Académique Documents
Professionnel Documents
Culture Documents
CHRONIC HEART FAILURE CASE STUDY
Transféré par
Mary Cris CanonDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
CHRONIC HEART FAILURE CASE STUDY
Transféré par
Mary Cris CanonDroits d'auteur :
Formats disponibles
CASE STUDY:
CHRONIC HEART FAlLURE (CHF)
Submitted by: Mary Cris D. Canon BSN 3W1-2 Submitted to: Ms. Catherine Cabrera
I.
INTRODUCTION
HEART FAILURE, the inability of the heart to pump enough blood to meet
the metabolic demands of the body, is the end result of many conditions. Frequently, it is a long - term effect of coronary heart disease and myocardial infarction when left ventricular damage is extensive enough to impair cardiac output. Cardiac output falls, leading to decreased tissue
perfusion. These normal mechanisms may result in vascular congestion and hence, the commonly used term congestive heart failure (CHF). As these mechanisms are exhausted, heart failure ensues, with increased morbidity and mortality. Heart failure, also called congestive heart failure, occurs when cardiac output is inadequate to meet the metabolic demands of the body. The heart rate increase as a Compensatory mechanism to increase cardiac output, and vasoconstriction occurs to try to maintain blood pressure. Eventually, the chronic increase in preload and after load contributes to chamber dilation and hypertrophy, worsening heart failure. Underlying causes of heart failure include congenital heart disease, rheumatic heart disease, endocarditis, myocarditis, and no cardiovascular causes such as, chronic pulmonary disease, various metabolic diseases, Diseases and anemia. Complications of heart failure include pneumonia, pulmonary edema, pulmonary emboli, refractory heart failure, and myocardial failure.
II.
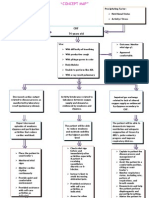
PATHOPHYSIOLOGY
decreased cardiac output decreased systemic BP decreased perfusion to kidneys
Myocardial dysfunction
Ischemic heart disease Hyperthyroidism Myocardial infarction
Valve disease Alcohol, cocaine abuse HPN Activation of baroreceptors Left ventricle Aortic arch
Stimulation of vasomotor regulatory centers in medulla
Activation of sympathetic nervous system
Increased Ca echolamines
Aldosteron
vasoconstriction
Sodium & H2O retention Anginine vasopressin Endothelin Cytokines
Increased after load Increased BP Increased heart rate
VENTRICULAR
PATHOPHYSIOLOGY
REMODELING
Heart Failure, also known as Congestive Heart Failure, is a clinical syndrome that results from the progressive process of remodeling, in which mechanical and biochemical forces alter the size, shape, and function of the ventricles ability to pump enough oxygenated blood to meet the bodys metabolic requirements. Compensatory mechanisms of increased heart rate, vasoconstriction, and hypertrophy eventually fail, leading to the characteristic syndrome of heart failure:
Elevated ventricular or atrial pressures, sodium and water retention, decreased cardiac output, and circulatory and pulmonary congestion. Systolic dysfunction occurs when the left ventricle is unable to relax and fill sufficiently to accommodate enough oxygenated blood returning from the pulmonary circuit. Systolic dysfunction leads to increased vascular resistance and increased after load. Diastolic dysfunction leads to pulmonary vascular congestion.
III.
HISTORY
My patient name is E.V.S, 48 years old, single parent. Birthday is July 24 1963, lives in Malabon City. She is a Filipino citizen and she is Roman Catholic. She is admitted last August 5 2011. This interview was taken Aug 08 2011, and the information was the client herself.
Chief Complaint Nahihirapan ako huminga. As verbalized by the patient as stated. Medical Diagnosis History of Present Illness 4 days prior to consult patient experienced headache and BP of 160/90 mmHg. She just stay rested on her bed until the pain subsides. 1 day prior to consult, patient complained of dizziness and blurring of vision, she decided to seek consultation.
IV.
NURSING PHYSICAL ASSESSMENT
General Appearance Client has medium frame body built. Upright in posture smooth rhythmic gait. She is appropriately dressed. Well groomed and has no body and breath odor. No obvious physical deformity. Weight is 54.5
kgs; Height is 53. Vital signs : Temp: 36.6; BP: 150/100 mmhg ; PR : 63 and RR : 22 HR : 51 Eyes: Eye condition is straight normal, has thick eyebrows, has effective closure of the eyelids with no fallen lashes. Bilateral and frequent blink response. The eyeballs are symmetrical and firm. Conjunctiva is clear and bulbar is clear while palpebral is pink in color. Sclera is white. Lacrimal apparatus is moist. Patient experienced blurring of vision. Ears: The auricle is in normal racial tone, symmetrical and non tender. Pinna recoils when folded. External canal has some cerumen. Patient was able to respond to normal voice and also to whispered voice. Nose: External nose is in normal racial tone. Non flaring and septum is at midline. Mucosa is pink, both nares are potent. Nasal cavity is moist and sinuses are non tender. Mouth: Lips are slightly dry and symmetrical. Mucosa is pink. Tongue is in midline, rough, pink and is movable. Teeth are complete and gums are pink and non tender. Pharynx: Uvula is in midline, mucosa is pink and tonsils are not inflamed as well as the posterior pharynx and gag reflex is present. Upper Extremities: Motor strength is 4/5. Good muscle tone. No lesions and deformities. Peripheral pulses are normal and lymph nodes are not palpable. Lower Extremities: Motor strength is 3/5 no lesions and deformities noted. Peripheral pulses are normal and lymph nodes are not palpable.
Genitalia: Patient refuses to asses her genitals. Pubic hair is present without any lesions and any diseases.
V.
RELATED TREATMENT
Administer medication and assess the patients response to pharmacologic regimen. Assess fluid intake, including intake and output -optimize volume status. Weigh pt. daily at the same time and on the same scale after urination Auscultate lung sounds to detect an increase or decrease in pulmonary crackles. Determine the degree of jugular venous distention. Identify and evaluate the severity of dependent edema. Monitor PR and BP. Checking for postural hypotension due to dehydration. Examine skin turgor and mucous membrane for signs and symptoms of fluid overload.
VI.
NCP
DIAGNOOSIS PLANNING INNTERVENTION EVALUATION
Nursing Care Plan # 1
ASSESSMENT
Subjective: Nahihirapan ako huminga. As verbalized by the patient. Decreased cardiac output related to altered contractility of Pre load and After load. Short term goal: 15 mins. After nursing intervention, the client will be able to have a patent airway. Long term goal: After 4 hours of nursing intervention, the patient heart will pump effectively. INDEPENDENT: Position client semi- fowlers position. Advice client to Increase water intake Advice client to Decrease sodium intake Weigh client daily Assess edema. Check and Auscultate for crackles. Monitor vs. Short term goal: ACHIEVED 15 mins. After nursing intervention, the client was able to have a patent airway. Long term goal: ACHIEVED After 4 hours of nursing intervention, the patient heart was able to pump effectively.
Objective: Peripheral edema (+2) Wt. gain of 1kg/week Dyspnea Cough Oliguria RR: 45 cpm Wheezes orthopnea
collaborative: Administer oxygen as prescribed. Administer medication that reduces after load.
Nursing Care Plan # 2
ASSESSMENT SUBJECTIVE: Namumutla na ako as verbalize by The client. OBJECTIVE: Cool, ashen Skin. Orthopnea Crackles V/S taken as Follows: T: 36.2 C PR: 130 bpm RR: 45 cpm Bp: 90/70 mmHg
DIAGNOOSIS Decreased cardiac output related to altered myocardial contractility /isotropic Changes.
PLANNING Short term goal : 30 mins. After nursing intervention the client will be able to normalize her vital signs.
INNTERVENTION INDEPENDENT: Auscultate apical pulse; assess heart rate, and Rhythm. Inspect skin for pallor, Cyanosis. Monitor urine output, noting decreasing output and dark or concentrated urine Note changes in Sensory. Provide quiet Environment. Collaborative: Administer supplemental oxygen As indicated. Administer diuretics as Prescribed.
EVALUATION Short term : ACHIEVED 30 mins. After nursing intervention the client was able to normalize her vital signs.
Long term goal: After 8 hours of nursing intervention the patient will display vital signs within acceptable limits, dysrhythmias controlled and no symptoms of Failure.
Long term: ACHIEVED After 8 hours of nursing intervention the patient was able to display vital signs within acceptable limits, dysrhythmias controlled and no symptoms of Failure.
Nursing Care Plan # 3
ASSESSMENT Subjective: Nahihirapan ako kumilos, nanghihina ang katawan ko. As verbalized by the patient.
DIAGNOOSIS Activity intolerance and fatigue related to imbalance between oxygen supply and demand because of decreased cardiac output.
PLANNING Short term goal: 1 hour after nursing intervention the client will be able to perform light activity with minimal assistance.
INNTERVENTION INDEPENDENT: Assist the client while performing daily activity Increase potassium intake, by eating foods rich in potassium (banana). Position client semifowlers position. Advice client to Increase water intake Monitor vs. Ensure safety and security of the client.
EVALUATION Short term goal: ACHIEVED 1 hour after nursing intervention the client verbalized that she can perform light activity with minimal assistance.
Objective: Fatigue Feeling of heaviness of arms and legs Dyspnea Chest pain RR : 45 cpm
Long term goal: After 5 hours of nursing intervention the client will be able to perform activity of daily living.
Long term goal: ACHIEVED After 5 hours of nursing intervention the client verbalized that she was able to perform activity of daily living.
COLLABORATIVE: Administer supplemental oxygen As indicated.
VII.
NURSING DIAGNOSIS AND PATIENT GOAL
DIAGNOSIS GOAL
Nahihirapan ako huminga. As verbalized by the patient.
Short term goal: 15 mins. After nursing intervention, the client will be able to have a patent airway. Long term goal: After 4 hours of nursing intervention, the patient heart will pump effectively.
Namumutla na ako as verbalize by The client
Short term goal : 30 mins. After nursing intervention the client will be able to normalize her vital signs.
Long term goal: After 8 hours of nursing intervention the patient will display vital signs within acceptable limits, Dysrhythmias controlled and no symptoms of Failure.
Nahihirapan ako kumilos, nanghihina ang katawan ko. As verbalized by the patient.
Short term goal: 1 hour after nursing intervention the client will be able to perform light activity with minimal assistance.
Long term goal: After 5 hours of nursing intervention the client will be able to perform activity of daily living.
VIII. NURSING MANAGEMENT
1. Monitor for signs of respiratory distressI a. Provide pulmonary hygiene as needed b. Administer oxygen as prescribed c. Keep the head of the bed elevated d. Monitor ABG values. 2. Monitor for signs of altered cardiac output, including a. Pulmonary edema
3.
4.
5. 6.
b. Arrhythmias, including extreme tachycardia and bradycardia c. Characteristic ECG and heart sound changes Evaluate fluid status a. Maintain strict fluid intake and output measurements b. Monitor daily weights c. Assess for edema and severe diaphoresis d. Monitor electrolyte values and hematocrit level e. Maintain strict fluid restrictions as prescribed Administer prescribed medications which may include: a. Antiarrhythmias to increase cardiac performance b. Diuretics, to reduce venous and systemic congestion c. Iron and folic acid supplements to improve nutritional status. Prevent Infection Reduce cardiac demands a. Keep the child warm b. Schedule nursing interventions to allow for rest c. Do not allow an infant to feed for more than 45 minutes at a time d. Provide gavages feedings if the infant becomes fatigued before ingesting an adequate amount 7. Promote adequate nutrition. Maintain a high-calorie, low-sodium as prescribed. 8. Promote optimal growth and development 9. As appropriate, refer the family to a community health nurse for follow up care after discharge.
0 IX. EVALUATION
Vous aimerez peut-être aussi
- NCP-Case Presentation (CHF)Document4 pagesNCP-Case Presentation (CHF)Jessamine EnriquezPas encore d'évaluation
- Congestive Heart Failure PathophysiologyDocument16 pagesCongestive Heart Failure PathophysiologyDale LaurentePas encore d'évaluation
- ARDSDocument57 pagesARDSnesjohnvPas encore d'évaluation
- HCVDDocument5 pagesHCVDkhrizaleehPas encore d'évaluation
- Ineffective Cerebral Tissue Perfusion Related ToDocument7 pagesIneffective Cerebral Tissue Perfusion Related TohannahPas encore d'évaluation
- Risk For Fluid ImbalanceDocument8 pagesRisk For Fluid Imbalanceapi-277522722100% (1)
- Cva NCPDocument1 pageCva NCPxiang jinPas encore d'évaluation
- Nursing Care Plan HF FinalDocument10 pagesNursing Care Plan HF FinalCristina L. JaysonPas encore d'évaluation
- Pathophysiolgoy Coronary Artery DiseaseDocument3 pagesPathophysiolgoy Coronary Artery DiseaseNursesLabs.comPas encore d'évaluation
- Risk For Bleeding - Cirrhosis NCPDocument2 pagesRisk For Bleeding - Cirrhosis NCPPaula AbadPas encore d'évaluation
- NCP Fluid Volume DeficitDocument3 pagesNCP Fluid Volume DeficitNecheal BaayPas encore d'évaluation
- Hypokalemia NCP PDFDocument4 pagesHypokalemia NCP PDFMussaib MushtaqPas encore d'évaluation
- Chronic Renal FailureDocument28 pagesChronic Renal FailurePatricia Nadine Sarcadio NeffePas encore d'évaluation
- Acs Nstemi Vs Ua - PathoDocument2 pagesAcs Nstemi Vs Ua - PathoJerom YamatPas encore d'évaluation
- PathophysiologyDocument2 pagesPathophysiologyKarla Karina Dela CruzPas encore d'évaluation
- NCP CHFDocument2 pagesNCP CHFaldrin1920Pas encore d'évaluation
- Drugs in CHFDocument48 pagesDrugs in CHFBishnu BhandariPas encore d'évaluation
- Massive AscitesDocument12 pagesMassive Ascitesranitidin100% (1)
- Nursing Care Plan For Pulmonary Edema PDFDocument2 pagesNursing Care Plan For Pulmonary Edema PDFAsmaa100% (1)
- CHF Case Study (Document35 pagesCHF Case Study (EzraManzanoPas encore d'évaluation
- Nursing Care Plan Renal FailureDocument11 pagesNursing Care Plan Renal Failurenosevad88850% (2)
- NCP Ineffective Cardiopulmonary PerfusionDocument3 pagesNCP Ineffective Cardiopulmonary PerfusionjamiemapanaoPas encore d'évaluation
- NSTEMI Case PresentationDocument24 pagesNSTEMI Case PresentationMHIEMHOIPas encore d'évaluation
- Pulmonary EmbolismDocument8 pagesPulmonary EmbolismspoilttbrattPas encore d'évaluation
- Decreased Cardiac OutputDocument1 pageDecreased Cardiac OutputPrecious Heart Sotero TababaPas encore d'évaluation
- What Is Stroke?: BY: Luis Alberto Sanchez Hernandez Physical TherapistDocument12 pagesWhat Is Stroke?: BY: Luis Alberto Sanchez Hernandez Physical TherapistLidiaAMonroyRPas encore d'évaluation
- Pathophysiology of COPD - The BasicsDocument11 pagesPathophysiology of COPD - The BasicstiaranindyPas encore d'évaluation
- Nursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisDocument19 pagesNursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisRiza Angela BarazanPas encore d'évaluation
- CAP and Hypertension: Predisposing and Precipitating FactorsDocument5 pagesCAP and Hypertension: Predisposing and Precipitating FactorsLeonaPunzalanPas encore d'évaluation
- Two Mechanisms of Hypertensive NephrosclerosisDocument2 pagesTwo Mechanisms of Hypertensive NephrosclerosisJessica Damasen Caballero0% (1)
- Hypertension Pathophysiology and Treatment PDFDocument6 pagesHypertension Pathophysiology and Treatment PDFBella TogasPas encore d'évaluation
- Dilated Cardiomyopathy Case StudyDocument29 pagesDilated Cardiomyopathy Case Studydvalitz100% (2)
- Angina Pectoris PathophysiologyDocument2 pagesAngina Pectoris PathophysiologyALIANA KIMBERLY MALQUESTOPas encore d'évaluation
- Asthma Nanda Diagnoses Goals InterventionsDocument4 pagesAsthma Nanda Diagnoses Goals InterventionsZinya RobinsonPas encore d'évaluation
- NCP - Poststreptococcal GlomerulonephritisDocument12 pagesNCP - Poststreptococcal GlomerulonephritisAya BolinasPas encore d'évaluation
- Assessing and reassuring an elderly postoperative patientDocument1 pageAssessing and reassuring an elderly postoperative patientNestor CabacunganPas encore d'évaluation
- Decrease Cardiac OutputDocument6 pagesDecrease Cardiac OutputGerardeanne ReposarPas encore d'évaluation
- Pneumo HemothoraxDocument126 pagesPneumo HemothoraxLyra Jan Roo100% (1)
- General ObjectivesDocument1 pageGeneral ObjectivesErwin DegraciaPas encore d'évaluation
- ThiazideDocument4 pagesThiazideEkarthi KeyanPas encore d'évaluation
- Actual NCPDocument3 pagesActual NCPMabz BoholPas encore d'évaluation
- Final Major Case StudyDocument17 pagesFinal Major Case Studyapi-546876878Pas encore d'évaluation
- Hypothyroidism Case AnalysisDocument3 pagesHypothyroidism Case AnalysisKrisianne Mae Lorenzo FranciscoPas encore d'évaluation
- Pathophysiology of HyperthyroidismDocument4 pagesPathophysiology of HyperthyroidismKitty YuffiePas encore d'évaluation
- Hypertensive Cardiovascular Disease Also Known As Hypertensive Heart Disease Occurs Due To The Complication of Hypertension or High Blood PressureDocument3 pagesHypertensive Cardiovascular Disease Also Known As Hypertensive Heart Disease Occurs Due To The Complication of Hypertension or High Blood Pressurejoanneceline16Pas encore d'évaluation
- Anxiety R:T Death ThreatDocument8 pagesAnxiety R:T Death ThreatAlfredo BaulaPas encore d'évaluation
- Anatomy and Physiology PneumoniaDocument4 pagesAnatomy and Physiology PneumoniaJohnson MallibagoPas encore d'évaluation
- ISBAR DocumentationDocument1 pageISBAR DocumentationFrancorussPas encore d'évaluation
- Case Study in KidneyDocument3 pagesCase Study in KidneyVenice VelascoPas encore d'évaluation
- Cardiac Case Study NDDocument11 pagesCardiac Case Study NDapi-313165458Pas encore d'évaluation
- Discharge Planning PaperDocument5 pagesDischarge Planning Paperapi-283173905Pas encore d'évaluation
- Nursing Care Plan For Myocardial InfarctionDocument1 pageNursing Care Plan For Myocardial InfarctionIshaBrijeshSharmaPas encore d'évaluation
- Case Study ReportDocument23 pagesCase Study Reportapi-290866384Pas encore d'évaluation
- Multiple Physical Injuries Secondary To Vehicular AccidentDocument31 pagesMultiple Physical Injuries Secondary To Vehicular AccidentJane Arian BerzabalPas encore d'évaluation
- Concept Map - Abby !Document2 pagesConcept Map - Abby !Abegail Abaygar100% (3)
- PathophysiologyDocument4 pagesPathophysiologyAngelou Joefred Congreso100% (1)
- Myocardial Infarction Concept MapDocument7 pagesMyocardial Infarction Concept Mapkarelclarke629280% (5)
- Hypertensive Cardiovascular DiseaseDocument16 pagesHypertensive Cardiovascular DiseaseTintin Ponciano100% (1)
- Hypovolemic Shock Nursing Care Management and Study GuideDocument1 pageHypovolemic Shock Nursing Care Management and Study GuideRoselyn VelascoPas encore d'évaluation
- NURSING CARE PLAN for 8yo Male with CHDDocument5 pagesNURSING CARE PLAN for 8yo Male with CHDDonna Co IgPas encore d'évaluation
- NICU 2021clinical Reference Manual For Advanced Neonatal Care FINALDocument254 pagesNICU 2021clinical Reference Manual For Advanced Neonatal Care FINALTewodros Demeke100% (7)
- BioconDocument16 pagesBiocongirishchanduPas encore d'évaluation
- Language For Understanding COVID-19Document8 pagesLanguage For Understanding COVID-19Rohani YusofPas encore d'évaluation
- CKHA 2013 Salary DisclosureDocument2 pagesCKHA 2013 Salary DisclosureChatham VoicePas encore d'évaluation
- Cordia Viral MeningitisDocument7 pagesCordia Viral MeningitisAyuagung Chandra Maha DewiPas encore d'évaluation
- Diuretics: Dr. Sadat MemonDocument28 pagesDiuretics: Dr. Sadat MemonCham PianoPas encore d'évaluation
- Physical Examination by DRDocument25 pagesPhysical Examination by DRapi-3739910100% (2)
- Back Pain Symptoms, Causes and Treatment OptionsDocument4 pagesBack Pain Symptoms, Causes and Treatment OptionsPotchie PFIZERPas encore d'évaluation
- Radiology 101Document2 pagesRadiology 101Nadhirah AnandaPas encore d'évaluation
- Romovac DrainDocument3 pagesRomovac DrainKanchhi MaharjanPas encore d'évaluation
- TURPDocument55 pagesTURPJulfikar KhanPas encore d'évaluation
- Activated Charcoal OverviewDocument3 pagesActivated Charcoal OverviewCarlos Laureano Martinez FloresPas encore d'évaluation
- College of Nursing: Short Term: IndependentDocument3 pagesCollege of Nursing: Short Term: IndependentJames Matthew MacanlalayPas encore d'évaluation
- Oral Squamous Cell Carcinoma (OSCC)Document37 pagesOral Squamous Cell Carcinoma (OSCC)Yusra Shaukat100% (1)
- The Acupuncture Point Book 151 200Document50 pagesThe Acupuncture Point Book 151 200mamun31100% (1)
- Perioperative Medicines Management V8Document7 pagesPerioperative Medicines Management V8Waleed Ahmad.Pas encore d'évaluation
- Investigative DHHS Report - Horizon Health and RehabDocument29 pagesInvestigative DHHS Report - Horizon Health and RehabLas Vegas Review-JournalPas encore d'évaluation
- Sitel Medical PagesDocument68 pagesSitel Medical PagesswiftsilentPas encore d'évaluation
- CMS Medicine 4 (Q&A)Document59 pagesCMS Medicine 4 (Q&A)M. Baidar SaeedPas encore d'évaluation
- HBP C315HIS Implant Procedure-eLearnDocument35 pagesHBP C315HIS Implant Procedure-eLearnRichiPas encore d'évaluation
- Clsi GP20 A2Document44 pagesClsi GP20 A2Cristian Gutiérrez VeraPas encore d'évaluation
- NCP Acute PainDocument3 pagesNCP Acute PainjrilleraPas encore d'évaluation
- Bates' Visual Guide To Physical Examination OSCE 3: Sore ThroatDocument6 pagesBates' Visual Guide To Physical Examination OSCE 3: Sore ThroatghPas encore d'évaluation
- Test Report: Naso and Oropharyngeal SwabDocument2 pagesTest Report: Naso and Oropharyngeal SwabSanjay ThakkarPas encore d'évaluation
- Non-Motor Symptom Assessment Scale For Parkinson's Disease (NMSS)Document2 pagesNon-Motor Symptom Assessment Scale For Parkinson's Disease (NMSS)ganpur01Pas encore d'évaluation
- Mucopyocele of The Maxillary Sinus A Case StudyDocument3 pagesMucopyocele of The Maxillary Sinus A Case StudyInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- What Is Post-Acute Withdrawal Syndrome (PAWS) ?Document2 pagesWhat Is Post-Acute Withdrawal Syndrome (PAWS) ?DeAn WhitePas encore d'évaluation
- M1 Intro To Disease IntroDocument35 pagesM1 Intro To Disease IntrorealforgivePas encore d'évaluation
- Renting Homes and Visiting Doctors in EnglandDocument5 pagesRenting Homes and Visiting Doctors in EnglandDheaaPas encore d'évaluation
- CSPD Presentation On The Northgate Entertainment DistrictDocument18 pagesCSPD Presentation On The Northgate Entertainment DistrictKBTXPas encore d'évaluation