Académique Documents
Professionnel Documents
Culture Documents
Drug Medicine
Transféré par
Dereck Martil LibaoDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Drug Medicine
Transféré par
Dereck Martil LibaoDroits d'auteur :
Formats disponibles
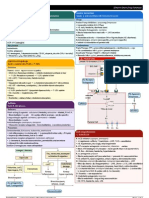
DRUG
MECHANISM OF ACTION Inhibits the enzyme responsible for the conversion of purines to uric acid, thus reducing the production of uric acid with a decrease in serum and sometimes in urinary uric acid levels, relieving the signs and symptoms of gout
Indicatioins
ADVERSE REACTIONS
NURSING RESPONSIBILITIES Assessment
allopurinol (al oh pure i nole) Aloprim, ApoAllopurinol (CAN), Purinol (CAN), Zyloprim Pregnancy Category C Drug class
Antigout drug
Management of the signs and symptoms of primary and secondary gout Management of patients with malignancies that result in elevations of serum and urinary uric acid Management of patients with recurrent calcium oxalate calculi whose daily uric acid excretion exceeds 800 mg/day (males) or 750 mg/day (females) Orphan drug use: Treatment of Chagas disease; cutaneous and visceral leishmaniasis Unlabeled uses: Amelioration of granulocyte suppression with 5-FU; as a mouthwash to prevent 5-FU-induced stomatitis
CNS: Headache, drowsiness, peripheral neuropathy, neuritis, paresthesias Dermatologic: Rashes maculopapular, scaly or exfoliativesometimes fatal GI: Nausea, vomiting, diarrhea, abdominal pain, gastritis, hepatomegaly, hyperbilirubinemia, cholestatic jaundice GU: Exacerbation of gout and renal calculi, renal failure Hematologic: Anemia, leukopenia, agranulocytosis, thrombocytopenia, aplastic anemia, bone marrow depression
History: Allergy to allopurinol, blood dyscrasias, liver disease, renal failure, lactation
Physical: Skin lesions, color; orientation, reflexes; liver evaluation, normal urinary output; normal output; CBC, LFTs, renal function tests, urinalysis Interventions
Administer drug following meals. Encourage patient to drink 2.5 to 3 L/day to decrease the risk of renal stone development.
Check urine alkalinityurates crystallize in acid urine; sodium bicarbonate or potassium citrate may be ordered to alkalinize urine. WARNING: Discontinue drug at first sign of skin rash; severe to fatal skin reactions have occurred. Arrange for regular medical follow-up and blood tests.
Teaching points
Take the drug after meals.
Avoid over-the-counter medications. Many of these preparations contain vitamin C or other agents that might increase the likelihood of kidney stone formation. If you need an over-the-counter preparation, check with your health care provider. You may experience these side effects: Exacerbation of gouty attack or renal stones (drink 2.53 liters of fluids per day while on this drug); nausea, vomiting, loss of appetite (takes after meals or eat frequent small meals); drowsiness (use caution while driving or performing hazardous tasks). Report unusual bleeding or bruising; fever, chills; gout attack; numbness or tingling; flank pain, skin rash. Generic Name : captopril Brand Names: Captopril competitively inhibits the conversion of angiotensin I (ATI) to angiotensin II (ATII), thus resulting in reduced ATII levels and aldosterone secretion. It also increases plasma renin activity and bradykinin levels. Reduction of ATII leads to decreased sodium and water retention. By these mechanisms, captopril produces a hypotensive effect and a beneficial effect in congestive heart failure.
Apo-Capto (CAN), Capoten, Gen-Captopril (CAN), Novo-
Treatment of hypertension alone or in combination with thiazide-type diuretics Treatment of CHF in patients unresponsive to conventional therapy; used with diuretics and digitalis Treatment of diabetic nephropathy Treatment of left ventricular dysfunction after MI Unlabeled uses: Management of
Hypotension, tachycardia, chest pain, palpitations, pruritus, hyperkalemia. Proteinuria; angioedema, skin rashes; taste disturbance, nonproductive cough, headache. Potentially Fatal: Neutropenia, usually occurs within 3 mth of starting therapy especially in patients with renal dysfunction or collagen
Assessment History: Allergy to captopril, history of angioedema, impaired renal function, CHF, salt or volume depletion, pregnancy, lactation Physical: Skin color, lesions, turgor; T; P, BP, peripheral perfusion; mucous membranes, bowel sounds, liver evaluation; urinalysis, LFTs, renal function tests, CBC and differential Interventions Administer 1 hr before meals.
Captopril (CAN), Nu-Capto (CAN) Classification: ACE inhibitor, Antihypertensive
hypertensive crises; treatment of rheumatoid arthritis; diagnosis of anatomic renal artery stenosis, hypertension related to scleroderma renal crisis; diagnosis of primary aldosteronism, idiopathic edema; Bartters syndrome; Raynauds syndrome
diseases. Hyperkalaemia. Anaphylactic reactions.
WARNING: Ensure that patient is not pregnant before beginning treatment. Encourage use of contraceptives; if pregnancy is detected, stop drug. WARNING: Alert surgeon and mark patients chart with notice that captopril is being taken; the angiotensin II formation subsequent to compensatory renin release during surgery will be blocked; hypotension may be reversed with volume expansion. Monitor patient closely for fall in BP secondary to reduction in fluid volume (due to excessive perspiration, and dehydration, vomiting, or diarrhea); excessive hypotension may occur. Reduce dosage in patients with impaired renal function. Teaching points
Pregnancy Category C (first trimester) Pregnancy Category D (second and third trimesters)
Take drug 1 hour before meals; do not take with food. Do not stop without consulting your health care provider. Be careful of drop in blood pressure (occurs most often with diarrhea, sweating, vomiting, or dehydration); if light-headedness or dizziness occurs, consult your health care provider. Severe fetal damage can occur if captopril is taken during pregnancy. Use of contraceptives is advised; if pregnancy should occur, stop drug and notify health care provider. Avoid over-the-counter medications, especially cough, cold, allergy medications that may contain ingredients that will interact with ACE inhibitors. Consult your health care provider. You may experience these side effects: Cough, GI upset, loss of appetite, change in taste perception (limited effects, will pass); mouth sores (frequent mouth care may help); rash; fast heart rate; dizziness, light-headedness (usually passes after the first few days; change position slowly, and limit your activities to those that do not require alertness and precision). Report mouth sores; sore throat, fever, chills; swelling of the hands or feet; irregular heartbeat, chest pains; swelling of the face, eyes, lips or tongue; difficulty breathing.
LEVOFLOXACIN Antibiotic fluroquinolones
Levofloxacin is a broad-spectrum antibiotic that is active against both Gram-positive and Gramnegative bacteria. It functions by inhibiting DNA gyrase, a type II topoisomerase, and topoisomerase iv,[99]which is an enzyme necessary to separate replicated DNA, thereby inhibiting cell division.
Levofloxacin pharmacokinetics are linear and predictable after single and multiple oral or IV dosing regimens. Levofloxacin is rapidly and, in essence, completely absorbed after oral administration. Peak plasma concentrations are usually attained one to two hours after oral dosing. The plasma concentration profile of levofloxacin after IV administration is similar and comparable in extent of exposure (AUC) to that observed for LEVAQUIN Tablets when equal doses (mg/mg) are administered. Levofloxacin is excreted largely as unchanged drug in the urine. The mean terminal plasma elimination half-life of levofloxacin ranges from approximately 6 to 8 hours
The serious adverse effects that may occur as a result of levofloxacin therapy include irreversible peripheral neuropathy, [52][62] spontaneous tendon rupture and tendonitis,[8][9][63][64][65] QTc prolongation/torsades de pointes, [8] toxic epidermal necrolysis (TEN) [8] and Stevens-Johnson syndrome, erythema multiforme, [66] severe central nervous system disorders (CNS), including seizures[67][68] and clostridium difficile associated disease (CDAD: Pseudomembranous colitis)[69][70][71] [72] photosensitivity/phototoxicity reactions,[66][73] fatal hypoglycemia,
Levofloxacin should be administered only as described within the Dosage Guidelines table found within the most current package insert. The status of the patient's renal function and hepatic functionmust also be taken into consideration to avoid an accumulation that may lead to a fatal drug overdose. Levofloxacin is eliminated primarily by renal excretion. However, the drug is also metabolized and partially cleared through the liver and the intestine. Modification of the dosage is recommended using the table found within the package insert for those with impaired liver or kidney function (particularly for patients with severe renal dysfunction). Within the package insert, it is stated "...since the drug is known to be substantially excreted by the kidneys, the risk of toxic reactions to this drug may be greater in patients with impaired renal function."[5] The duration of treatment depends upon the severity of infection and the duration varies anywheres from 3 days to 60 days.[5] Note: The patient's serum levels should be monitored during therapy to avoid a drug overdose. See the most current package insert for proper dosing guidelines and relevant warnings/precautions.
following single or multiple doses of levofloxacin given orally or intravenously.[5][7] Glucuronidation and hydroxylation have been cited as one of the major metabolic pathways for levofloxacin hydrochloride.[98] However the drug card for levofloxacin (DB01137) states that the biotransformation information is not [7] available. Specific information regarding biotransformation does not appear to be readily available within the package inserts.
[74] [75]
kidney damage, rhabdomyolysis (muscle wasting),[56][76][77] as well as anaphylactoid reactions[78][79] and myasthenia crisis.[80] Additional serious adverse reactions include acute pancreatitis, [81][82] temporary as well as permanent loss of vision, irreversible double vision, [83] impaired color vision, exanthema, abdominal pain, malaise, drug fever,[84] dysaesthesia and eosinophilia. Pseudotumor cerebri, commonly known as idiopathic intracranial hypertension (IIH), (also referred to as increased intracranial pressure),[85] has been reported to occur as a serious adverse reaction to levofloxacin. Another serious adverse effect is autoimmune hemolytic anemia.
[86]
aspirin (ass pir in) Apo-ASA (CAN), Aspergum, Bayer, Easprin, Ecotrin, Empirin, Entrophen (CAN), Genprin, Halfprin 81, 1/2 Halfprin, Heartline, Norwich, Novasen (CAN), PMS-ASA (CAN), ZORprin Buffered aspirin products: Alka-Seltzer, Ascriptin, Asprimox, Bufferin, Buffex, Magnaprin Pregnancy Category D
Analgesic and antirheumatic effects are attributable to aspirins ability to inhibit the synthesis of prostaglandins, important mediators of inflammation. Antipyretic effects are not fully understood, but aspirin probably acts in the thermoregulatory center of the hypothalamus to block effects of endogenous pyrogen by inhibiting synthesis of the prostaglandin intermediary. Inhibition of platelet aggregation is attributable to the inhibition of platelet synthesis of thromboxane A2, a potent vasoconstrictor and inducer of platelet aggregation. This effect occurs at low doses and lasts for the life of the platelet (8 days). Higher doses inhibit the synthesis of prostacyclin, a potent vasodilator and inhibitor of platelet aggregation.
Mild to moderate pain Fever
Inflammatory conditions rheumatic fever, rheumatoid arthritis, osteoarthritis Reduction of risk of recurrent TIAs or stroke in males with history of TIA due to fibrin platelet emboli Reduction of risk of death or nonfatal MI in patients with history of infarction or unstable angina pectoris MI prophylaxis
Unlabeled use: Prophylaxis against cataract formation with long-term use
Acute aspirin toxicity: Respiratory alkalosis, hyperpnea, tachypnea, hemorrhage, excitement, confusion, asterixis, pulmonary edema, seizures, tetany, metabolic acidosis, fever, coma, CV collapse, renal and respiratory failure (dose related, 2025 g in adults, 4 g in children) Aspirin intolerance: Exacerbation of bronchospasm, rhinitis (with nasal polyps, asthma, rhinitis) GI: Nausea, dyspepsia, heartburn, epigastric discomfort, anorexia, hepatotoxicity Hematologic: Occult
Assessment of aspirin
History: Allergy to salicylates or NSAIDs; allergy to tartrazine; hemophilia, bleeding ulcers, hemorrhagic states, blood coagulation defects, hypoprothrombinemia, vitamin K deficiency; impaired hepatic function; impaired renal function; chickenpox, influenza; children with fever accompanied by dehydration; surgery scheduled within 1 wk; pregnancy; lactation Physical: Skin color, lesions; T; eighth cranial nerve function, orientation, reflexes, affect; P, BP, perfusion; R, adventitious sounds; liver evaluation, bowel sounds; CBC, clotting times, urinalysis, stool guaiac, LFTs, renal function tests Interventions of aspirin
BLACK BOX WARNING: Do not use in children and teenagers to treat chickenpox or flu symptoms without review for Reyes syndrome, a rare but fatal disorder. Give drug with food or after meals if GI upset occurs. Give drug with full glass of water to reduce risk of tablet or capsule lodging in the esophagus. Do not crush, and ensure that patient does not chew SR preparations. Do not use aspirin that has a strong vinegar-like odor.
Drug classes of aspirin
Antipyretic
Analgesic (nonopioid) Antiinflammatory Antirheumatic
blood loss, hemostatic defects Hypersensitivity: Anap hylactoid reactions to anaphylactic shock Salicylism: Dizziness, tinnitus, difficulty hearing, nausea, vomiting, diarrhea, mental confusion, lassitude (dose related)
WARNING: Institute emergency procedures if overdose occurs: Gastric lavage, induction of emesis, activated charcoal, supportive therapy. Teaching points of aspirin
Take extra precautions to keep this drug out of the reach of children; this drug can be very dangerous for children. Use the drug only as suggested; avoid overdose. Avoid the use of other over-the-counter drugs while taking this drug. Many of these drugs contain aspirin, and serious overdose can occur. Take the drug with food or after meals if GI upset occurs.
Antiplatelet Salicylate NSAID
Do not cut, crush, or chew sustained-release products. Over-the-counter aspirins are equivalent. Price does not reflect effectiveness.
You may experience these side effects: Nausea, GI upset, heartburn (take drug with food); easy bruising, gum bleeding (related to aspirins effects on blood clotting). Report ringing in the ears; dizziness, confusion; abdominal pain; rapid or difficult breathing; nausea, vomiting, bloody stools.
ISDN Isosorbide dinitrate belongs to the class of medications called antianginals.
It works by relaxing blood vessels and increasing the blood and oxygen supply to the heart. Isosorbide dinitrate may reduce the number, length, and severity of angina attacks. Tolerance for exercise may be increased and the need for fastacting nitroglycerin (tablets and spray) may be reduced.
It is used to prevent chest pain associated with angina
dizziness or lightheadedness, especially when getting up from a lying or sitting position fast pulse flushing of face and neck headache nausea or vomiting restlessness blurred vision dryness of mouth fainting headache (severe or prolonged) skin rash
Assessment & Drug Effects
Monitor effectiveness of drug in relieving angina. Note: Headaches tend to decrease in intensity and frequency with continued therapy but may require administration of analgesic and reduction in dosage. Note: Chronic administration of large doses may produce tolerance and thus decrease effectiveness of nitrate preparations.
Patient & Family Education
Make position changes slowly, particularly from recumbent to upright posture, and dangle feet and ankles before walking. Lie down at the first indication of light-headedness or faintness. Keep a record of anginal attacks and the number of sublingual tablets required to provide relief. Do not drink alcohol because it may increase possibility of light-headedness and faintness. Do not breast feed while taking this drug without consulting physician.
(e-noxa-pa-rin) Lovenox Classifications: blood formers, coagulators, and
Enoxaparin is a blood thinner, also called anticoagulant (an-tye-koeAG-yoo-lant). Enoxaparin prevents
Enoxaparin is used to prevent blood clots that are sometimes called deep vein thrombosis (DVT), which can lead to blood clots in the lungs. A DVT can
bleeding that won't pale skin, easy
stop;
Assessment & Drug Effects Lab tests: Baseline coagulation studies; periodic CBC, platelet count, urine and stool for occult blood.
Monitor platelet count closely. Withhold drug and notify physician if platelet count less than
anticoagulants; low molecular weight heparin Pregnancy Category: B
the formation of blood clots.
occur after certain types of surgery, or in people who are bed-ridden due to a prolonged illness. DVT sometimes occurs suddenly for other reasons. Enoxaparin is also used to prevent blood vessel complications in people with certain types of angina (chest pain) or heart attacks called non-Q-wave myocardial infarction or ST-segment elevation myocardial infarction. Enoxaparin may also be used for other purposes not listed in this medication guide.
bruising, unusual weakness; swelling, bruising, or bleeding where an incision was made during a surgery or other medical procedure; sudden numbness or weakness, headache, confusion, problems with vision, speech, or balance; pain or swelling in one or both legs; cough, chest pain, trouble breathing; or slow heart rate, weak pulse, muscle weakness, tingly feeling. Less serious side effects may include:
100,000/mm3. Monitor closely patients with renal insufficiency and older adults who are at higher risk for thrombocytopenia. Monitor for and report immediately any sign or symptom of unexplained bleeding. Patient & Family Education Report to physician promptly signs of unexplained bleeding such as: pink, red, or dark brown urine; red or dark brown vomitus; bleeding gums or bloody sputum; dark, tarry stools. Do not take any OTC drugs without first consulting physician.
Do not breast feed while taking this drug without consulting physician.
nausea, diarrhea;
swelling in your hands or feet; or mild swelling, pain, bruising, or redness where the medicine was injected.
Brand Name: TRAMADOL CLASSIFICATIONS Therapeutic: Analgesics (centrally acting)
Physiologic Mechanism Decreased pain. Pharmacologic Mechanism Binds to mu-opioid receptors. Inhibits reuptake of serotonin and norepinephrine in the CNS.
Moderate to moderately severe pain
Respiratory depression Seizures Prolonged duration of action and cumulative effect may occur in patients with impaired hepatic or renal function.
Assess type, location, and intensity of pain before and 2-3 hr (peak) after administration. Assess BP & RR before and periodically during administration. Respiratory depression has not occurred with recommended doses. Assess bowel function routinely. Prevention of constipation should be instituted with increased intake of fluids and bulk and with laxatives to minimize constipating effects. Assess previous analgesic history. Tramadol is not recommended for patients dependent on opioids or who have previously received opioids for more than 1 wk; may cause opioid withdrawal symptoms. Prolonged use may lead to physical and psychological dependence and tolerance, although these may be milder than with opioids. This should not prevent patient from receiving adequate analgesia. Most patients who receive tramadol for pain d not develop psychological dependence. If tolerance develops, changing to an opioid agonist may be required to relieve pain. Tramadol is considered to provide more analgesia than codeine 60 mg but less than combined aspirin 650mg/codeine 60 mg for acute postoperative pain. Monitor patient for seizures. May occur within recommended dose range. Risk increased with higher doses and inpatients taking antidepressants (SSRIs, tricyclics, or Mao inhibitors), opioid analgesics, or other durgs that decrese the seizure threshold. Overdose may cause respiratory depression and seizures. Naloxone (Narcan) may reverse some, but not all, of the symptoms of overdose. Treatment should be symptomatic and supportive. Maintain adequate respiratory
exchange. Encourage patient to cough and breathe deeply every 2 hr to prevent atelactasis and pneumonia.
Brand Name: ApoMetoprolol (CAN), Betaloc (CAN), Lopresor (CAN), Lopressor, Novometoprol (CAN), Nu-Metop (CAN), Toprol-XL Pregnancy Category C Drug classes: Beta1selective adrenergic blocker, Antihypertensive
Competitively blocks betaadrenergic receptors in the heart and juxtaglomerular apparatus, decreasing the influence of the sympathetic nervous system on these tissues and the excitability of the heart, decreasing cardiac output and the release of renin, and lowering BP; acts in the CNS to reduce sympathetic outflow and vasoconstrictor tone.
Hypertension, alone or with other drugs, especially diuretics Prevention of reinfarction in MI patients who are hemodynamically stable or within 310 days of the acute MI (immediate-release tablets and injection) Treatment of angina pectoris Treatment of stable, symptomatic CHF of ischemic, hypertensive, or cardiomyopathic origin (Toprol-XL only)
Pharyngitis, erythematous rash, fever, sore throat, laryngospasm Dizziness, vertigo, tinnitus, fatigue, emotional depression, paresthesias, sleep disturbances, hallucinations, disorientation, memory loss, slurred speech CHF, cardiac arrhythmias, peripheral vascular insufficiency, claudication, CVA, pulmonary edema, hypotension Rash, pruritus, sweating, dry skin Eye irritation, dry eyes, conjunctivitis, blurred vision Gastric pain, flatulence, constipation, diarrhea, nausea, vomiting, anorexia, ischemic colitis, renal and mesenteric arterial thrombosis, retroperitoneal fibrosis, hepatomegaly, acute pancreatitis Impotence, decreased libido, Peyronie's disease, dysuria, nocturia, frequent urination The most frequently reported adverse reactions were diarrhea in 3% of the patients and rash in less than 2% of the patients. Additional systemic reactions reported in less than 1% of the patients were: itching,nausea, vomiting, candidiasis, fatigue, mala ise, headache, chest pain, flatulence,abdominal distensi on, glossitis, urine retention, dysuri a, edema, facial swelling,erythema, chills, tightness in throat, substernal pain, epistaxis and mucosal bleeding
Do not discontinue drug abruptly after long-term therapy (hypersensitivity to catecholamines may have developed, causing exacerbation of angina, MI, and ventricular arrhythmias). Taper drug gradually over 2 wk with monitoring. Ensure that patient swallows the ER tablets whole; do not cut, crush, or chew. Consult physician about withdrawing drug if patient is to undergo surgery (controversial). Give oral drug with food to facilitate absorption. Provide continual cardiac monitoring for patients receiving IV metoprolol.
SULBACTAMBrand Name: UNASYN CLASSIFICATIONS Therapeutic: Anti-infectives Pharmacologic: Aminopenicillins/ beta lactamase inhibitors
Physiologic Mechanism Bactericidal action. Active against: Streptococci, Penumococci, Enterococci, Haemophilus influenzae, Use should be reserved for infections caused by beta-lactamaseproducing strains. Pharmacologic Mechanism Binds to bacteria cell wall, resulting in cell death, spectrum is broader than that of penicillin. Addition of sulbactam increases resistance to beta-lactamase, enzymes produced by bacteria that may inactivate ampicillin.
Treatment of respiratory infections
Assess patient for infection (vital signs, wound appearance, sputum, urine, stool, and WBCs) at beginning and throughout therapy. Obtain a history before initiating therapy to determine previous use of and reactions to penicillins or cephalosporins. Persons with a negative history of penicillin sensitivity may still have an allergic response. Obtain specimens for culture and sensitivity before therapy. First dose may be given before receiving results. Observe patients for signs and symptoms of anaphylaxis (rash, pruritus, laryngeal edema, wheezing). Discontinue the drug and notify the physician immediately if these occur. Keep epinephrine, an antihistamine, and resuscitation equipment close by in the event of an anaphylactic reaction. Caution patient to notify physician if fever and diarrhea occur, especially if stool contains blood, pus, or mucus. Advise patient not to treat diarrhea without consulting health care professional. May occur up to several weeks after discontinuation of medication. Instruct patient to notify physician if symptoms do not improve.
Generic
It relieves nasal congestion and reversible bronchospasm by relaxing
Indications 1. To control and prevent
1. 2.
Nervousness Restlessness
1. 2.
Assess lung sounds, PR and BP before drug administration and during peak of medication. Observe fore paradoxical spasm and withhold medication and notify physician if condition occurs.
Name: Albuterol Brand Name: Salbutamol, Proventil, Ventolin, Accuneb, airet, NovoSalbutamol, Proventil HFA, Gen-salbutamol, Ventodisk, Ventolin HFA, Volmax, VoSpira ER Classification: Bronchod ilator (therapeutic); adrenergics (pharmacologic)
the smooth muscles of the bronchioles. The relief from nasal congestion and bronchospasm is made possible by the following mechanism that takes place when Salbutamol is administered. 1. First, it binds to the beta2-adrenergic receptors in the airway of the smooth muscle which then leads to the activation of the adenyl cyclase and increased levels of cyclic35-adenosine monophosphate (cAMP). 2. When cAMP increases, kinases are activated. 3. Kinases inhibit the phosphorylation of myosin and decrease intracellular calcium. 4. Decreased in intracellular calcium will result to the relaxation of the smooth muscle airways.
reversible airway obstruction caused by asthma or chronic obstructive pulmonary disorder (COPD) 2. Quick relief for bronchospasm 3. For the prevention of exercise-induced bronchospasm 4. Long-term control agent for patients with chronic or persistent bronchospasm
3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13.
Tremor Headache Insomnia Chest pain Palpitations Angina Arrhythmias Hypertension Nausea and vomiting Hyperglycemia Hypokalemia
3. Administer PO medications with meals to minimize gastric irritation. 4. Extended-release tablet should be swallowed-whole. It should not be crushed or chewed. 5. If administering medication through inhalation, allow at least 1 minute between inhalation of aerosol medication. 6. Advise the patient to rinse mouth with water after each inhalation to minimize dry mouth. 7. Inform the patient that Albuterol may cause an unusual or bad taste.
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Opioid Agonists and AntagonistsDocument5 pagesOpioid Agonists and AntagonistsCas BuPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Medical EmergenciesDocument115 pagesMedical EmergenciesRamya ReddyPas encore d'évaluation
- Drug SummaryDocument5 pagesDrug Summarybriancripe100% (2)
- Chioma M. Okeoma (Eds.) - Chikungunya Virus - Advances in Biology, Pathogenesis, and Treatment-Springer International Publishing (2016)Document202 pagesChioma M. Okeoma (Eds.) - Chikungunya Virus - Advances in Biology, Pathogenesis, and Treatment-Springer International Publishing (2016)sayeed_opso100% (1)
- Modified Oswestry Low Back Pain Disability QuestionnaireDocument2 pagesModified Oswestry Low Back Pain Disability QuestionnaireVivis MvPas encore d'évaluation
- Zhang Et Al 2012Document9 pagesZhang Et Al 2012Meek ElPas encore d'évaluation
- Soapp R Sample WatermarkDocument2 pagesSoapp R Sample Watermarkapi-351447133Pas encore d'évaluation
- Pharmacology - Technology TrendsDocument2 pagesPharmacology - Technology TrendsGisellePas encore d'évaluation
- Pain Management Guidelines HCANJ May 12 FinalDocument31 pagesPain Management Guidelines HCANJ May 12 FinalSudin SamPas encore d'évaluation
- Anestesia y Analgesia Veterinaria Lumb Adjuvant Analgesics in Acute Pain ManagementDocument3 pagesAnestesia y Analgesia Veterinaria Lumb Adjuvant Analgesics in Acute Pain ManagementGilliPas encore d'évaluation
- Buscopan - Medicine To Treat Stomach Cramps and IBS - NHSDocument9 pagesBuscopan - Medicine To Treat Stomach Cramps and IBS - NHSAdityaWijayaPas encore d'évaluation
- Drug Study Rle Final 1Document18 pagesDrug Study Rle Final 1YBH Construction SupplyPas encore d'évaluation
- Post Operative Pain Management in Elderly Patients: Alketa Dervishi, Kiri ZallariDocument3 pagesPost Operative Pain Management in Elderly Patients: Alketa Dervishi, Kiri ZallarianuradhaPas encore d'évaluation
- Drug Study For AMCDocument3 pagesDrug Study For AMCTrixia RiveraPas encore d'évaluation
- Drug Study CSDocument7 pagesDrug Study CSFrancis MendozaPas encore d'évaluation
- A Longitudinal Supra-Inguinal Fascia Iliaca ComparDocument8 pagesA Longitudinal Supra-Inguinal Fascia Iliaca ComparSyahrul Mubarak Danar SumantriPas encore d'évaluation
- DARK Classics in Chemical Neuroscience: U 47700: AccessDocument9 pagesDARK Classics in Chemical Neuroscience: U 47700: AccessStephen RileyPas encore d'évaluation
- British Pain SocietyDocument76 pagesBritish Pain SocietyMoloce BeatricePas encore d'évaluation
- Pharmanovaprice List July ExcelDocument13 pagesPharmanovaprice List July ExcelSagar GargPas encore d'évaluation
- Hypertrophic Osteodystrophy: (A Bone Disease of Rapidly Growing Puppies)Document4 pagesHypertrophic Osteodystrophy: (A Bone Disease of Rapidly Growing Puppies)Gavrilo Janja VlajinacPas encore d'évaluation
- Treatment of Neuropathic Pain or Post Herpetic PainDocument8 pagesTreatment of Neuropathic Pain or Post Herpetic PainSalwa ZeinPas encore d'évaluation
- Test Bank For Pharmacology For Canadian Health Care Practice 2nd Edition LilleyDocument7 pagesTest Bank For Pharmacology For Canadian Health Care Practice 2nd Edition Lilleymoneyedcoronal1ah2y100% (25)
- Ncm-212-Pain Reliever and Anti-Inflammatory DrugsDocument8 pagesNcm-212-Pain Reliever and Anti-Inflammatory Drugskristine caminPas encore d'évaluation
- Paracetamol - DSDocument3 pagesParacetamol - DSEnoch LabianoPas encore d'évaluation
- Chronic Pancreatitis - Management - UpToDateDocument22 pagesChronic Pancreatitis - Management - UpToDateJose Miranda ChavezPas encore d'évaluation
- Orthopedic Nursing: - Bone FractureDocument67 pagesOrthopedic Nursing: - Bone FractureRachel QuionPas encore d'évaluation
- Gonzales Cannon May 30 IssueDocument30 pagesGonzales Cannon May 30 IssueGonzales CannonPas encore d'évaluation
- Legalizing Marijuana: Utilitarian ViewpointDocument3 pagesLegalizing Marijuana: Utilitarian ViewpointGiselle LisondraPas encore d'évaluation
- Forensic Medicine & Toxicology - Topical Past PapersDocument24 pagesForensic Medicine & Toxicology - Topical Past PapersRohama Qubra 279Pas encore d'évaluation
- P. PellucidaDocument32 pagesP. PellucidaMartin OgbacPas encore d'évaluation