Académique Documents
Professionnel Documents
Culture Documents
N262+HH Paper
Transféré par
xquisiteludaDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
N262+HH Paper
Transféré par
xquisiteludaDroits d'auteur :
Formats disponibles
1
N262 Health History and Interview Genogram Paper Interviewers Name_Kynesa Myler________ Patient Information: Initials: KAP Age: 52 Occupation: college deans secretary Religion: Christian Country of Birth: USA Date of Admission: 01/19/2012 Admitting Medical Diagnosis: Rheumatoid arthritis Date _01/20/2012_____
Chief Complaint & Reason for Hospitalization: patient complains of intense pain in the joints of the hands, wrists and knees on both sides of the body making job as a secretary very painful and difficult
Patient Problem: P: Palliative, Provocative- pain most intense in the mornings or after periods of inactivity. Patient has tried OTC pain medications Q: R: S: Quality, Quantity- severe and feels inflamed Region, Radiation- in wrists, hands and knees on both sides of body Scale of severity- on a pain scale of 0-10; patient stated 10. Patient is on leave from work because of the pain, doing chores around the house and dressing herself is a hardship
T: Timing- a few months before being diagnosed with rheumatoid arthritis. Pain became increasingly worst and lasts longer, stiffness lasts for about an hour U: Understand Patients Perception- patient thinks disease is getting worse of the problem
Past History: broke left ankle at 5, appendicitis in 1999, car accident in 2004 resulting in broken clavicle and a concussion.
Immunizations: all up to date. Received flu shot last season.
Allergies: patient denies any allergies
Habits: Cigarettes: quit 20 years ago after smoking for 15 years Alcohol: drinks two glasses of wine a week Hard drugs: denies doing hard drugs Coffee, tea or other caffeine (coke): denies drinking coffee but drinks a cup of tea every day Medications (currently taking): Aleve for pain Exercise: worked the treadmill daily but now pain interferes
REVIEW OF PHYSICAL SYSTEMS (ROS): Obtain information from the patient on the systems noted. Questions should include those below, but are not limited to them. General Health: 57 ; 178lbs. Patient admits to fatigue, malaise and limited mobility in the mornings, some difficulty sleeping if pain is intense, denies chills and sweats
Skin: area around joints are swollen, tender and inflamed, denies any petechiae, ecchymosis, lesions, hair loss, brittle hair and nails.
Head: denies pain, dizziness, vertigo, headache, history of injury or loss of consciousness
Eyes: eye burning and itching, had corrective eye surgery 5 years ago for nearsightedness
Ears: patient denies any hearing loss, discharge, pain, irritation or ringing in ear
Nose & Sinuses: patient denies pain, congestion and discharge, excessive sneezing, epistaxis, soreness. Also denies obstructed breathing, injuries and inability to smell
Mouth & Throat: last dental visit was October 2011. Brushes twice a day, flosses at night. Denies toothaches, lesions, and soreness. Has sensitivity to hot and cold foods and dry mouth,
but denies lack of taste, hoarseness, and frequent sore throat
Neck: patient denies any stiffness, pain, limited ROM or masses. No enlarged tender nodes in neck, axilla, or inguinal areas
Breasts: tenderness in left breast. Patient denies any masses, pain, or discharge. Never conducts self-breast examination. Date of last mammogram was December 2011. Date of last physical examination of breasts was November 2011
Chest & Respiratory System: patient has chest pain when taking a breath. Denies wheezing or shortness of breath, hemoptysis, or cough. No history of asthma, bronchitis, or pneumonia. Cannot remember date of last TB skin test and never had a chest x-ray
Cardiovascular System: patient has chest pain when taking a breath. Denies any palpitations, cyanosis, heart murmur, hypertension. History of hypertension in family. Denies coronary heart disease and no history of rheumatic fever. Activity tolerance is appropriate for age.
Peripheral Vascular System: edema in knees and wrists. Denies varicose veins, swelling of arms or legs or intermittent claudication. Also denies thrombophlebitis, and color or temperature changes of upper and lower extremities
Gastrointestinal System: appetite is normal. Denies constipation or diarrhea, or flatulence. Also denies nausea, vomiting, hemorrhoids, hernias, jaundice, or bleeding. Yesterdays food and fluid intake: oatmeal, vegetarian burger, french fries, soup, cheesecake, orange juice, diet iced tea, water.
Genitourinary System: denies bladder or kidney conditions or STDs. Denies hematuria, urgency, frequency, dysuria, incontinence, nocturia, polyuria, or dysmenorrhea. Onset of menses at age 12, normal flow once a month, date of last menstral cycle was 3 years ago. Age of menopause was 49. Date of last Pap smear was November 2011.
Sexual History: had first intercourse at 20. Denies any problems with intercourse. Has had 3 sexual partners. Denies use of birth control.
Musculoskeletal System: pain and stiffness in joints. Denies deformity or gout. Has arthritis and has limited ROM with joints. Denies history of disc disease, fractures, or low back pain.
Central Nervous System: denies loss of consciousness, or clumsiness. Also denies difficulty with balance, weakness, or paralysis. Denies any tremor, neuralgia, paresthesia. No history of emotional disorder or speech articulation.
Endocrine System: denies diabetes, polyuria, polydipsia. Also denies intolerance to heat and cold, or hirsutism. Hematologic System: denies excessive bruising or bleeding, or blood transfusions. Patient is unaware of blood type. Denies any excessive exposure to x-rays or toxic agents.
Social/Cultural System: immediate family is husband of 24 years and two sons ages 23, 21. Both sons are away at college. Patient has worked as a secretary for the Dean of Education at a University. Patient is very spiritual and believes everything happens for a reason, although she worries about not being able to do things for herself anymore. Patient has a solid support group with many siblings, both parents passed away. She and her family are active in searching for treatments and cures to lessen the pain she suffers. Genogram: Answer the following three questions: 1. Does the patients present problem appear related to the family history or individual health habits?
2. What risk factors, if any, are suggested by the patients health habits or the family history? (e.g. smoking or alcoholism in family)
3. What preventive teaching should be included in the nurses care plan for this individual? Insert or attach Genogram:
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- SketchyPharm Antimicrobials FINALDocument51 pagesSketchyPharm Antimicrobials FINALKl100% (2)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Substance Misuse MnemonicDocument3 pagesSubstance Misuse MnemonicAmrAlaaEldin0% (1)
- MOH DHA HAAD Dental Study Material Part 2Document33 pagesMOH DHA HAAD Dental Study Material Part 2Junaid Ramzan89% (37)
- FLU Strategies PreparednessDocument7 pagesFLU Strategies PreparednessxquisiteludaPas encore d'évaluation
- Abx ClassesDocument1 pageAbx ClassesxquisiteludaPas encore d'évaluation
- Int. J. Epidemiol. 2006 Chen 121 30Document10 pagesInt. J. Epidemiol. 2006 Chen 121 30xquisiteludaPas encore d'évaluation
- Evidence Based Practice Step by Step The Seven.30Document3 pagesEvidence Based Practice Step by Step The Seven.30Putra PurnamaPas encore d'évaluation
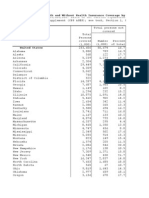
- United States: Table With Row Headers in Column A and Column Headers in Rows 4 and 5. Leading Dots Indicate Sub-PartsDocument4 pagesUnited States: Table With Row Headers in Column A and Column Headers in Rows 4 and 5. Leading Dots Indicate Sub-PartsxquisiteludaPas encore d'évaluation
- Signed Management of Dehydration in Palliative CareDocument7 pagesSigned Management of Dehydration in Palliative CareMarianne LayloPas encore d'évaluation
- Severe Hyperglycemia: Effects of Rehydration On Endocrine Derangements and Blood Glucose ConcentrationDocument8 pagesSevere Hyperglycemia: Effects of Rehydration On Endocrine Derangements and Blood Glucose Concentrationmohamadafif_drPas encore d'évaluation
- Dr. Dian Kusumaningrum - PRESENTASI JCCA-ANTIBIOTIC DOSING IN CRITICALLY ILLDocument31 pagesDr. Dian Kusumaningrum - PRESENTASI JCCA-ANTIBIOTIC DOSING IN CRITICALLY ILLRestu TriwulandaniPas encore d'évaluation
- Hepatorenal SyndromeDocument6 pagesHepatorenal SyndromeAditi Ujjawal0% (1)
- Approach To Abdominal PainDocument4 pagesApproach To Abdominal PainShamen KohPas encore d'évaluation
- Takayasu S Arter It IsDocument5 pagesTakayasu S Arter It IsButarbutar MelvaPas encore d'évaluation
- Herbal MedicinesDocument8 pagesHerbal MedicinesKrishna BalsarzaPas encore d'évaluation
- 674-Article Text-5409-1-10-20210430Document6 pages674-Article Text-5409-1-10-20210430Rizca Cholidatun Ni'mahPas encore d'évaluation
- Per-Pl 206Document266 pagesPer-Pl 206Wan YusufPas encore d'évaluation
- Epilepsy: Dr. Hj. Meiti Frida, SP.SDocument47 pagesEpilepsy: Dr. Hj. Meiti Frida, SP.SZacky Aulia MursiPas encore d'évaluation
- CareofolderadultsDocument8 pagesCareofolderadultsMonique FranciscoPas encore d'évaluation
- Disorders of The Thyroid and Parathyroid Glands: Ms TeamDocument36 pagesDisorders of The Thyroid and Parathyroid Glands: Ms TeamShy Dela PuertaPas encore d'évaluation
- Nursing SkillDocument1 pageNursing SkillMarina Wasem NetzlaffPas encore d'évaluation
- What Is An Intravenous Pyelogram (IVP) ? How Should I Prepare?Document4 pagesWhat Is An Intravenous Pyelogram (IVP) ? How Should I Prepare?MarcelitaTaliaDuwiriPas encore d'évaluation
- Respiratory Syncytial Virus in LowerDocument6 pagesRespiratory Syncytial Virus in LowerShailendra ParajuliPas encore d'évaluation
- Hallucinations and Hearing VoicesDocument4 pagesHallucinations and Hearing VoicesCazacu ParascoviaPas encore d'évaluation
- Nclex RN GI & Burns & FracturesDocument87 pagesNclex RN GI & Burns & Fracturesgraceface55100% (4)
- SHEA-APIC Guideline - Infection Prevention and Control in The Long-Term Care FacilityDocument53 pagesSHEA-APIC Guideline - Infection Prevention and Control in The Long-Term Care FacilityAqsha RamadhanisaPas encore d'évaluation
- A Concept Paper: HIV: By: Nichol Niño H. BanaagDocument2 pagesA Concept Paper: HIV: By: Nichol Niño H. Banaaglhuk banaagPas encore d'évaluation
- What Happens After The Cystoscopy ProcedureDocument2 pagesWhat Happens After The Cystoscopy ProcedureStepyn SalvadorPas encore d'évaluation
- Thesis On Computer Vision SyndromeDocument8 pagesThesis On Computer Vision Syndromebsqfc4d5100% (2)
- Practical 3: Blood Grouping Test ObjectiveDocument2 pagesPractical 3: Blood Grouping Test ObjectiveTHASVIN OFFICIAL NETWORKPas encore d'évaluation
- OPD Rot Exam StudentDocument3 pagesOPD Rot Exam StudentFerdinand TerceroPas encore d'évaluation
- Obsessive - Compulsive Personality Disorder: A Current ReviewDocument10 pagesObsessive - Compulsive Personality Disorder: A Current ReviewClaudia AranedaPas encore d'évaluation
- Mapping R5B PDFDocument12 pagesMapping R5B PDFSulung Ade PratamaPas encore d'évaluation
- The Role of EEG in Epilepsy - A Critical ReviewDocument12 pagesThe Role of EEG in Epilepsy - A Critical ReviewNicki Pinzon NariñoPas encore d'évaluation
- Leaflet Final Ann PERKENI 2023Document2 pagesLeaflet Final Ann PERKENI 2023ngurahardhi88Pas encore d'évaluation