treated. The client should also be instructed
to (a) breathe through the mouth to prevent aspiration of the medication into the trachea and brochi, (b) remain in a back-lying position for at least 1 minute so that the solution will come into contract with all of the nasal surface, and (c) avoid blowing the nose for several minutes. VAGINAL MEDICATIONS Vaginal medications, or instillations, are inserted as creams, jellies, foams, or suppositories to treat infection or to relieve vaginal discomfort (e.g., itching or pain). Medical aseptic technique is usually used. Vaginal creams, jellies, and foams are applied by using a tabular applicator with a plunger. Suppositories are inserted with the index finger of a gloved hand. Suppositories are designed to melt at body temperature, so they are generally stored in the refrigerator to keep them firm for insertion. See Procedure for administering vaginal instillations. A vaginal irrigation (douche) is the washing of the vagina by a liquid at a low pressure. Vaginal irrigations are not necessary for ordinary female hygiene but are used to prevent infection by applying an antimicrobial solution that discourages the growth of microorganisms, to remove an offensive or irritating discharge, and to reduce inflammation or prevent hemorrhage by the application of heat or cold. In hospitals sterile supplies and equipment are used; in a home, sterility is not usually necessary because people are accustomed to the microorganisms in their environments. Sterile technique, however, is indicated if there is an open wound. SUPPOSITORY Lubricate the rounded (smooth) end of the suppository, which is inserted first. Lubrication facilitates insertion. Lubricate your gloved index finger. Expose the vaginal orifice by separating the labia with your nondominant hand. Insert the suppository about 8 to 10 cm (3 to 4 in.)along the posterior wall of the vagina, or as far as it will go. The posterior wall of the vagina is about 2.5 cm (1 in.) longer than the anterior wall because the cervix protrudes into the uppermost portion of the anterior wall. Ask the client to remain lying in the supine position for 5 to 10 minutes following insertion. The hips may also be elevated on a pillow. This position allows the medication to flow onto the posterior fornix after it has melted. VAGINAL CREAM, JELLY, OR FOAM Gently insert the applicator about 5 cm (2 in.). Slowly push the plunger until the applicator is empty Remove the applicator and place it on the towel. The applicator is put on the towel to prevent the spread of microorganisms. Discard the applicator if disposal or clean it according to the manufacturers directions. Ask the client to remain lying in the supine position for 5 to 10 minutes following the insertion. IRRIGATION RECTAL MEDICATIONS Insertion of medications into the rectum in the form of suppositories is a frequent practice. Rectal administration is a convenient and safe method of giving certain medications. Advantages include the following: It avoids irritation of the upper gastrointestinal tract in clients who encounter this problem.
It is advantageous when the medication has an objectionable taste or odor. The drug is released at slow but steady rate. Rectal suppositories are thought to provide higher bloodstream levels (titers) of medication because the venous blood from the lower rectum is not transported through the liver. To insert a rectal suppository: Assist the client to a left lateral position, with the upper leg flexed. Fold back the top bedclothes to expose the buttocks. Put on a glove on the hand used to insert the suppository. Unwrap the suppository and lubricate the smooth rounded end, or see manufactures instructions. The rounded end is usually inserted first and lubricant reduces irritation of the mucosa. Lubricate the glove index finger. Encourage the client to relax by breathing through the mouth. This usually relaxes the external and sphincter. Insert the suppository gently into the cannal, rounded end first (according to manufacturers instructions), along the rectal wall using the gloved index finger. For an adult, insert the suppository beyond the internal sphincter (i.e., 10 cm [4 in]). Avoid embedding the suppository in feces in order for the suppository to be absorbed effectively. Press the clients buttocks together for a few minutes. Ask the client to remain in the left lateral or supine position for at least 5 minutes to help retain the suppository. The suppository should be retained for at least 30 to 40 minutes or according to manufacturers instructions. RESPIRATORY INHALATION Nebulizers deliver most medications administered through the inhaled route. A nebulizer is used to deliver a fine spray (fog or mist) o medication or moisture to a client. There are two kinds of nebulization: atomization and aerosolization. In atomization, a device called atomizer produces rather large droplets for inhalation. In aerosolization, the droplets are suspended in a gas, such as oxygen. The smaller the droplets, the further they can be inhaled for the nasal mucosa, it is inhaled through the nose; when it is intended for the trachea, bronchi, and/or lungs, it is inhaled through the mouth. A large-volume nebulizer can provide a heated or cool mist. It is used for long-term therapy, such as that following a tracheostomy. The ultrasonic nebulizer provides 100% humidity and can provide particles small enough to be inhaled deeply into the respiratory tract. The meter-dose inhaler (MDI), a handheld nebulizer is pressurized container of medication through a nosepiece or mouthpiece. The force with which the air moves through the nebulizer causes the large particles of medicated solution to break up into finer particles, forming a mist or fine spray. To ensure correct delivery of the prescribed medication by MDIs, nurses need to instruct the client to use aerosol inhalers correctly. The client compresses the medication canister by hand to release medication through a mouthpiece. An extender or spacer maybe attached to the mouthpiece to facilitate medication absorption for better results. Spacers are holding chambers into which the medication is fired and from which the client inhales, so that the dose is not lost by exhalation. The Teaching: Client Care feature provides instruction for clients about using an MDI. Newer breath-activated MDIs are being produced in which inhalation triggers there lease of a premeasured dose of medication. CLINICAL ALERT
A clients ability to use an MDI correctly decreases over time (Togger & Brenner, 2001). It is important for the nurse to continuously assess if the client is using the MDI correctly. Teaching: Client Care Using a Metered-Dose Inhaler Make sure the canister is firmly and fully inserted into the inhaler. Remove the mouthpiece cap and, holding the inhaler upright, shake the inhaler vigorously for 3 to 5 seconds to mix the medication evenly. Exhale comfortably (as in a normal full breath). Hold the canister upside down. i. Hold the MDI 2 to 4 cm (1 to 2 in.) from the open mouth ii. Put the mouthpiece far enough into the mouth with its opening toward the throat. Close the lips tightly around the mouthpiece. An MDI with a spacer or extender is always placed in the mouth. Administering the Medication Press down once on the MDI canister (which releases the close) and inhale slowly and deeply through the mouth. Hold your breath for 10 seconds. This allows the aerosol to reach deeper airways. Remove the inhaler from or away from the mouth. Exhale slowly through pursed lips. Controlled exhalation keeps the small airways open during exhalation. Repeat the inhalation if ordered. Wait 20 to 30 seconds between inhalations of bronchodilator medications so the first inhalation has a chance to work and the subsequent dose reaches deeper into the lungs. After the inhalation is completed, rinse mouth with tap water to remove any remaining medication and reduce irritation and risk of infection. Clean the MDI mouthpiece after each use. Use mild soap and water, rinse it, and let it air dry before replacing it on the device. Store the canister at room temperature. Avoid extremes of temperature. Report adverse reactions such as restlessness, palpitations, nervousness, or rash to the physician. Many MDIs contain steroids for an anti-inflammatory effect. Prolonged use increases the risk of fungal infections in the mouth. Home Care Considerations Metered-Dose Inhalers Disinfect the metered-dose inhaler mouthpieces weekly by soaking for 20 minutes in 1 pint of water with 2 ounces of vinegar added. Teach clients how to determine the amount of medication remaining in a metered-dose inhaler canister: i. Calculate the number of days doses in a canister. Divide the number of doses (puffs) in the canister (on the label) by the number of puffs taken per day. According to Togger and Brenner (2001), this is the only accurate method. The previous method of floating the canister in water is not accurate because some
of the propellant may remain (even after the medication is gone), which leads the client to incorrectly believe he is receiving medication. Review instructions for using an inhaler spacer or chamber. Research shows that these devices assist in delivering the medication deeply into the lungs rather than only to the oropharynx.
IRRIGATIONS An irrigation (lavage) is the washing out of the body cavity by a stream of water or other fluid that may or may not be medicated. Irrigation is performed for one or more of the following reasons: To clean the area, that is, to remove a foreign object or excessive secretions or discharge To apply heat or cold To apply a medication, such as an antiseptic To reduce inflammation To relieve discomfort Surgical asepsis is required when there is a break in the skin (e.g., in a wound irrigation) or whenever a sterile body cavity (e.g., the bladder) is entered. Some irrigations (e.g., a vaginal, rectal, or gastric irrigation) are often safely conducted using medical asepsis. Different kinds of syringe are used for irrigations. The most common are the Asepto and the rubber bulb. The syringe are often calibrated, permitting the nurse to determine the amount of irrigant being delivered at any given time. The Asepto syringe is a plastic (or glass) syringe with a rubber bulb produces negative pressure, and fluid can be sucked into the syringe. When the bulb is squeezed again, the fluid is ejected from the syringe. Asepto syringe come in several sizes ranging from 30 mL (1 oz) to 120 mL (4 oz). The rubber bulb syringe is often used for irrigating the ears. Like the Asepto syringe, the rubber bulb syringe comes in a range of sizes. Other syringes that can be used are the piston syringe, which has a tip to which a catheter can be attached, and the Pomeroy syringe. Catheters may be used for deep-wound irrigations and for some types of bladder irrigations. The Pomeroy syringe is a metal syringe commonly used for ear irrigations. A shield near the tip prevents the solution from spraying outward. Plastic squeezable bottles are also available for irrigations. These are commonly used for perineal irrigations and some wound irrigations. The type, amount, temperature, and strength of the solution and the frequency of the irrigation are ordered by the physician. Generally, normal saline at body temperature (37c [98.6F]) is used unless specified otherwise. The amount of solution used varies with the site and purpose of the irrigation.
http://www.umassmed.edu/diabeteshandbook/chap08.htm http://www-instruct.nmu.edu/nursing/asanford/Pictures/ http://www.drugs.com/PDR/Heparin_Sodium_Injection__USP.html http://cop.utmem.edu/pharmacy/phsc212/PHSC_212_16.html http://www.miami-med.com/ear_wash_system.htm http://www.med.umich.edu/1libr/aha/aha_supposit_art.htm
Vous aimerez peut-être aussi
- Historical and Philosophical Perspective of Guidance Power PointDocument12 pagesHistorical and Philosophical Perspective of Guidance Power PointYep Yep60% (5)
- Patrick Meyer Reliability Understanding Statistics 2010Document160 pagesPatrick Meyer Reliability Understanding Statistics 2010jcgueinj100% (1)
- Preparing MedicationsDocument18 pagesPreparing MedicationsJuliezel IringanPas encore d'évaluation
- Psychomotor Skills Activity On Parenteral Routes of Drug AdministrationDocument15 pagesPsychomotor Skills Activity On Parenteral Routes of Drug AdministrationEmerson QuimbaPas encore d'évaluation
- InjectionDocument67 pagesInjectionSudhadKPas encore d'évaluation
- Administration of Parenteral MedicationsDocument6 pagesAdministration of Parenteral Medicationsjoel david knda mjPas encore d'évaluation
- Administering Intravenous (IV) Medication - OSCE Guide - Geeky MedicsDocument7 pagesAdministering Intravenous (IV) Medication - OSCE Guide - Geeky MedicslortifukkuPas encore d'évaluation
- InjectionDocument29 pagesInjectionIlham S. GaniPas encore d'évaluation
- Im Self InjectionDocument9 pagesIm Self InjectionInc hrgPas encore d'évaluation
- Administering Oral MedicationDocument25 pagesAdministering Oral MedicationAngelo P. VeluzPas encore d'évaluation
- Finals Pharmaco LabDocument24 pagesFinals Pharmaco LabAubrey Nicole MacapagalPas encore d'évaluation
- Parenteral MedicationDocument36 pagesParenteral Medicationmam "o"Pas encore d'évaluation
- Aspirating Drugs From Ampules and VialsDocument9 pagesAspirating Drugs From Ampules and VialsmariallenPas encore d'évaluation
- Preparing Med From A Vial ChecklistDocument5 pagesPreparing Med From A Vial ChecklistRalf FiedalinoPas encore d'évaluation
- PDF 1Document101 pagesPDF 1Ma. Ferimi Gleam BajadoPas encore d'évaluation
- Parenteral Medication Step by Step ProcedureDocument8 pagesParenteral Medication Step by Step ProcedureAubrey De GraciaPas encore d'évaluation
- Ward 29 Guide To The Safe Preparation and Administration of Intravenous (IV) Antibiotics at HomeDocument18 pagesWard 29 Guide To The Safe Preparation and Administration of Intravenous (IV) Antibiotics at HomeSebut Saja MawarPas encore d'évaluation
- Giving Subcutaneous InjectionDocument6 pagesGiving Subcutaneous Injection100WejdanPas encore d'évaluation
- Medication Administration (Guide)Document6 pagesMedication Administration (Guide)Alane MorenoPas encore d'évaluation
- Parenteral MedicationDocument36 pagesParenteral Medicationupendrabpkihs100% (2)
- Subkutan InjeksiDocument5 pagesSubkutan InjeksiAnggrian Clara DewiPas encore d'évaluation
- Withdrawing Medication From An Ampule: EquipmentDocument6 pagesWithdrawing Medication From An Ampule: EquipmentMj Andayog100% (1)
- Parenteral Doasge Forms-1Document8 pagesParenteral Doasge Forms-1vikilsoni2Pas encore d'évaluation
- Appendix 5 - Factsheet - AstraZeneca - MDV - Preparation - 16 April 2021Document10 pagesAppendix 5 - Factsheet - AstraZeneca - MDV - Preparation - 16 April 2021Atawit SomsiriPas encore d'évaluation
- Hospital Report by P.LDocument16 pagesHospital Report by P.LArchie CabachetePas encore d'évaluation
- Parenteral Catheterization Enema ChecklistDocument8 pagesParenteral Catheterization Enema ChecklistJessoliver GalvezPas encore d'évaluation
- Good Practice GuideDocument8 pagesGood Practice GuideRiana WindiariPas encore d'évaluation
- Parenteral Routes of Administration&Dosage FormsDocument8 pagesParenteral Routes of Administration&Dosage FormsSonal SoniPas encore d'évaluation
- Skills Enhancement Medication PrepDocument2 pagesSkills Enhancement Medication PrepEllayza OperanaPas encore d'évaluation
- Obat Injeksi Parenteral AdministrationDocument43 pagesObat Injeksi Parenteral Administrationlistya dewiPas encore d'évaluation
- MedicationsDocument40 pagesMedicationsqopcyrus10Pas encore d'évaluation
- Procedure For Insertion of Saf T Intima Cannula and Subcutaneous InjectionDocument16 pagesProcedure For Insertion of Saf T Intima Cannula and Subcutaneous Injectionmadimadi11Pas encore d'évaluation
- Procedure Checklist Chapter 37, Skill 37-01: Reconstituting and Withdrawing Medication From A VialDocument2 pagesProcedure Checklist Chapter 37, Skill 37-01: Reconstituting and Withdrawing Medication From A VialNursyNursePas encore d'évaluation
- Giving Subcutaneous InjectionsDocument6 pagesGiving Subcutaneous Injectionsmushroom620Pas encore d'évaluation
- Intramuscular Injection: 1-DefinitionDocument11 pagesIntramuscular Injection: 1-DefinitionkingPas encore d'évaluation
- Administering Intradermal InjectionDocument17 pagesAdministering Intradermal InjectionPattPas encore d'évaluation
- 37 ( (L P0oracyzvw7Document7 pages37 ( (L P0oracyzvw7CRISTINE DELPas encore d'évaluation
- Trans Health Injection GuideDocument30 pagesTrans Health Injection GuideLukas BerredoPas encore d'évaluation
- Subcutaneous InjectionDocument5 pagesSubcutaneous InjectionNovita sariPas encore d'évaluation
- Drawing Up InsluinDocument4 pagesDrawing Up InsluinÀi ZìjǐPas encore d'évaluation
- Module-Intradermal Etool PDFDocument7 pagesModule-Intradermal Etool PDFErika Danalle ArceoPas encore d'évaluation
- B12-Self-Injecting ..Document3 pagesB12-Self-Injecting ..RuDe ZiRlPas encore d'évaluation
- Administering MedicationDocument13 pagesAdministering MedicationOfficially RandomPas encore d'évaluation
- Administering Z-Track Injection: Prepared By: Paul Allen Gabriel R. Tablico, RN, ManDocument9 pagesAdministering Z-Track Injection: Prepared By: Paul Allen Gabriel R. Tablico, RN, ManJamesClaveriaPas encore d'évaluation
- AmpuleDocument2 pagesAmpulethadzamingPas encore d'évaluation
- Parenteral Medication AdministrationDocument19 pagesParenteral Medication AdministrationMadhavi ModaPas encore d'évaluation
- Observation Competence Checklist For Administration of An Intramuscular InjectionDocument24 pagesObservation Competence Checklist For Administration of An Intramuscular InjectionNada S'jPas encore d'évaluation
- Chapter 64 - Administration of Injectable MedicationsDocument11 pagesChapter 64 - Administration of Injectable Medicationskristie donaldPas encore d'évaluation
- Activity 2 Updated MurilloDocument22 pagesActivity 2 Updated MurilloAraw GabiPas encore d'évaluation
- Procedure Checklist Chapter 23: Administering Subcutaneous MedicationsDocument2 pagesProcedure Checklist Chapter 23: Administering Subcutaneous Medicationsmacs_smacPas encore d'évaluation
- 2 Intramuscular InjectionDocument5 pages2 Intramuscular InjectionKEANNA ZURRIAGAPas encore d'évaluation
- Medication Administration LabDocument9 pagesMedication Administration Labapi-688305379Pas encore d'évaluation
- Intra Muscular Injection in ChildrenDocument9 pagesIntra Muscular Injection in ChildrenssPas encore d'évaluation
- College of Nursing: (Dalubhasaan NG Narsing)Document5 pagesCollege of Nursing: (Dalubhasaan NG Narsing)Honey VargasPas encore d'évaluation
- IM Injuction: Definition of Intramuscular InjectionDocument8 pagesIM Injuction: Definition of Intramuscular InjectiondhanasundariPas encore d'évaluation
- Rle Lectures Medications: Arturo G. Garcia JR RN, MSN, U.S RNDocument33 pagesRle Lectures Medications: Arturo G. Garcia JR RN, MSN, U.S RNMaria Paula Amor GeronimoPas encore d'évaluation
- Procedure Checklist Chapter 23: Mixing Medications in One Syringe, Using A Prefilled Cartridge and Single-Dose Vial - For Intravenous AdministrationDocument2 pagesProcedure Checklist Chapter 23: Mixing Medications in One Syringe, Using A Prefilled Cartridge and Single-Dose Vial - For Intravenous AdministrationjthsPas encore d'évaluation
- Drug Preparation: (Ampule and Vial)Document25 pagesDrug Preparation: (Ampule and Vial)Ron Lucernas MayugaPas encore d'évaluation
- Insulin Injection Tutorial ExmDocument13 pagesInsulin Injection Tutorial ExmAslah NabilahPas encore d'évaluation
- Reading Guide CH 10Document3 pagesReading Guide CH 10Mariana PuyuPas encore d'évaluation
- Pipettes and Their Safely UseDocument14 pagesPipettes and Their Safely UseTapeshwar Yadav100% (1)
- Dimensional Analysis For Nursing StudentsD'EverandDimensional Analysis For Nursing StudentsPas encore d'évaluation
- Chain of Infection 2Document35 pagesChain of Infection 2Yep YepPas encore d'évaluation
- H.A LAB - Midterm H.ADocument6 pagesH.A LAB - Midterm H.AYep YepPas encore d'évaluation
- Breast CareDocument20 pagesBreast CareAna100% (3)
- PartographDocument6 pagesPartographYep Yep100% (2)
- Objective.: 1. A) B) C) D) 2. A) B) C) D) 3. A) B) C) D)Document7 pagesObjective.: 1. A) B) C) D) 2. A) B) C) D) 3. A) B) C) D)Yep YepPas encore d'évaluation
- Learning Outcomes Content Learning Strategies Resources Assessment Classroom RLE Skills Lab Clinical CommunityDocument1 pageLearning Outcomes Content Learning Strategies Resources Assessment Classroom RLE Skills Lab Clinical CommunityYep YepPas encore d'évaluation
- F.A. 3 Health AssessmentDocument3 pagesF.A. 3 Health AssessmentYep YepPas encore d'évaluation
- F.A. 5 Health AssessmentDocument6 pagesF.A. 5 Health AssessmentYep YepPas encore d'évaluation
- COPAR LectureDocument57 pagesCOPAR LectureYep Yep100% (2)
- F.A. 2 Health AssessmentDocument2 pagesF.A. 2 Health AssessmentYep YepPas encore d'évaluation
- TFN F.A. Module 1Document4 pagesTFN F.A. Module 1Yep YepPas encore d'évaluation
- CVP PPPDocument13 pagesCVP PPPYep Yep100% (1)
- NCM Renal DisordersDocument72 pagesNCM Renal DisordersYep Yep100% (1)
- WAQF Podium Design Presentation 16 April 2018Document23 pagesWAQF Podium Design Presentation 16 April 2018hoodqy99Pas encore d'évaluation
- Case CapsuleDocument8 pagesCase CapsuleLiza BulsaraPas encore d'évaluation
- Chapter 2Document13 pagesChapter 2Kumkumo Kussia KossaPas encore d'évaluation
- Neonatal Mortality - A Community ApproachDocument13 pagesNeonatal Mortality - A Community ApproachJalam Singh RathorePas encore d'évaluation
- Assistant Cook Learner Manual EnglishDocument152 pagesAssistant Cook Learner Manual EnglishSang Putu Arsana67% (3)
- Canoe Matlab 001Document58 pagesCanoe Matlab 001Coolboy RoadsterPas encore d'évaluation
- An Evaluation of MGNREGA in SikkimDocument7 pagesAn Evaluation of MGNREGA in SikkimBittu SubbaPas encore d'évaluation
- Micro EvolutionDocument9 pagesMicro EvolutionBryan TanPas encore d'évaluation
- Delusion in SocietyDocument2 pagesDelusion in SocietyGasimovskyPas encore d'évaluation
- Antena TelnetDocument4 pagesAntena TelnetMarco PiambaPas encore d'évaluation
- Catedral de SevillaDocument28 pagesCatedral de SevillaAnonymous LkgNmKePas encore d'évaluation
- Quarter 1-Week 2 - Day 2.revisedDocument4 pagesQuarter 1-Week 2 - Day 2.revisedJigz FamulaganPas encore d'évaluation
- Anemia in PregnancyDocument5 pagesAnemia in PregnancycfgrtwifhPas encore d'évaluation
- Meno's Paradox of Inquiry and Socrates' Theory of RecollectionDocument10 pagesMeno's Paradox of Inquiry and Socrates' Theory of RecollectionPhilip DarbyPas encore d'évaluation
- Week 4 - Theoretical Framework - LectureDocument13 pagesWeek 4 - Theoretical Framework - LectureRayan Al-ShibliPas encore d'évaluation
- Department of Education: Republic of The PhilippinesDocument1 pageDepartment of Education: Republic of The PhilippinesJonathan CayatPas encore d'évaluation
- Design of Penstock: Reference Code:IS 11639 (Part 2)Document4 pagesDesign of Penstock: Reference Code:IS 11639 (Part 2)sunchitk100% (3)
- Cambridge IGCSE™: Information and Communication Technology 0417/13 May/June 2022Document15 pagesCambridge IGCSE™: Information and Communication Technology 0417/13 May/June 2022ilovefettuccinePas encore d'évaluation
- Apron CapacityDocument10 pagesApron CapacityMuchammad Ulil AidiPas encore d'évaluation
- Lieh TzuDocument203 pagesLieh TzuBrent Cullen100% (2)
- Interlocking Block TechnologyDocument15 pagesInterlocking Block TechnologyChaula Trivedi100% (5)
- RFID Seminar AbstractDocument2 pagesRFID Seminar Abstractanushabhagawath80% (5)
- Activity On Noli Me TangereDocument5 pagesActivity On Noli Me TangereKKKPas encore d'évaluation
- W25509 PDF EngDocument11 pagesW25509 PDF EngNidhi SinghPas encore d'évaluation
- Rajiv Gandhi University of Health Sciences, Bengaluru, KarnatakaDocument9 pagesRajiv Gandhi University of Health Sciences, Bengaluru, KarnatakaNavin ChandarPas encore d'évaluation
- SachinDocument3 pagesSachinMahendraPas encore d'évaluation
- SweetenersDocument23 pagesSweetenersNur AfifahPas encore d'évaluation
- Phytotherapy On CancerDocument21 pagesPhytotherapy On CancerSiddhendu Bhattacharjee100% (1)
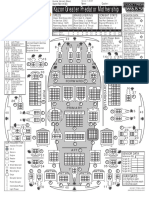
- Kazon Greater Predator MothershipDocument1 pageKazon Greater Predator MothershipknavealphaPas encore d'évaluation