Académique Documents
Professionnel Documents
Culture Documents
Iodine
Transféré par
ประดิพัทธ์ ประมุขDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Iodine
Transféré par
ประดิพัทธ์ ประมุขDroits d'auteur :
Formats disponibles
Auris Nasus Larynx 39 (2012) 193197 www.elsevier.
com/locate/anl
Clinical impact of iodine staining for diagnosis of carcinoma in situ in the oor of mouth, and decision of adequate surgical margin
Akihito Watanabe a,*, Masanobu Taniguchi a, Hitoshi Tsujie a, Masao Hosokawa b, Masahiro Fujita c, Shigeyuki Sasaki d
Department of Otolaryngology, Keiyukai Sapporo Hospital, Sapporo, Japan b Department of Surgery, Keiyukai Sapporo Hospital, Sapporo, Japan c Keiyukai Institute of Clinical & Surgical Pathology, Sapporo, Japan d Department of Medical Science, Health Science, University of Hokkaido, Ishikari-tobetsu, Japan Received 4 October 2010; accepted 3 August 2011 Available online 31 August 2011
a
Abstract Objective: The use of iodine staining has been recommended for the early detection of squamous cell carcinoma (SCC) in the upper aerodigestive tract. The purpose was to verify the effectiveness of iodine staining in detecting early squamous cell carcinoma in the oor of mouth. Methods: Between 1995 and 2005, otolaryngological examinations including the oor of mouth were performed for 2278 esophageal cancer patients as a screening program of high-risk patient group. Iodine staining was applied to a lightly reddish and/or white patch, and/or uneven lesions in the oor of the mouth. Forceps biopsy was performed for demarcated unstained or lightly stained lesions. Three patients with the tumors in the oor of mouth, which were diagnosed as more over T2 level just by visual examination, were excluded from this study. If SCC was found in the specimen, mucosal resection was performed with a safety margin of 2 mm from the unstained or lightly stained lesion. The incidence, rate of carcinoma in situ, and prognosis of cancer of the oor of mouth (CFOM) were assessed. Results: Iodine staining was performed for 72 of 2278 patients (3.2%) according to the presence of suspicious reddish and/or whitish and/or uneven lesions. Of these, unstained or lightly stained areas after iodine staining were recognized in 47 patients and SCC was revealed in 28 of 47 patients. The diagnosis of other 19 patients included inammatory mucosa (n = 11), low grade dysplasia (n = 6), and hyperkeratosis (n = 2). Sensitivity and specicity of iodine staining for detecting SCC were 100% and 59.6%, respectively. Pathological diagnosis of the 28 patients included squamous cell carcinoma in situ (n = 12), microinvasive squamous cell carcinoma (n = 15) disease, and focal invasive squamous cell cancer (n = 1). Twenty-four of 28 patients were treated with mucosal resection without mandible resection. The other 4 patients did not receive the treatment of CFOM due to concomitant far advanced esophageal cancer. In 24 patients undergoing mucosal resection, no patients developed local recurrence or metastasis to the cervical lymph nodes during an average of 74.2 months of follow-up period (from 7 to 156 months). The 5-year cause-specic survival of these patients was 100%. Conclusion: The use of iodine staining as a part of otolaryngological examinations may be benecial for the early detection of CFOM, including carcinoma in situ and micro-invasive SCC. Moreover, it would be very useful to determine an adequate surgical margin for locally mucosal resection. # 2011 Elsevier Ireland Ltd. All rights reserved.
Keywords: Iodine staining; Carcinoma in situ; Early diagnosis; Cancer of oor of mouth; Surgical margin
1. Introduction
* Corresponding author at: Department of Otolaryngology, Keiyukai Sapporo Hospital, Kita 1-1, Hondori 14-chome, Shiroishi-ku, Sapporo 003-0027, Japan. Tel.: +81 11 863 2101; fax: +81 11 864 1032. E-mail address: akihito-watanabe@keiyukaisapporo.or.jp (A. Watanabe).
Cancer of the oor of mouth (CFOM) is one of the tumors that are difcult to be detected in early stages. It is usually recognized when it becomes symptomatic, and often reaches
0385-8146/$ see front matter # 2011 Elsevier Ireland Ltd. All rights reserved. doi:10.1016/j.anl.2011.08.004
194
A. Watanabe et al. / Auris Nasus Larynx 39 (2012) 193197
an advanced stage at the time of diagnosis [13]. According to previous reports, stage III and IV disease comprised 42 84% of all patients with CFOM [1,36]. These patients with advanced CFOMs frequently have cervical nodal involvement that affects survival, and may require the deformities and disabilities that impair the quality of life as a result of surgical treatment including mandibular resection. Therefore, the early diagnosis of CFOM is of critical importance to increase the probability of cure with minimum impairment and deformity [7]. Recently there has been an increase in the development of oral cancer screening tools, however, visual examination and palpation have remained the gold standard techniques for the identication of mucosal lesion of the oral cavity [8]. In other eld such as esophagus [9] and hypopharynx [10], it is recognized that iodine staining is very useful to detect early squamous cell carcinoma (SCC) and to decide its surgical margin. Since 1995, we have routinely performed otolaryngological examination for patients with esophageal cancer (EC) before and after treatment of EC, because EC patients are at a high risk for developing additional SCC of the head and neck. We have previously reported the validity of this screening program for early diagnosis of SCC of the head and neck, with signicant improvements in survival of EC patients [11]. This screening program includes endoscopic examinations in the larynx, hypopharynx, oropharynx, and oral cavity associated with iodine staining if necessary. In our limited experience, mucosa of the oor of mouth can be assessed with iodine staining like pharyngeal mucosa and esophageal mucosa, under the condition that saliva is rinsed out. In this article, we focus on the detection of CFOM, especially carcinoma in situ, and report a clinical signicance of iodine staining in the screening of EC patients. Moreover, we examine another benet of iodine staining in determination of adequate surgical margin when mucosal resection is applied to the CFOM.
reddish lesion and/or whitish lesion and/or minute uneven lesion in the oor of mouth. Patients without such a lesion did not receive an iodine staining and underwent the screening examination 6 months later. If such a lesion was detected in the oor of mouth, iodine staining was performed at outpatient clinic without anesthesia. A cotton ball soaked in 1.5% iodine solution was put on to coat the oor of the mouth, after wiping saliva on the mucosa of the mouth with dry cotton ball. If a distinctly demarcated unstained or lightly stained lesion measuring 5 mm or more in greatest diameter was detected, a forceps biopsy specimen was obtained from the lesion and immediately stained with hematoxylin and eosin for histopathological examination. The mean follow-up period was 50 months (range 1184 months). In principle, these procedures were performed after full explanation for all EC patients, except for those who had refused to receive the screening program, and those who lived a long distance away and were followed by the local hospital. The prevalence of CFOM, the clinical stage (determined by the 2002 UICC (International Union Against Cancer) Classication), treatment, and survival were investigated. All results were assessed and analyzed on 1 October 2010. Survival rates were calculated by the KaplanMeier method. All analyses were performed with SPSS software (SPSS Inc, Chicago, IL). A p value of less than 0.05 was considered signicant.
3. Results Of 2278 EC patients who had received otolaryngological examinations, 72 patients (3.2%) underwent iodine staining based on the criteria described above. There were 1 patient with a reddish and depressed lesion, 3 patients with at reddish and whitish lesions, 7 patients with slightly elevated reddish and whitish lesions, 10 patients with slightly elevated whitish lesions, 24 patients with slightly elevated reddish lesions and 27 patients with at reddish lesions. Iodine staining revealed demarcated unstained or demarcated lightly stained areas in 47 of 72 patients, who subsequently received a forceps biopsy. All 72 patients were asymptomatic for the lesion of the oor of the mouth. Of the biopsy specimens taken from the 47 patients, SCC was detected in 28 patients, before (n = 9) and after (n = 19) treatment of EC. Thus, the nal prevalence of CFOM among 2278 EC patients who had received otolaryngological examinations was 1.2% (28 of 2278). These 28 patients with CFOM had any of the following, squamous cell carcinoma in situ (n = 12), microinvasive squamous cell carcinoma (n = 15), or focal invasive squamous cell carcinoma (n = 1), which were all asymptomatic tumors. Clinical stages of the 28 patients were stage 0 in 12, stage I in 10, and stage II in 6 patients, respectively. No SCCs have arisen in 25 patients with a macroscopic demarcated reddish and/or whitish lesion and/or uneven lesion but stained with iodine.
2. Materials and methods Between May 1995 and December 2005, otolaryngological examinations were performed for 2278 patients with esophageal cancer (EC), as a screening program of patients who were at a high risk for developing SCC. There were 2029 men and 249 women, with a mean age of 65.1 0.2 years (mean standard error) at the initial diagnosis of EC. All patients were Japanese. Their alcohol index and Brinkman index were 2837 73 and 730 15, respectively. The screening program included otolaryngological examinations before treatment of EC and periodical examinations at every 6 months after treatment of EC, which were carried out by one otorhinolaryngologist (A.W.). The oral cavity, nasal cavity, pharynx (naso-, oro-, hypo-) and larynx were checked very carefully to detect early SCCs with the use of exible berscope. The criteria for performing iodine staining were the presence of a suspicious
A. Watanabe et al. / Auris Nasus Larynx 39 (2012) 193197
195
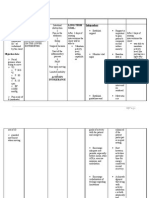
Table 1 Results of 72 patients undergoing iodine staining to detect carcinoma of the oor of mouth. Unstained area (+) SCC (+) SCC () 28 19 Unstained area () 0 25
Sensitivity: 28/28 = 100%; specicity: 25/44 = 56.8%.
Likewise, no SCCs have arisen in 19 patients who received a forceps biopsy that was negative for malignancy. Thus, sensitivity and specicity of iodine staining for detecting SCC was 100% and 56.8%, respectively (Table 1). Of the 28 patients with CFOM, 24 received a locally mucosal resection, 1 received a locally mucosal resection plus radiotherapy due to close vertical surgical margin from focal invasive tumor, and 4 received no treatment for CFOM due to the presence of far advanced EC. Locally mucosal resection was performed using contact YAG laser, in principle with a safety margin of 2 mm from unstained lesion of iodine staining, since tumors were judged to have only a slight involvement to mucosal layer and submucosal layer. If the tumor involved the anterior oor of the mouth, the Whartons duct was also excised because tumor was considered to involve its orice. After submandibular duct was repositioned and sutured to the mucosa with two or three sutures, articial dermis was applied to the defect of mucosa of the oor of mouth. Representative pictures of CFOM are shown (Fig. 1).
Pathological examination revealed SCC of the oor of mouth extending close to the horizontal surgical margin. Unstained areas, which can be clearly visible, in all cases corresponded to cancer formation in pathological examination. Thus we could leave the stump of the margin negative for SCC in all 28 patients undergoing locally mucosal resection (Fig. 2). After mucosal resection with (n = 1) or without (n = 16) additional radiotherapy, none of these patients developed local recurrence and metastasis to the cervical lymph nodes during an average of 74.2 months of follow-up period (from 7 to 156 months). No patients received mandibulectomy and died from CFOM, however, 11 patients, including 4 patients who did not received locally mucosal resection due to the advanced EC, died from EC and 2 patients died from other disease. The 5year crude and cause-specic survival of these 28 patients was 57.1% and 100% at a mean follow up of 64.4 months (Fig. 3), respectively. During this study period, 3 patients with EC who had dropped out from this screening program developed symptomatic CFOMs and found as those with stage IV disease. These 3 patients received neck dissection and wide resection of the oral oor and tongue with marginal mandibulectomy, followed by postoperative radiotherapy (4050 Gy). Unfortunately, all these patients died a mean of 29.3 months after initial treatment. The cause of death was the recurrence (46 months after treatment), lung metastases (28 months), and aspiration pneumonia (14 months), respectively.
Fig. 1. Procedure of local mucosal resection for carcinoma of the oor of mouth: (A) an overview before iodine staining. Arrows indicate a slightly reddish area; (B) after iodine staining, a distinctly demarcated, unstained lesion was clearly recognized; (C) the surgical margin (dots) was marked using laser; (D) an overview after mucosal resection; (E) articial dermis was applied to the defect of mucosa of the oor of mouth. (For interpretation of the references to color in this gure legend, the reader is referred to the web version of the article.)
196
A. Watanabe et al. / Auris Nasus Larynx 39 (2012) 193197
Fig. 2. Histologic hematoxylin and eosin stained section taken from the resected specimen. Original magnication: 500.
4. Discussion CFOM remains to be one of the most aggressive neoplasms of the head and neck [13]. Its propensity to invade the mandible and the lymphatic beds of both necks often makes local and regional control exceedingly difcult [1]. In addition, most CFOMs are asymptomatic until they reach an advanced disease, which may require mandibular resection and cause deformities and disabilities. The reported incidence of mandibulectomy requirement ranged from 52% to 56% in patients with CFOM [1,12]. In this study, CFOMs that were developed in patients who had dropped out from this screening program were all stage IV disease, and treated with neck dissection and wide resection of the oral oor with marginal mandibulectomy. In fact, it seems to be very difcult to detect carcinoma in situ in the oor of mouth by usual examination like visual examination and palpation, because there are only minute objective changes in the mucosa without subjective symptoms. In general, in the presence of only minute uneven and lightly reddish lesions without subjective symptoms, very few physicians may attempt to take biopsy specimens from the
Fig. 3. KaplanMeier survival curves for patients whose tumors were detected by screening program. Cause-specic and crude survival curves are shown.
lesions. However, from our experience, some carcinoma in situ may be present in these lesions, which are similar to those caused by inammation. Subsites in oral cavity are covered with mucosa of different thickness; for example, dorsum of tongue, gingival and hard palate are covered with thick mucosa and oor of the mouth is covered with thin mucosa. I think that mucosa of the oral oor is similar to and can be evaluated like that of the pharynx or esophagus from its features of mucosa thickness or other reason. Thus I recommended using iodine staining especially at the oor of mouth. In this study, we have applied iodine staining to such reddish lesions to determine whether they needed biopsy. In the presence of a demarcated unstained area or a lightly stained area after staining, we took biopsy specimens from the lesion. In the absence of such demarcated area, we did not carry out biopsy. We believe that iodine staining can reduce unnecessary biopsy procedure as well as increase the chance of detection of carcinoma in situ in the oor of mouth. In this study, carcinoma in situ was detected in 12 patients, which comprised 42.9% of all 28 patients whose CFOMs were detected by our screening program including iodine staining. These patients were treated with mucosal resection without mandibulectomy, and obviously had an earlier stage disease and better survival than the usual patient population with CFOM. In general, iodine has irritate reaction so that it is thought not to apply the pharynx even under topical anesthesia [10]. But it is acceptable to use it in the oor of mouth even though no topical anesthesia. In this study, all patients could complete this method. However, we have to rinse out saliva in the use of iodine staining. It reduces the staining power of iodine solution, and thus reduces the contrast of unstained area. Iodine solution per se stimulates the salivary secretion, thus the area for forceps biopsy should be determined immediately after staining of iodine solution on the oor of the mouth. The decrease in the contrast of unstained area would make the diagnosis of SCC more difcult in the oor of the mouth than in the esophagus or hypopharynx, but the diagnostic specicity can be improved if saliva is adequately rinsed and wiped out. Regarding the criteria for performing iodine staining, our criteria the presence of a suspicious reddish or whitish color lesion, or minute uneven lesion would be appropriate because no CFOM was developed in patients who did not undergo iodine staining. In other words, SCC was revealed only in patients undergoing iodine staining based on the criteria described above. There was no false-negative case in relation to the iodine staining with the presence of SCC. The iodine staining itself is not a new method for the detection of early cancer in other areas, our study seems to be worth reporting according to the following two points: (1) there have been very few reports showing the value of iodine staining even for the CIS in this area and (2) it would be a new nding that leaving a margin of 2 mm from unstained lesion of iodine staining can be enough for locally mucosal resection in this area.
A. Watanabe et al. / Auris Nasus Larynx 39 (2012) 193197
197
The nal prevalence of CFOM detected by our screening program, 1.2% in this study, might be lower than expected in the high-risk patient group. Of course, the cost benet performance would not be good if such screening is performed only for the purpose of detection of CFOM. However, the procedure presented in this study can be performed as a part of total otolaryngologic examinations. In our previous experiences, SCCs of the head and neck were found in approximately 10% of EC patients [11]. In addition, iodine staining of the oor of mouth can be easily performed in the outpatient clinic whereas that of the pharynx and larynx may require general anesthesia in the operation room, due to its mucosal irritation [10]. Its easiness of procedure may have contributed to the detection of many CIS lesions in this study. Moreover, decision of surgical margin is another advantage associated with the use of iodine staining. In the mucosal resection of CFOM, we resected CFOM with safety margin of only 2 mm from unstained lesion, but no patients have developed local recurrence. The iodine staining application for the detection of CFOM may be justied in patients who are at a high risk for developing SCC, for example, those with a preceding upper aerodigestive malignancy or heavy-drinkers with habitual smoking. Recently, narrow band imaging endoscopy has been developed and showed the power to detect early pharyngeal cancer and laryngeal cancer [13,14]. We have started to conduct cancer screening in oor of mouth by utilizing NBI endoscope. We would like to show this result in the near future. In conclusion, the screening program for the detection of CFOM associated with iodine staining based on our criteria revealed 28 CFOMs (1.2%) among 2278 patients with esophageal cancer. All 28 patients had early stage of disease, which could be treated with mucosal resection without mandible resection. No patients developed recurrence of CFOMs after locally mucosal resection with a safety margin of 2 mm from unstained lesion. Sensitivity and specicity of iodine staining for detecting SCC based on our criteria was 100% and 59.6%, respectively. The use of iodine staining as a part of otolaryngological examinations may be benecial
for the early detection of CFOM and decision of surgical margin for locally mucosal resection in patients who are at a high risk for developing CFOM. References
[1] Klotch DW, Muro-Cacho C, Gal TJ. Factors affecting survival for oor-of-mouth carcinoma. Otolaryngol Head Neck Surg 2000;122:4958. [2] Epstein JB, Scully C, Spinelli J. Toluidine blue and Lugol 1s iodine application in the assessment of oral malignant disease and lesions at risk of malignancy. J Oral Pathol Med 1992;21:1603. [3] Harrold CC. Management of cancer of the oor of the mouth. Am J Surg 1971;122:48793. [4] Marks JE, Lee F, Smith PG, Ogura JH. Floor of mouth cancer: patient selection and treatment results. Laryngoscope 1983;93:47580. [5] Araki LT, Ebihara S, Ohta Y, Yoshizumi T, Ohyama W, Saikawa M, et al. Surgical management of squamous cell carcinoma of the oor at the mouth. Jpn J Clin Oncol 1990;20:38791. [6] Shaha AR, Spiro RH, Shar JP, Strong EW. Squamous carcinoma of the oor of the mouth. Am J Surg 1984;148:4559. [7] Joseph BK. Oral cancer: prevention and detection. Med Prin Pract 2002;11:325. [8] Lin YC, Watanabe A, Chen WC, Lee KF, Lee IL, Wnag WH. Narrowband imaging for early detection of malignant tumors and radiation effect after treatment of head and neck cancer. Arch Otolaryngol Head Neck Surg 2010;136:2349. [9] Shimizu Y, Omori T, Yokoyama A, Yoshida T, Hirota J, Ono Y, et al. Endoscopic diagnosis of early squamous neoplasia of the esophagus with iodine staining: high-grade intra-epithelial neoplasia turns pink within a few minutes. J Gastroenterol Hepatol 2008;23:54650. [10] Watanabe A, Hosokawa M, Taniguchi M, Tsujie H, Sasaki S. Impact of endoscopic screening on early detection of hypopharyngeal cancer. Head Neck 2006;28:3504. [11] Watanabe A, Hosokawa M, Taniguchi M, Sasaki S. Periodic pharyngolaryngoscopy detect early head and neck cancer and improves survival in esophageal cancer. Ann Thorac Surg 2003;76:1699705. [12] Hicks Jr WL, Loree TR, Garcia RI, Maamoun S, Marshall D, Orner JB, et al. Squamous cell carcinoma of the oor of mouth: a 20-year review. Head Neck 1997;19:4005. [13] Watanabe A, Taniguchi M, Tsujie H, Hosokawa M, Fujita M, Sasaki S. The value of narrow band imaging endoscope for early head and neck cancers. Otolaryngol Head Neck Surg 2008;44:6451. [14] Watanabe A, Taniguchi M, Tsujie H, Hosokawa M, Fujita M, Sasaki S. The value of narrow band imaging for early detection of laryngeal cancer. Eur Arch Otorhinolaryngol 2009;101:71023.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Seafarer Health Forms for COVID-19 ClearanceDocument3 pagesSeafarer Health Forms for COVID-19 ClearanceYuraPas encore d'évaluation
- 13 IMPLANT SUPPORTED FIXED PROSTHESESmic PDFDocument52 pages13 IMPLANT SUPPORTED FIXED PROSTHESESmic PDFManaila GeorgianPas encore d'évaluation
- Food Safety: HABC Level 2 Award in Food Safety in Catering (QCF)Document3 pagesFood Safety: HABC Level 2 Award in Food Safety in Catering (QCF)Caroline FrostPas encore d'évaluation
- ABYIP of SK of Brgy. EspanaDocument7 pagesABYIP of SK of Brgy. EspanaCindy RoyoPas encore d'évaluation
- What Is Stomatitis DiseaseDocument4 pagesWhat Is Stomatitis DiseaseRoyster CabralPas encore d'évaluation
- RadiologyDocument2 pagesRadiologyImrose MahinePas encore d'évaluation
- UPITNIK Oswestry Low Back Pain Disability Questionnaire (In Dutch) PDFDocument4 pagesUPITNIK Oswestry Low Back Pain Disability Questionnaire (In Dutch) PDFiplascakPas encore d'évaluation
- Memorandum of Agreement - Brgy and SalisDocument3 pagesMemorandum of Agreement - Brgy and SalisBARANGAY MOLINO IIPas encore d'évaluation
- Dental Trauma WorksheetDocument2 pagesDental Trauma WorksheetSteliana CaramanPas encore d'évaluation
- Restorative dentistry for worn teethDocument7 pagesRestorative dentistry for worn teethSohrab KhanPas encore d'évaluation
- Stomach Ulceration Leaflet and Drugs Used To Treat Peptic Ulcer DiseaseDocument4 pagesStomach Ulceration Leaflet and Drugs Used To Treat Peptic Ulcer DiseasePrisma TridaPas encore d'évaluation
- Ebstein's Anomaly: Tricuspid Valve Defect ExplainedDocument3 pagesEbstein's Anomaly: Tricuspid Valve Defect ExplainedAndrei FetcoPas encore d'évaluation
- Robinson Mesothelioma LIVRODocument381 pagesRobinson Mesothelioma LIVROdocPas encore d'évaluation
- Wound DressingDocument23 pagesWound DressingKryztalGhail Llanora100% (1)
- Reaction PaperDocument2 pagesReaction PaperLinzie CariquetanPas encore d'évaluation
- Woman With DysuriaDocument26 pagesWoman With DysuriaAlFi KamaliaPas encore d'évaluation
- Vaccine Adverse Reaction Reporting System by Vaccine and MaufacturerDocument1 191 pagesVaccine Adverse Reaction Reporting System by Vaccine and MaufacturerGuy RazerPas encore d'évaluation
- BCG Vaccine: Serum Institute of India Pvt. LTDDocument1 pageBCG Vaccine: Serum Institute of India Pvt. LTDkemalahmadPas encore d'évaluation
- Why Period Friendly Toilets MatterDocument1 pageWhy Period Friendly Toilets MatterMaria Nativity BanarioPas encore d'évaluation
- Comp ReDocument15 pagesComp ReROBERT C. REÑA, BSN, RN, MAN (ue)Pas encore d'évaluation
- Activity IntoleranceDocument3 pagesActivity IntoleranceRheegell Ellar-Fuertes50% (2)
- Why I Desire to Study Medical MicrobiologyDocument2 pagesWhy I Desire to Study Medical MicrobiologyRobert McCaul100% (1)
- Parchem 2018 A Multidisciplinary Approach To Equipment Use in Pediatric Patient Mobilization.Document10 pagesParchem 2018 A Multidisciplinary Approach To Equipment Use in Pediatric Patient Mobilization.Evelyn_D_az_Ha_8434Pas encore d'évaluation
- Step by Step of QAP 1Document73 pagesStep by Step of QAP 1Suhazeli Abdullah100% (2)
- NRHM InitiativeDocument2 pagesNRHM InitiativeBabita DhruwPas encore d'évaluation
- Jurnal Infeksi Saluran PencernaanDocument22 pagesJurnal Infeksi Saluran PencernaanDini Okta PutriPas encore d'évaluation
- Homeopathy VithoulkasDocument8 pagesHomeopathy VithoulkassakibdPas encore d'évaluation
- Drug study criteria and cefotaxime nursing responsibilitiesDocument3 pagesDrug study criteria and cefotaxime nursing responsibilitiesChoox PriiPas encore d'évaluation
- Doctor LLLLL 4Document54 pagesDoctor LLLLL 4lovePas encore d'évaluation
- MCPS COVID-19 Simplified Decision Making ModelDocument2 pagesMCPS COVID-19 Simplified Decision Making ModelNBC MontanaPas encore d'évaluation