Académique Documents
Professionnel Documents
Culture Documents
Cornell Clinpath
Transféré par
chockulaDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Cornell Clinpath
Transféré par
chockulaDroits d'auteur :
Formats disponibles
Hemoglobin Hemoglobin concentration (Hb) is reported as grams of hemoglobin per deciliter of blood (g/dL).
Since red cells are approximately 33% hemoglobin, the hemoglobin concentration of whole blood normally is about one third of the HCT (i.e., the MCHC is 33%). Mean Cell Volume (MCV) The mean cell volume indicates the volume of the "average" red cell in a sample. It is expressed in femtoliters (fl; 10-15 liters). Traditionally, MCV was a calculated parameter, derived by using the following formula: MCV = (PCV x 10) RBC Red cell populations with the MCV above the reference interval are termed macrocytic. Conversely, red cell populations with the MCV below the reference interval are termed microcytic. Mean Cell Hemoglobin MHC is the mean cell hemoglobin. This represents the absolute amount of hemoglobin in the average red cell in a sample. Its units are picograms (pg) per cell. The MCH is calculated from the [Hb] and the RBC using the following equation: MCH (pg) = (Hb x 10) RBC
Mean Cell Hemoglobin Concentration (MCHC) MCHC is the mean cell hemoglobin concentration, expressed in g/dL. It can be calculated from the [Hb] and the PCV using the following formula: MCHC = (Hb PCV) x 100 The normal value for MCHC is about 33%. Red cell populations with values below the reference interval can be termed "hypochromic". This can occur in a strongly regenerative anemia, where an increased population of reticulocytes with low Hb content "pull" the average value down (an increased MCV would be expected under this scenario). Low MCHC can also occur in iron deficiency anemia, where microcytic, hypochromic red cells are produced as a result of the lack of iron to support hemoglobin synthesis. Values for MCHC significantly above the reference interval are not physiologically possible due to limitations on the solubility of Hb. Sample-related problems of analysis, however, can result in spurious high values. Lipemia or other causes of turbidity in the lysate can cause falsely high [Hb] values, which raises the apparent MCHC.
Reticulocytes Reticulocytes ("retics") are young, anucleate erythrocytes, which are released from bone marrow into the blood in increased numbers as a response to anemia caused by hemolysis (destruction) or loss (hemorrhage) of erythrocytes in most species (horses are a notable exception - see more below). Identification of immature anucleate red blood cells allows us to determine if the bone marrow is responding to an anemia (given sufficient time) by increasing red blood cell production. This is termed a regenerative response. The bone marrow response is evaluated by detecting immature erythrocytes by virtue of the presence of RNA in the form of ribosomes and rough endoplasmic reticulum in their cytoplasm. The more immature the cell, the more RNA it contains. In contrast, mature red blood cells, which are no longer synthesizing hemoglobin, contain very small amounts or no RNA (they are essentially small sacs of hemoglobin).
The RNA can be detected in immature red blood cells in several ways: With a supravital dye, such as new methylene blue: When immature red blood cells are stained with a supravital dye, the cytoplasmic RNA is precipitated into a reticulum-like network. Thus the term, reticulocyte, was coined. With these dyes, two types of reticulocytes are seen - those with big aggregates of RNA, which are also called aggregate reticulocytes and those with small dots of RNA, which are called punctate reticulocytes(see image to the right). Since cells with more RNA are younger, aggregate reticulocytes are more immature than punctate reticulocytes. In most species, this does not matter because both types of reticulocytes have similar half lives in the circulation, but in cats, aggregate reticulocytes only persist for 12-24 hours before they mature into In a Wright's-stained blood smear of a regenerative anemia in a cat (top image), the larger purple cell (P) is a punctate reticulocytes. Punctate reticulocytes can persist for several days polychromatophil which corresponds to an aggregate reticulocyte (A) in the new methylene blue-stained smear (7-10 days usually) in this species. Since (bottom image). In contrast, the larger red cell is a punctate reticulocytes last for a while in macrocyte (M) that corresponds to a punctate the circulation of cats, we only count reticulocyte (PR). aggregate reticulocytes when assessing whether the bone marrow is currently responding to an anemia in this species. Standard hematogy stains: Depending on their RNA content, reticulocytes can be detected with routine polychrome stains (eg, Wright's, DiffQuik) used for staining blood smears. RNA (or DNA) stains blue with these dyes, whereas hemoglobin stains red. When the immature red blood cells contain large amounts of RNA, the blue mixes with the hemoglobin to yield a purple color and the cells are termed polychromatophilic red blood cells. These polychromatophils correspond to aggregate reticulocytes. Thus, we can examine a blood smear for the presence of polychromasia to assess if the marrow is responding to an anemia in most species, other than the horse. Indeed, the proportion of polychromatophils can be used as a rough guide to estimate the reticulocyte count. In contrast to aggregate reticulocytes, punctate reticulocytes will stain red and not purple because they only contain small amounts of RNA (the hemoglobin dominates). Therefore, they are a lot harder to identify on a regular blood smear. Punctate reticulocytes can be larger than normal (until they are remodeled by splenic macrophages as they recirculate), i.e. they can be macrocytes, and may be detected on routine blood smears by their larger size. Unfortunately, there are other causes of large red blood cells so not all macrocytes are punctate reticulocytes and we do not rely on these cells to evaluate the regenerative response in most species (the horse is an exception). Total Protein by Refractometry
The protein value reported on the routine CBC is only an estimate, based on the refractive index of the plasma. Three important points need to be made regarding this procedure. 1. Since it is determined using EDTA plasma (which contains fibrinogen), this value usually will be higher than the total protein on a chemistry panel (which is performed on serum). 2. The use of refractometry is valid for providing an estimate of plasma protein concentration, since protein is the major determinant of refractive index of plasma. It is not, however, the only contributor. All other dissolved solids (glucose, urea, cholesterol, etc) also make a contribution. In using a refractometer to "measure" protein, one is assuming that all nonprotein solids are identical from one sample to the next. This is a big assumption, and it is not always correct. The estimate of protein based on refractometry will be significantly biased in patients with marked deviations from normal concentration of non-protein solids in blood. 3. For valid results, the plasma sample must be optically clear. Lipemic blood (or chylous pleural fluid), for example, will yield erroneously high results. In hemolyzed samples, the line can be difficult to read. In these cases, the total protein by refractometer result may be cancelled.
Blood Smear Examination Examination of a blood smear is an integral part of a hemogram. Blood smear analysis allows quantitation of the different types of leukocytes (called the differential count), estimation of the platelet count, and detection of morphologic abnormalities that may
be indicators of pathophysiologic processes. In some instances, a diagnosis may be evident. Deriving full value from blood smear examination requires a well-prepared, well-stained blood smear and some basic skills in the methods of assessment. This short movie clip demonstrates the proper technique for making a good quality blood smear. Though some automated hematology analyzers provide a differential count as part of their ouput, this does not fully take the place of a microscopic exam by an experienced observer. A systematic approach is important so that all the available information is derived from each smear examined. Follow this protocol: 1. Scan the smear at low magnification (10x objective) to locate the optimal area for examination at higher magnification, and check the feathered edge to evaluate the distribution of leukocytes on the smear 2. Perform the differential count (100x objective) 3. Assess platelet numbers (100x objective) 4. Perform a morphologic assessment of blood cells (100x objective) Distribution of cells A second goal of scanning is to check that leukocytes are uniformly distributed throughout the smear and not excessively concentrated at the feather edge. In some ill-made smears, most of the leukocytes are dragged to the end of the smear. If this is found to be the case, prepare another smear and move the spreader slide more quickly, which should ensure that white cells are adequately distributed.
Low magnification (100x) view of the feathered edge. Such poor distribution of leukocytes adversely affects the accuracy of the differential count.
Blood cell morphology To complete the blood smear analysis, assess the different types of blood cells for significant morphologic abnormalities and describe your findings. This part of the hemogram is the most subjective and difficult to quantitate, although
there are published guidelines for grading morphologic abnormalities (Vet Clin Path 13:27-31, 1984). If abnormalities are found, these should be modified with adjectives such as slight, few, moderate, many or marked. For example, if there is a slightly increased number of polychromatophilic red cells in the smear, this should be reported as slight polychromasia. Normal blood cells and some common leukocyte abnormalities are shown later in this module, but a detailed discourse on red cell shape changes is beyond the scope of this laboratory session. Proficiency in recognizing and interpreting morphologic abnormalities comes only with practice and familiarity with normal features of each species. An important preliminary to gaining such expertise is knowledge of the common artifacts of preparation that affect blood smears: [ Crenation ] [ Water artifact ] [ Stain precipitate ] [ Smudged cells ]
Introduction to Hemostasis
Normal hemostasis is dependent upon the complex interaction of plasma coagulation and
fibrinolytic proteins, platelets, and the blood vasculature. Hemostasis can be divided into three categories, which makes this complex process easier to understand. In addition, each of these categories usually produce different clinical signs, which can aid in narrowing down a differential diagnostic list in a bleeding animal. For example, a defect in primary hemostasis should be considered first in a dog presenting with epistaxis (as shown in the image on the right), whereas a defect in secondary hemostasis is likely in a dog with hemarthrosis. However, it must be realized that all three processes occur simultaneously and not sequentially in vivo. The 3 categories are: Primary hemostasis: This is defined as the formation of the platelet plug. Secondary hemostasis: This is defined as the formation of fibrin through the coagulation cascade. Tertiary hemostasis: This is defined as the formation of plasmin for breakdown of the clot. Inhibitors are important as they serve to limit hemostasis to the site of vessel injury and prevent over-production of the clot, which could lead to pathological thrombosis.
Tests for Hemostasis
The most important aspect of diagnosis of hemostatic disorders is the collection and submission of an optimal sample for testing. Unlike many other clinical pathologic tests, coagulation assays are unforgiving with respect to poor sample collection and handling. Many causes of prolonged clotting times or decreased factor concentrations are artifactual, due to poor sample collection and
handling. To obtain the best information from coagulation samples, the following procedures should be adhered to when collecting samples for any coagulation assays: The preferred anticoagulant for coagulation asssays is trisodium citrate (blue-top vacutainer tube). Clean venipuncture is essential. Poor venipuncture will result in activation of coagulation due to contamination with tissue factor. This means that large peripheral veins are optimal sites for obtaining coagulation samples (to ensure rapid blood flow) and if the vein is not entered on the first attempt, a fresh needle should be used. The sample should be mixed with anticoagulant rapidly to prevent clotting occurring within the tube. Therefore, vacutainer collection is preferred, although in some instances vacutainers can underfill. The tube should be filled properly (to the blue line) since the amount of citrate anticoagulant in the tube is calculated to give a final volume of 1 part citrate to 9 parts blood. Grossly underfilling the tube can alter the test results (usually by prolonging the coagulation times). This means that if the needle comes out of the vein during sample collection, you need to start from scratch (new needle, new collection tube). The hematocrit of the patient should be considered. Severe hemoconcentration or polycythemia can result in overcitration of the plasma, which will artifactually prolong clotting times (especially the APTT). The converse is true in anemic animals, in which a sample may clot due to undercitration. In very severely anemic (PCV < 15%) or polycythemic (PCV > 65%) animals, the amount of citrate should be adjusted using the following formula: Volume of citrate = 0.00185 x blood volume to be collected x (100 - Hct [%]) Coagulation factors are notoriously unstable. Samples should be submitted as soon as possible after collection. As most of us do not have access to a clinical laboratory laboratory on site, this usually means shipping the sample. It is far better to ship a sample to a veterinary diagnostic laboratory, then to run the sample up to the local hospital, because (as mentioned previously) not all coagulation instruments and reagents are created equal. For shipping, the sample should be centrifuged as soon as possible after collection and the plasma removed from the cells (keep the sample refrigerated until centrifugation). The plasma can then be stored refrigerated and shipped (with a cool pack) to reach the laboratory within 24 hours of collection. However, if the delay before submission is longer than that (the usual situation), the sample should be frozen and kept frozen until it reaches the laboratory (shipped on dry ice). A sample from a healthy animal of the same species could be collected, handled, and sent with the patient's plasma to serve as a control for artifacts induced by sample handling, especially when using a non-veterinary laboratory or species-specific reference ranges are not provided by the laboratory.
Activated coagulation time
The ACT is a useful screen for evaluation of the intrinsic and common pathways. Whole blood without anticoagulant is added to a special tube containing diatomaceous earth as a contact activator, and the tube is gently agitated at specific intervals until a clot is detectable. The ACT tube can be purchased from suppliers of Becton-Dickson products and is shown on the right. To minimize variability in test results due to temperature, the tube should be kept at 37 C in a heating block (although the armpit can serve as the heating block). The ACT relies on the patient's platelets for provision of phospholipid to support the reaction. The ACT is an insensitive test (sensitive to single factor deficiencies of <10%) compared to the APTT (sensitive to deficiencies of < 30%), but it is sufficient to demonstrate severe clotting factor deficiencies, whether inherited or acquired. Animals with the most common causes of acquired clotting factor deficiencies (namely anticoagulant rodenticide poisoning) will have prolonged ACT. Normal ACT for dogs is 60 - 90 seconds and for cats is 45 - 160 seconds. Due to reliance on endogenous platelets for the reaction, platelet counts of < 10,000/l may result in a mildly prolonged ACT (by 10-20 seconds).
Tests for fibrinogen
Fibrinogen concentration can be measured in 3 ways. Fibrinogen concentration is usually reported in milligrams per deciliter (mg/dl). Heat precipitation: This test is performed on EDTA samples only and is used for determination of fibrinogen concentration as an indicator of inflammation in large animals. Fibrinogen is an acute phase reactant protein and elevated values are seen in inflammation and renal disease (for the latter, in the cat and cow especially). This method of fibrinogen determination is not sensitive enough to detect decreased fibrinogen concentration in coagulation abnormalities. The method is as follows: Two microhematocrit tubes are filled with EDTA-anticoagulated blood. One is centrifuged and the total protein in the plasma is measured by refractometer. The second tube is heated at 56 C for 3 minutes, which precipitates the fibrinogen. The second tube is then centrifuged and the protein result read similarly. The protein result in the heated tube is subtracted from the result in the unheated tube; the difference is equivalent to the fibrinogen that was removed from the plasma in the second tube by heating and centrifuging.
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- 2 - Elements of Interior DesignDocument4 pages2 - Elements of Interior DesignYathaarth RastogiPas encore d'évaluation
- PC3 The Sea PeopleDocument100 pagesPC3 The Sea PeoplePJ100% (4)
- KINETIC THEORY OF GASES TUTORIALDocument6 pagesKINETIC THEORY OF GASES TUTORIALMat SyafiqPas encore d'évaluation
- Lyceum of The Philippines University Cavite Potential of Peanut Hulls As An Alternative Material On Making Biodegradable PlasticDocument13 pagesLyceum of The Philippines University Cavite Potential of Peanut Hulls As An Alternative Material On Making Biodegradable PlasticJayr Mercado0% (1)
- Compare Blocks - ResultsDocument19 pagesCompare Blocks - ResultsBramantika Aji PriambodoPas encore d'évaluation
- Hypophosphatemic Rickets: Etiology, Clinical Features and TreatmentDocument6 pagesHypophosphatemic Rickets: Etiology, Clinical Features and TreatmentDeysi Blanco CohuoPas encore d'évaluation
- 07 Raction KineticsDocument43 pages07 Raction KineticsestefanoveiraPas encore d'évaluation
- A Fossil Hunting Guide To The Tertiary Formations of Qatar, Middle-EastDocument82 pagesA Fossil Hunting Guide To The Tertiary Formations of Qatar, Middle-EastJacques LeBlanc100% (18)
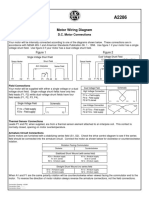
- Motor Wiring Diagram: D.C. Motor ConnectionsDocument1 pageMotor Wiring Diagram: D.C. Motor Connectionsczds6594Pas encore d'évaluation
- Chapter 16 - Energy Transfers: I) Answer The FollowingDocument3 pagesChapter 16 - Energy Transfers: I) Answer The FollowingPauline Kezia P Gr 6 B1Pas encore d'évaluation
- Mechanical Specifications For Fiberbond ProductDocument8 pagesMechanical Specifications For Fiberbond ProducthasnizaPas encore d'évaluation
- Helmitin R 14030Document3 pagesHelmitin R 14030katie.snapePas encore d'évaluation
- Entrepreneurship Project On Jam, Jelly & PicklesDocument24 pagesEntrepreneurship Project On Jam, Jelly & Picklesashish karshinkarPas encore d'évaluation
- Lightwave Maya 3D TutorialsDocument8 pagesLightwave Maya 3D TutorialsrandfranPas encore d'évaluation
- Proposal Anguria Pasta NewDocument24 pagesProposal Anguria Pasta NewNOOR IRDINA HAFIZAH BT TAUPISPas encore d'évaluation
- Chapter 10 AP GP PDFDocument3 pagesChapter 10 AP GP PDFGeorge ChooPas encore d'évaluation
- WOOD Investor Presentation 3Q21Document65 pagesWOOD Investor Presentation 3Q21Koko HadiwanaPas encore d'évaluation
- An Online ECG QRS Detection TechniqueDocument6 pagesAn Online ECG QRS Detection TechniqueIDESPas encore d'évaluation
- Lathe - Trainer ScriptDocument20 pagesLathe - Trainer ScriptGulane, Patrick Eufran G.Pas encore d'évaluation
- Diia Specification: Dali Part 252 - Energy ReportingDocument15 pagesDiia Specification: Dali Part 252 - Energy Reportingtufta tuftaPas encore d'évaluation
- India - Wikipedia, The Free EncyclopediaDocument40 pagesIndia - Wikipedia, The Free EncyclopediaPrashanth KrishPas encore d'évaluation
- WK 43 - Half-Past-TwoDocument2 pagesWK 43 - Half-Past-TwoKulin RanaweeraPas encore d'évaluation
- Front Wheel Steering System With Movable Hedlights Ijariie5360Document6 pagesFront Wheel Steering System With Movable Hedlights Ijariie5360Ifra KhanPas encore d'évaluation
- The Simple PendulumDocument5 pagesThe Simple PendulumDexter TorringtonPas encore d'évaluation
- Fraktur Dentoalevolar (Yayun)Document22 pagesFraktur Dentoalevolar (Yayun)Gea RahmatPas encore d'évaluation
- Emerson EPC48150 1800 FA1EPC48300 3200 FA1 V PDFDocument26 pagesEmerson EPC48150 1800 FA1EPC48300 3200 FA1 V PDFRicardo Andrés Soto Salinas RassPas encore d'évaluation
- Letter of MotivationDocument4 pagesLetter of Motivationjawad khalidPas encore d'évaluation
- Uhf Leaky Feeder Rev CDocument4 pagesUhf Leaky Feeder Rev CLuis Isaac PadillaPas encore d'évaluation
- TILE QUOTEDocument3 pagesTILE QUOTEHarsh SathvaraPas encore d'évaluation
- Transport of OxygenDocument13 pagesTransport of OxygenSiti Nurkhaulah JamaluddinPas encore d'évaluation