Académique Documents
Professionnel Documents
Culture Documents
Conventional and Alternative Pharmaceutical Methods To Improve Oral Bio Availability of Lipophilic Drugs
Transféré par
raju1559405Description originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Conventional and Alternative Pharmaceutical Methods To Improve Oral Bio Availability of Lipophilic Drugs
Transféré par
raju1559405Droits d'auteur :
Formats disponibles
Asia n Jou r n a l of
Pha rm aceut ics
Re v ie w Ar t icle s
CONVENTIONAL AND ALTERNATIVE PHARMACEUTICAL METHODS TO IMPROVE ORAL BIOAVAILABILITY OF LIPOPHILIC DRUGS
BHUPENDRA G. PRAJAPATI AND MADHABHAI M. PATEL
S. K. Patel College Of Pharmaceutical Education & Research, Ganpat Vidyanagar, Ganpat University, Kherva. Pin: 382711, Mehsana, Gujarat, India. E-mail: bhupen_27@yahoo.co.in and bhupen27@gmail.com. ABSTRACT Out of new ly discov er ed dr ugs m or e t hen 40 % dr ugs ar e lipophilic and out of w hich up t o 40 % of pharmacologically active new molecules failed to reach to market only due to little or no water solubility; a serious challenge for the successful development and commercialization of new drugs in the pharmaceutical industry. Therefore various formulation strategies have been investigated to improve the solubilit y and t he r at e of dissolut ion t o enhance t he or al bioav ailabilit y of lipophilic dr ugs. I n t he pr esent review the different approaches discussed to overcome this problem, and successfully deliver the lipophilic drug for mankind. Keywords: Lipophilic, bioavailability, dissolution, solubility
INTRODUCTION
It is one of the major challenges to synthesize any new molecule, which is pharmacologically active for the researchers and pharmaceutical companies. It not only takes a long time but also consumes a lot of money. Out of this research around 40% of lipophilic drug candidates fail to reach market although exhibiting potential pharmacodynamic activities.
1, 2
Although pharmaceutical companies have been able to overcome difficulties with very slightly soluble drugs, those with aqueous solubility of less than 0.1 mg/ml present some unique challenges. These drugs are particularly good candidates for advanced solubilization technologies developed by companies specializing in drug delivery. These strategies include the solubilization and surfactants, the use of different polymorphic/ amorphic drug forms, the reduction of drug particle size, the complexation (e.g., cyclodextrins) and the formation of solid drug solutions/dispersions.4,
5
No matter how ac-
tive or potentially active a new molecular entity (NME) is against a particular molecular target, if the NME is not available in solution at the site of action, it is not a viable development candidate. As a result, the development of many exciting NMEs is stopped before their potential is realized or confirmed because pharmaceutical companies cannot afford to conduct rigorous preclinical and clinical studies on a molecule that does not have a sufficient pharmacokinetic profile due to poor water solubility. Even some of the lipophilic drugs on the market have to be administered at high doses. More than 90% of drugs approved since 1995 have poor solubility, poor permeability, or both 3. A marketed drug with poor water solubility can still show performance limitations, such as incomplete or erratic absorption, poor bioavailability, and slow onset of action. Effectiveness can vary from patient to patient, and there can be a strong effect of food on drug absorption. Finally, it may be necessary to increase the dose of a poorly soluble drug to obtain the efficacy required.
Volume 1, Issue 1, April - June, 2007 1
Solubilization and Surfactants
One approach to increase the bioavailability of lipophilic drugs is the solubilization of the drugs by means of pH adjustment, cosolvent, microemulsification, self-emulsification, micelles, liposomes and emulsions.6 Each has its advantages and limitations.
pH adjustment
pH adjustment is the simplest and most commonly used method to increase water solubility of ionizable compounds. However, this salt formation is infeasible for unionized compounds. The formed salts may also converse to respective acid or base forms in gastrointestinal-tract (GIT).
Colsolvent
Colsolvents are the mixtures of miscible solvents often
Asia n Jou r n a l of
Pha rm aceut ics
used to solubilize lipophilic drugs. The solubilizing excipients used in commercially available oral and injectable formulations are listed in Table 1. Currently, the water-soluble organic solvents are polyethylene glycol 400 (PEG 400), ethanol, propylene glycol, and glycerin. For example, Procardia (nifidipine) was developed by Pfizer contains glycerin, peppermint oil, PEG 400 and sodium saccharin in soft gelatin capsules. The waterinsoluble solvents include long-chain triglycerides (i.e. peanut oil, corn oil, soybean oil, sesame oil, olive oil, peppermint oil, hydrogenated vegetable oil and hydrogenated soybean oil), medium-chain triglycerides (Miglyol 812), beeswax, d-a- tocopherol (vitamin E) and oleic acid. Progesterone is a water-insoluble steroid and is solubilized in peanut oil (Prometrium).
Re vie w Ar t icle s
few parameters have been proposed to characterize the self-emulsifying performance including the rate of emulsification, the emulsion size distribution and the charge of resulting droplets. Among them, emulsion droplet size is considered to be a decisive factor in selfemulsification/ dispersion performance, since it determines the rate and extent of drug release and absorption.11 In addition, positively charged emulsion droplets could be obtained by incorporation of a small amount of cationic lipid (oleylamine) into such system.
10, 12
The oral en-
bioavailability of progesterone was significantly
hanced in rats by forming positively charged emulsion in comparison to the corresponding negatively charged formulation.
12
One of the advantages of SEDDS in relation to scale-up
Microemulsion
Microemulsion is a thermodynamically stable iso-tropical dispersion composed of a polar solvent, oil, a surfactan t an d a cosurfactan t. Th e form ation of microemulsions is spontaneous and does not involve the input of external energy. One theory considers negative interfacial tension while another considers swollen micelles. The surfactant and the cosurfactant alternate each other forming a mixed film at the interface contributin g to the stabil ity of the mi croemu lsion. Microemulsions are potential drug delivery systems for poorly water-soluble drugs due to their ability to solubilize the drugs in the oil phase, thus increasing their dissolution rate. 7 Even if the microemulsions are diluted after oral administration below the critical micelles concentration (CMC), the resultant drug precipitates have a fine particle size allowing enhanced absorption.8
and manufacture is that they form spontaneously upon mixing their components under mild agitation and they are thermodynamically stable. The drawbacks of this system include chemical instabilities of drugs and high surfactant concentrations. The large quantity of surfactant in self-emulsifying formulations (30-60%) irritates GIT. Consequently, the safety aspect of the surfactant vehicle had to be considered. Moreover, volatile cosolvents in the conventional self-emulsifying formulations are known to migrate into the shells of soft or hard gelatin capsules, resulting in the precipitation of the lipophilic drugs. As an example of self-emulsification, Neoral is composed of ethanol, corn oil-monoditriglycerides, Cremophor RH 40 and propylene glycol. It exhibits less variability and better drug uptake compared to Sandimmune. There is a long list of water soluble, insoluble and surfactants, which can use as solubilizing excipients.
13
Self Emulsification
In the absence of external phase (water), the mixture of oil, surfactant, cosurfactant, one or more hydrophilic solvents and cosolvent forms a transparent isotropic solution that is known as the self-emulsifying drug delivery system (SEDDS). This forms fine O/W emulsions or microemulsions spontaneously upon dilution in the aqueous phase and is used for improving lipophilic drug dissolution and absorption
9, 10
Polymeric Modification (Polymorphs)
Polymorphs are different crystalline forms of a drug that may have different physicochemical properties and biological activities, such as shelf-life, melting point, vapor pressu re, sol ubil ity,
14, 15
morphology,
den si ty
and
bioavailability.
Metastable forms are associated with
15, 16
The self-emulsification
higher energy with increased surface area, subsequently solubility, bioavailability and efficacy. With regard to bioavailability, it is preferable to change drug from crystal forms into metastable or amorphous forms. However, the possibility of a conversion of the high energy amorphous or metastable polymorph into a low energy crystal form having low solubility cannot be ruled out
2 Volume 1, Issue 1, April - June, 2007
process is specific to the nature of the oil/surfactant pair, surfactant concentration, oil/surfactant ratio and temperature at which self-emulsification occurs. The ease of emulsification could be associated with the ease of water penetrating into the various liquids crystalline or gel phases formed on the surface of the droplet. A
Asia n Jou r n a l of
Pha rm aceut ics
during manufacture and storage. It is preferable to develop the most thermodynamically stable polymorph of the drug to assure reproducible bioavailability of the product over its shelf-life under a variety of real-world storage conditions. For instance, ritonavir is the active ingredient in Norvir, a protease inhibitor used to treat HIV/AIDS. It was launched by Abbott Laboratories in 1996 as an amorphous semisolid dispersion consisting of medium chain triglycerides, polyoxyl 35 castor oil, citric acid, ethanol, polyglycolyzed glycerides, polysorbate 80, propylene glycol and 100 mg of ritonavir. The dissolution and the oral bioavailability were decreased due to crystallization of amorphous ritonavir into an insoluble crystal form during storage. This polymorph (form II) was 50% less soluble than the original form in the market, and caused the drug to fail its regulatory dissolution specifications. Finally, the drug was relaunched with the form II polymorph in a soft gelatin formulation that required refrigeration. Therefore, it is important to note that the selection of a polymorph of a drug should balance between solubility and stability to maintain its potency over the shelf-life period.
Re vie w Ar t icle s
Overall in general the limitation of the pearl milling process is the introduction of contamination to the product from the grinding material, batch-to-batch variations and the risk of microbiological problems after milling in an aqueous environment.
High-pressure homogenization
DissoCubes manufacture involves dispersing a drug powder in an aqueous surfactant solution and passing through a high-pressure homogenizer, subsequently nanosuspensions are obtained. The cavitation force experienced is sufficient to disintegrate drug from microparticles to nanoparticles. The particle size is dependent on the hardness of the drug substance, the processing pressure and the number of cycles applied. The possible interesting features of nanosuspensions are, 18: Increase in saturation solubility and dissolution rate of drug Increase in adhesive nature, thus resulting in enhanced bioavailability Increase the amorphous fraction in the particles, leading to a potential change in the crystalline structure and higher solubility Possibili ty of surface modi fi cation of
Particle Size Reduction
Micronization or nanonization is one of the most promising approaches to improve the bioavailability of lipophilic drugs by an increase in surface area and saturation solubility via reduction of the particle size to less than 1 .10 Such size reduction cannot be achieved by the conventional milling techniques. Patented engineering processes have come up based on the principles of pearl milling (NanoCrystals), high-pressure homogenization (DissoCubes), solution enhanced dispersion by supercritical fluids (SEDS), rapid expansion from supercritical to aqueous solution (RESAS), spray freezing into liquid (SFL) and evaporative precipitation into aqueous solution (EPAS).
17
nanosuspensions for site-specific delivery Possibility of large-scale production, the prerequisite for the introduction of a delivery system to the market However, only brittle drug candidates might be broken up into nanoparticles by this technique. A few points has to be considered, such as chemical instability of fragile drugs under the harsh production conditions, Ostwald ripening in long-term storage, toxicity of surfactants, redispersibility of the dried powder, batch-to-batch variation in crystallinity level and finally the difficulty of quality control and the stability of the partially amorphous nanosuspensions.
Pearl milling
Based on pearl milling the drug microparticles are ground to nanoparticles (< 400 nm) in between the moving milling pearls. The milling efficiency is dependent on the properties of the drug, the medium and the stabilizer. Rapamune, an immune suppressant agent, is the first FDA approved nanoparticle drug using NanoCrystals technology developed by Elan Drug Delivery. Emend is another product containing 80 or 125 mg aprepitant formulated by this technique.
Volume 1, Issue 1, April - June, 2007 3
Solution enhanced dispersion by the supercritical fluids (SEDS)
The SEDS process was developed and patented by the
Asia n Jou r n a l of
Pha rm aceut ics
University of Bradford.19 The use of a coaxial nozzle provides a means whereby the drug in the organic solvent solution mixes with the compressed fluid CO2 (antisolvent) in the mixing chamber of the nozzle prior to dispersion, and flows into a particle-formation vessel via a restricted orifice. Such nozzle achieves solution breakup through the impaction of the solution by a higher velocity fluid. The high velocity fluid creates high frictional surface forces, causing the solution to disintegrate into droplets. A wide range of materials has been prepared as carriers of microparticles and nanoparticles using the SEDS process
19
Re vie w
face area and excellent wettability.25
Ar t icle s
amorphous nanostructured aggregates with high sur-
Evaporative precipitation into aqueous solution (EPAS)
The EPAS process utilizes rapid phase separation to nucleate and grow nanoparticles and microparticles of lipophilic drugs. The drug is first dissolved in a low boiling point organic solvent. This solution is pumped through a tube where it is heated under pressure to a temperature above the solvent's boiling point and then sprayed through a fine atomizing nozzle into a heated aqueous solution. Surfactants are added to the organic solution and the aqueous solution to optimize particle formation and stabilization. In EPAS, the surfactant migrates to the drug-water interface during particle formation, and the hydrophilic segment is oriented towards the aqueous continuous phase.4 The hydrophilic stabilizer on the surface inhibits crystallization of the growing particles and therefore facilitates dissolution rates.
. A key step in the formation
of nanoparticles is to enhance the mass transfer rate between the droplets and the antisolvent before the droplets coalesce to form bigger droplets. In another study, a significant decrease in the particle size is achi ev ed by u si ng the ul trason ic nozz le-based supercritical antisolvent process.20,
21
Rapid expansion from supercritical to aqueous solution (RESAS)
This process induces rapid nucleation of the supercritical fluid dissolved drugs and surfactants resulting in particle formation with a desirable size distribution in a very short time. The surfactants in the supercritical fluid stabilize the newly formed small particles and suppress any tendency of particle agglomeration or particle growth when spraying this solution (drug + surfactant + CO2) into an aqueous solution containing a second surface modifier.22,
23
Complexation
Cyclodextrins and their derivatives have been employed as complexing agents to increase water solubility, dissolution rate and bioavailability of lipophilic drugs for oral or parenteral delivery.26 The solubility enhancement factors of pancratistatin, hydrocortisone, and paclitaxel are 7.5, 72.7 and 99000 by forming complexes with cyclodextrin derivatives.27 The lower the aqueous solubility of the pure drug, the greater the relative solubility enhancement obtained through cyclodextrin complexation. Pharmaceutical applications of cyclodextins in drug solubilization and stabilization 27, in vivo drug delivery 28 , toxicological issues and safety evaluation and mechanisms of cyclodextrins modifying drug release from polymeric drug delivery systems have been previously reviewed. Commercially available cyclodextrin based pharmaceutical products enumerated in Table 1 and many are waiting for approval.29 Cyclodextrins are a group of cyclic oligosaccharides obtained from enzymatic degradation of starch. The three major cylcodextins -, -, and - (CD) are composed of six, seven, and eight D(+)-glucopyranose units. These agents have a torus structure with primary and secondary hydroxyl groups orientated outwards. Consequently, cyclodextrins have a hydrophilic exterior and a hydrophobic internal cavity. This cavity enables cyclodextrins to complex guest drug molecules and hence alters the properties of the drugs such as solubility, stability, bioavailability and toxicity
4 Volume 1, Issue 1, April - June, 2007
The low solubility of poorly water soluble
drugs and surfactants in supercritical CO2 and the high pressure required for these processes restrict the utility of this technology in pharmaceutical industry.
Spray freezing into liquid (SFL)
The SFL technology was developed and patented by the University of Texas at Austin in 2003 and commercialized by the Dow Chemical Company. This technique involves atomizing an aqueous, organic, aqueous-organic cosolvent solution, aqueous-organic emulsion or suspension containing a drug and pharmaceutical excipients directly into a compressed gas (i.e. CO2, helium, propane, ethane), or the cryogenic liquids (i.e. nitrogen, argon, or hydrofluoroethers). The frozen particles are then lyophilized to obtain dry and free-flowing micronized powders
24
. Using of acetonitrile as the
solvent increased the drug loading and decreased the drying time for lyophilization. The dissolution rate was remarkably enhanced from the SFL powder contained
Asia n Jou r n a l of
Pha rm aceut ics
profiles.30 The forces driving complexation were attributed to (i) the exclusion of high energy water from the cavity, (ii) the release of ring strain particularly in the case of -CD, (iii) Vanderwall s interactions, and (iv) hydrogen and hydrophobic bindings (Ross and Rekharsky, 1996). -CD, the most widely used native cyclodextrins, is limited in its pharmaceutical application by its low aqueous solubility (1.85 g/100 ml, 25C), toxicity profile and low aqueous solubility of the formed complexes. Accordingly, derivatives such as hydroxypropyl--CD (HP- CD; Enapsin) and sulphobutylether--CD (SE--CD; Captisol) have been developed to produce more water-soluble and less toxic entities.
Re vie w
Ar t icle s
riers than the drugs, drug-rich layers were formed over the surfaces of dissolving plugs, which prevented further dissolution of drug from solid dispersions. Therefore, surface-active or self-emulsifying agents including bile salts, lecithin, lipid mixtures, Gelucire 44/14 Vitamin E TPGS NF
34 33
and
were used as additional additives,
acting as dispersing or emulsifying carriers for the liberated drug to prevent the formation of any water-insoluble surface layer. In addition, the release behaviors of many drugs are also improved by using waterinsoluble polymers such as crospovidone
35, 36
and en-
teric polymers such as hydroxypropyl methylcellulose phthalate (HPMCP), cellulose acetate phthalate (CAP), Eudragit L100 and S100 (Takada et al., 1989) and Eudragit E.
37
Solid solutions/dispersions
Solid dispersion was firstly introduced to overcome the low bioavailability of lipophilic drugs by forming of eutectic mixtures of drugs with water-soluble carriers. It was defined as the dispersion of one or more active ingredients in an inert carrier matrix in solid-state prepared by melting (fusion), solvent or melting-solvent method More than 500 papers have been published on the subject and various materials are employed as drug carriers. Despite an active research interest, the number of marketed products arising from this approach is disappointing mainly caused by the physical and chemical instability and scale-up problems.31 Only two commercial products, a griseofulvin in polyethylene glycol 8000 solid dispersion (Gris-PEG, Novartis) and a nabilone in povidone solid dispersion (Cesamet, Lilly) were marketed during the last four decades following the initial work of Sekiguchi and Obi.32
Controlled Precipitation
Controlled precipitation is a particle engineering technology that creates crystalline nanostructured drug particles with rapid dissolution rates. With this technology, the drug is dissolved in a suitable solvent then precipitated into an aqueous solution in the presence of crystal growth inhibitors to form drug nanoparticles. Particles prepared by controlled precipitation have the advantage of a narrower particle size distribution as compared to particle size reduction technologies, such as wet milling. The process is fast, continuous, and scalable with conventional process equipment. Levels of residual solvents are low, and the excipients used are pharmaceutically acceptable. The danazol powder prepared by controlled precipitation shows substantially improved bioavailability compared to the drug as-received (micronized danazol). Tablets prepared on a Carver press from precipitated danazol (equivalent to 200 mg danazol) formulated with microcrystalline cellulose and carboxymethylcellulose (47.5:47.5:5) show further enhancement in bioavailability. The increased bioavailability observed with the control is due to an excipient effect that enhances wettability of the powder.38
Carriers
Many water-soluble excipients were employed as carriers of solid solutions/dispersions. Among them, polyethylene glycols (PEG, Mw 1500-20000) were the most commonly used due to their good solubility in water and in many organic solvents, low melting points (under 65C), ability to solubilize some compounds and improvement of compound wettability. The marketed GrisPEG is the solid dispersion of griseofulvin in PEG 8000. The others carriers include polyvinyl pyrrolidone (PVP), poly vi ny lalcoh ol (PVA ), pol yvi ny lpyrroli done polyvinylacetate copolymer (PVP-PVA), hydroxypropyl methylcellulose (HPMC), hydroxypropyl cellulose (HPC), urea, Poloxamer 407, sugars, emulsifiers (SDS, Tween 80) and organic acids (succinic acid and citric acid). Because of the rapid dissolution of the water-soluble carVolume 1, Issue 1, April - June, 2007 5
Ultra-Rapid Freezing
Ultra-rapid freezing is a novel, cryogenic technology that creates nanostructured drug particles with greatly enhanced surface area. The technology has the flexibility to produce particles of varying particle morphologies, based on control of the solvent system and process conditions.
Asia n Jou r n a l of
Pha rm aceut ics
The technology involves dissolving a drug in a watermiscible or anhydrous solvent along with a stabilizer acting as a crystal growth inhibitor. The drug/stabilizer solution is then applied to a cryogenic substrate. The solvent is removed by lyophilization or atmospheric freeze-drying, resulting in highly porous, agglomerated
Re vie w
Ar t icle s
particles. As with controlled precipitation, this process uses pharmaceutically acceptable solvents, excipients and conventional process equipment making it fast and scalable. An additional feature is that polymer absorption on the crystal surface upon freezing aids reduction of Ostwald ripenin, e.g. Ketoconazole.38
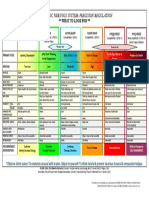
Table 1: Cyclodextrin based commercially available products Cyclodextrin/Drug
SE7 - - CD ( CAPTI SOL) / Zipradidone Voriconazole - CD PG1, Alprostadil IV Europe, Japan, USA OP-1206 Cefotiam hexetil HCl -CD Piroxicam PGE2 Benexate Iodine Dexamethasone Glyteer Nitroglycerin Nimesulide Tiaprofenic acid Omeprazole ME 1207 Cephalosporin Oral, Rectal Buccal Oral Topical Dermal Buccal Oral Oral Oral Oral - CD HP--CD (Encapsin) Itraconazole Cisapride Mitomycin Oral, IV Rectal IV Europe, USA Europe USA SporanoxPrepusid Mitozytrex Europe Japan Japan Japan Japan Japan Europe Europe Europe Japan Brexin, Cycladol, Brexidol Prostarmon E Ulgut, Lonmiel Mena-Galgle Glymesason Nitropen Nimedex, Mesulid Fast Surgamyl Ombeta Meiact Oral Oral Japan Japan Prostanding, Prostavasin, Edex Opalmon Pansporin T
Route
IM IV
Market
Trade names
Europe, USA Europe, USA
Zeldox, Geodon Vfend
CONCLUSION
By using one of the above techniques many lipophilic drug were utilized successfully and will going to be many more in future. The success ratio may depend on many factors from pilotization of techniques to uniformity of the product, as well as characterization. However, in future it may be possible to utilize all the NMEs, no matter what their properties are, if they are pharmacologically active.
6
REFERENCES
1. Radtke M. Pure drug nanoparticles for the formulation of lipophilic drugs, New Drugs, 3, 2001, 62-68. 2. Lipinski C. Poor aqueous solubility-an industry wide problem in drug delivery, Am. Pharm. Rev., 5, 2002, 82-85. 3. Mehta MU. A APS/FD A Workshop on
Volume 1, Issue 1, April - June, 2007
Asia n Jou r n a l of
Pha rm aceut ics
Biopharmaceutics Classification System: Implementation Challenges and Extension Opportunities. September 2002, Arlington, VA, 25-27. 4. Chen X, Young TJ, Sarkari M, Williams RO and Johnston KP. Preparation of cyclosporine A nanoparticles by evaporative precipitation into aqueous solution, Int. J. Pharm, 242, 2002, 314. 5. Pinnamaneni S, Das NG, and Das SK. Formulation approaches for orally administered lipophilic drugs, Pharmazie, 57, 2002, 291-300. 6. Strickley RG. Solubilizing excipientsin oral and injectable formulations, Pharm.Res., 21, 2004, 201-230. 7. Kawakami K, Yoshikawa T, Moroto Y, Kanaoka E, Takahashi K , Nishi hara Y an d Masuda K. Microemulsion formulation for enhanced absorption of lipophilic drugs. I. Prescription design, J. Control. Rel., 81, 2002, 65-74. 8. Lieberman HA, Rieger MM and Banker GS, Pharmaceutical dosage forms, Disperse systems, volume 1, Marcel Dekker, New York and Basel, 1998, 149 181. 9. Gershanik T, Benzeno S and Benita S. Interaction of the self-emulsifying lipid drug delivery system with mucosa of everted rat intestine as a function of surface charge and droplet size, Pharm. Res., 15, 1998, 863-869. 10. Gershanik T and Benita S. Self-dispersing lipid formulations for improving oral absorption of lipophilic drugs, Eur. J. Pharm. Biopharm, 50, 2000, 179-188. 11. Shah NH, Carvajal MT, Patel CI, Infeld MH and Malick AW. Self-emulsifying drug delivery systems (SEDDS) with polyglycolyzed glycerides for improving in vitro dissolution and oral absorption of lipophilic drugs, Int. J. Pharm., 106, 1994, 15-23. 12. Gershanik T and Benita S. Positively charged selfemulsifying oil formulation for improving oral bioavailability of progesterone, Pharm. Dev. Technol., 1996, 1(2), 147- 157.
Volume 1, Issue 1, April - June, 2007 7
Re vie w
13.
Ar t icle s
Kobayashi P, Ito S, Itai S and Yamamoto K. Physicochemical properties and bioavailability of carbamazepine polymorphs and dehydrate, Int. J. Pharm., 193, 2000, 137-146.
14.
Kachi S, Terada M and Hashimoto M. Effect of amorphous and polymorphs of PF1022A, a new an ti nematode 235-245. drug on an giostrongyl us costaricensis in mice, Jpn. J. Pharmacol, 77, 1998,
15.
Vippagunta, SR, Brittain, HG and Grant DJ. Crystalline solids, Adv. Drug Del. Rev., 48, 2001, 326.
16.
Merisko-Liversidge E., Liversidge GG and Cooper ER. Nanosizing: a formulation approach for poorly-water-soluble compounds, Eur. J. Pharm. Sci., 18, 2003, 113-120.
17.
Hu J., John son K P an d Wil li am s III RO. Nanoparticle engineering processes for enhancing the dissolution rates of poorly water soluble drugs, Drug Dev. Ind. Pharm., 30(3), 2004, 233245.
18.
M ll er
RH ,
Jacobs
an d
K ay ser
O.
Nanosuspensions as particulate drug formulations in therapy rationale for development and what we can expect for the future, Adv. Drug Deliv. Rev., 54, 2001, 131-155. 19. Hanna MH and York P. Method and apparatus for the formulation of particles, US Patent 5, 851, 1998, 453. 20. Subramaniam B, Rajewski RA and Snavely K. Pharmaceutical processing with supercritical carbon dioxide, J. Pharm. Sci, 86, 1997, 885-890. 21. Subramaniam B, Saim S, Rajewski RA and Stella V. Method of particle precipitation and coating using nearcritical and supercritical antisolvents, US Patent 5,833, 1997, 891. 22. Young TJ, Mawson S, Johnston KP, Henriksen IB, Pace GW and Mishra AK. Rapid expansion from supercritical to aqueous solution to produce submicron suspensions of water-insoluble drugs, Biotechnol. Prog., 16, 2000, 402-407.
Asia n Jou r n a l of
Pha rm aceut ics
23. Pace GW, Vachon MG, Mishra AK, Henrikson IB and Krukonis V. Processes to generate submicron particles of water-insoluble compounds, US Patent 6,177, 2001, 103. 24. Williams RQ, Hu J, Rogers TL, Barron MK, Young TJ, Yu Z and Johnston KP. Process for production of nanoparticles and microparticles by spray freezi ng in to li qu id, US Patent, 2003, 20030041602. 25. Rogers TL, Hu J, Yu Z, Johnston KP and Williams III RO. A novel particle engineering technology: spray-freezing into liquid, Int. J. Pharm., 242, 2002, 93-100. 26. Koester LS, Bertuol JB, Groch KR, Xavier CR, Moellerke R, Mayorga P, Dalla Costa T and Bassani VL. Bioavailability of carbamazepine: beta-cyclodextrin complex in beagle dogs from hydroxypropylmethylcellulose matrix tablets, Eur. J. Pharm. Sci., 22(2-3), 2004, 201-207 27. Loftsson T and Brewster ME. Pharmaceutical applications of cyclodextrins-1. Drug solubilization and stabilization, J. Pharm. Sci., 85, 1996, 1017-1025. 28. Rajewski RA and Stella VJ. Pharmaceutical applications of cyclodextrins. 2. In vivo drug delivery, J. Pharm. Sci., 85, 1996, 1142-1169. 37. 29. CD Cydex. Captisol: A reality in commercial formulation, 2003, www.captisol.com. 30. Thompson DO. Cyclodextrins, enabling excipients: their present and future use in pharmaceuticals, Crit. Rev. Therap. Drug Carrier Syst. 14, 1997, 1-104. 31. Craig DQM. The mechanisms of drug release from solid dispersions in water soluble polymers, Int. J. Pharm., 203, 2002, 131-144. 38. 36. 35. 34. 33. 32.
Re vie w
Ar t icle s
Sekiguchi K and Obi N. Studies on absorption of eutectic mixture. I. A comparison of the behavior of eutectic mixture of sulfathiazole and that of ordinary sulfathiazole in man, Chem. Pharm. Bull, 9, 1961, 866-872. Hlsmann S, Backensfeld T, Keitel S and Bodmeier R. Melt extrusion-an alternative method for enhancing the dissolution rate of 17-estradiol hemihydrate, Eur. J. Pharm. Biopharm., 49, 2000, 237-242. Khoo SM, Porter CJH and Charman WN. The formu lati on of Halofantrin e as either nonsolubilising PEG 6000 or solubilising lipid based solid dispersions: physical stability and absolute bioavailability assessment, Int. J. Pharm., 205, 2000, 65-78. Hirasawa N, Ishise S, Miyata H and Danjo K. Application of nilvadipine solid dispersion to tablet form ul ation an d man uf actu ri ng u si ng crospovidone and methylcellulose as dispersion carriers, Chem. Pharm. Bull, 52, 2004, 244-247. Hirasawa N, Ishise S, Miyata H and Danjo K. Physicochemical characterization and drug release studies of nilvadipine solid dispersions using water-insoluble polymer as a carrier, Drug Dev. Ind. Pharm., 29(3), 2003, 339-344. Horisawa E, Danjo K, and Haruna M. Physical properties of solid dispersion of a nonsteroidal anti-inflammatory drug (M-5011) with Eudragit E, Drug Dev. Ind. Pharm., 26,2000, 1271-1278. Connors RD and Elder EJ. Using a Portfolio of Particle Growth Technologies to Enable Delivery of Drugs With Poor Water Solubility. Drug Delivery Tech . Onl in e, h ttp:// www.drugdeliverytech.com/cgi-bin/ articles.cgi?idArticle=262.
Volume 1, Issue 1, April - June, 2007
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Manufacturing Process Scale UpDocument5 pagesManufacturing Process Scale Upraju1559405Pas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Calculating Forklift Aisle Width MinimumsDocument2 pagesCalculating Forklift Aisle Width Minimumsraju1559405Pas encore d'évaluation
- GEA-Article - Courtoy MUPS - Innovation in Pharmaceutical TechnologyDocument3 pagesGEA-Article - Courtoy MUPS - Innovation in Pharmaceutical Technologyraju1559405Pas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Reactivity QuinolineDocument107 pagesReactivity QuinolineIan Otto100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- PROSOLV-tech Info Prosolv Func Inv GB 1809Document12 pagesPROSOLV-tech Info Prosolv Func Inv GB 1809raju1559405Pas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Order Picking: Safe Work GuidelinesDocument5 pagesOrder Picking: Safe Work Guidelinesraju1559405Pas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The Work of Eurovent: What's in Eurovent?Document3 pagesThe Work of Eurovent: What's in Eurovent?raju1559405Pas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Training-Coating Machine OperationDocument12 pagesTraining-Coating Machine Operationraju1559405Pas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Manufacturing Process Scale UpDocument5 pagesManufacturing Process Scale Upraju1559405Pas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- GEA-The Reality of Continuous Pharmaceutical Manufacturing Conference - Hosted by GEA, Siemens & Perceptive EngineeringDocument4 pagesGEA-The Reality of Continuous Pharmaceutical Manufacturing Conference - Hosted by GEA, Siemens & Perceptive Engineeringraju1559405Pas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Mobile Pharmaceutical Work StationDocument4 pagesMobile Pharmaceutical Work Stationraju1559405Pas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- EUROVENT Programme DescriptionsDocument1 pageEUROVENT Programme Descriptionsraju1559405Pas encore d'évaluation
- Operational Performance and Optimization of RO Wastewater Treatment PlantsDocument12 pagesOperational Performance and Optimization of RO Wastewater Treatment PlantsalesclPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- GEA-Article - Courtoy MUPS - Innovation in Pharmaceutical TechnologyDocument3 pagesGEA-Article - Courtoy MUPS - Innovation in Pharmaceutical Technologyraju1559405Pas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Eurovent-Rating Standard For The Certification of Air Handling Units - rs-6c005-2016 - AhuDocument3 pagesEurovent-Rating Standard For The Certification of Air Handling Units - rs-6c005-2016 - Ahuraju1559405Pas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- FiveDocument8 pagesFiveraju1559405Pas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- HeatingDocument134 pagesHeatingraju1559405Pas encore d'évaluation
- Fgi Guidelines 2014 Hop TocDocument10 pagesFgi Guidelines 2014 Hop TocZaw Moe KhinePas encore d'évaluation
- Aia Guidelines Patient VentilationDocument3 pagesAia Guidelines Patient Ventilationraju1559405Pas encore d'évaluation
- SurgicalDocument3 pagesSurgicalraju1559405Pas encore d'évaluation
- Demand of Pharmaceutical Facility Functionality - Validation and Qualification of HVAC SystemDocument17 pagesDemand of Pharmaceutical Facility Functionality - Validation and Qualification of HVAC Systemraju1559405Pas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Demand of Pharmaceutical Facility Functionality - Validation and Qualification of HVAC SystemDocument17 pagesDemand of Pharmaceutical Facility Functionality - Validation and Qualification of HVAC Systemraju1559405Pas encore d'évaluation
- 349 893 1 SMDocument5 pages349 893 1 SMrambabuPas encore d'évaluation
- 349 893 1 SMDocument5 pages349 893 1 SMrambabuPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- AIA Guidelines Patient Care Construction Air ChangeDocument2 pagesAIA Guidelines Patient Care Construction Air ChangeMinh van LePas encore d'évaluation
- Microbiological Assessment of Compressed Gases in Pharmaceutical FacilitiesDocument6 pagesMicrobiological Assessment of Compressed Gases in Pharmaceutical Facilitiesraju1559405Pas encore d'évaluation
- Autocad ShortcutsDocument13 pagesAutocad ShortcutsKriscel CaraanPas encore d'évaluation
- Sampling Water Table ContentsDocument2 pagesSampling Water Table Contentsraju1559405Pas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- Ultra Pure Water Treatment For Pharmaceutical IndustryDocument4 pagesUltra Pure Water Treatment For Pharmaceutical Industryraju1559405100% (1)
- How Efficient Is Your Boiler HouseDocument3 pagesHow Efficient Is Your Boiler Houseraju1559405Pas encore d'évaluation
- Caries Risk Assesment: Disha Jandial Mds 1 Year Deptt. of Pediatrics and Preventive DentistryDocument134 pagesCaries Risk Assesment: Disha Jandial Mds 1 Year Deptt. of Pediatrics and Preventive Dentistrydisha 146jandial100% (1)
- Job Safety Analysis: Date/ Jsa No: Jsa Team Members Job: Location: Project/ Client: SupervisorDocument1 pageJob Safety Analysis: Date/ Jsa No: Jsa Team Members Job: Location: Project/ Client: SupervisorMuhammad Akbar Al BardawiPas encore d'évaluation
- QA/QC of Nuclear Medicine Imaging Equipment - Current PracticesDocument38 pagesQA/QC of Nuclear Medicine Imaging Equipment - Current PracticesRosendo DacuyanPas encore d'évaluation
- Sistema NervosoDocument1 pageSistema NervosoPerisson Dantas100% (2)
- Stretch To Win (2017) PDFDocument241 pagesStretch To Win (2017) PDFmmpersonal2010100% (4)
- Lab Exercise 11 Urine Specimen CollectionDocument7 pagesLab Exercise 11 Urine Specimen CollectionArianne Jans MunarPas encore d'évaluation
- Skripsi Tanpa Pembahasan PDFDocument73 pagesSkripsi Tanpa Pembahasan PDFMutmainnah MunirPas encore d'évaluation
- Commercial LawDocument66 pagesCommercial LawBradley MusonzaPas encore d'évaluation
- Triamcinolone AcetonideDocument12 pagesTriamcinolone Acetonideawais khanPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Test I. True or False. Write TRUE If The Statement Is Correct and FALSE If The Statement Is IncorrectDocument2 pagesTest I. True or False. Write TRUE If The Statement Is Correct and FALSE If The Statement Is IncorrectMariecris Barayuga Duldulao-AbelaPas encore d'évaluation
- Medicine List With DosageDocument9 pagesMedicine List With DosageonovPas encore d'évaluation
- L 65 - Prevention of Fire and Explosion, and Emergency Response On Offshore Installations - Approved Code of Practice and Guidance - HSE - 2010Document56 pagesL 65 - Prevention of Fire and Explosion, and Emergency Response On Offshore Installations - Approved Code of Practice and Guidance - HSE - 2010Barkat UllahPas encore d'évaluation
- Notice, Caution, Warning Evaluation I Ix Graders: Acces For Residents OnlyDocument2 pagesNotice, Caution, Warning Evaluation I Ix Graders: Acces For Residents OnlyRizqiyah SakinahPas encore d'évaluation
- Chapter 4 and Chapter 5Document58 pagesChapter 4 and Chapter 5Aria DiemPas encore d'évaluation
- Risk Management in Military AviationDocument16 pagesRisk Management in Military AviationSp AndaPas encore d'évaluation
- Triad Color TestDocument37 pagesTriad Color TestC.O.M.A research -stopalienabduction-0% (1)
- Jamie's Story 15q21.3-22.2 DeletionDocument1 pageJamie's Story 15q21.3-22.2 DeletionNatasha RadcliffePas encore d'évaluation
- E The Real Facts Supporting Jeanne Calment As The Oldest Ever HumanDocument9 pagesE The Real Facts Supporting Jeanne Calment As The Oldest Ever Humanliz201177Pas encore d'évaluation
- Maria MontessoriDocument2 pagesMaria MontessoriGiulia SpadariPas encore d'évaluation
- BingggDocument12 pagesBingggZulham YahyaPas encore d'évaluation
- Is Iso 10555 1 1995Document21 pagesIs Iso 10555 1 1995Hemant SharmaPas encore d'évaluation
- Validated HPTLC Method For Assay of Prednisolone in Tablets and Comparison With Pharmacopeial MethodsDocument4 pagesValidated HPTLC Method For Assay of Prednisolone in Tablets and Comparison With Pharmacopeial MethodsSyifa KhairunnisaPas encore d'évaluation
- Biological Spill Clean UpDocument5 pagesBiological Spill Clean UpNAMPEWO ELIZABETHPas encore d'évaluation
- Ammonia SafetyDocument46 pagesAmmonia SafetyMikechal AwacayPas encore d'évaluation
- Maternal Collapse During PregnancyDocument57 pagesMaternal Collapse During PregnancytapayanaPas encore d'évaluation
- HRM - CompleteDocument12 pagesHRM - Completedhou_4Pas encore d'évaluation
- 2018 State of The StateDocument26 pages2018 State of The StateRuss LatinoPas encore d'évaluation
- Health Economics: Which of The Following Is Not A Reason For Increased Health Spending?Document8 pagesHealth Economics: Which of The Following Is Not A Reason For Increased Health Spending?Arjun Aryal100% (1)
- 1823 - Part - A - DCHB - Kamrup Metropolitan PDFDocument224 pages1823 - Part - A - DCHB - Kamrup Metropolitan PDFSaddam FaruquePas encore d'évaluation
- Umbilical Cord Blood BankingDocument290 pagesUmbilical Cord Blood BankingcmPas encore d'évaluation
- Water-Based Paint Formulations, Vol. 3D'EverandWater-Based Paint Formulations, Vol. 3Évaluation : 4.5 sur 5 étoiles4.5/5 (6)
- Process Steam Systems: A Practical Guide for Operators, Maintainers, and DesignersD'EverandProcess Steam Systems: A Practical Guide for Operators, Maintainers, and DesignersPas encore d'évaluation
- Nuclear Energy in the 21st Century: World Nuclear University PressD'EverandNuclear Energy in the 21st Century: World Nuclear University PressÉvaluation : 4.5 sur 5 étoiles4.5/5 (3)
- Process Plant Equipment: Operation, Control, and ReliabilityD'EverandProcess Plant Equipment: Operation, Control, and ReliabilityÉvaluation : 5 sur 5 étoiles5/5 (1)
- Sodium Bicarbonate: Nature's Unique First Aid RemedyD'EverandSodium Bicarbonate: Nature's Unique First Aid RemedyÉvaluation : 5 sur 5 étoiles5/5 (21)