Académique Documents
Professionnel Documents
Culture Documents
FINALNSGHEALTHHX
Transféré par
James Michael BalicocoDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
FINALNSGHEALTHHX
Transféré par
James Michael BalicocoDroits d'auteur :
Formats disponibles
NURSING HEALTH HISTORY Nursing health history is the first part and one of the most significant aspects
in case studies. It is a systematic collection of subjective and objective data, ordering and step-by-step process inculcating detailed information in determining clients history, health status, and functional status and coping pattern. This vital information provide a conceptual baseline data utilized in developing nursing diagnosis, subsequent plans for individualized care and for the nursing process application as a whole. The health history is a current collection of organized information unique to an individual. Relevant aspects of the history include biographical, demographic, physical, mental, emotional, sociocultural, sexual, and spiritual data. In this rotation, the student affiliates were assigned at Manuel J. Santos Hospital that started on August 18, 2011. The group was designated at the Surgery ward and OR/DR area and for the entire four weeks, the affiliates were tasked to handle pre-operative, intra-operative and post-operative patients. On August 25, 2011 the group has chosen a patient for their Grand Par Presentation. On the following day, the patients significant others were informed and asked for permission. A thorough physical assessment was performed to gather important data regarding the clients state of health. In keeping with the private life of the patient and to maintain confidentiality in compliance with the ethical guidelines in conducting a nursing research, the group decided to withhold the real name of the patient. In this case, she will be addressed as Patient X. BIOGRAPHIC DATA Patient X is 74 years old and born on December 3, 1936 via Normal Spontaneous Vaginal Delivery by a hilot in their place at Jabonga, Agusan del Norte. Patient X was second to the last among the 6 siblings; with 4 sisters and a brother. She took her elementary education at Sto. Nino Elementary School and had her secondary level education at Jabonga National High School. She attained an educational level up until second year high school. Patient X is a Roman Catholic by faith and a Filipino citizen. Patient X is unemployed since she stopped selling siakoy, ensaymada and binangkal a year ago. Patient X is 4 feet and 11 inches tall and weighs 57 kgs. She has a Body mass Index of 27.53 and she is considered overweight. Patient X met the love of her life, Mr. Y at their place at Baleguian Jabonga, Agusan del Norte. On September 15, 1956 Patient X and her husband got married. Patient X has 11 children, 3 boys and 8 girls. LIFESTYLE AND ACTIVITIES OF DAILY LIVING Patient X usually wakes up at 4 in the morning, does rosary and does her walk around the living room. Sometimes she walks around their house for 30 minutes as her exercise. By 7 am, Patient X will have her breakfast together with her husband and maid. Her food usually consists of milk and rice with sugar on it. Patient X verbalized Dili naman kayo ko hilig mukaon basta pamahaw. After eating, Patient X will help her maid do the chores such as cleaning their bedroom and dusting the furnitures. Magbugha sad ko ug kahoy. Maglaba sad ko tas akong lukdohon akong nilabhan sa akong ulo. Magtahi pud ko sa among makina ug mga panty, kanang naay mga buslot pag-ganahan ko.At 11:00 am, Patient X will have her lunch which usually consists of tinolang isda, sinabawang gulay and law-uy. Dili man ko ganahan mukaon ug mga pinirito, sabaw ra jud na ang ako. Every time Patient X will eat, she can usually drink 1 glass of water. According to her, Dili man ko ganahan mu-inom ug tubig. Di ko ganahan ug bugnaw kay magsakit akong kuto-kuto. Then, Patient X will watch her favorite television shows. According to her, she is not fond of taking naps but sees to it that her granddaughters and sons do. By 3:00 in the afternoon, Patient X will have her 3 oclock prayer then she will take her snacks which commonly includes loaf bread and margarine on it. Patient X doesnt drink soft drinks and other juices except for apple juice. According to her, Nagpa-ultrasound man ko tas nay nakit-an sa akong doctor kanang sintomas sa bato sa akong gall bladder bantug di nako pa-imnon ug mga ing-ana. Around 6:00 in the evening, after doing prayer, Patient X will have her dinner of rice and paksiw. Patient X verbalized, Dili gid ko hilig mukaon ug manok, isda ug karne ra jud na.Also every after meal, Patient
X washes her hands. She often goes to bed by 9 after watching Willtime Bigtime. Patient X doesnt use electric fan or air conditioner when going to sleep. Patient X usually takes a bath thrice a week. Tigulang na biya ko tas tugnawon sad ko, as verbalized by Patient X. According to her, she usually changes clothes every time she is perspiring especially on the neck area but she changes her underwear every day. She often changes three times a day. Katulo pud ko sa isa ka-adlaw mag-toothbrush oi after asking if she is brushing her teeth. Patient X usually urinates 5 times a day and sometimes she wakes up about 4 times just to urinate in the evening. Usahay dili na gane ko ka-ihi sa akong arinola kay di naman nako mapugngan ug maka-ihi na lang ko sa akong panty. According to her, the color of her urine is light yellow. Patient X said that she defecates twice or thrice a week. Hilig man gid mi ug saging na tondan, makatobol biya na, as verbalized by Patient X. She often goes to church every Sunday and sometimes every Friday if she feels alright. According to Patient X, she doesnt smoke but her husband often smokes and can consume up to 1 pack of cigarettes a day. Also, she doesnt drink coffee and alcoholic beverages. She drinks milk twice a day. MENSTRUAL AND OBSTETRIC HISTORY Patient X was 13 years old when she had her menarche. According to her, it lasted for about 3 to 4 days. Dili man ko layagan. Patient X used extra pieces of cloth as her sanitary napkin since she experience having rashes when using sanitary pads. Di pud ko magsuot ug panty pagmatulog ko arung washout tanan ang akong dugo. Patient X doesnt encounter any pains during her monthly period. When Patient X was 21 years old, she had her first pregnancy. According to her, she often visited health centers to have prenatal check-ups and have her immunizations. She gave birth to 11 children via Normal spontaneous vaginal delivery (G11, P11OO8). 1O of them were aided by a mananabang in their house and the youngest was aided by a midwife in the health center. According to her, it was her fifth child that she was able to deliver a large baby that weighs 8 lbs. Patient X delivered a baby with the following years 1957, 1958, 1960, 1961, 1963, 1965, 1967, 1968, 1971, 1972 and 1974. Kaluoy sa Diyos wala man pud ko nakuhaan. She was 48 years old when she entered the menopausal stage. FAMILY HISTORY Patient Xs mother has a history of Diabetes Mellitus and uterine prolapse. Her mother died at the age of 76. Also in her mothers side, they have a history of hypertension. Patient Xs brother died of Diabetes Mellitus due to the wound on his buttocks. On the other hand Patient Xs father had gout arthritis. Her father died at the age of 86. Namatay man ako tatay sa katiguwangan, as verbalized by Patient X. Both of her parents were heavy smokers. Grabe man kaayo to manigarilyo akong mga ginikanan, as verbalized by Patient X. PAST MEDICAL HISTORY During the interview, upon asking about her immunization status, she verbalized Kumpleto man ko ug bakuna na nadawat. Patient X experienced the common childhood diseases such as sore eyes and mumps. She also had cough, colds and fever. Every time she had these illnesses, she usually take over the-counter drugs such as Tuseran and Biogesic to relieve the existing condition. Also, Patient X drinks herbal decoction from the leaves of sayote, tuba2x, gabon and yerba buena and go to a certain albularyo to relieve the illness felt. According to Patient X, she has allergy to feldine. Para man to sa akong arthritis, tas pagtumar nako mura kog gi-dapaw na nagpula-pula akong nawong ug kamot. After that incident, the doctor discontinued the medicine and changed it into Diclofenac. According to Patient X, she is taking Nifedipine constantly since she was diagnosed to have high blood pressure that reached to as high as 180/100 mmHg. Upon asking, the patient verbalized that she has enlargement of the heart based on her previous chest x-ray from Butuan Medical Center and she went to Manila to have her heart examined but failed to present the result due to its loss. She had no known allergies to any food. Patient X has been in and out of the hospital due to illnesses and accident. Upon asking about the exact date and time, Patient X verbalized, Kalimot najud ko kung kanus-a to basta naospital nako
kapila. Basta ang ako lang nadumduman adtong 2004 na-slide ko tapos gidala ko sa Butuan Doctors Hospital tapos nakit-an nga naa koy fracture sa spinal cord, dili jud ko kalakaw adto mga isa kabulan ug tunga. Two years ago according to Patient X, she verbalized that Niguwa sa akong puerta ang akong matris tas gi-tan-aw sa doctor sa DOA sa Cabadbaran, iyang gi-repair tas iyang gi-tulod tas gitahi. Upon asking about all of the datas whereabouts, Patient X verbalized Ambot day kung aha nato, nangawala naman to. PRESENT HEALTH HISTORY It was two weeks ago that she first noticed presence of vaginal bleeding. According to Patient X, Naglaba man ko ato gikan tas akong gi-hayhay ang mga sanina sa terrace, unya nagsaka panaog man ko ato sa terrace, natingala na dayun ko ato na murag naay mugawas-sulod sa akong puerta. Pagtanaw nako sa akong panty nay dugo na nigawas. After the incident, Patient X told no one especially her husband that she was having bleeding. Patient X verbalized Ang nigawas sa ako na dugo kay baho, wala pud ko nag-gamit ug napkin. Unya hinay-hinay na sakit akong pus-on kadugayan kay ni ngutngut na. Nagsakit sad akong bat-ang, as verbalized by Patient X. A day after, her daughter from Manila called her to know if they were doing okay with Mr. Y and it was the time that Patient X told her daughter that there is something wrong with her and that she was thinking that her uterus was moving in and out of her vagina, so her daughter decided that she should be brought to the hospital. When her daughter arrived from Manila, she was immediately rushed to Butuan Medical Center. She stayed there for almost 3 days. She was diagnosed to have uterine prolapse. But then, her doctor, Dr. R alongside with Dr. D told her that she should be transferred to M. J. Santos Hospital for cardiac monitoring during the surgery. Though bleeding was still noted, she was discharged from the hospital. By Saturday and Sunday, she stayed in their house for a while since she missed their house at that time. Gimingaw man jud ko ato sa among balay bantug gi-ingnan nako si (name of her daughter) na mapauli sa mi tas inig ka lunes nako muadto sa Santos. It was August 22, 2011 at around 4 in the afternoon when Patient X was brought to the Emergency room due to vaginal bleeding. She was seen and examined by Dr. D with admitting diagnosis of Uterine Prolapse 3rd degree with the following vital signs of Temp- 36. 2 oC, BP- 120/80 mmHg, CR- 94 bpm, RR- 21 bpm, O2sat- 94%. On the same day, Patient X was admitted with the doctors order as follows: TPR q 4 Hours, Inform Dr. G regarding the patient. With medications: Bisacodyl I tab po @hs x 2 doses
DRUGS NAME: Bisacodyl GENERIC NAME: Bisacodyl CLASSIFICATION: Laxatives MECHANISM OF ACTION: Stimulant laxative that increases peristalsis, probably by direct effect on smooth muscle of the intestine, by irritating the muscle or stimulating the colonic intramural plexus. Drug also promotes fluid accumulation in colon and small intestine. INDICATION: preparation for surgery CONTRAINDICATIONS: Contraindicated in patients hypersensitive to drug or its components and in those with rectal bleeding, gastroenteritis, intestinal obstruction, abdominal pain, nausea, vomiting, orother symptoms of appendicitis or acute surgical abdomen. SIDE EFFECTS/ TOXIC EFFECTS: Dizziness, abdominal cramps, vomiting, diarrhea, alkalosis, tetany NURSING CONSIDERATIONS: 1. Give drug at times that dont interfere with scheduled activities or sleep. Soft, formed stools are usually produced 15 to 60 minutes after rectal use. 2. Before giving for constipation, determine whether patient has adequate fluid intake, exercise and diet. 3. Advise patient to swallow enteric-coated tablet whole to avoid GI irritation. Instruct him not to take within1 hour of milk or antacid. 4. Advise patient to report adverse effects to prescriber.
5. Tables and suppositories are used together to clean the colon before and after surgery and before barium enema. Metronidazole 500mg BID
DRUGS NAME: Metronidazole GENERIC NAME: Metronidazole CLASSIFICATION: Antibiotic, Amebicide, Antiprotozoal MECHANISM OF ACTION: Undergoes intracellular chemical reduction during anaerobic metabolism. After metronidazole is reduced, it damages DNAs helical structure and breaks its strands, which inhibits bacterial nucleic acid synthesis and causes cell death. INDICATION: Trichomoniasis, Refractory trichomoniasis, Pelvic inflammatory disease, Bacterial Vaginosis CONTRAINDICATION: Breast-feeding, hypersensitivity to metronidazole or its components SIDE EFFECTS/ TOXIC EFFECTS: CNS: headache, seizures, fever, vertigo, dizziness, confusion, irritability, depression, weakness, insomnia CV: edema, flushing EENT: rhinitis, sinusitis GI: nausea, vomiting, abdominal cramping or pain, constipation, diarrhea, dry mouth GU: darkened urine, vaginitis, polyuria, dysuria, cystitis, dryness of vagina and vulva, genital puritus Musculoskeletal: transient joint pain Respiratory: upper respiratory tract infection Skin: rash NURSING CONSIDERATIONS: 1. If pt has adverse CNS reactions, such as seizures or peripheral neuropathy, tell prescriber and stop drug immediately. 2. Monitor pt with severe liver disease because slowed metronidazole metabolism may cause drug to accumulate in the body and increase the risk of adverse effects. 3. If skin irritation occurs, apply topical gel less frequently or discontinue it, as ordered. 4. Monitor CBC and culture and sensitivity test if therapy lasts longer than10 days or if second course of treatment is needed. 5. Caution patient to avoid alcohol while being treated with vaginal preparation. Conjugated Estrogen 0.625 mg 4 tabs TID to start now.
DRUGS NAME: Conjugate estrogen (Premarin) GENERIC NAME: Conjugated estrogens CLASSIFICATION: Estrogen MECHANISM OF ACTION: Increases synthesis of DNA, RNA, and protein in responsive tissues, also reduces release of follicle-stimulating and luteinizing hormones from the pituitary gland. INDICATION: Vulvar or vaginal atrophy, abnormal uterine bleeding (hormonal imbalance). CONTRAINDICATION: Contraindicated in pregnant patients and in patients with thrombophlebitis, thromboembolic disorders, estrogen-dependent neoplasia, breast or reproductive cancer (except for palliative treatment), or undiagnosed abnormal genital bleeding. SIDE EFFECTS/ TOXIC EFFECTS: CNS: dizziness, headache, stroke and seizure CV: edema, pulmonary embolism, MI GI: dyspepsia, GI pain, nausea, constipation or diarrhea, flatulence, peptic ulceration and vomiting GU: renal failure Hematologic: decreased platelet adhesion, prolonged bleeding time Skin: diaphoresis, pruritus, rash GI: nausea, vomiting, abdominal cramping, bloating, increased appetite EENT: worsening myopia or astigmatism GU: breakthrough bleeding, amenorrhea, altered cervical secretion Hepatic: cholestatis jaundice Skin: melasma, chloasma, hairloss, dermatitis Metabolic: weight changes, hypercalcemia
Other: breast tenderness changes in libido NURSING CONSIDERATIONS: 1. Periodically monitor lipid levels, blood pressure, body weight, and hepatic function. 2. Glucose tolerance may be impaired. Monitor glucose level closely in patients with diabetes. 3. If pt has adverse CNS reactions tell prescriber and stop drug immediately. 4. Tell diabetic patient to report elevated glucose level so that antidiabetic dosage can be adjusted. 5. Encourage patient to stop smoking because of the risk of CV complications
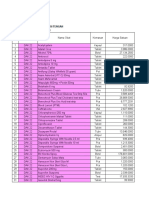
-With CBC Serum now. LABORATORY RESULT HEMATOLOGY -branch of medicine concerned with the nature, function, and diseases of the blood. It covers the cellular and serum composition of blood, the coagulation process, blood-cell formation, hemoglobin synthesis, and disorders of all these. Date Taken: August 22, 2011 4:40 pm CBC TEST Hemoglobin DEFINITION NORMAL 117-140 RESULT 126 UNIT g/L INTERPRETATION Normal. IMPLICATION
Hemoglobin is the protein molecule in red blood cells that carries oxygen from the lungs to the body's tissues and returns carbon dioxide from the tissues to the lungs. Hematocrit The hematocrit or packed cell volume (PCV) is the percentage of blood volume that is occupied by red blood cells. WBC White blood cells or leukocytes are cells of the immune system involved in defending the body against both infectious disease and foreign materials. DIFFERENTIAL COUNT Segmenters Segmenters (segmented neutrophils, or just segs) are one of the types of neutrophils, which are the most common type of white blood cells. Most mature neutrophils.ead more Lymphocytes Lymphocytes are small white blood cells that plays a large role in defending the body against disease. They are
0.34-0.44
0.38
Normal.
5.0-15.0
6.50
X 10^9/L
Normal.
0.37-0.72
0.40
Normal.
0.20-0.50
0.34
Normal.
Band
responsible for immune responses. Less mature neutrophils.
0.02-0.05
0.00
Decreased.
Eusinophil
Monocyte
Basophil
Platelets
Eosinophils are associated with antigen-antibody reactions. Monocytes are the body's natural reaction to infection or inflammation. Basophils are phagocytes and contain heparin, histamines, and serotonin. Platelets are irregularlyshaped, colorless bodies that are present in blood. Their sticky surface lets them, along with other substances, form clots to stop bleeding.
0.00-0.06
0.14
Increased.
Signifies immunosuppr ession. Indicates allergic reactions.
0.08-0.14
0.12
Normal.
0-0.01
0.00
Normal.
150-390
168
X 10^9/L
Normal.
Blood Type: O+
On the same day, Dr. G ordered the following: Thank you for referring this patient for evaluating prior to surgery; she has Hypertensive CardioVascular Disorder not in failure. She may undergo the contemplated surgery with high risk for Perioperative complication; I will do intra-op cardiac monitoring. Please inform me once admitted. It was 5 pm that she was transferred in the surgical ward awake and coherent, without IVF, with scanty vaginal bleeding. It was 7: 20 pm that Dr. G ordered: Thank you for the referral may have full, low salt, low fat diet. Continue meds (pts stock). Zinnat 500 mg I tab BID (D4)
DRUGS NAME: Zinnat GENERIC NAME: Cefuroxime Sodium CLASSIFICATION: Cephalosporins MECHANISM OF ACTIONS: Second-generation cephalosporins that inhibitscell-wall synthesis, promoting osmotic instability; usually bactericidal. INDICATION: treatment of infections caused by sensitive bacteria CONTRAINDICATION: Sensitivity to cephalosporins and related antibiotics; pregnancy (category B), lactation. SIDE EFFECTS/ TOXIC EFFECTS: CV: phlebitis, thrombophlebitis GI: diarrhea, nausea, anorexia, vomiting Hematologic: hemolytic anemia Skin: maculopapular and erythematous rashes, urticaria, pain, induration, sterile abscesses, temperature elevation Other: hypersensitivity reaction, serum reaction NURSING CONSIDERATION: 1. Monitor patient for signs symptoms of superinfection. 2. Determine history of hypersensitivity reactions to cephalosporins, penicillins, and history of allergies, particularly to drugs, before therapy is initiated. 3. Report onset of loose stools or diarrhea. Although pseudomembranous colitis.
4. Monitor I&O rates and pattern: Especially important in severely ill patients receiving high doses. Report any significant changes. 5. Tell patient to take drug as prescribed, even after he or she feels better. Adalat GITS 30 mg 1 tab OD OK
DRUGS NAME: Adalat GITS GENERIC NAME: Nifedipine CLASSIFICATION: Calcium channel blocker MECHANISM OF ACTION: Thought to inhibit calcium ion influx across cardiac and smooth-muscle cells, decreasing contractility and oxygen demand. Also may dilate coronary arteries and arteriole. INDICATION: Hypertension CONTRAINDICATION: Contraindicated in patients with bronchial asthma, sinus bradycardia and greater than first-degree heart block, cardiogenic shock, and overt heart failure. SIDE EFFECTS/ TOXIC EFFECTS: CNS: dizziness, light headedness, headache, weakness, syncope, nervousness CV: flushing peripheral, edema, heart failure, MI, hypotension, palpitations EENT: nasal congestion GI: nausea, diarrhea, constipation, abdominal discomfort Musculoskeletal: muscle cramps Respiratory: dyspnea, pulmonary edema, cough Skin: rash, pruritus NURSING CONSIDERATIONS: 1. Monitor Blood pressure and heart rate regularly, especially in patients who take beta-blockers or antihypertensives. 2. Watch for symptoms of heart failure. 3. Monitor blood sugar in diabetic patients. Nifedipine has diabetogenic properties. 4. Encourage patient to stop smoking while taking the nifedipine. 5. Observe 10 rights in giving the drugs. BP norm 10 mg tab OD
DRUGS NAME: BP norm GENERIC NAME: Fosinopril Sodium CLASSIFICATION: ACE inhibitor, Antihpertensives MECHANISM OF ACTION: May inhibit ACE, preventing conversion of angiotensin I to angiotensin II, a potent vasoconstrictor. Less angiotensin II decreases peripheral arterial resistance, thus decreasing aldosterone secretion, which reduces sodium and water retention and lowers blood pressure. INDICATION:Hypertension and Heart failure CONTRAINDICATION: Contraindicated in patients hypersensitive to drug or other ACE inhibors and in breast-feeding women. SIDE EFFECTS/ TOXIC EFFECTS: CNS: dizziness, stroke, headache fatigue, paresthesia, sleep disturbance CV: MI, chest pain, angina pectoris, rhythm disturbance, palpitations, hypotension, orthostatic hypotension EENT: tinnitus, sinusitis GI: pancreatitis, nausea, vomiting, diarrhea, dry mouth, abdominal distention and pain, constipation GU: sexual dysfunction, renal insufficiency, hepatitis Metabolic: Hypercalemia Musculoskeletal: musculoskeletal pain Respiratory: dry, persistent, tickling, non-productive cough, bronchospasm Skin: Urticaria, rash, photosensitivity reactions, pruritus Other: angioedema, decrease libido, gout NURSING CONSIDERATIONS: 1. Monitor Blood Pressure for drug effects.
2. Monitor Potassium intake and potassium level. Diabetic patients, those with impaired renal function, and those receiving drugs that can increase potassium level may develop hyperkalemia. 3. Assess renal and hepatic function before and periodically throughout therapy. 4. Tell patient to avoid salt substitutes; these products may contain potation, which can cause high potassium level in patients taking drug. 5. Instruct patient to call prescriber if he develops easy bruising or bleeding; swelling of tongue, lips, face, eyes, mucous membranes, arms, or legs; difficulty swallowing or breathing; and hoarseness. Lipitor 80 mg tab OD pc dinner
DRUGS NAME: Lipitor GENERIC NAME: Atorvastatin calcium CLASSIFICATION: HMG-CoA reductase inhibitor, Antilipemics MECHANISM OF ACTION: Inhibits HMG-CoA reductase, and early(rate-limiting) step in cholesterol biosynthesis. INDICATION: In patients with clinically evident coronary heart disease, to reduce the risk of nonfatal MI, fatal and nonfatal strokes, angina, heart failure, and revascularization procedures To reduce the risk of MI, stroke, angina, or revascularization procedures in patient with multiple risk factors for CAD but who dont yet have the disease. Adjunct to diet to reduce LDL, total cholesterol, apolipropotein B, and triglyceride levels and to increase HDL levels in patients with primary hypercholesterolemia and mixed dyslipidemia; adjunct to diet to reduce triglyceride level; primary dysbetalipoproteinemia in patients who dont respond adequately to diet. Alone or as an adjunct to lipid-lowering treatments, such as LDL apheresis, to reduce total and LDL Cholesterol in patients with homozygous familial hypercholesterolemia Heterozygous familial hypercholesterolemia CONTRAINDICATION: Contraindicated in patients hypersensitive to drug and in those with active liver disease or unexplained persistent elevations of transaminase levels. Contraindicated in pregnant and breastfeeding women and in women of child-bearing age. SIDE EFFECTS/ TOXIC EFFECTS: CNS: headache, asthenia, insomnia CV: peripheral edema EENT: Pharyngitis, Rhinitis, Sinusitis GI: Abdominal Pain, Constipation, Diarrhea, dyspepsia, flatulence, nausea GU: UTI NURSING CONSIDERATIONS: 1. Patient should follow a standard cholesterol-lowering diet before and during therapy. 2. Before treatment, assess patient for underlying causes for hypercholesterolemia and obtain a baseline lipid profile. Obtain periodic liver function test result and lipid levels before starting treatment and at 6 and 12 weeks after initiation, of after an increase in dosage and periodically thereafter 3. Drug may be given as a single dose at any time of day, with or without food. 4. Advise patient to inform prescriber of adverse reactions, such as muscle pain, malaise, and fever. 5. Warn patient to avoid alcohol. Please give Hydroxyzine (Iterax)25 mg I tab po now
DRUGS NAME: Iterax GENERIC NAME: Hydroxyzine diHCL CLASSIFICATION: Piperazine derivative MECHANISM OF ACTION: A piperazine antihistamine whose action may result from suppression of activity in certain essential regions of the subcortical area of the CNS.
INDICATION: Anxiety, Preoperative and Postoperative adjunctive therapy for sedation, pruritus, Psychiatric and emotional emergencies, including acute alcoholism, nausea and vomiting (excluding nausea and vomiting of pregnancy), Antepartum and post partum adjunctive therapy. CONTRAINDICATION: Contraindicated in patients hypersensitive to drug, early pregnancy; hypersensitivity to hydroxyzine or cetirizine and breast feeding women. SIDE EFFECTS/ TOXIC EFFECTS: CNS: drowsiness, involuntary motor activity GI: dry mouth, constipation SKIN: Pain at I.M. injection site OTHER: Hypersensitivity reactions NURSING CONSIDERATIONS: 1. If patient takes other CNS drugs, watch for oversedation 2. Elderly patient maybe more sensitive to adverse anticholinergic effects; monitor these patients for dizziness, excessive sedation, confusion, hypotension, and syncope. 3. Warn patient to avoid hazardous activities that require alertness and good coordination until effects of drug are known. 4. Tell patient to avoid alcohol while taking drug. 5. Warn woman of childbearing age to avoid use during pregnancy and breastfeeding.
It was August 23, 2011, 9:30 am Dr. G had the following order: Will do intra-operative cardiac monitoring, Please inform me once scheduled for OR. On that day, vaginal bleeding was not noted. She was without IVF. On the same day Dr. G ordered: Continue po meds, for vaginal hysterectomy once re-evaluation of uterus is okay for surgery, most likely 8/26/11 5:30, consent. August 24, 2011 with the order to continue po meds. August 25, 2011, 4:30 in the morning, the Dr. D ordered: D/C Zinnat when stocks are consumed. Also the doctor ordered: schedule for Vaginal Hysterectomy + AP Colporrhaphy in 8/27/11, 8 am, Secure signed consent, Inform OR/ Dr. A, secure 1 u whole blood pts blood type, segment only xmatching. It was on August 25, 2011 at around 9:00 am that we first met our client. We decided to have Patient X as our client for the Grand PAR presentation. She was handled by one of our group mates. She was lying on bed, awake and coherent without IVF with initial vital signs taken and recorded as follows: Temp-36 degree C, PR- 110 bpm, RR-24 bpm and BP- 120/70 mmHg. Patient was observed to have tremors in the hand and feet. Also, Patient X was unable to stand unassisted and needs assistance on positioning. Also on this day Patient X verbalized that Di sa ko maglakaw-lakaw day kay murag nanghupoy akong tiil ug kamot. The problem identified was Activity Intolerance (Level 1). Care was rendered. Patient X was able to participate in passive Range of Motion such as Flexing and extending upper and lower extremity. Deep breathing exercise and partial self care activity such as combing hair and oral care was demonstrated. Latest vital signs were taken and recorded with Temp36.3 degree C ,PR- 82 bpm, RR- 20 bpm and BP- 120/70 mmHg. Another problem was also identified, it was Impaired Skin Integrity. Patient X was observed to have limited range of motion, slowed movement and redness and rashes on inguinal area. Patient X was noted to use sanitary pad daily.
Interventions were done. Patient X kept her clothes dry and frequently washes the area with mild soap every time she changed her sanitary pad. Also she prevents herself from scratching the area and applied chamomile powder. August 26, 2011 at around 9:45 am the Dr. G ordered: pls. inform me once pt is transferred to OR. NPO post midnight, Start IVF with D5NSS 1 L @ 6 am x KVO. Also, the doctor ordered: X- ray of thoracolumbar spine (APL), please have x-rays read this pm, relay result, history of Spinal cord Injury with Fracture of Spine 2004, Date Taken: August 26, 2011 Radiology Department X-Ray Section X-rays are a form of electromagnetic radiation, just like visible light. In a health care setting, a machine sends individual x-ray particles through the body. A computer or special film is used to record the images that are created. A thoracic spine x-ray is an x-ray of the twelve chest (thoracic) vertebrae. The vertebrae are separated by flat pads of cartilage that cushion them. Interpretation Thoraco- Lumbar Spine AP/Lateral There is flattening of L1 and L3 vertebral bodies producing kyphotic deformity at the thoracolumbar junction. There is narrowing of T12-L1 and L1-L2 intervertebral discal spaces. Minimal to moderate osteophytic formations are seen along the margins of vertebral endplates. There is diffuse osteopenia of the spine with associated biconcave configuration of the rest of the vertebral bodies. Pedicles appear intact. Negative for paravertebral soft tissue masses. Included sacroiliac and hip joints are intact bilaterally. Impression: 1. Minimal to moderate hypertrophic degenerative disease of the spine. 2. Compression fractures of L1 and L3 vertebral bodies. 3. Diffuse osteopenia of the spine likely secondary to osteoporosis. It was August 26, 2011 that we had our interview and assessment at around 1:30 p.m. We received Patient X lying flat on bed, awake and without IVF with the vital signs of: Temp- 36.2 oC, PR119 bpm, RR- 25 bpm ,O2 sat-98%, BP- 110/70 mmHg. Patient X verbalized Nakulbaan naman ko mahitungod aning muabutay na operasyon. Patient X was cold to touch and observed to have hand tremors. She had reduced interaction to people and environment. The problem identified was Anxiety (Moderate). Care was rendered. Provided comfort measures by allowing patient to assume in a comfortable position. Encouraged to do deep breathing exercise. Patient X was able to listen and talk to the student nurse assigned. Latest vital signs were taken and recorded with BP- 110/70 mmHg, PR- 99 bpm, RR- 20 bpm. Patient X verbalized Wala na kaayo ko nakulbaan karon. The problems identified in the Pre-Operative phase were Anxiety (Moderate), Activity Intolerance (Level 1) and Impaired Skin Integrity. August 27, 2011, 8:00 am, Dr. D ordered: Fleet enema, now.
It was on August 27, 2011, 8:40 in the morning that Patient X was wheeled into the Operating area from the ward via wheelchair, awake and coherent with # 1 D5NSS I liter at the level of 900 cc at KVO rate attached to right metacarpal vein with initial vital signs taken as follows: BP- 142/88, HR-94, RR-20, Oxygen saturation-98%.Pre-operative diagnosis was Uterine prolapse 3rd degree with marked cystocele and rectocele. Patient X was transferred into a stretcher in a supine position and was wheeled inside the Operating room # 1 and transferred to the OR table at around 8:50 am. Then, a cardiac monitor was attached to her chest and a nasal cannula with the rate of 2L/min. It was 10:00 am prior to the operation, Patient X requested that they will have a rosary together with the surgical team. At 10:25 am, Patient X was positioned on sidelying then Bupivacaine 8% was inducted.
DRUGS NAME: Bupivacaine hydrochloride GENERIC NAME: Bupivacaine hydrochloride CLASSIFICATION: amide type local anaesthetic INDICATION: production of local or regional anesthesia or analgesia for surgery procedures COMMON SIDE EFFECTS: Mild dizziness or drowsiness Nausea and vomiting NURSING CONSIDERATIONS: 1. Patients should be informed in advance that they may experience temporary loss of sensation and motor activity, usually in the lower half of the body following proper administration of caudal or lumbar epidural anesthesia. 2. Inform the patient before using this medication, to tell his/her doctor or pharmacist of all prescription and nonprescription/herbal products he/she may use. 3. Do not start or stop any medicine without doctor or pharmacist approval. After that, she was positioned on lithotomy, perineal preparation was done. Operation started on vaginal hysterectomy started at 10:46 am. At around 11:30 am, a catheter was inserted. 11:41 am, the uterus was out. IV was consumed and followed up by #2 D5LR 1 L @ 30 gtt/min at 11:58 am. Patient X was complaining of pain on her abdomen so the anesthesiologist ordered for Ketamine 1 ml.
DRUGS NAME: Ketamine GENERIC NAME: Ketamine HCl CLASSIFICATION: Dissociative anesthetic, hallucinogen, psychotomimetic MECHANISM OF ACTION: Ketamine has been shown to block afferent impulses associated with the affective-emotional component of pain perception within the medical medullary reticular formation, to suppress spinal cord activity, and to interact with several central nervous system (CNS) transmitter systems. Ketamine blocks the NMDA glutamate receptor by a dual mechanism, blocking both the closed channel from the aqueous phase and the closed channel from the membrane phase. INDICATION: Anesthetic agent for diagnostic and surgical procedures that do not require skeletal muscle relaxation. CONTRAINDICATION: Patients in whom significant BP elevation would be a serious hazard; hypersensitivity to the drug. COMMON SIDE EFFECTS: Blurred vision, confusion, drowsiness, increased or decreased blood pressure or heart rate Mental status changes, nausea, vomiting NURSING CONSIDERATIONS: 1. Monitor circulatory and respiratory status 2. Assess the blood pressure of the patient before the administration.
3. Theophylline should not be coadministered with ketamine, it may interact and can cause unpredictable seizure. 4. Because of rapid induction following the initial IV injection, the patient should be in a supported position during administration. 5. Rapid administration may result in respiratory depression and enhanced pressor response It was injected via IV at around 12:00 noon. By 12:30 pm, Patient X complained again for pain so another Ketamine was injected by the circulating nurse. It was on 12:50 pm that Patient X was given another set of Ketamine since she was complaining of pain again. The operation ended at about 1:06 p.m. By 1:08 pm, the operation for AP Colporrhaphy started and ended at 1:45 p.m. After the operation, vital signs were BP- 138/ 82 mmHg, PR- 78 bpm, RR- 20 bpm, O2Sat- 98%. Epidural anesthesia (medazolam) was inducted.
DRUGS NAME: Dormicum GENERIC NAME: midazolam hydrochloride CLASSIFICATION:benzodiazepine MECHANISM OF ACTION: May potentiate the effects of GABA, depress the CNS, and suppress the spread of seizure activity. INDICATION: Sedation in Premed before surgical or diagnostic procedures, induction and maintenance of anesthesia. CONTRAINDICATION: Contraindicated in patients hypersensitive to drug and in those with acute angleclosure glaucoma, shock, coma, or acute alcohol intoxication. SIDE EFFECTS/ TOXIC EFFECTS: Nausea, vomiting,headache, hiccoughs, laryngospasm, dyspnea hallucination, drowsiness, amnesic episode. NURSING CONSIDERATIONS: 1. Have oxygen and resuscitation equipment available in case of severe respiratory depression. 2. Monitor blood pressure, heart rate and rhythm, respirations, airway integrity, and arterial oxygen saturation during procedure. 3. Use cautiously in patients with uncompensated acute illness and in elderly or debilitated patients. 4. Because drug diminishes patients recall of events around the time of surgery, provide written information, family member instructions, and follow-up contact. 5. Warn patient to avoid hazardous activities that require alertness of good coordination until effects of drug are known. Patient X was transferred into the Recovery room at around 2:05 in the afternoon, semiunconscious with the IV Level of 850 cc with the urine output of 1500 ml. At about 2:15, skin test was done for pain medication which was Dynastat. During the operation, the problem identified was Risk for Deficient Fluid Volume deficit. Patient was observed to have poor skin turgor, irritable and skin was dry. Interventions were made by noting changes in vital signs, limiting the movement by ensuring restraints and assisting in suctioning fluids. Another problem was identified; it was Risk for Imbalanced Body Temperature. Patient was seen to have hand tremors, chilling, fluctuating temperature in the monitor and was exposed to cold environment. Interventions were done. Monitored the body temperature, kept patients skin as dry as possible and maintained a comfortable environment by regulating the air conditions thermostat. Patient X was able to maintain a body temperature. The problems identified in the Intra-operative phase were Risk for Deficient Fluid volume and Risk for Imbalanced Body Temperature.
Post operative orders were made, Dr. A ordered Patient X transferred to PACU x 2 hours, v/s q 15 minutes, encourage deep breathing, flat on bed x 6 hours, IVF D5LR 1 L X 30 gtts, IVF to follow Plain NSS 1L x 30 gtts, DAT, I/O hourly and to refer. With the following medications Cefuroxime (Zegen) 750 mg IVTT q 8H ANST
DRUGS NAME: Cefuroxime (Zegen) GENERIC NAME: Cefuroxime Sodium CLASSIFICATION: Second-generation cephalosporin, Pregnancy risk category B GENERIC NAME: Cefuroxime Sodium CLASSIFICATION: Cephalosporins MECHANISM OF ACTIONS: Second-generation cephalosporins that inhibitscell-wall synthesis, promoting osmotic instability; usually bactericidal. INDICATION: treatment of infections caused by sensitive bacteria CONTRAINDICATION: Sensitivity to cephalosporins and related antibiotics; pregnancy (category B), lactation. SIDE EFFECTS/ TOXIC EFFECTS: CV: phlebitis, thrombophlebitis GI: diarrhea, nausea, anorexia, vomiting Hematologic: hemolytic anemia Skin: maculopapular and erythematous rashes, urticaria, pain, induration, sterile abscesses, temperature elevation Other: hypersensitivity reaction, serum reaction NURSING CONSIDERATION: 1. Monitor patient for signs symptoms of superinfection. 2. Determine history of hypersensitivity reactions to cephalosporins, penicillins, and history of allergies, particularly to drugs, before therapy is initiated. 3. Report onset of loose stools or diarrhea. Although pseudomembranous colitis. 4. Monitor I&O rates and patter: Especially important in severely ill patients receiving high doses. Report any significant changes. 5. Tell patient to take drug as prescribed, even after he or she feels better. Parecoxib (Dynastat) 40 mg IVTT now
DRUGS NAME: Parecoxib (Dynastat) GENERIC NAME: Parecoxib Na CLASSIFICATION: Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) MECHANISM OF ACTION: By inhibition of both peripheral and central COX-2, valdecoxib reduces the production of prostaglandins that are important medicators of pain and inflammation. INDICATION: Short term treatment of acute pain and postop pain. CONTRAINDICATION: Contraindicated in patients with known hypersensitivity to parecoxib sodium, valdecoxib or to any other ingredient of the product. It should not be given to patients who have experienced asthma. Contraindicated in patients who have demonstrated allergic-type reactions to sulfonamides. SIDE EFFECTS/ TOXIC EFFECTS: Postop anemia, Hypokalemia, agitation, insomnia, hypoesthesia, HTN, Hypotension, Paryngitis, respitarory insufficiency, alveolar osteitis, dyspepsia, flatulence, pruritis, back pain, arthralgia, oliguria, paripheralm edema, increase blood creatinine. NURSING CONSIDERATIONS: 1. Monitor for signs of hypersensitivity. 2. Observe 10 rights in giving the drugs. 3. Monitor vital signs. 4. Assess renal function of the patient. 5. NSAIDs may mask signs and symptoms of infection because of their antipyretic and antiinflammatory actions.
Nalbuphine (Nubain) 5 mg slow IV q 6H x 4 doses then PRN for pain next due at 6 pm
DRUGS NAME: Nalbuphine (Nubain) GENERIC NAME: Nalbuphine HCl CLASSIFICATION: Opioid Analgesics MECHANISM OF ACTION: Binds with opiate receptors in the CNS, altering perception of and emotional response to pain. INDICATION: Relief of moderate to severe pain; Preoperative analgesia, anesthesia adjunct, obstetric analgesia. CONTRAINDICATION: Contraindicated in patients hypersensitive to drug SIDE EFFECTS/ TOXIC EFFECTS: Sedation Infrequently sweating, GI upsets, Vertigo, Dizziness Dry mouth Headache, allergic reactions NURSING CONSIDERATIONS: 1. Reassess patients level of pain at least 15 to 30 minutes after parenteral administration. 2. Drug acts as an opioid antagonist and may cause withdrawal syndrome. For patients who have received long-term opioids, give 25% of the usual dose initially. 3. Drug causes respiratory depression produced by 10mg of morphine. 4. Monitor circulatory and respiratory status and bladder and bowel function. If respirations are shallow or rate is below 12 breaths/ minute, withhold dose and notify prescriber. 5. Caution ambulatory patient about getting out of bed or walking. Warn outpatient to avoid driving and other hazardous activities that require mental alertness until drugs CNS effects are known. August 27, 2011 at 3:30 in the afternoon, Dr. A ordered: 1 vaginal OS to be removed tomorrow 8/28/11 at 6 am c/o NOD. It was 9:00 in the evening that Dr. D ordered: Ketorolac 30 mg slow IV now ANST then 15 mg slow IV q 6H x 2 doses.
DRUGS NAME: Ketorolac GENERIC NAME: Ketorolac tromethamine CLASSIFICATION: NSAID, Pregnancy Risk Category C; D in 3rd trimester INDICATION: Short-term management of moderate severe, acute pain for single and multiple-dose treatment ADVERSE REACTION: CNS: dizziness, headache, drowsiness, sedation CV: edema, hypertension, palpitation GI: dyspepsia, GI pain, nausea, constipation or diarrhea, flatulence, peptic ulceration and vomiting GU: renal failure Hematologic: decreased platelet adhesion, prolonged bleeding time Skin: diaphoresis, prurotus, rash NURSING CONSIDERATION: 1. Correct hypovolemia before giving 2. NSAIDs may increase the risk of serius thrombotic events, MI, or stoke,which can be fatal. The risk may be greater with longer use or in patients with CV disease or risk factors for CV disease. 3. Carefully observe patients with coagulopathies and those taking anticoagulants. Drug inhibits platelet aggregation and can prolong bleeding time. This effect disappears within 48 hours of stopping drug and doesnt alter platelet count, INR, PTT, or PT. On August 28,2011 , Dr. D ordered the following: decrease IVF Rate to 25 gtts/min once on diet, encourage fluid intake, Incorporate biomix @present IVF and last dose of cefuroxime (Zegen) 750 mg @12 nn (08/28/11).
DRUGS NAME: Biomix GENERIC NAME: AMINO ACIDS + B-COMPLEX + TAURINE + DEXTROSE t CLASSIFICATION: Parenteral Nutritional Products INDICATION: Nutritional supplement CONTRAINDICATION: Hypersensitivity With new medication ordered: Paracetamol 500 mg TID.
DRUGS NAME: Acetaminophen GENERIC NAME: Paracetamol CLASSIFICATION: para-aminophenol derivative, Pregnancy risk category B INDICATION: Mild pain or Fever ADVERSE REACTION: Hematologic: hemolytic anemia, leucopenia, neutropenia, pancytopenia Hepatic: Jaundice Metabolic: hypoglycemia Skin: rash, urticaria NURSING CONSIDERATION: 1. Many OTC and prascription products contain acetaminophen; be aware of this when calculating total daily dose. 2. Observe any signs of adverse reaction. 3. Observe 10 rights in giving the drugs. At around 10:45 in the morning, Dr. G ordered: Plain NSS I L + 1 amp Biomix @25 gtts/min. It was 11:30 am that the doctor ordered to encourage deep breathing exercises 5x q 30 mins while awake, to revise Fosinopril (BP norm) 10 mg tab OD and with medication of Lipitor 80 mg tab OD pc dinner. Hemoglobin determination, release blood at the laboratory if Hgb > 10 g Date Taken: August 28, 2011 10:48 am HEMATOLOGY TEST DEFINITION NORMAL RESULT UNIT INTERPRETATION IMPLICATION
Hemoglobin
Hemoglobin is the protein molecule in red blood cells that carries oxygen from the lungs to the body's tissues and returns carbon dioxide from the tissues to the lungs.
117-140
119
g/L
Normal.
On the same day, Dr. G ordered for Perilight/Perineal care BID. Also IVF TWC, Zegen IVTT to D/C once IVF is terminated then shift to po 500 BID to start in am post breakfast. With medications of Clindamycin 150 mg TID po OK
GENERIC NAME: Clindamycin Hydrochloride CLASSIFICATION: Lincomycin derivative, Antibiotic, anti-infectives MECHANISM OF ACTION: Inhibits bacterial proten synthesis by binding to 50S subunit of ribosome. Hinders or kills susceptible bacteria.
INDICATION: Infections caused by sensitive staphylococci, streptococci, and other sensitive aerobic and anaerobic organism CONTRAINDICATION: Contraindicated in patients hypersensitive to drug or lincomycin. SIDE EFFECTS/ TOXIC EFFECTS: CV: thrombophlebitis GI: nausea, abdominal pain, diarrhea, vomiting Skin: rashes Others: anaphylaxis NURSING CONSIDERATIONS: 1. Take each dose with a full glass of water (decreases esophageal irritations). 2. May be taken without regard for meals. 3. Monitor BP and pulse after administration. 4. Complete full course of therapy. 5. Instruct patient to notify prescriber of adverse reactions (especially diarrhea). Warn him/her not to treat such diarrhea himself/herself because clindamycin therapy may cause severe, even lifethreatening, colitis.
Disflatyl I tab TID X 3 doses and D/C.
DRUGS NAME: Disflatyl GENERIC NAME: Dimethicone/Simethicone CLASSIFICATION: Antacids, adsorbents, and antiflatulents MECHANISM OF ACTION: By its defoaming action, drug disperses or prevents formation of mucussurrounded gas pockets in the GI tract. INDICATION: accumulation of gases in the gastrointestinal tract, flatulence, functional gastric bloating CONTRAINDICATION: Contraindicated in patients hypersensitive to drug. SIDE EFFECTS/ TOXIC EFFECTS: Bleching, flatus NURSING CONSIDERATIONS: 1. Drug doesnt prevent gas formation 2. Tell patient to chew tablet before swallowing. 3. Advise patient that changing positions often and walking will help pass flatus. 4. Dont confuse simethicon with cimetidine. 5. Observe 10 rights in giving the medication. During the visit to the client at around 10:00 am, we received patient sitting on bed with moderate high back rest. Vital signs were taken and recorded with BP- 110/70 mmHg, PR- 74 bpm, RR25 bpm. Patient X verbalized Agaka lang ko kay mag-adto ko ug C.R. kay maglisud pa ko ug lakaw kay tungod ani akong tahi. Patient X was observed to have difficulty turning. She manifested limited range of motion and slowed movement. Also, she was seen to have postural instability. The problem identified during the day was Impaired Physical Mobility (Level 2). After identifying the problem, the patient was encouraged to have recreational activity such as watching TV at the watchers area. The patient was seen sitting up on bed and frequently turned position. On this day, another problem was also identified it was Acute Pain. Patient X was observed to have facial grimace and guarding behavior on the sutured area. Ang kasakit kay naa sa 9 sa numero nga imung giingon, as verbalized by Patient X.
Interventions were made. Patient X was able to demonstrate deep breathing exercise and have adequate rest periods. Naa pa may sakit pero gamay na lang, mga 3 base sa imung giingon nga 10 ang pinakasakit unya 0 ang walay sakit, as verbalized by Patient X. Latest vital signs were BP- 110/70 mmHg, PR- 73 bpm, RR- 19 bpm. On the same day, the problem identified was Risk for Infection. According to her daughter who is a nurse, swelling, redness and moisture noted on the sutured area. Patient X was on diaper at that time. Patient X refused to show the vaginal area to the student nurse. Care was rendered. Instructed client to do hand washing and stressed the importance of preventing infection at the area. Patent X was able to demonstrate techniques to prevent infection as evidenced by hand washing and maintain a clean and free environment. The problems identified in the Post-operative phase were Acute Pain, Impaired Physical Mobility (Level 2) and Risk for infection. On August 29, 2011, Dr. G ordered: hold BP norm, pls. refer for BP > 140/90 mmHg and with new medication: Omeprazole (Omepron) 20 mg i cap BID.
DRUGS NAME: Omepron GENERIC NAME: Omeprazole CLASSIFICATION: Antiulcer drugs MECHANISM OF ACTION: Inhibits activity of acid (proton) pump and binds to hydrogen-potassium ATP at secretory surface of gastric parietal cells to block formation of gastric acid. INDICATION: Short term treatment for gastric ulcer CONTRAINDICATION: Contraindicated with hypersensitivity to omeprazole or its components. Use cautiously with pregnancy, lactation. SIDE EFFECTS/ TOXIC EFFECTS: CNS: dizziness, headache GI: abdominal pain, constipation, diarrhea, flatulence, nausea, vomiting Musculoskeletal: back pain Respiratory: cough, upper respiratory tract infection. Skin: rash NURSING CONSIDERATIONS: 1. Amoxicillin may trigger anaphylaxis in patients with a history of penicillin hypersensitivity. 2. Tell the patient to swallow tablets or capsules whole and not to open, crush, or chew them. 3. Administer before meals. 4. Evaluate for therapeutic response like relief of Gastrointestinal symptoms. 5. Report severe headache, worsening of symptoms, fever, chills. It was on August 30, 2011, Dr. G ordered the following: continue other po meds and Hepato Billiary Tree ultrasound. Date Taken: August 30, 2011 Radiology Department Utrasound Section Ultrasound is an examination that uses high-frequency sound waves to look at organs and structures inside the body. During an ultrasound test, a special technician or doctor moves a device called a transducer over part of your body. The transducer sends out sound waves, which bounce off the tissues inside your body. The transducer also captures the waves that bounce back. Images are created from these sound waves.
Interpretation Upper Abdomen Sonogram The liver is unenlarged exhibiting diffuse increased parenchymal echogenicity with coarsened and heterogenous echotexture. Contour is wavy to irregular. No focal mass lesions are seen. The intrahepatic ducts as well as the common bile duct as non-dilated. The gall bladder measures 9.12 x 3.84 cm. It contains numerous tiny to small reflective echoes layering on the dependent portion, the largest measures 0.77 cm. Gallbladder walls appear smooth and not thickened. The common bile duct measures 0.65 cm. The pancreas and spleen are normal in size and both show homogenous parenchymal echotexture. Both kidneys are within normal in size and parenchymal echogenicity. Contour is fairly smooth bilaterally. Corticomedullary differentiation is fairly delineated. Right kidney measures 9.67 x 4.13 x 4.34 cm with cortical thickness of 1.17 cm. Left kidney measures 9.93 x 4.19 x 4.83 with cortical thickness of 1 .13 cm. Renal parenchymal echotexture is homogenous. Both pelveocaliceal systems are non-dilated. No lithiasis is noted bilaterally. Impression: 1. Diffuse liver parenchymal disease suggestive of cirrhosis. 2. Distended gall bladder containing numerous tiny to small calculi as described. 3. Unremarkable sonogram of the pancreas, spleen and both kidneys. 4. Non-dilated biliary tree. At around 8: 20 pm Dr. G ordered to hold Adalat Gits. On the following day, August 31, 2011 at around 3:30 in the afternoon Dr. G ordered to suggest surgical consult if okay with Dr. D and also to decrease Lipitor to 20 mg I tab OD pc dinner. It was 3:50 pm when the doctor ordered to refer Patient X to Dr. R for surgical consult. On the same day, Dr. D orders were: Thank you very much for referring Patient X and will schedule Patient on with later date probably in 5 months time. Also Dr. D ordered for daily perineal flushing. On September 1, 2011 Dr. G ordered to continue po meds and with new medication to give, Tramadol 500 mg for 6H PRN thereafter.
DRUGS NAME: Tramadol GENERIC NAME: Tramadol Hydrochloride CLASSIFICATION: Opiods analgesics MECHANISM OF ACTIONS: Binds to opiate receptors in the CNS causing inhibition of ascending pain pathways, altering the perception of and response to pain; also inhibits there uptake of norepinephrine and serotonin, which also modifies the ascending pain pathway. INDICATION: moderate to moderately severe pain CONTRAINDICATION: Hypersensitivity to tramadol, opiods, or any component of the formulation; opioddependent patients; acute intoxication with alcohol, hypnotics, centrally-acting analgesics, opiods, or psychotropic drugs. SIDE EFFECTS/ TOXIC EFFECTS: Dizziness. Headache, confusion, sleep disorder, vasodilation, urinary frequency, nausea, vomiting, flatulence, respiratory depression, rash, diaphoresis NURSING CONSIDERATIONS: 1. Monitor CV and respiratory status. 2. Reassess patients level of pain at least 30 minutes after administration. 3. For better analgesic effect, give drug before onset of intense pain. 4. Take with meals if upset stomach occurs. 5. If pt has adverse reactions tell prescriber and stop drug immediately. During this day, we had our duty and one of my group mates was able to handle Patient X. At around 9:00 in the morning, Patient X was lying on bed awake and coherent without IVF. Initial vital
signs were taken and recorded with Temp- 36.4 degree C, RR- 20, PR- 78 and BP-110/70 mmHg. Also with Foley Bag Catheter attached to urobag draining at 80 ml. Care was rendered. Patient X was seen and examined by AP with orders carried out. With latest vital signs of BP- 110/70, Temp- 36.3 degree C, RR-20 bpm, HR- 73 bpm and O2 sat- 97%. It was September 2, 2011 at around 9:50 am Dr. G ordered to resume Fosinopril (BP Norm) 10 mg tab OD. On the same day, there was an order to clamp catheter for 2H then release 30 minutes thereafter and to do self perineal care BID. On this day we had our duty and we are able to interact and handle our client. We received Patient X sitting on bed without IVF with initial vital signs taken and recorded with Temp- 36 degree C, RR- 18 bpm, PR- 80 bpm and BP- 130/90 mmHg. With Foley Bag catheter attached to urobag draining at 120 ml. Care was rendered. Patient X was seen and examined by Dr. G with orders carried out. Latest vital signs were Temp- 36 degree C, RR- 22 bpm, PR- 25 bpm and BP- 110/ 70 mmHg. At around 10:00 p.m Dr. D ordered to unclamp foley catheter. On September 3, 2011 at around 12 noon, Dr. D ordered: Pull out Foley bag catheter, now. Please inform if able to void after 2 hours. With medications of Buscopan 1 tab q 8 hrs prn for abdominal pain
DRUGS NAME: Buscopan GENERIC NAME: Hyoscine ButyleBromide CLASSIFICATION: Anticholinergics MECHANISM OF ACTION: Inhibits muscarinic actions of acetylcholine on autonomic effectors innervated by postganglionic cholinergic neurons. May effect neural pathways originating in the inner ear to inhibit nausea and vomiting. INDICATION: spasm. Irritable bowel syndrome CONTRAINDICATION: Contraindicated in patients with angleclosure glaucoma, obstructive uropathy, obstructivedisease of the GI tract, asthma, chronic pulmonary disease, myasthenia gravis, paralyticileus, intestinal atony, unstable CV status in acute hemorrhage, tachycardia from cardiacinsufficiency, or toxic megacolon. Contraindicated in patients with hypersensitive to belladonna or barbiturates. SIDE EFFECTS/ TOXIC EFFECTS: Constipation, dry mouth, trouble urinating, or nausea, rash, dizziness, diarrhea, NURSING CONSIDERATIONS: 1. Instruct patient to remove one patch before applying another 2. Instruct patient to wash and dry hands thoroughly before and after applying the transdermal patch (on dry skin behind the ear) and before touching the eye because pupil may dilate. Tell patient to discard patch after removing it and to wash application site thoroughly. 3. Tell patient that if patch becomes displaced, he should remove it and apply another patchon a fresh skin site behind the ear. 4. Alert patient to possible withdrawal signs or symptoms (nausea, vomiting, headache,dizziness) when transdermal system is used for longer than 72 hours. 5. Urge patient to report urinary hesitancy or urine retention. MVT + Iron (Sorbifer) 500mg I cap OD.
DRUGS NAME: Sorbifer GENERIC NAME: Multivitamins + iron CLASSIFICATION: Multivitamins MECHANISM OF ACTION: Essential for promoting growth, health, vitality, life, general well being, necessary for metabolic processes responsible for transforming foods into energy or tissue; formation and maintenance of red blood cells, chemical supporting the nervous system, hormones and genetic material. Provides elemental iron an essential component in the formation of hemoglobin. INDICATION: Iron deficiency, Treatment and prevention of vitamin deficiencies. CONTRAINDICATION: Hypersensitivity to preservative, colorants or additives, including tartrazine, saccharin, and aspartame. SIDE EFFECTS/ TOXIC EFFECTS:
Allergic reactions to preservatives, additives or colorants. NURSING CONSIDERATIONS: 1. Assess patient for signs of nutrition deficiency prior to and throughout the therapy. 2. Instruct to notify side effects of medications to physician. 3. Encourage to comply on medications. 4. Encourage patient to comply with physicians recommendations. Explain that the best source of vitamins is a well balanced diet with foods forms the 4 basic food groups. 5. Advise patients not to refer to chewable multivitamins for children as candy. It was September 4, 2011, Dr. D ordered: May go home tomorrow if okay with Dr. G., Continue self perineal care BID @ home, to continue Zegen and clindamycin @ home x 4 days, to come back on 9/10/11 @my clinic, kindly give all her due meds for the whole day prior to discharge. At around 12 noon, Dr. G ordered: okay for discharge, with meds BP norm 10 mg tab OD, Lipitor 40 mg tab OD, ASA EC 80 mg 1 tab OD, MVT with iron I cap OD, Buscopan 1 tab TID prn for abdominal pain, advised and for follow-up 9/11/11. The patient was still in for about 1 day after the doctor ordered for home per request for reasons that they were settling their account. The patients chart was billed and account settled. It was September 5, 2011, Patient X was discharged with final diagnosis of Uterine Prolapse 3rd degree marked Cystocele 3rd degree and Rectocele 3rd degree.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- This Study Resource Was: Head-To - Toe Assessment Documentation SampleDocument2 pagesThis Study Resource Was: Head-To - Toe Assessment Documentation SampleA Sung100% (3)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Strategic Considerations in Treatment Planning Deciding When To Treat, Extract, or Replace A Questionable Tooth PDFDocument12 pagesStrategic Considerations in Treatment Planning Deciding When To Treat, Extract, or Replace A Questionable Tooth PDFItzel Marquez100% (1)
- UCSD Internal Medicine Handbook 2011Document142 pagesUCSD Internal Medicine Handbook 2011ak100007100% (5)
- Sample Sba Questions GynaecologyDocument6 pagesSample Sba Questions GynaecologyIshola Segun SamuelPas encore d'évaluation
- Pediatrics MCQs - DR Ranjan Singh - Part 2Document10 pagesPediatrics MCQs - DR Ranjan Singh - Part 2k sagarPas encore d'évaluation
- Comparison of Hemorrhoid Sclerotherapy Using Glucose 50% vs. Phenol in Olive OilDocument4 pagesComparison of Hemorrhoid Sclerotherapy Using Glucose 50% vs. Phenol in Olive OilGabrielEnricoPangarianPas encore d'évaluation
- Patient Safety and The Informed ConsentDocument13 pagesPatient Safety and The Informed ConsentPatricia Elena ManaliliPas encore d'évaluation
- Treatment of Dengue Joe de LiveraDocument11 pagesTreatment of Dengue Joe de Liverakrishna2205100% (1)
- Case No 37Document5 pagesCase No 37Aila GoliasPas encore d'évaluation
- Pharm 451-Historical Development of Chemotherapy 2021Document22 pagesPharm 451-Historical Development of Chemotherapy 2021Akowuah SamuelPas encore d'évaluation
- Scientific Programme Isnacc 2017Document11 pagesScientific Programme Isnacc 2017sujithra RameshPas encore d'évaluation
- Laporan Perencanaan Perbekalan FarmasiDocument11 pagesLaporan Perencanaan Perbekalan FarmasikarinaPas encore d'évaluation
- Microbiology - Exercise 3e AntibiogramDocument5 pagesMicrobiology - Exercise 3e Antibiogramapi-253346521Pas encore d'évaluation
- The Evolving Role of Midwives As Laborists: Original ReviewDocument8 pagesThe Evolving Role of Midwives As Laborists: Original Reviewmnazri98Pas encore d'évaluation
- EVC Isquemico AHADocument52 pagesEVC Isquemico AHAalejandromagno1984Pas encore d'évaluation
- Components of Physical FitnessDocument4 pagesComponents of Physical FitnessTj CabacunganPas encore d'évaluation
- Surgical ICU Exam Content OutlineDocument6 pagesSurgical ICU Exam Content OutlineDarren DawkinsPas encore d'évaluation
- Pathophysiology of Tinnitus and Evidence-Based Options For Tinnitus ManagementDocument12 pagesPathophysiology of Tinnitus and Evidence-Based Options For Tinnitus ManagementEli HuertaPas encore d'évaluation
- Name of The Medicinal Product: Novaminsulfon Abz 500 MG/ML TropfenDocument8 pagesName of The Medicinal Product: Novaminsulfon Abz 500 MG/ML TropfenRiriPas encore d'évaluation
- Hematocrit (HCT) (Packed Cell Volume PCV) : Objectives: ToDocument19 pagesHematocrit (HCT) (Packed Cell Volume PCV) : Objectives: ToRamadan PhysiologyPas encore d'évaluation
- Type 2 Diabetes MellitusDocument4 pagesType 2 Diabetes MellitusMazhar WarisPas encore d'évaluation
- Test Bank For Medical Terminology For Health Professions 8th Edition by EhrlichDocument13 pagesTest Bank For Medical Terminology For Health Professions 8th Edition by Ehrlichuriquanofg00Pas encore d'évaluation
- LEUKEMIA, MPDs & MDSsDocument11 pagesLEUKEMIA, MPDs & MDSsMary Kaye Yvonne OtillaPas encore d'évaluation
- Effect of Nonsurgical Periodontal Therapy. I. Moderately Advanced Periodontitis. Badersten A, Nilvéus R, Egelberg J. J Clin Periodontol. 1981 Feb8 (1) 57 72 PDFDocument17 pagesEffect of Nonsurgical Periodontal Therapy. I. Moderately Advanced Periodontitis. Badersten A, Nilvéus R, Egelberg J. J Clin Periodontol. 1981 Feb8 (1) 57 72 PDFMashal AmirPas encore d'évaluation
- Chronic Bronchitis and EmphesemaDocument2 pagesChronic Bronchitis and Emphesemanursing concept maps100% (2)
- Acetaminophen Poisoning Cases - SeptiDocument15 pagesAcetaminophen Poisoning Cases - SeptiseptianasptrPas encore d'évaluation
- Redcord Medical Active Sport - v3 - 2013Document12 pagesRedcord Medical Active Sport - v3 - 2013Sang Ah YooPas encore d'évaluation
- Therapeutic UltrasoundDocument18 pagesTherapeutic UltrasoundPhysio Ebook100% (1)
- Manual of Obstetrics, 8e (Jun 25, 2014) - (1451186770) - (LWW) PDFDocument766 pagesManual of Obstetrics, 8e (Jun 25, 2014) - (1451186770) - (LWW) PDFPrem100% (9)
- Puskesmas: Modo Kecamatan: Bukal Kab/Kota: Buol Propinsi: Sulawesi Tengah Bulan: JanuariDocument42 pagesPuskesmas: Modo Kecamatan: Bukal Kab/Kota: Buol Propinsi: Sulawesi Tengah Bulan: JanuariFransiskaPas encore d'évaluation