Académique Documents
Professionnel Documents
Culture Documents
Bruins - IDAST Directo Del Frasco de HC P BGN - 2004
Transféré par
Nidiam2Description originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Bruins - IDAST Directo Del Frasco de HC P BGN - 2004
Transféré par
Nidiam2Droits d'auteur :
Formats disponibles
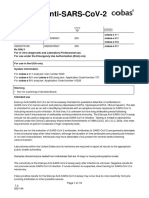
JOURNAL OF CLINICAL MICROBIOLOGY, Jan. 2004, p. 711 0095-1137/04/$08.00 0 DOI: 10.1128/JCM.42.1.711.2004 Copyright 2004, American Society for Microbiology.
. All Rights Reserved.
Vol. 42, No. 1
Identication and Susceptibility Testing of Enterobacteriaceae and Pseudomonas aeruginosa by Direct Inoculation from Positive BACTEC Blood Culture Bottles into Vitek 2
Marjan J. Bruins,* Peter Bloembergen, Gijs J. H. M. Ruijs, and Maurice J. H. M. Wolfhagen
Laboratory of Clinical Microbiology and Infectious Diseases, Isala Klinieken, 8021 AM Zwolle, The Netherlands
Received 29 August 2003/Returned for modication 26 September 2003/Accepted 7 October 2003
Inoculation of an automated system for rapid identication (ID) and antimicrobial susceptibility testing (AST) directly from positive blood culture bottles will reduce the turnaround time of laboratory diagnosis of septicemic patients, which benets clinical outcome and decreases patient costs. Direct test results, however, must always be conrmed by testing a pure overnight culture, which is the gold standard. We studied the accuracy of direct testing versus repeat testing in order to investigate the possibility of refraining from repeat testing. We also assessed the clinical risk of reporting results based on direct testing only. We inoculated Vitek 2 (bioMerieux) directly from 410 positive BACTEC 9240 (BD) blood culture bottles containing gram-negative rods and studied the ID and AST results. In a comparison of direct inoculation with the standard method, a total of 344 isolates of Enterobacteriaceae and Pseudomonas aeruginosa were tested, and 93.0% were correctly identied. Of the 39 (10.2%) samples that contained bacilli not identiable by Vitek 2, only 1 gave a conclusive, correct result. The overall MIC agreement among 312 isolates was 99.2%, with 0.8% very major and 0.02% major error rates. Of only three (polymicrobial) samples, the direct susceptibility pattern would be reported to the clinician as too sensitive. Vitek 2 results obtained from direct inoculation of blood culture bottles containing gram-negative bacilli are safe enough for immediate reporting, provided that ID and AST are consistent. Repeat testing is not necessary, unless Gram stain or overnight subculture results raise doubt about the purity of the culture. Shortening the turnaround time of microbiological analyses with an automated system for rapid identication and susceptibility testing of bacteria leads to a signicant reduction of patient morbidity, mortality, and cost (1, 2). In particular, for patients with septicemia, rapid laboratory results are essential for appropriate treatment and improving clinical outcome (21). An automated blood culture system that monitors culture bottles for microbial growth minimizes the time necessary to detect positive blood cultures. Another way to save time might be to inoculate an automated system for rapid identication and susceptibility testing directly from positive blood culture bottles. The conventional way is to wait for the overnight subculture on agar to prepare a standard inoculum according to the manufacturers guidelines. Of all bacteria involved in bloodstream infections, the fastgrowing Enterobacteriaceae will probably produce the quickest and best-correlating results for direct and standard inoculation. Several studies have compared direct and standard methods for different (combinations of) automated systems, but to our knowledge no study has yet done this for Vitek 2 (7, 8, 18, 20, 22). We routinely inoculate Vitek 2 directly from BACTEC 9240 blood culture bottles that are positive for gram-negative rods. To check the direct results, we repeat the tests the next day with suspensions made from pure cultures according to the Vitek 2 manufacturers instructions.
* Corresponding author. Mailing address: Isala Klinieken, Laboratory of Clinical Microbiology and Infectious Diseases, Rhijnvis Feithlaan 62, 8021 AM Zwolle, The Netherlands. Phone: 31-38-424-3111. Fax: 31-38-424-3146. E-mail: m.j.bruins@isala.nl. 7
Downloaded from jcm.asm.org by Daniel Sordelli on September 1, 2009
The two aspects we studied were (i) the accuracy of direct testing versus standard (repeat) testing in order to be able to refrain from repeat testing and (ii) the clinical risk of an approach using results of direct testing only.
MATERIALS AND METHODS Samples. The Laboratory of Clinical Microbiology and Infectious Diseases of the Isala Klinieken, a 1,100-bed, multisite hospital in Zwolle, The Netherlands, processes 9,500 blood cultures yearly by using the BACTEC 9240 system (software version V4.40A; culture bottles PLUS Aerobic/F and PLUS Anaerobic/F [BD, Erembodegem-Aalst, Belgium]). The data were collected from November 2000 to March 2003; during this period, every blood culture positive for gram-negative bacilli was inoculated into Vitek 2 directly, preferably from the aerobic bottle. Per patient, every rst positive culture of a septicemic episode containing gram-negative rods that appeared to be monomicrobial on Gram staining was included in the study. VT2. The Vitek 2 system (Vitek 2 software, version R02.03; Advanced Expert System [AES] software, version R02.00N [bioMerieux, Marcy lEtoile, France]) was used with the ID-GNB card and the AST-N020 card for identication (ID) and antimicrobial susceptibility testing (AST), respectively, of gram-negative bacilli. The antimicrobial agents tested were amikacin, amoxicillin-clavulanic acid, ampicillin, cefalotin, cefepime, cefotaxime, cefoxitin, cefpodoxime, ceftazidime, cefuroxime, ciprooxacin, gentamicin, meropenem, nitrofurantoin, noroxacin, ooxacin, piperacillin, piperacillin-tazobactam, tobramycin, and trimethoprim-sulfamethoxazole. Vitek 2 identies gram-negative rods within 3 h at the species level by interpreting 41 uorescent biochemical tests. If the biopattern does not match one particular taxon in the database, results are reported as low discrimination (2 to 3 taxa), inconclusive ( 3 taxa), or unidentied (no match). Ambiguous results due to slowly metabolizing nonfermenters are reported as various nonfermenting gram-negative bacilli. Susceptibility testing takes 5 to 19 h to obtain complete results. Vitek 2 needs a conclusive ID to establish and report denitive results. The AES analyzes whether ID and susceptibility data are consistent by consulting the phenotype descriptions in the database and, if necessary, recommends a correction in a MIC to complete the biological validation. The AES may also suggest a change in an
BRUINS ET AL.
J. CLIN. MICROBIOL.
interpretation from sensitive (S) to intermediate (I) or resistant (R), based on recognized resistance mechanisms, to prevent therapeutic failure. These changes of interpretation are according to the software parameters dened by the user (19). For the tests in the present study, interpretations as recommended by the National Committee for Clinical Laboratory Standards (15) and the AES conguration parameters set natural resistance, European hospitals, never more susceptible, and least risk were used. The AES knowledge base contains phenotypes of most Enterobacteriaceae and of Pseudomonas aeruginosa, Acinetobacter baumannii, Burkholderia cepacia, Pasteurella multocida, and Stenotrophomonas maltophilia (only trimethoprim-sulfamethoxazole). If a species other than these is identied, expert analysis cannot be completed. For this reason, if the standard inoculation method is used, in our laboratory we inoculate Vitek 2 according to the manufacturers instruction, but only with isolates that are suspected of being Enterobacteriaceae or P. aeruginosa, based on their appearance on (differential) agar media and biochemical reactions such as the oxidase test. Direct method. A serum separator tube (BD Vacutainer Systems, Plymouth, United Kingdom) was aseptically inoculated with 4 ml from a positive BACTEC 9240 bottle by using a 5-ml syringe, and a Gram stain was done. If the culture contained gram-negative rods and appeared to be monomicrobial, the tube was centrifuged at 1,525 g for 10 min, and the supernatant was carefully aspirated. With a cotton swab, the lm of bacteria on top of the gel layer was removed and used to make a 0.5 to 0.63 McFarland suspension in 3 ml of 0.45% saline (modication of Waites et al. [22]). The suspension was processed according to the standard Vitek 2 inoculation procedure. Standard method. Some of the blood culture uid was inoculated onto a combination of agar plates, suited for culturing aerobic, anaerobic, and fastidious microorganisms. After overnight incubation, several colonies of isolates suspected of being Enterobacteriaceae or P. aeruginosa were used to make a 0.5 to 0.63 McFarland suspension in 0.45% saline. The suspension was processed according to standard Vitek 2 inoculation procedure. Quality control. Weekly ID-GNB and AST-N020 cards were tested once each with Klebsiella oxytoca strain ATCC 700324 and Escherichia coli strain ATCC 25922, respectively. Data analysis. Direct and standard inoculation were compared for Enterobacteriaceae and P. aeruginosa, except for AST of Pantoea spp., for which genus the AES does not contain expert data. The Vitek 2 standard method results were used as the gold standard for ID testing, except in a few cases where the API system was necessary to provide the denitive identication. The Vitek 2 identications Klebsiella pneumoniae subsp. pneumoniae (planticola/terrigena) and K. pneumoniae subsp. ozaenae were considered identical and reported as K. pneumoniae; K. oxytoca and K. oxytoca (planticola/terrigena) were reported as K. oxytoca. Our category not identied includes the Vitek 2 reports inconclusive, unidentied, and terminated. For susceptibility testing, we compared direct and standard inoculation only of isolates with results biologically validated by Vitek 2 for both methods. The standard method results were considered the gold standard. The MIC agreement (direct MIC within one twofold dilution of the standard MIC) (14) without any changes made by the AES and discrepancies in interpretation after AES analysis were determined for each antibiotic. A minor error was dened as a susceptibility result of I by the direct method and S or R by the standard method or I by the standard method and S or R by the direct method. A major error was dened as R by the direct method and S by the standard method, and a very major error was dened as S by the direct method and R by the standard method. We also assessed the outcome of direct testing of blood cultures containing anaerobic, fastidious, and other gram-negative bacilli not identiable by Vitek 2. We investigated whether these results could lead to misleading reports if reporting was based on direct testing only. For these isolates standard diagnostic methods such as the API system (bioMerieux) were used for identication. If the agar plate culture of an apparently monomicrobial sample yielded two or more different species, we evaluated the therapeutic risk involved in the immediate reporting of the direct (mixed) susceptibility pattern.
blood bottles subculture. Table 1 lists the results of 383 direct identications from monomicrobial blood cultures. In all, 39 (10.2%) samples contained anaerobic, fastidious, or gram-positive bacilli or nonfermenting gram-negative rods other than P. aeruginosa. Of these, only one strain of S. maltophilia gave a conclusive result. Of 311 Enterobacteriaceae and 33 P. aeruginosa strains, 93.0% (320 of 344) were correctly identied, 2.6% (9 of 344) were reported as low discrimination, 2.3% (8 of 344) were not identied, and 2.0% (7 of 344) were misidentied according to our denitions. The ve most frequently isolated species were E. coli, P. aeruginosa, K. pneumoniae, Proteus mirabilis, and Enterobacter cloacae. Of the 320 correctly identied isolates of Enterobacteriaceae and P. aeruginosa, 8 were excluded from AST evaluation due to termination or omission of the standard method AST (n 4), a standard method identication result of low discrimination (n 2), an inconsistent direct ID and susceptibility pattern combination (n 1), or identication as Pantoea spp. (no expert analysis possible) (n 1). In all, 6,477 MICs were determined for 312 isolates by both methods. MIC agreement and interpretation discrepancies are shown in Table 2. The overall MIC agreement between direct and standard inoculation was 99.2%. Except for piperacillin (95.2%), all individual antimicrobial agents scored as 98.7%. Most minor discrepancies occurred with cefalotin, nitrofurantoin, piperacillin, and cefuroxime. The overall minor error rate was 2.1% (133 of 6,477). Only one major error occurred for E. coli tested against ampicillin, which yielded an overall major error rate of 0.02% (1 of 6,477). Six very major errors occurred, which yielded an overall very major error rate of 0.1% (6 of 6,477). Murray et al. recommend calculating major and very major rates by dividing the number of discrepancies by the number of strains tested as sensitive and resistant, respectively, with the reference method (12, 13). According to this calculation, the major error rate would be 0.02% (1 of 5,508) and the very major error rate would be 0.8% (6 of 748). The very major errors were distributed among two isolates of E. cloacae and two isolates of E. coli and concerned test results associated with piperacillin, cefotaxime, and ceftazidime. Of the 21 polymicrobial samples, 11 (52.4%) identications yielded an unambiguous and conclusive result. For three of these samples, the AST results were reported as inconsistent; for one, they were terminated. Of the other seven samples with a falsely conclusive ID, three were reported with the susceptibility pattern of the most sensitive bacillus. One of these samples contained K. oxytoca and P. aeruginosa; the other two both contained two different phenotypes of E. coli. DISCUSSION In our study we focused on the direct inoculation of blood cultures containing gram-negative bacilli. Because in our experience direct inoculaton of gram-positive cultures yielded unsatisfactory results, we discontinued this after a trial period (data not shown). We used the Vitek 2 standard method as the gold standard for comparing direct and standard ID and AST results of Vitek 2 identiable isolates, since its performance has been compared to reference methods extensively and with good results
Downloaded from jcm.asm.org by Daniel Sordelli on September 1, 2009
RESULTS Of the 410 blood cultures that met the study inclusion criteria, results of direct inoculation of six samples could not be retrieved because of missing or deleted data (n 2), omission of direct testing (n 1),or Vitek 2 malfunction (n 1). Twenty-one samples (5.1%) that appeared to be monomicrobial in the Gram stain yielded more than one isolate in the
VOL. 42, 2004
DIRECT INOCULATION OF VITEK 2 FROM BLOOD CULTURES
TABLE 1. Results of direct inoculation of Vitek 2 ID-GNB card from blood cultures containing monomicrobial gram-negative rods
No. of strains Organism group and namea Tested Correctly identied Low discrimination Not identiedb Misidentied (misidentication)d
Nonfermentersc Acinetobacter spp. Alcaligenes spp. Brevundimonas spp. Flavimonas spp. Ochrobactrum spp. Pseudomonas stutzeri Ralstonia pickettii Stenotrophomonas maltophilia Anaerobic gram-negative rods Bacteroides spp. Fusobacterium spp. Fastidious gram-negative rods Haemophilus inuenzae Streptobacillus moniliformis Gram-positive rods Clostridium spp. Enterobacteriaceae Citrobacter koseri Citrobacter freundii Enterobacter aerogenes Enterobacter cloacae Enterobacter sakazakii Escherichia coli Ewingella americana Klebsiella oxytoca Klebsiella pneumoniae Leclercia adecarboxylata Morganella morganii Pantoea spp. Proteus mirabilis Salmonella spp. Serratia marcescens Pseudomonas aeruginosa Total
a
4 3 1 1 1 1 1 3 14 2 6 1 1 1 3 2 21 1 188 1 13 30 1 4 3 25 7 11 33 383
1 1 1 1 1 1
3 (VNGNB) 2 (VNGNB)
1 14
1 (VNGNB) 1 (VNGNB)
2 (VNGNB)
Downloaded from jcm.asm.org by Daniel Sordelli on September 1, 2009
1 (VNGNB)
1 1 2 2 20 183 13 26 1 3 1 25 6 11 26 321 3 1 1 1 3 1 1 3 16 1 29 3 (VNGNB) 17 1 (Bergeyella zoohelcum)
1 1 1 (Enterobacter cloacae) 1 (VNGNB), 1 (Klebsiella oxytoca)
Names determined by Vitek 2 standard method or API system. b Includes Vitek 2 reports unidentied, inconclusive, and terminated. c Other than Pseudomonas aeruginosa. d VNGNB, various nonfermenting gram-negative bacilli.
(4, 5, 6, 10). In a few instances the API system helped out where the standard ID was inconclusive. Routinely, we inoculate Vitek 2 only with isolates suspected of being Enterobacteriaceae or P. aeruginosa grown in pure culture from agar plates, for which the AES knowledge base contains the data to complete expert analysis of the AST. Although for ID testing Vitek 2 is approved by the Food and Drug Administration for a much larger range of gram-negative rods, in our experience and that of others its performance is best for identifying bacilli belonging to these groups (4, 6, 10). Therefore, direct and standard results of these species only (except Pantoea spp.) were compared; all other gram-negative bacilli were considered not identiable by Vitek 2. Direct inoculation of blood cultures containing gram-negative bacilli indistinguishable from organisms identiable by Vitek 2 in the Gram stain might cause misleading reports.
However, in the present study, none of the isolated anaerobic, fastidious, or gram-positive bacilli or nonfermenters, other than P. aeruginosa, yielded an unambiguous Vitek 2 ID result, except for S. maltophilia, which was correctly identied. With the direct method, 93.0% of Enterobacteriaceae and P. aeruginosa strains together and 94.5% of Enterobacteriaceae strains alone were correctly identied. For selecting a new system for identication, at least 90% overall agreement with a reference system and at least 95% accuracy in identifying commonly isolated organisms such as Enterobacteriaceae are recommended (13). We view our results as more than acceptable, since they are consistent with this and with the percentages determined in studies comparing Vitek 2 (used according to standard protocol) to reference methods (4, 6, 10, 16). The top ve most frequently isolated bacilli (E. coli, P. aeruginosa, K. pneumoniae, P. mirabilis, and E. cloacae) are
10
BRUINS ET AL. TABLE 2. MIC agreement and errors for antimicrobial agents between direct and standard methoda
MIC agreement Antimicrobial agent No. of tests MIC unagreement MIC agreement % MIC agreement Minor
J. CLIN. MICROBIOL.
Error Major Very major
Amikacin Amoxicillin-clavulanic acid Ampicillin Cefalotin Cefepime Cefotaxime Cefoxitin Cefpodoxime Ceftazidime Cefuroxime Cefuroxime axetil Ciprooxacin Gentamicin Meropenem Nitrofurantoin Noroxacin Ooxacin Piperacillin Piperacillin-tazobactam Tobramycin Trimethoprim-sulfamethoxazole Total
a
302 311 312 311 301 310 301 301 311 310 300 311 312 311 312 312 311 312 312 302 312 6,477
0 4 2 3 0 4 0 4 2 4 4 0 3 0 3 2 0 15 3 0 0 53 (0.8)
302 307 310 308 301 306 301 297 309 306 296 311 309 311 309 310 311 297 309 302 312 6,424 (99.2)
100.0 98.7 99.4 99.0 100.0 98.7 100.0 98.7 99.4 98.7 98.7 100.0 99.0 100.0 99.0 99.4 100.0 95.2 99.0 100.0 100.0
1 4 2 15 0 5 4 1 1 17 24 0 2 0 30 5 1 17 3 1 0 133 (2.1)
0 0 1 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 1
0 0 0 0 0 2 0 0 1 0 0 0 0 0 0 0 0 3 0 0 0 6
Downloaded from jcm.asm.org by Daniel Sordelli on September 1, 2009
Values in parentheses are percentages.
similar to those reported from the United States and Canada and from Europe (3, 17). The strains of Enterobacteriaceae or P. aeruginosa misidentied as Bergeyella zoohelcum and various nonfermenting gram-negative bacilli (no expert analysis possible) would be retested from a subculture before being reported. Enterobacter sakazakii identied as E. cloacae would not lead to inappropriate antimicrobial treatment. Probably a too-low inoculum was responsible for the misidentication of E. coli as K. oxytoca. The overall 99.2% MIC agreement between direct and standard susceptibility testing was very high. For every antimicrobial agent the MIC agreement was 90%, as required by the selection criteria for an antimicrobial susceptibility testing system proposed by Jorgensen (9). Overall, error rates were very low (major, 0.02%; very major, 0.8%). A too-low inoculum probably caused very major errors with direct testing of piperacillin, cefotaxime, and ceftazidime for only four isolates. The falsely sensitive results with cefotaxime and ceftazidime for E. cloacae would be of no consequence, since Enterobacter spp. capable of producing an inducible betalactamase would not be treated with any of these drugs. Only 5.1% of the 410 samples inoculated directly into Vitek 2 were found to be polymicrobial when subcultured, which does not differ from other ndings (11, 22). In seven samples there would have been a false report. Their identication and AST results were conclusive and consistent, so the fact that the cultures were not pure would not have been recognized. Of these, only three were reported with too-sensitive AST results, probably because of a lower inoculum or slower growth rate of the more resistant strain in the mixed culture. We found that direct inoculation of Vitek 2 from BACTEC
9240 blood culture bottles to analyze gram-negative bacilli involved in bloodstream infection is safe enough for immediate reporting, provided that ID and AST are conclusive and consistent. Repeat testing by the standard method seems necessary only, if subculturing of the bottle yields isolates suspected of being Enterobacteriaceae or P. aeruginosa and the direct results are inconclusive. Nevertheless, direct inoculation should not be applied when the Gram stain raises any doubt about the purity of the culture.
ACKNOWLEDGMENTS We thank bioMerieux for technical help in retrieving Vitek 2 data and Helen Klip and Teun Groenendijk for help in data analysis.
REFERENCES 1. Barenfanger, J., C. Drake, and G. Kacich. 1999. Clinical and nancial benets of rapid bacterial identication and antimicrobial susceptibility testing. J. Clin. Microbiol. 37:14151418. 2. Doern, G. V., R. Vautour, M. Gaudet, and B. Levy. 1994. Clinical impact of rapid in vitro susceptibility testing and bacterial identication. J. Clin. Microbiol. 32:17571762. 3. Fluit, A. C., M. E. Jones, F.-J. Schmitz, J. Acar, R. Gupta, J. Verhoef, and the SENTRY participants group. 2000. Antimicrobial susceptibility and frequency of occurrence of clinical blood isolates in Europe from the SENTRY antimicrobial surveillance program, 1997 and 1998. Clin. Infect. Dis. 30:454 460. 4. Funke, G., D. Monnet, C. deBernardis, A. von Graevenitz, and J. Freney. 1998. Evaluation of the VITEK 2 system for rapid identication of medically relevant gram-negative rods. J. Clin. Microbiol. 36:19481952. 5. Garcia-Garrote, F., E. Cercenado, and E. Bouza. 2000. Evaluation of a new system, VITEK 2, for identication and antimicrobial susceptibility testing of enterococci. J. Clin. Microbiol. 38:21082111. 6. Gavin, P. J., J. R. Warren, A. A. Obias, S. M. Collins, and L. R. Peterson. 2002. Evaluation of the Vitek 2 system for rapid identication of clinical isolates of gram-negative bacilli and members of the family streptococcaceae. Eur. J. Clin. Microbiol. Infect. Dis. 21:869874. 7. Hansen, D. S., A. G. Jensen, N. Norskov-Lauritsen, R. Skov, and B. Bruun. 2002. Direct identication and susceptibility testing of enteric bacilli from positive blood cultures using VITEK (GNI /GNS-GA). Clin. Microbiol. Infect. 8:3844.
VOL. 42, 2004
DIRECT INOCULATION OF VITEK 2 FROM BLOOD CULTURES
11
8. Howard, W. J., B. J. Buschelman, M. J. Bale, M. A. Pfaller, F. P. Koontz, and R. N. Jones. 1996. Vitek GPS card susceptibility testing accuracy using direct inoculation from BACTEC 9240 blood culture bottles. Diagn. Microbiol. Infect. Dis. 24:109112. 9. Jorgensen, J. H. 1993. Selection criteria for an antimicrobial susceptibility testing system. J. Clin. Microbiol. 31:28412844. 10. Ling, T. K., P. C. Tam, Z. K. Liu, and A. F. Cheng. 2001. Evaluation of VITEK 2 rapid identication and susceptibility testing system against gramnegative clinical isolates. J. Clin. Microbiol. 39:29642966. 11. Moore, D. F., S. S. Hamada, E. Marso, and W. J. Martin. 1981. Rapid identication and antimicrobial susceptibility testing of gram-negative bacilli from blood cultures by the AutoMicrobic system. J. Clin. Microbiol. 13:934 939. 12. Murray, P. R., A. C. Niles, and R. L. Heeren. 1987. Comparison of a highly automated 5-h susceptibility testing system, the Cobas-Bact, with two reference methods: Kirby-Bauer disk diffusion and broth microdilution. J. Clin. Microbiol. 25:23722377. 13. Murray, P. R., E. J. Baron, M. A. Pfaller, F. C. Tenover, and R. H. Yolken (ed.). 1999. Manual of clinical microbiology, 7th ed. American Society for Microbiology, Washington, D.C. 14. National Committee for Clinical Laboratory Standards. 1997. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 4th ed. Approved standard M7-A4. National Committee for Clinical Laboratory Standards, Wayne, Pa. 15. National Committee for Clinical Laboratory Standards. 2002. Performance standards for antimicrobial susceptibility testing. Twelfth informational supplement M100-S12. National Committee for Clinical Laboratory Standards, Wayne, Pa.
16. OHara, C. M., and J. M. Miller. 2003. Evaluation of the Vitek 2 ID-GNB assay for identication of members of the family Enterobacteriaceae and other nonenteric gram-negative bacilli and comparison with the Vitek GNI card. J. Clin. Microbiol. 41:20962101. 17. Pfaller, M. A., R. N. Jones, G. V. Doern, K. Kugler, and the Sentry participants group. 1998. Bacterial pathogens isolated from patients with bloodstream infection: frequencies of occurrence and antimicrobial susceptibility patterns from the SENTRY antimicrobial surveillance program (United States and Canada, 1997). Antimicrob. Agents Chemother. 42:17621770. 18. Putnam, L. R., W. J. Howard, M. A. Pfaller, F. P. Koontz, and R. N. Jones. 1997. Accuracy of the Vitek system for antimicrobial susceptibility testing Enterobacteriaceae bloodstream infection isolates: use of direct inoculation from Bactec 9240 blood culture bottles. Diagn. Microbiol. Infect. Dis. 28: 101104. 19. Sanders, C. C., M. Peyret, E. Smith Moland, S. J. Cavalieri, C. Shubert, K. S. Thomson, J.-M. Boeufgras, and W. E. Sanders, Jr. 2001. Potential impact of the VITEK 2 system and the advanced expert system on the clinical laboratory of a university-based hospital. J. Clin. Microbiol. 39:2379 2385. 20. Stager, C. E., and J. R. Davis. 1992. Automated systems for identication of microorganisms. Clin. Microbiol. Rev. 5:302327. 21. Trenholme, G. M., R. L. Kaplan, P. H. Karakusis, T. Stine, J. Fuhrer, W. Landau, and S. Levin. 1989. Clinical impact of rapid identication and susceptibility testing of bacterial blood culture isolates. J. Clin. Microbiol. 27:13421345. 22. Waites, K. B., E. S. Brookings, S. A. Moser, and B. L. Zimmer. 1998. Direct Susceptibility testing with positive BacT/Alert blood cultures by using MicroScan overnight and rapid panels. J. Clin. Microbiol. 36:20522056.
Downloaded from jcm.asm.org by Daniel Sordelli on September 1, 2009
Vous aimerez peut-être aussi
- Chapter 19Document29 pagesChapter 19Carmela Laraya Alayon100% (3)
- Bi0 310 Bacteria Lab ReportDocument11 pagesBi0 310 Bacteria Lab ReportChiletso PhiriPas encore d'évaluation
- BC 7Document8 pagesBC 7Lucky_megaPas encore d'évaluation
- Bacterial Pellet PreparationDocument5 pagesBacterial Pellet PreparationNitin KalePas encore d'évaluation
- Protocolo Acelerado Desde HemocultivoDocument4 pagesProtocolo Acelerado Desde HemocultivoSharom Zelene Cordova RomanPas encore d'évaluation
- Maldi Vs VitekDocument5 pagesMaldi Vs VitekFrancisca Valenzuela100% (1)
- JTD 06 05 539Document6 pagesJTD 06 05 539gombasgPas encore d'évaluation
- Laboratory Based Evaluation of The ColorimetricDocument8 pagesLaboratory Based Evaluation of The ColorimetricNidia MaradiagaPas encore d'évaluation
- 2 Comparacion BD Phoenix Vitek MicroscanDocument10 pages2 Comparacion BD Phoenix Vitek MicroscanBenjamin MendozaPas encore d'évaluation
- Pneumoniae: Comparison of The Automated Phoenix With The Vitek 2 For The Identification of StreptococcusDocument8 pagesPneumoniae: Comparison of The Automated Phoenix With The Vitek 2 For The Identification of StreptococcusJade BilkeyPas encore d'évaluation
- MainDocument7 pagesMainmalla ashwiniPas encore d'évaluation
- JCDR 9 DC06Document4 pagesJCDR 9 DC06Paula Andrea VillamarinPas encore d'évaluation
- Re 1Document6 pagesRe 1HArdik NegiPas encore d'évaluation
- Methicillin-Resistant Staphylococcus Aureus: Comparison of Susceptibility Testing Methods and Analysis ofDocument6 pagesMethicillin-Resistant Staphylococcus Aureus: Comparison of Susceptibility Testing Methods and Analysis ofNguyễn Đức LongPas encore d'évaluation
- Re 9Document6 pagesRe 9HArdik NegiPas encore d'évaluation
- The Veterinary Journal: Jun Zhang, Gui-Hong Zhang, Lin Yang, Ren Huang, Yu Zhang, Kun Jia, Wen Yuan, Shou-Jun LiDocument4 pagesThe Veterinary Journal: Jun Zhang, Gui-Hong Zhang, Lin Yang, Ren Huang, Yu Zhang, Kun Jia, Wen Yuan, Shou-Jun LiEdgar DíazPas encore d'évaluation
- Performance Verification of Anti-Sars-Cov-2-Specific Antibody Detection by Using Four Chemiluminescence Immunoassay SystemsDocument6 pagesPerformance Verification of Anti-Sars-Cov-2-Specific Antibody Detection by Using Four Chemiluminescence Immunoassay SystemsadnanPas encore d'évaluation
- EUA Roche Elecsys IfuDocument25 pagesEUA Roche Elecsys IfusaidaPas encore d'évaluation
- Clinical Microbiology Newsletter: Genexpert Testing: Applications For Clinical Microbiology, Part IDocument5 pagesClinical Microbiology Newsletter: Genexpert Testing: Applications For Clinical Microbiology, Part ImagicianchemistPas encore d'évaluation
- Ejifcc 27 147Document9 pagesEjifcc 27 147Riski Nur RamadhaniPas encore d'évaluation
- 108820lateral Move Molecular Assay For Horse StranglesDocument3 pages108820lateral Move Molecular Assay For Horse StranglesneriktjpcoPas encore d'évaluation
- Journal of Clinical Microbiology-2021-Higgins-JCM.03149-20.fullDocument20 pagesJournal of Clinical Microbiology-2021-Higgins-JCM.03149-20.fullOmar Cucho GamboaPas encore d'évaluation
- Diagnosis Brucella TurkeyDocument5 pagesDiagnosis Brucella TurkeyJoshua SmithPas encore d'évaluation
- Rapid Isothermal Amplification and Portable Detection System For Sars-Cov-2Document9 pagesRapid Isothermal Amplification and Portable Detection System For Sars-Cov-2peri umardianaPas encore d'évaluation
- Specimen Nasopharyngeal Swab & Throat Swab Sars-Cov-2 Rna Target (S)Document2 pagesSpecimen Nasopharyngeal Swab & Throat Swab Sars-Cov-2 Rna Target (S)manwanimuki12Pas encore d'évaluation
- Clin Microbiology Infect - 2007 - Wilson - The Use of Antibiotic Containing Agars For The Isolation of Extended SpectrumDocument3 pagesClin Microbiology Infect - 2007 - Wilson - The Use of Antibiotic Containing Agars For The Isolation of Extended SpectrumYousra SoumaPas encore d'évaluation
- Antibiogram of Gram Negative Uropathogens in A TerDocument5 pagesAntibiogram of Gram Negative Uropathogens in A TerDumitraPas encore d'évaluation
- Current Technologies in Antimicrobial Susceptibility Testing and Microbial Identification:-Advantages, Limitations/challenges & Future PerspectiveDocument21 pagesCurrent Technologies in Antimicrobial Susceptibility Testing and Microbial Identification:-Advantages, Limitations/challenges & Future Perspectivebonsa dadhiPas encore d'évaluation
- Comparison of The VersaTREK Blood CultureDocument5 pagesComparison of The VersaTREK Blood CulturedatitoxPas encore d'évaluation
- Modern Methods For Identifying Bacteria: Central Science Laboratory, Sand Hutton, York, Y04 L2, UkDocument2 pagesModern Methods For Identifying Bacteria: Central Science Laboratory, Sand Hutton, York, Y04 L2, UkGalana BiratuPas encore d'évaluation
- Germ Tube TestDocument3 pagesGerm Tube TestirnaresaPas encore d'évaluation
- GeneFluidics Announces CE-IVD Marking of UtiMax™ Uropathogen Identification (ID) and Antimicrobial Susceptibility Testing (AST)Document3 pagesGeneFluidics Announces CE-IVD Marking of UtiMax™ Uropathogen Identification (ID) and Antimicrobial Susceptibility Testing (AST)PR.comPas encore d'évaluation
- Journal of Clinical Virology: SciencedirectDocument3 pagesJournal of Clinical Virology: SciencedirectVictor VargasPas encore d'évaluation
- Comparison: of Micro-ID and API 20E Systems For Identification of EnterobacteriaceaeDocument4 pagesComparison: of Micro-ID and API 20E Systems For Identification of EnterobacteriaceaeDede DarmawanPas encore d'évaluation
- HB&L System: Rapid Determination of Antibiotic Sensitivity of Bacteria Isolated From Blood CulturesDocument4 pagesHB&L System: Rapid Determination of Antibiotic Sensitivity of Bacteria Isolated From Blood CulturesmosaabPas encore d'évaluation
- Pooling of Samples For Sars-Cov-2 Detection Using A Rapid Antigen TestDocument5 pagesPooling of Samples For Sars-Cov-2 Detection Using A Rapid Antigen TestErickson OngPas encore d'évaluation
- Specimen Nasopharyngeal Swab & Throat Swab Sars-Cov-2 Rna Target (S)Document2 pagesSpecimen Nasopharyngeal Swab & Throat Swab Sars-Cov-2 Rna Target (S)manwanimuki12Pas encore d'évaluation
- Detection of Vesicular Stomatitis Virus Using A Capacitive ImmunosensorDocument4 pagesDetection of Vesicular Stomatitis Virus Using A Capacitive ImmunosensorAlex WongPas encore d'évaluation
- Journal of Clinical Virology: SciencedirectDocument6 pagesJournal of Clinical Virology: SciencedirectVictor VargasPas encore d'évaluation
- Use of Machine Learning and Artificial Intelligence To P 2020 InternationalDocument8 pagesUse of Machine Learning and Artificial Intelligence To P 2020 Internationaltshikutu bikengelaPas encore d'évaluation
- AbtrascDocument2 pagesAbtrascbebo94Pas encore d'évaluation
- Comparison of Microscan Walkaway System and Vitek System For Identification of Gram-Negative BacteriaDocument3 pagesComparison of Microscan Walkaway System and Vitek System For Identification of Gram-Negative BacteriaPurple basketPas encore d'évaluation
- Ofab 220Document10 pagesOfab 220angel.paternina423Pas encore d'évaluation
- Enterobacter Cloacae in A HighlyDocument4 pagesEnterobacter Cloacae in A HighlyMICHAEL AMARILLO CORREAPas encore d'évaluation
- The Causes of Postoperative Meningitis The Comparison of Gram-Negative and Gram-Positive PathogensDocument8 pagesThe Causes of Postoperative Meningitis The Comparison of Gram-Negative and Gram-Positive PathogensPietroRossidisPas encore d'évaluation
- JCM 43 8 4194-4196 2005Document3 pagesJCM 43 8 4194-4196 2005Sumesh ShresthaPas encore d'évaluation
- Understanding Antigen Tests and Results ENG FinalDocument4 pagesUnderstanding Antigen Tests and Results ENG FinalAna CatarinaPas encore d'évaluation
- Journal of Clinical Microbiology-2020-Theel-JCM.01243-20.fullDocument23 pagesJournal of Clinical Microbiology-2020-Theel-JCM.01243-20.fullRaya KurniawanPas encore d'évaluation
- Microbiology and Immunology - 2010 - Iorio - A Combination of Methods To Evaluate Biofilm Production May Help To DetermineDocument6 pagesMicrobiology and Immunology - 2010 - Iorio - A Combination of Methods To Evaluate Biofilm Production May Help To DetermineAriane Barcellos Dos SantosPas encore d'évaluation
- 4garima EtalDocument7 pages4garima EtaleditorijmrhsPas encore d'évaluation
- 10.33073 - PJM 2022 023Document6 pages10.33073 - PJM 2022 023Andy SetiawanPas encore d'évaluation
- 2011 Pseudomonas AeruginosaDocument4 pages2011 Pseudomonas AeruginosasazunaxPas encore d'évaluation
- Research Proposal-2Document12 pagesResearch Proposal-2Leonardo Andres Pimentel SirittPas encore d'évaluation
- Research On Pathogenic Bacteria and Antibiotic Resistance of Enterobacteriaceae in Hospitalized Elderly PatientsDocument5 pagesResearch On Pathogenic Bacteria and Antibiotic Resistance of Enterobacteriaceae in Hospitalized Elderly PatientsVishwas gargPas encore d'évaluation
- 1 s2.0 S0022030282822455 MainDocument6 pages1 s2.0 S0022030282822455 Maindilipgupta66Pas encore d'évaluation
- Development of A New Protocol For Rapid Bacterial Identification and Susceptibility Testing Directly From Urine SamplesDocument19 pagesDevelopment of A New Protocol For Rapid Bacterial Identification and Susceptibility Testing Directly From Urine SamplesPatricio Suazo SotoPas encore d'évaluation
- Sensitive On-Site Detection of SARS-CoV-2 by ID NOW COVID-19Document12 pagesSensitive On-Site Detection of SARS-CoV-2 by ID NOW COVID-19luis.achaPas encore d'évaluation
- Evaluation of A Manual Identification System For Detection of Mycobacterium Tuberculosis in A Primary Tuberculosis Laboratory in ChinaDocument10 pagesEvaluation of A Manual Identification System For Detection of Mycobacterium Tuberculosis in A Primary Tuberculosis Laboratory in ChinaTonny YuliantoPas encore d'évaluation
- JM 002076Document5 pagesJM 002076Malú CarranzaPas encore d'évaluation
- MEDRXIV 2021 267417v1 SigalDocument9 pagesMEDRXIV 2021 267417v1 Sigalenota15Pas encore d'évaluation
- MEDRXIV 2021 267417v1 SigalDocument9 pagesMEDRXIV 2021 267417v1 SigalAme DPas encore d'évaluation
- VIDAS Emergency PDF Brochure-4Document6 pagesVIDAS Emergency PDF Brochure-4Nidiam2Pas encore d'évaluation
- Newsletter10-1 SebiaDocument4 pagesNewsletter10-1 SebiaNidiam2100% (1)
- Understanding Protein ElectrophoresisDocument14 pagesUnderstanding Protein ElectrophoresisSukma EffendyPas encore d'évaluation
- DYS057 MiniParasepSFDocument4 pagesDYS057 MiniParasepSFpepatorreta5826Pas encore d'évaluation
- CH 11 Lecture PresentationDocument53 pagesCH 11 Lecture PresentationBellezzaPas encore d'évaluation
- Kingdom ArchaebacteriaDocument20 pagesKingdom ArchaebacteriaMarielle Baliwag100% (2)
- Thayer Martin Agar Procedure 08Document1 pageThayer Martin Agar Procedure 08Hadi FirmansyahPas encore d'évaluation
- AnaisDocument272 pagesAnaisJean Gabriel V. Coutinho100% (2)
- Article On Probiotics Nfs 4950Document3 pagesArticle On Probiotics Nfs 4950api-281851020Pas encore d'évaluation
- Kefir and Kombucha Bacteria StrainsDocument2 pagesKefir and Kombucha Bacteria StrainsRobert EdwardsPas encore d'évaluation
- Wound InfectionDocument41 pagesWound Infectionparacetamollyacid100% (2)
- Monera KingdomDocument3 pagesMonera Kingdomtadashii100% (1)
- 152 Experiment 3Document2 pages152 Experiment 3Earl CañoneroPas encore d'évaluation
- Gram StainingDocument2 pagesGram StainingJospes_Pas encore d'évaluation
- Oxoid UTIDocument2 pagesOxoid UTISicoe AdrianPas encore d'évaluation
- Literature ReviewDocument3 pagesLiterature ReviewNurul Nadia Jaafar100% (2)
- Coliform Analysis in Wastewater 2012Document24 pagesColiform Analysis in Wastewater 2012engrbvgPas encore d'évaluation
- For SchoolDocument1 pageFor Schoolapi-252841138Pas encore d'évaluation
- Lab 3 Phage Titration 2014Document6 pagesLab 3 Phage Titration 2014hiteshPas encore d'évaluation
- 1 IntroDocument5 pages1 IntroJeanjayannseptoemanPas encore d'évaluation
- Bomba A Et Al 2002 Probiotics and PUFAsDocument5 pagesBomba A Et Al 2002 Probiotics and PUFAsSandip PatilPas encore d'évaluation
- Bugs and Drugs: A Summary of Pharmaceutical MicrobiologyDocument20 pagesBugs and Drugs: A Summary of Pharmaceutical MicrobiologyaKureishiPas encore d'évaluation
- Microbiology Memorization SheetDocument5 pagesMicrobiology Memorization Sheetalobrien100% (1)
- PlanctomycetesDocument2 pagesPlanctomycetessujithasPas encore d'évaluation
- BSC 1 MicrobiologyDocument4 pagesBSC 1 MicrobiologyRuchiTripathiPas encore d'évaluation
- Binax Product InsertDocument96 pagesBinax Product Insertuber6791Pas encore d'évaluation
- 02 Cell Structure and Function of Prokaryotes (Student)Document37 pages02 Cell Structure and Function of Prokaryotes (Student)Shafira AnandaPas encore d'évaluation
- Staphylococcus AureusDocument3 pagesStaphylococcus AureusDenisse Watt CuarterosPas encore d'évaluation
- Gram Staining Protocol or ProcedureDocument4 pagesGram Staining Protocol or Procedurearavindbt2523Pas encore d'évaluation
- Free Ebook - Microbiology Review Notes by MedpgnotesDocument103 pagesFree Ebook - Microbiology Review Notes by Medpgnotesdr dixit100% (1)
- Protocol For: Gram StainingDocument19 pagesProtocol For: Gram StainingmourighoshPas encore d'évaluation
- Bifidobacterium Agar, Modified: Instructions For Use - Ready-To-Use Plated MediaDocument4 pagesBifidobacterium Agar, Modified: Instructions For Use - Ready-To-Use Plated MediapratechPas encore d'évaluation