Académique Documents
Professionnel Documents
Culture Documents
Drug Study
Transféré par
Marc AnchetaDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Drug Study
Transféré par
Marc AnchetaDroits d'auteur :
Formats disponibles
NAME Phenytoin
ACTION The mechanism of action is not definitely known, but extensive research strongly suggests that its main mechanism is to block frequency-, useand voltagedependent neuronal sodium channels, and therefore limit repetitive firing of action potentials.
ADVERSE REACTION Dizziness Drowsiness Difficulty focusing Unsteady gate Tiredness Abnormal involuntary movements Nausea Vomiting Constipation Abdominal Pain Loss of appetite
INTERACTION Phenytoin can increase the metabolism (elimination) of many drugs, reducing their concentrations in the body. Drugs that may be affected include: digoxin, carbamazepine, clonazepam, corticosteroids (e.g. prednisone), cyclosporine, disopyramide, doxycycline, estrogens, felodipine, levodopa, lidocaine, methadone, mexiletine, oral contraceptives, paroxetine, quinidine, tacrolimus, theophylline, phenobarbital, and warfarin
CONTRAINDICATIO N
NURSING CONSIDERATION Continuously monitor vital signs and symptoms during IV infusion and for an hour afterward. Watch for respiratory depression. Constant observation and a cardiac monitor are necessary with older adults or patients with cardiac disease. Margin between toxic and therapeutic IV doses is relatively small.
Observe patient closely for neurologic adverse effects following IV administration. Have on hand oxygen, atropine, vasopressor, assisted ventilation, seizure precaution equipment (mouth gag, nonmetal airway, suction apparatus)
Be alert to symptoms of hypomagnesemia (see Appendix F); neuromuscular symptoms: tetany, positive Chvosteks and Trousseaus signs, seizures, tremors, ataxia, vertigo, nystagmus, muscular fasciculations. NAME lactulose ACTION ADVERSE REACTION GI Gaseous distention with flatulence or belching, abdominal discomfort and cramping; diarrhea; nausea; vomiting. INTERACTION Neomycin, other antiinfectives May interfere with desired degradation of lactulose and prevent acidification of colonic contents. Nonabsorbable antacids May inhibit colonic acidification. CONTRAIND ICATION Use in patients who require lowgalactose diet. NURSING CONSIDERATION Advise patient that drug can be mixed with fruit juice, water, or milk to make it more palatable. Inform patient that drug may cause belching, flatulence, or abdominal cramps. Instruct patient to notify health care provider if these symptoms become bothersome or if diarrhea occurs. Instruct patient not to take other laxatives while receiving lactulose therapy. Encourage patient to increase dietary fiber and fluid intake and participate in regular exercise.
NAME
ACTION
ADVERSE
INTERACTION
CONTRAINDICATIO
NURSING
Azithromycin
REACTION Cardiovascular Chest pain, palpitations (1% or less); arrhythmias including ventricular tachycardia, hypotension, QT prolongation, syncope, torsades de pointes (postmarketing). CNS Dizziness, headache (1%); agitation, fatigue, hyperkinesia, insomnia, malaise, nervousness, somnolence, vertigo (1% or less); aggressive reaction, anxiety, asthenia, convulsions, hyperactivity, paresthesia (postmarketing). Dermatologic Rash (5%); dermatitis, pruritus (2%); eczema, fungal dermatitis, photosensitivity,
Aluminum- and magnesium-containing antacids May reduce the peak serum levels but not the AUC of azithromycin. Carbamazepine, hexobarbital, phenytoin Serum concentrations of these agents have been elevated by azithromycin, increasing the pharmacologic effects and risk of adverse reactions. Monitor serum concentrations of these agents and observe the patient for adverse reactions. Adjust the dose as needed. Cyclosporine, theophyllines Levels may be elevated by azithromycin, increasing the risk of toxicity. Monitor drug levels and adjust the dose as needed. Digoxin Digoxin plasma concentrations may be elevated, increasing the
N Hypersensitivity to azithromycin, erythromycin, or to any macrolide or ketolide antibiotic.
CONSIDERATION Review dosing schedule and prescribed length of therapy with patient. Advise patient that dose, dosing frequency, and duration of therapy are dependent on site and cause of infection. Advise patient or caregiver that injection will be prepared by a health care provider and administered in a health care setting. Instruct patient using tablets to take prescribed dose with a full glass of water. Instruct patient or caregiver using oral suspension to shake suspension well and then measure and administer prescribed dose
swelling, urticaria, vesiculobullous rash (1% or less); erythema multiforme, StevensJohnson syndrome, TEN (postmarketing). EENT Eye irritation with ophthalmic solution (1% to 2%); conjunctivitis, pharyngitis, rhinitis (1% or less); deafness, hearing disturbances including hearing loss, smell perversion or loss, taste perversion or loss, tinnitus (postmarketing). Ophthalmic Blurring vision, eye pain, eyelid swelling, itching eye, reduced visual acuity (postmarketing). GI Nausea (18%); diarrhea/loose
risk of toxicity. Monitor digoxin levels and observe the patient for signs of digoxin toxicity. Adjust the digoxin dose as needed. Dronedarone Dronedarone plasma concentrations and pharmacologic effects may be increased. Avoid coadministration. Ergot derivatives (eg, dihydroergotamine, ergotamine) Acute ergotism manifested as peripheral ischemia has been reported. Closely monitor for ergotism. Nelfinavir Azithromycin levels may be elevated, increasing the risk of adverse reactions (eg, abnormal LFTs, hearing impairment). Monitor for azithromycin adverse reactions. Nilotinib Increased nilotinib plasma concentrations with cardiotoxicity may occur. Avoid coadministration. Pimozide
using dosing spoon, dosing syringe, or medicine cup. Advise patient to take prescribed dose without regard to meals, but to take with food if stomach upset occurs. Instruct patient to take Zmax ER oral suspension on an empty stomach, at least 1 h before or 2 h after a meal. Advise patient to take 2 h before or after antacids containing aluminum or magnesium. Advise patients that Zmax ER suspension may be taken without regard to antacids containing magnesium and/or aluminum hydroxide. Instruct patient to consume
stools, vomiting (14%); abdominal pain (5%); anorexia (2%); dyspepsia (1%); constipation, enteritis, flatulence, gastritis, melena (1% or less); oral candidiasis, pancreatitis, pseudomembranous colitis, tongue discoloration (postmarketing). Genitourinary Vaginitis (3%); monilia, nephritis (1% or less); acute renal failure, interstitial nephritis (postmarketing). HematologicLymphatic Decreased lymphocytes, decreased neutrophils, increased eosinophils, increased lymphocytes, increased
Pimozide plasma concentrations may be elevated, increasing the risk of cardiotoxicity. Coadministration is contraindicated. Risk of life-threatening cardiac arrhythmias, including torsades de pointes, may be increased. Use with caution. Avoid coadministration with paliperidone or propafenone. Close clinical and ECG monitoring is advised. Rifabutin Risk of neutropenia may be increased. Triazolam Plasma concentrations may be elevated by azithromycin, increasing the pharmacologic effect and risk of adverse reactions. Observe the clinical response of the patient and adjust the triazolam dose as needed. Warfarin The anticoagulant effect
reconstituted Zmax ER oral suspension within 12 h and to discard any suspension remaining after dosing. Instruct patient to complete entire course of therapy, even if symptoms of infection have disappeared. Advise patient to discontinue therapy and contact health care provider immediately if skin rash, hives, itching, or shortness of breath occur. Advise patient to report signs of superinfection to health care provider: black, furry tongue; white patches in mouth; foulsmelling stools; vaginal itching or discharge. Warn
neutrophils, increased platelet count (at least 1%); anemia, leukopenia (1% or less); thrombocytopenia (postmarketing). Hepatic Cholestatic jaundice, jaundice (1% or less); abnormal liver function including hepatic failure, hepatic necrosis, hepatitis (postmarketing). Hypersensitivity Angioedema (1% or less); anaphylaxis (postmarketing). Ophthalmic Allergic reactions including facial swelling, hives, periocular swelling, rash, and urticaria (postmarketing). Musculoskeletal Arthralgia (postmarketing). Respiratory Cough, pleural
may be increased, increasing the risk of hemorrhage. Monitor anticoagulant parameters and adjust the warfarin dose as needed.
patient that diarrhea containing blood or pus may be a sign of a serious disorder and to seek medical care if noted and to not treat at home. Instruct patient or caregiver to contact health care provider for further treatment if the patient vomits within the first hour. Advise patients using the ophthalmic solution not to wear contact lenses if they have signs or symptoms of bacterial conjunctivitis. Advise patients to wash their hands prior to use of the ophthalmic solution. Advise patients to avoid contaminating the ophthalmic solution's
effusion (1% or less).
applicator tip by not allowing it to touch the eye, fingers, or other surfaces. Advise patients using the ophthalmic solution to invert closed bottle and shake once before each use.
NAME Citicholine
ACTION Citicoline activates the biosynthesis of structural phospholipids in the neuronal membrane, increases cerebral metabolism and increases the level of various neurotransmitters, including acetylcholine and dopamine. Citicoline has shown neuroprotective effects in situations of hypoxia and ischemia.
ADVERSE REACTION citicoline may exert a stimulating action of the parasympathetic, as well as a fleeting and discrete hypotensor effect
INTERACTION
CONTRAINDICATIO N hypertonia of the parasympathetic
NURSING CONSIDERATION Watch out for hypotensive effects Somazine must not be administered along with medicaments containing
NAME
ACTION
ADVERSE REACTION
INTERACTION
CONTRAINDIC
NURSING CONSIDERATION
Omeprazole
Cardiovascular Angina or chest pain, bradycardia, elevated BP, palpitations, peripheral edema, tachycardia (postmarketing). CNS Headache (7%); dizziness (2%); asthenia (1%); abnormal dreams, aggression, agitation, anxiety, apathy, confusion, depression, fatigue, hallucinations, insomnia, malaise, nervousness, paresthesia, sleep disturbances, somnolence, tremors, vertigo (postmarketing). Dermatologic Rash (2%); alopecia, dry skin, erythema multiforme, hyperhidrosis, petechiae, photosensitivity, pruritus, purpura, skin inflammation, StevensJohnson syndrome, TEN, urticaria (postmarketing). EENT Anterior ischemic optic neuropathy, blurred vision, double vision, dry eye syndrome, ocular irritation, optic atrophy, optic neuritis, pharyngeal pain, taste perversion, tinnitus (postmarketing). GI
Ampicillin The inhibition of gastric acid secretion may interfere with the absorption of ampicillin esters in which gastric pH is an important determinant of bioavailability. Atazanavir, nelfinavir, ritonavir Plasma concentrations may be reduced by omeprazole, decreasing the efficacy. Coadministration with omeprazole is not recommended. Azole antifungal agents (eg, itraconazole, ketoconazole) The bioavailability of certain azole antifungals may be decreased. Avoid coadministration if possible. Benzodiazepines (eg, diazepam) Cl of benzodiazepines may be decreased.
ATION Hypersensitivity to substituted benzimidazoles or to any component of the formulation
Instruct patient using OTC omeprazole tablets to carefully read the package instructions regarding warnings and dosing instructions. Advise patient to swallow tablet whole and not to split, crush, or chew tablet. Instruct patient to take each dose on an empty stomach at least 1 h before eating. Instruct patient to swallow capsules whole and not to open, crush, or chew the capsule. Advise patients having difficulty swallowing the capsule to open it and gently mix the pellets with 1 Tbsp of cool or cold applesauce and then immediately swallow the mixture without chewing. Remind patients not to crush or chew the pellets and not to prepare the pellet/applesauce mixture ahead of time or store for future use. Instruct patients using oral suspension to empty the contents of a 2.5 mg packet into a container containing 5 mL of water, or empty the contents of a 10 mg packet into a container containing 15 mL
Abdominal pain (5%); diarrhea, nausea (4%); flatulence, vomiting (3%); acid regurgitation, constipation (2%); abdominal swelling, anorexia, dry mouth, esophageal candidiasis, fecal discoloration, gastric fundic gland polyps, gastroduodenal carcinoids, irritable colon, mucosal atrophy of the tongue, pancreatitis, stomatitis (postmarketing). Genitourinary Elevated serum creatinine, glucosuria, gynecomastia, hematuria, interstitial nephritis, microscopic pyuria, proteinuria, testicular pain, urinary frequency, UTI (postmarketing). Hepatic Cholestatic disease, elevated LFTs (alkaline phosphatase, bilirubin, ALT, AST, GGT), hepatic encephalopathy, hepatic failure (some fatal), hepatocellular disease, jaundice, liver necrosis, mixed hepatitis (postmarketing). Hematologic-Lymphatic Agranulocytosis, anemia, hemolytic anemia, leukocytosis, leukopenia, neutropenia, pancytopenia, thrombocytopenia (postmarketing). Hypersensitivity
Monitor for increased CNS impairment and reduce the benzodiazepine dosage or increase the dosing interval if needed. Benzodiazepines not metabolized by oxidation (eg, lorazepam) may not interact. Carbamazepine Carbamazepine plasma concentrations may be elevated, increasing the risk of toxicity. Additional carbamazepine concentration and clinical monitoring is warranted. Adjust the carbamazepine dose as needed when starting or stopping omeprazole. Clarithromycin Omeprazole and clarithromycin plasma concentrations may be elevated. Based upon available data, no special action is needed. Digoxin Coadministration may increase serum digoxin
of water. Stir. Leave for 2 to 3 min to thicken. Stir and drink within 30 min. If any material remains after drinking, add more water, stir, and drink immediately. Instruct patients with NG or gastric tubes using oral suspension to add 5 mL of water to a cathetertipped syringe and then add the contents of a 2.5 mg packet (or 15 mL of water for the 10 mg packet). Inform patients that it is important to only use a catheter-tipped syringe when administering omeprazole through an NG tube or gastric tube. Immediately shake the syringe and leave for 2 to 3 min to thicken. Shake the syringe and inject through the NG or gastric tube, French size 6 or larger, into the stomach within 30 min. Refill the syringe with an equal amount of water. Shake and flush any remaining contents from the nasogastric tube into the stomach. Remind patients that omeprazole is to be taken every day, not as needed or only when symptoms are present. Advises patient that this drug may take 1 to 4
Anaphylactic shock, anaphylaxis, angioedema, bronchospasm, interstitial nephritis, urticaria (postmarketing). Metabolic-Nutritional Hypoglycemia, hypomagnesemia, hyponatremia, weight gain (postmarketing). Musculoskeletal Back pain (1%); bone fracture, joint pain, leg pain, muscle cramps, muscle weakness, myalgia (postmarketing). Respiratory Upper respiratory tract infection (2%); cough (1%); epistaxis (postmarketing)
concentrations. The magnitude of this change would not be expected to be clinically important in most patients. Food Administration of omeprazole with applesauce may decrease the omeprazole C max with a change in the AUC. Methotrexate Omeprazole may decrease the renal elimination of methotrexate, increasing methotrexate concentrations and the risk of toxicity. Closely monitor methotrexate concentrations and monitor for signs of methotrexate toxicity. Propranolol Although no interaction with propranolol and omeprazole has been reported, interactions have been reported with other drugs metabolized
days for full effect to be seen. Inform patients that antacids may be taken concurrently with omeprazole. Instruct patients to report any of the following to health care provider: bloody or coffee ground like vomit; black, tarry stools; recurrent heartburn; recurrent indigestion or abdominal pain; increasing need for antacid use; bothersome side effects (eg, headache, constipation, gas).
by the CYP-450 system. Clinical and laboratory monitoring of propranolol is warranted. Adjust the propranolol dose as needed. Salicylates Enteric-coated salicylates may dissolve more rapidly, increasing gastric adverse effects. Patients at risk of serious gastric disorders due to the release of salicylates in the stomach should avoid concurrent use of these agents. Warfarin Increased INR and PT, which may lead to abnormal bleeding and increase the risk of death
NAME
ACTION
ADVERSE REACTION
INTERACTION
CONTRAINDICATIO N
NURSING CONSIDERATION
Calmoseptine
Calmoseptine Ointment is an analgesic, antiseptic, antipruritic, and skin protectant combination. It works by temporarily relieving itching and pain. It also decreases moisture in the affected area.
none
you are allergic to any ingredient in Calmoseptin e Ointment you are treating a deep wound or puncture wound
for external use only. Do not get it in your eyes, nose, or mouth. If you get it in any of these areas, rinse at once with cool water.Do not use Calmoseptine Ointment to treat deep wounds or puncture wounds. PREGNANCY and BREAST-FEEDING: If pregnant, contact the doctor. One will need to discuss the benefits and risks of using Calmoseptine Ointment while pregnant.
NAME
ACTION
ADVERSE REACTION
INTERACTION
CONTRAINDICATIO N
NURSING CONSIDERATION
Meropenem
Interferes with cell wall replication of susceptible organisms; osmotically unstable cell wall swells and bursts from osmotic pressure
CNS: fever, somnolence, seizures, dizziness, weakness, headache, myoclonia CV: hypotension, palpitations GI: diarrhea, nausea, vomiting, pseudomembraneou s colitis, hepatitis, glossitis Blood: eosinophilia, neutropenia, decreased Hgb, Hct Integumentary: rash, urticaria, pruritus, pain at inj site, phlebitis, erythema at inj site RESP: chest discomfort, dyspnea, hyperventilation
Hypersensitivity to meropenem or imipenem
Assess patient for previous sensitivity reaction to carbapenems Assess patient for signs and symptoms of infection, including characteristics of wounds, sputum, urine, stool Complete C/S tests before beginning drug therapy Assess for allergic reactions, anaphylaxis Identify urine output Monitor blood studies Monitor electrolytes Assess bowel pattern daily Monitor for bleeding
NAME
ACTION
ADVERSE REACTION
INTERACTION
CONTRAINDICATIO N
NURSING CONSIDERATION
Piperacillin Sodium Tazobactam Sodium
Piperacillin: Binds to bacterial cell wall membrane, causing cell death. Spectrum is extended compared with other penicillins Tazobactam: Inhibits betalactamase, an enzyme that can destroy penicillins
CNS: SEIZURES (HIGHER DOSES) , confusion, dizziness, headache, insomnia, lethargy. GI: PSEUDOMEMB RANOUS COLITIS, diarrhea, constipation, druginduced hepatitis, nausea, vomiting. GU: interstitial nephritis. Derm: rashes ( in cystic fibrosis patients), urticaria. Hemat: bleeding, leukopenia, neutropenia, thrombocytopenia
Assess patient for infection (vital signs; appearance of wound, sputum, urine, and stool; WBC) at beginning of and during therapy Obtain a history before initiating therapy to determine previous use of and reactions to penicillins or cephalosporins. Persons with a negative history of penicillin sensitivity may still have an allergic response
NAME Vitamin K
ACTION Required for
ADVERSE REACTION
INTERACTION
CONTRAINDICATIO N Severe liver disease
NURSING CONSIDERATION 1. assess for sulfites
hepatic synhesis of blood coagulation factors II (Prothrombin) , VII, IX and X.
sensitivity 2. Monitor for side effects and adverse reactions. 3. Patients receiving vitamin K therapy should be cautioned not to take over-thecounter drugs medications without the advice of health professionals.
NAME Fluimucil
ACTION : Exerts mucolytic action through its free sulfhydryl group which opens up the disulfide bonds in the mucoproteins thus lowering mucous viscosity. The exact mechanism of action in acetaminophen toxicity is unknown. It is thought to act by providing substrate for conjugation with the toxic metabolite.
ADVERSE REACTION Hypersensitivity reactions have been reported in patients receiving acetylcysteine, including bronchospasm, angioedema, rashes and pruritus, may occur. Other adverse effects reported include nausea and vomiting, fever, syncope, sweating, arthralgia, blurred vision, disturbances of liver function.
INTERACTION n/a
CONTRAINDICATIO N MAO inhibitor therapy within 14 days initiating therapy; severe hypertension; severe. Coronary artery disease, hypersensitivity to pseudoedephrine, acrivastine or any component; renal impairment.
NURSING CONSIDERATION Monitor effectiveness of therapy and advent of adverse/allergic effects. Instruct patient in appropriate use and adverse effects to report.
Vous aimerez peut-être aussi
- Phosphate Imbalances PDFDocument1 pagePhosphate Imbalances PDFKaye RicoPas encore d'évaluation
- Drug StudyDocument8 pagesDrug StudyBien EstrellaPas encore d'évaluation
- DB31 - Pathophysiology of Diabetes Mellitus and HypoglycemiaDocument5 pagesDB31 - Pathophysiology of Diabetes Mellitus and HypoglycemiaNeil Alcazaren かわいいPas encore d'évaluation
- Nursing Care Plans for Fever, Rashes & Knowledge DeficitDocument10 pagesNursing Care Plans for Fever, Rashes & Knowledge DeficitRobin HaliliPas encore d'évaluation
- Briviact Film-Coated Tablets Summary of Product CharacteristicsDocument110 pagesBriviact Film-Coated Tablets Summary of Product CharacteristicsBendisDacicaPas encore d'évaluation
- Management of Acute Gastroenteritis in ChildrenDocument14 pagesManagement of Acute Gastroenteritis in ChildrenYayaPas encore d'évaluation
- Understanding Anorexia NervosaDocument11 pagesUnderstanding Anorexia NervosaSashMalikPas encore d'évaluation
- Betnovate Scalp Solution Reduces Scalp ConditionsDocument7 pagesBetnovate Scalp Solution Reduces Scalp ConditionsdindaikaputriPas encore d'évaluation
- Organizing Health Data Using Gordon's 11 PatternsDocument1 pageOrganizing Health Data Using Gordon's 11 PatternsAMGPas encore d'évaluation
- Clopidogrel Bisulfate - PlavixDocument2 pagesClopidogrel Bisulfate - PlavixKristi WrayPas encore d'évaluation
- Safe Dosage and Side Effects of GravolDocument5 pagesSafe Dosage and Side Effects of GravoldrugcardrefPas encore d'évaluation
- Moira Mae B. Balite BSN 2A: Post Partum Care DefinitionDocument5 pagesMoira Mae B. Balite BSN 2A: Post Partum Care DefinitionMoiraMaeBeridoBalitePas encore d'évaluation
- SucralfateDocument3 pagesSucralfateViziteu AlexandraPas encore d'évaluation
- Drug Study: Aspirin (Asa)Document5 pagesDrug Study: Aspirin (Asa)Shara Lailanie A. AzisPas encore d'évaluation
- TriageDocument8 pagesTriageSarah GuintoPas encore d'évaluation
- KaliumDocument2 pagesKaliumJustine Kaye Iballa HarligaPas encore d'évaluation
- AutismDocument10 pagesAutismapi-314229616100% (1)
- Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeDocument4 pagesTotal Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeMiar QuestPas encore d'évaluation
- HyperphosphatemiaDocument2 pagesHyperphosphatemiatephPas encore d'évaluation
- Drug Class:: Prototype (Generic/Trade) : Eskalith, LithobidDocument1 pageDrug Class:: Prototype (Generic/Trade) : Eskalith, LithobidAaLona Robinson100% (2)
- Generic Name T Rade Name Classification Diltiazem Cardizem Antianginals, AntiarrhythmicsDocument1 pageGeneric Name T Rade Name Classification Diltiazem Cardizem Antianginals, AntiarrhythmicsChristopher LeePas encore d'évaluation
- Renal Concept MapDocument8 pagesRenal Concept MapXtine CajiPas encore d'évaluation
- Ketesse Pain Reliever GuideDocument8 pagesKetesse Pain Reliever GuideDhurai OnelyPas encore d'évaluation
- NCP For Impaired Oral Mucous MembraneDocument11 pagesNCP For Impaired Oral Mucous MembraneRYAN SAPLADPas encore d'évaluation
- Metformin: Dosing & UsesDocument8 pagesMetformin: Dosing & UsesMaria Alejandra Siachoque JaraPas encore d'évaluation
- UrethritisDocument11 pagesUrethritismarej143Pas encore d'évaluation
- Brand Name: Generic Name: Drug ClassificationDocument2 pagesBrand Name: Generic Name: Drug ClassificationChristine Pialan SalimbagatPas encore d'évaluation
- Drug Study CADocument8 pagesDrug Study CAAna Marie Besa Battung-ZalunPas encore d'évaluation
- Patient Education Power Point DVTDocument14 pagesPatient Education Power Point DVTMihaela PopescuPas encore d'évaluation
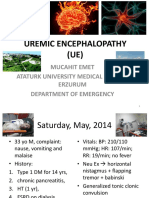
- Uremic EncephalophatyDocument48 pagesUremic EncephalophatySindi LadayaPas encore d'évaluation
- Case PresentationDocument6 pagesCase PresentationYrrem UbaganPas encore d'évaluation
- DM Case StudyDocument21 pagesDM Case StudyBern TolentinoPas encore d'évaluation
- CLONIDINE HYDROCHLORIDE: Cardiovascular and Analgesic AgentDocument2 pagesCLONIDINE HYDROCHLORIDE: Cardiovascular and Analgesic AgentDOni CorleonePas encore d'évaluation
- Drug Study - PiptazDocument1 pageDrug Study - PiptazMutya XDPas encore d'évaluation
- Maternal & Child Health NursingDocument22 pagesMaternal & Child Health Nursingtoledanagerald516Pas encore d'évaluation
- NCM 104 (DUTY) - Risperidone Drug StudyDocument1 pageNCM 104 (DUTY) - Risperidone Drug StudyArthur Christopher CorpuzPas encore d'évaluation
- Anes Drugs TableDocument20 pagesAnes Drugs TableKathleen Grace ManiagoPas encore d'évaluation
- Drug PrilosecDocument1 pageDrug PrilosecSrkocher100% (1)
- DimenhydrinateDocument2 pagesDimenhydrinateNinoska Garcia-Ortiz100% (1)
- Don't Get Bitten! Rabies Prevention TipsDocument24 pagesDon't Get Bitten! Rabies Prevention TipsTheother OnePas encore d'évaluation
- Page 17 ACUTE PAIN Related To Joint Stiffness Secondary To Aging.Document3 pagesPage 17 ACUTE PAIN Related To Joint Stiffness Secondary To Aging.Senyorita KHayePas encore d'évaluation
- Fluoracil Drug StudyDocument3 pagesFluoracil Drug StudyNicole Louize CaloraPas encore d'évaluation
- Drug Study: Phinma University of PangasinanDocument4 pagesDrug Study: Phinma University of PangasinanBrythym De GuzmanPas encore d'évaluation
- Drug StudyDocument4 pagesDrug StudyArdy PadamadaPas encore d'évaluation
- Chronic Kidney DiseaseDocument36 pagesChronic Kidney Diseasejabir100% (1)
- Potassium Chloride Injection Product MonographDocument18 pagesPotassium Chloride Injection Product MonographMatthew ParsonsPas encore d'évaluation
- Availability: Classifications: Antihistamine Antipruritic Pregnancy Category: CDocument4 pagesAvailability: Classifications: Antihistamine Antipruritic Pregnancy Category: CCay SevillaPas encore d'évaluation
- NCP Based On GordonsDocument10 pagesNCP Based On GordonsFate Ann Candle Dagutao100% (1)
- Availability: Classifications: Central Nervous System Agent Nsaid (Cox-1) Analgesic Antipyretic Pregnancy Category: BDocument4 pagesAvailability: Classifications: Central Nervous System Agent Nsaid (Cox-1) Analgesic Antipyretic Pregnancy Category: BCay SevillaPas encore d'évaluation
- DSM-IV Schizophrenia Types and AssessmentDocument32 pagesDSM-IV Schizophrenia Types and AssessmentJoyVee Pillagara-De LeonPas encore d'évaluation
- CVDDocument22 pagesCVDvijaymusic88100% (1)
- Regular Insulin: A Drug Study OnDocument9 pagesRegular Insulin: A Drug Study OnSophia IbuyanPas encore d'évaluation
- Drug Study CovidDocument5 pagesDrug Study CovidR Hornilla Arcega0% (1)
- Septic Shock: Supervisor: DR Ali Haedar, Sp. EM FAHA Dinisa Novaurahmah Nanin Aprilia PutriDocument42 pagesSeptic Shock: Supervisor: DR Ali Haedar, Sp. EM FAHA Dinisa Novaurahmah Nanin Aprilia PutriMutia Larasati AlbarPas encore d'évaluation
- Name of Drug Mechanism: MemantineDocument4 pagesName of Drug Mechanism: MemantineCarlmeister Ambray JudillaPas encore d'évaluation
- Generic NameDocument2 pagesGeneric NamePerdie Branden ReizPas encore d'évaluation
- Cyanosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandCyanosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÉvaluation : 5 sur 5 étoiles5/5 (1)
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Hypocalcemia, (Low Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandHypocalcemia, (Low Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- DiagnosticDocument3 pagesDiagnosticMarc AnchetaPas encore d'évaluation
- Types of Bone Fractures and Common Traction MethodsDocument3 pagesTypes of Bone Fractures and Common Traction MethodsMarc AnchetaPas encore d'évaluation
- DefinitionDocument4 pagesDefinitionMarc AnchetaPas encore d'évaluation
- Case Study (Acute Pyelonephritis) FINALDocument20 pagesCase Study (Acute Pyelonephritis) FINALian-movilla-751780% (10)
- Monitoring Fever and Breathing PatternsDocument4 pagesMonitoring Fever and Breathing PatternsMarc AnchetaPas encore d'évaluation
- Drug Study OSDocument9 pagesDrug Study OSMarc AnchetaPas encore d'évaluation
- Diabetes Mellitus 2Document25 pagesDiabetes Mellitus 2Marc AnchetaPas encore d'évaluation
- NCPpneumoniaDocument3 pagesNCPpneumoniamykat19Pas encore d'évaluation
- NCP HaDocument4 pagesNCP HaMarc AnchetaPas encore d'évaluation
- ECE SAR OldDocument168 pagesECE SAR OldNagaraja RaoPas encore d'évaluation
- Training Report On Machine LearningDocument27 pagesTraining Report On Machine LearningBhavesh yadavPas encore d'évaluation
- Financial ManagementDocument2 pagesFinancial ManagementSanna KazmiPas encore d'évaluation
- MMME 21 1st Long Exam Lecture NotesDocument74 pagesMMME 21 1st Long Exam Lecture NotesGraver lumiousPas encore d'évaluation
- A Report On Kantajew MandirDocument21 pagesA Report On Kantajew MandirMariam Nazia 1831388030Pas encore d'évaluation
- Lecture01 PushkarDocument27 pagesLecture01 PushkarabcdPas encore d'évaluation
- Ed Brown CatalogDocument44 pagesEd Brown CatalogssnvetPas encore d'évaluation
- Concise Operating Instructions: Frequency Converter For HOISTING - TRAVEL (Siemens)Document9 pagesConcise Operating Instructions: Frequency Converter For HOISTING - TRAVEL (Siemens)Pablo Hidalgo ValenzuelaPas encore d'évaluation
- Natural GasDocument86 pagesNatural GasNikhil TiwariPas encore d'évaluation
- Introduction to Globalization ExplainedDocument27 pagesIntroduction to Globalization ExplainedMichael Ron DimaanoPas encore d'évaluation
- X-Ray Generator Communication User's Manual - V1.80 L-IE-4211Document66 pagesX-Ray Generator Communication User's Manual - V1.80 L-IE-4211Marcos Peñaranda TintayaPas encore d'évaluation
- Syllabus PTSV3Document21 pagesSyllabus PTSV3Pablito Quispe RuizPas encore d'évaluation
- ASIA IVALUE Business ProfileDocument9 pagesASIA IVALUE Business ProfileDidiek PriambudiPas encore d'évaluation
- Document 25Document455 pagesDocument 25Pcnhs SalPas encore d'évaluation
- Introduction To Financial Planning Unit 1Document57 pagesIntroduction To Financial Planning Unit 1Joshua GeddamPas encore d'évaluation
- BC Sample Paper-3Document4 pagesBC Sample Paper-3Roshini APas encore d'évaluation
- Transformers Obj Questions PDFDocument8 pagesTransformers Obj Questions PDFphaniputta100% (2)
- Gartner CRM Handbook FinalDocument0 pageGartner CRM Handbook FinalghanshyamdassPas encore d'évaluation
- HFH ch04Document11 pagesHFH ch04Harikrishan RPas encore d'évaluation
- Danbury BrochureDocument24 pagesDanbury BrochureQuique MartinPas encore d'évaluation
- Finding The Answers To The Research Questions (Qualitative) : Quarter 4 - Module 5Document39 pagesFinding The Answers To The Research Questions (Qualitative) : Quarter 4 - Module 5Jernel Raymundo80% (5)
- 2008-14-03Document6 pages2008-14-03RAMON CALDERONPas encore d'évaluation
- Mechanism of Heat TransferDocument31 pagesMechanism of Heat Transferedna padrePas encore d'évaluation
- Parts of The Analog MultitesterDocument4 pagesParts of The Analog MultitesterDestiny Marasigan CanacanPas encore d'évaluation
- Ce Brochure 20july16Document76 pagesCe Brochure 20july16Yogesh SharmaPas encore d'évaluation
- 2019 Implementasie-SamsatdiBaliDocument10 pages2019 Implementasie-SamsatdiBaliDiannita SusantiPas encore d'évaluation
- 2 Integrated MarketingDocument13 pages2 Integrated MarketingPaula Marin CrespoPas encore d'évaluation
- Psych 1xx3 Quiz AnswersDocument55 pagesPsych 1xx3 Quiz Answerscutinhawayne100% (4)
- Computer ViruesDocument19 pagesComputer ViruesMuhammad Adeel AnsariPas encore d'évaluation
- NOV Completion ToolsDocument12 pagesNOV Completion Toolsfffggg777Pas encore d'évaluation