Académique Documents
Professionnel Documents
Culture Documents
Episiotomy
Transféré par
Karla Katrina CajigalDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Episiotomy
Transféré par
Karla Katrina CajigalDroits d'auteur :
Formats disponibles
RESEARCH AND EDUCATION
Effectivness of cooling gel pads and ice packs on perineal pain
By Shahin Navvabi, Zahra Abedian and Mary Steen-Greaves
Abstract
This article reports the findings of a randomized controlled trial undertaken at the Hazrat Ommolbanin University Maternity Hospital in Mashhad, Iran, which investigated the effectiveness of localized cooling treatments to alleviate perineal trauma. From October 2005 to February 2006, 121 primiparous women who were at term and had an episiotomy were randomly recruited to one of three treatment groups (Group 1 no localized cooling; Group 2 Ice pack; Group 3 cooling gel pad). The intensity of pain, wound healing and womens satisfaction levels were the main outcomes measured. The intensity of pain was measured by a Numeric Rating Scale (NRS) (110) and wound healing was evaluated by the REEDA scale within 4 hours of episiotomy repair; at days 1, 2, 5 and 10. The use of oral analgesia was measured at day 10. Womens satisfaction levels with oral analgesia and localized cooling treatments were also assessed at day 10 by a NRS. There was evidence that localized cooling treatments are effective in alleviating perineal pain, which was in favour of the cooling gel pad group. A statistical significant difference was reported at 4 hours (P=0.003); day 2 (P=0.004); and at day 10 (P=0.044). At days 1 and 5 there was evidence of a reduction in the intensity of pain but this did not reach a statistical significant difference. A reduction in the use of oral analgesia was reported in favour of the cooling gel pad group (P<0.001). Womens satisfaction levels with oral analgesia were similar within the three treatment groups but a higher level of satisfaction when assessing localized treatment was reported by the cooling gel pad group (P<0.001). Wound healing rates were also reported to be better in the cooling gel pad group when compared to the other two groups (P<0.001). Womens views and treatments to alleviate perineal pain without any adverse affects on wound healing are important aspects of midwifery care. This trial has demonstrated evidence that localized cooling of the perineum reduces the intensity of pain. Women were more satisfied when applying cooling gel pads and this treatment appeared to assist in wound healing.
erineal pain following an episiotomy often has numerous negative consequences for many women and the associated pain can dominate the experience of early motherhood (Steen, 2001). It is important that there are treatments readily available to alleviate the associated pain and discomfort. It is also important that treatments will not have an adverse effect on healing and are acceptable to use by women. In Iran, the standard method of pain relief for perineal pain is oral analgesia, acetaminophen (paracetamol), and is given systemically. Localized cooling treatments are not commonly used. In 2005, midwifery researchers based in Mashhad Iran carried out a literature search on perineal pain relief methods and found articles describing and discussing the use of localized cooling treatments as a pain relief method for perineal trauma. This lead to contacting a midwifery researcher in the UK who had undertaken research and development work which involved the designing and laboratory testing of a maternity cooling gel pad (femepad) (Steen and Cooper, 1997; 1999) and investigating the effectiveness of this new treatment in two randomized controlled trials. (Steen et al, 2000; Steen and Marchant, 2001; 2007) This led to collaborative work and a further randomized controlled trial was undertaken to evaluate the effectiveness of two cooling treatments (ice pack and gel pad) and compare these with a no localized treatment regime (control) on intensity of perineal pain after episiotomy in primiparous women who gave birth at Hazrat Ommolbanin University Materity Hospital in Mashhad, Iran from October 2005 to February 2006.
Methods
The following hypothesis was tested: The use of a cooling gel pad is more effective at reducing intensity of perineal pain following a normal delivery aided by an episiotomy when compared with an ice pack or no localized treatment.
Ethical considerations
Ethical approval was given by the study hospitals ethics committee and the hospitals research governance recommendations were followed. An information leaflet about the study was distributed to women during pregnancy and further information was given following episiotomy repair by the researcher (SN). Participants informed consent was sought before being recruited.
Shahin Navvabi is Midwife and Researcher, Zahedan University of Medical Science Nursing and Midwifery, Mashhad Iran; Zahra Abedian is Supervisor, Mashhad University of Medical Science, Iran; Mary Steen-Greaves is Reader in Midwifery and Reproductive Health, Faculty of Health and Social Care, University of Chester Email: shahinnaviba@yahoo.com
Inclusion criteria
Participants had to meet the following inclusion criteria: n Iranian (Dewill Mashhad) nationality n Primparous n Age 1635 years
BRITISH JOURNAL OF MIDWIFERY, NOVEMBER 2009, VOL 17, NO 11
724
RESEARCH AND EDUCATION
Assessed for eligibility 2 October 20052 February 2006. Total births during trial period n=1274) Vaginal births with episiotomy n=884)
n n n n
Occiput anterior presentation Singleton birth Birth weight (25004000 g) Have addresses and telephone number.
Exclusion criteria
Women were excluded for any of the following reasons: n Woman with any medical disorders or obstetric complications n Fetal anomally n Stillbirth n Needing neonatal intensive care unit n Retained placenta n Smoking n Consumption of alcohol or continuous drugs n Rupture membranes >12 hours n Stretch or massage of perineum in pregnancy or during delivery stages n Use of lubricant during delivery n Second stage of delivery >120 minutes n Postpartum haemorrhage n Haematoma.
Randomized n=121)
Excluded n=763 Inclusion criteria not met n=500; refused to participate n=250; other reasons n=3
No treatment group n=40
Ice pack group n=40
Gel pad group n=41
Randomization
Lost to follow-up n=4 Discontinued intervention day 2 n=2 day 10 n=2 Lost to follow-up n=5 Discontinued intervention day 2 n=3 day 10 n=2 Lost to follow-up n=2 Discontinued intervention day 5 n=2
Analysed n=36
Analysed n=35
Analysed n=39
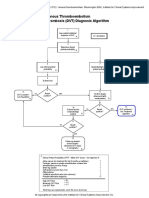
Figure 1. Flow chart to demonstrate process of the trial.
n n n n n
5 4 3 2 1 0
Term fetus (3742 weeks gestation) Normal delivery Lives with a partner Ability to read and write (Farsi) at 5th primary level Mediolateral episiotomy
Before analgesia After analgesia
Primiparous women (n=121) who were at term and had an episiotomy were randomly recruited to one of three treatment groups: n Group 1 No localized cooling n Group 2 Ice pack n Group 3 Cooling gel pad. Randomization was undertaken by a random number table. All particpants gave birth in the lithotomy position and were sutured with chromic catgut (routine in Iranian hospitals). Women received oral analgesia and the randomized localized treatment within 4 hours of episiotomy repair by researcher (SN), then self-adminstered pain relief based on their individual needs at home.
Outcome measures
The intensity of pain, wound healing, use of analgesia and womens satisfaction levels were the main outcomes measured. The intensity of pain was measured by a Numeric Rating Scale (NRS) (010) and wound healing was evaluated by the REEDA scale within 4 hours of episiotomy repair (baseline), at days 1, 2, 5 and 10. A descriptive scale known as the REEDA scale (Davidson, 1974) measuring five components associated with the healing process, graded 03 points, using direct measurement and observation, was used. The acronym REEDA is derived from five components that have been identified to be associated with the healing process. These are: redness, edema, ecchymosis, discharge and approximation of skin edges. Each category is assessed and a number assigned for a total REEDA score ranging from 015. The higher scores indicate increased tissue trauma. This tool appears to be the first systematic attempt to evaluate postpartum healing, which acknowledges the need for a standardized assessment tool independent of the severity of the perineal injury. The use of oral analgesia (acetaminophen) was measured at
BRITISH JOURNAL OF MIDWIFERY, NOVEMBER 2009, VOL 17, NO 11
Control
Ice pack
gel pad
Before analgesia use: ANOVA test: P=0.522 degrees of freedom=2 After analgesia use: K-W test: P=0.003 degrees of freedom=2
Figure 2. Comparison of mean score intensity of perineal pain during 4 hours after episiotomy
726
RESEARCH AND EDUCATION
day 10. Womens satisfaction levels with oral analgesia and localized cooling treatments were also assessed at day 10 by a NRS.
Table 1. Compare mean (standard deviation) intensity perineal pain after episiotomy
Test Day 1 P=0.429 3.96 Mean (ANOVA) Day 2 P=0.004 Mean (ANOVA) Day 5 P=0.056 Mean (ANOVA) Total Gel pad Icepack 4.07 3.84 2.11 2.97 2.29 2.8 1.91 2.33 3.83 1.94 3.17 1.70 Control 4.42 1.87 4.36 2.01 3.83 1.99 SD
Data analysis
Data were recorded on a coded questionnaire and analysed by descriptive and inferential statistical methods: chisquare; Kruskal Wallis (K-W); Mann-Whitney U; Jonckheere Trepstra. Analysis of variance (ANOVA) and exact tests were used with a SPSS software package.
2.11 3.66 2.08 3.26 1.91
SD
Findings
The flowchart (Figure 1) demonstrates the process women went through during the trial and shows the phases of a trial, as recommended by the CONSORT statement (Moher et al, 2001). Women were assessed for eligibility at the beginning of the trial and information is shown on the number of women recruited and then randomized to each of the three treatment groups. Loss to follow-up and discontinuation of intervention encountered during the trial period are highlighted and the final numbers included in the analysis are shown. There was evidence that localized cooling treatments are effective at alleviating perineal pain which was in favour of the cooling gel pad group. A statistical significant difference was reported at 4 hours (P=0.003) (Figure 2), day 2 (P=0.004) and at day 10 (P=0.044). At days 1 and 5 there was evidence of a reduction in the intensity of pain but this did not reach a statistical significant difference (Table 1). A reduction in the usage of oral analgesia was reported in favour of the cooling gel pad group (P<0.001) (Table 2). Womens satisfaction levels with oral analgesia were similar within the three treatment groups but a higher level of satisfaction when assessing localized treatment was reported by the cooling gel pad group (P<0.001). Wound healing rates were also reported to be better in the cooling gel pad group when compared to the other two groups (P<0.001) (Table 3).
SD
Table 2. Satisfaction with analgesia
Mean number of tablets (acetaminophen) in 3 groups during 10 days (K-W) Mean (SD) score satisfaction Mean oral analgesia (K-W) Mean (SD) score satisfaction Test P=0.001 Gel pad Icepack Control 8.33 12.84 17.22
P=0.089
5.17 2.13 9.05
6.22 2.10 7.65
5.86 2.47 SD
P=0.001
Table 3. Mean (standard deviation) REEDA score after episiotomy in 3 groups (Kruskal Wallis test)
4 Hours Day 1 Day 2 Day 5 Day 10 Test P=0.004 P=0.416 P=0.001 P=0.001 P=0.001 Gel pad 3.02 1.12 2.30 1.74 1.50 1.12 0.79 1.08 0.17 0.50 Icepack 2.57 1.50 2.17 1.41 1.70 1.20 1.61 1.18 0.80 1.2 Control 2.20 1.34 2.55 1.85 2.89 2.39 3.13 2.62 2.27 2.03 Mean SD Mean SD Mean SD Mean SD Mean SD
Discussion
Perineal trauma can involve injury to the labia, clitoris, urethra, vagina, perineal muscles and anal sphincters (Royal College of Obstetricians and Gynaecologists (RCOG), 2004) and is sometimes referred to as genital tract trauma (Steen, 2005). It can occur spontaneously during a vaginal birth, be caused by trauma during an instrumental delivery or by a surgical incision (episiotomy). The majority of women will sustain some degree of injury during childbirth and rates as high as 8595% have been reported (Albers, 2005). However, there is evidence that an episiotomy is more painful when compared with perineal tears and can take longer to heal (McGuiness et al; 1990 Sleep, 1990). Alleviating perineal pain, therefore, is vitally important for any woman who has sustained some form of injury, but especially for those women who have had an episiotomy performed. In the UK, a combination of systemic and localized treatments are used for pain relief to meet individual womens needs (Steen, 2005). Oral analgesia is the most common systemic method used while in hospital and is continued on the womans return to her own home (Steen and Marchant, 2007). Paracetamol is usually advised for mild to moderate perineal
BRITISH JOURNAL OF MIDWIFERY, NOVEMBER 2009, VOL 17, NO 11
pain (Moffatt et al, 2001). If a woman reports more severe pain then a combination of paracetamol and dextropoxephene (coproxomal) is sometimes offered, or an anti-inflammatory drug such as ibuprofen (brufen) (Sleep, 1990; Steen, 2002). Ice packs have been reported as a commonly used localized treatment to relieve perineal pain (Greenshields and Hulme, 1993; Steen and Cooper, 1998; Steen and Marchant, 2007) Ice bags were originally applied to the rectal region to alleviate haemorrhoidal pain and with the increase in episiotomy rates in the 1970s and 1980s, they became a popular method to alleviate perineal trauma (Rhodes and Barger, 1990). The application of ice packs to the perineum appears to give some short-term pain relief by numbing the superficial tissue surrounding the injury through its action on local nerve fibres (Hill, 1989; Steen and Cooper, 1998). In the 1990s, some concerns as to whether an ice pack can delay healing were voiced (Walker, 1990; Sleep, 1990; Grundy, 1997). Low and Reed (2000) and Palastanga (1994), however, have discussed
727
RESEARCH AND EDUCATION
in detail how the initial vasoconstriction, which is followed by a vasodilation, will increase circulation and promote healing. It has also been reported that ice application will effectively lower skin temperature only but the low conductivity of underlying subcutaneous fat tissue will prevent any cooling of deeper tissue (McMasters, 1977). A systematic review demonstrated that localized cooling treatments were effective at reducing perineal pain, swelling and bruising without any adverse effects on wound healing (Steen et al, 2006). Nevertheless, ice packs have been reported to cause some women unnecessary distress and discomfort; the hardness and rigidity, sharp corners and wet sensation make them unpleasant to use (Steen, 2005). For these reasons research and development work was undertaken to produce a specifically designed cooling maternity gel pad for women to use (Steen and Cooper, 1997; 1998; 1999). A randomized controlled trial undertaken in 19931994 demonstrated evidence that cooling gel pads were effective at reducing perineal oedema and pain within the first 48 hours of birth. Womens opinions demonstrated a preference for using cooling gel pad when compared to standard regimes, ice packs and epifoam (an anti-inflammatory steroid-based foam) (Steen et al, 2000). Another randomized controlled trial, alleviating perineal trauma (APT Study) was undertaken in 19981999 and this provided further evidence that cooling maternity gel pads were effective at reducing pain, swelling and bruising up to 2 weeks following birth with no adverse affects on healing. Womens views demonstrated a high level of satisfaction when using the new cooling gel pads when compared to ice packs and no localized treatment (Steen, 2002; Steen and Marchant, 2007). A recent Cochranes review assessed evidence from published and unpublished randomized and quasi-randomized trials (RCTs) that compared localized cooling treatment applied to the perineum with no treatment or other treatments applied to relieve pain related to perineal trauma
sustained during childbirth (East et al, 2007). This review reported limited evidence of the effectiveness of localized cooling treatments on perineal pain but highlighted that women preferred cooling gel pads when compared with icepacks and no localized treatments. This trial was not included in the review results and was recorded as an ongoing study. This trial, therefore, will need to be included in the next meta-analysis and updating of this review. Wound healing rates is also an important outcome measure (Steen, 2007) and will also need to be assessed in the next review. In Iran, before this trial, women who had an episiotomy were offered systemic pain relief in the form of oral analgesia, acetaminophen (paracetamol). Localized cooling treatments were not commonly used. The evidence reported from this trial first confirms the evidence reported in the two randomized controlled trials undertaken in the UK already mentioned and second, has provided evidence to support the use of localized cooling treatments to alleviate perineal pain in Iranian maternity hospitals. This trial has given Iranian women the opportunity for more effecitve pain relief.
Limitations
When undertaking any research there are always some limitations. It was impossible to blind the women as to what treatment they would be applying to their perineum. The difference in shape, size and texture of the cooling treatments and a clear no treatment group made informing the women unavoidable. The possiblility of researcher bias needs to be considered and while every attempt was made to blind the assessments, there is a possibility that the assessor may have become aware of some womens treatment allocation if women left these visible when the assessments were performed. Validated tools, however, were used by an experienced researcher and womens satisfaction with the treatment was sought. Nevertheless, there is always the possibility of the hawthorne effect, which is a form of reactivity whereby subjects improve an aspect
728
BRITISH JOURNAL OF MIDWIFERY, NOVEMBER 2009, VOL 17, NO 11
RESEARCH AND EDUCATION
of their behaviour being experimentally measured simply in response to the fact that they are being studied and not in response to any particular experimental manipulation. This is why it is important to measure several outcomes. All primiparous women in the three treatment groups had similar demographic characteristics and also had a routine episiotomy which was sutured with chromic catgut (routine care in Iranian maternity hospitals). While this assisted in a like-for-like critieria in their perineal managment and reduced potential bias in this trial, this approach is not based on the best available evidence and is based on traditional obstetric practices. There is evidence that routine episiotomy is not necessary and does not prevent perineal tears (Sleep, 1990). In addition, using chromic catgut can increase the intensity of pain and effect wound healing rates (Kettle and Johanson, 2004; Kettle et al, 2007). Vicryle rapide has been recommended as a better suture material to use (Kettle et al, 2002). Suturing technique and material, therefore, can significantly contribute to the severity of perineal pain. Research evidence that demonstrates the most beneficial suturing technique and material needs to be implemented into clinical practice. Since this trial, evidence to support changes in perineal management practices at the study hospital are being reviewed to update policies and procedures that are evidence based.
Key Points
n Perineal trauma can involve injury to the labia, clitoris, urethra, vagina, perineal muscles and anal sphincters. n There is evidence that an episiotomy is more painful when compared with perineal tears and can take longer to heal. n Perineal pain can dominate the experience of early motherhood. n Treatments to alleviate perineal pain without any adverse affects on wound healing is an important aspect of midwifery care. n Women were more satisfied when applying cooling gel pads and this treatment appeared to assist in wound healing.
material for perineal repair (Cochrane Review). In: The Cochrane Library, Issue 1, 2004. John Wiley and Sons, Chichester Kettle C, Hills RK, Jones P, Darby L, Gray R, Johanson RB (2002) Continuous versus interrupted perineal repair with standard or rapidly absorbed sutures after spontaneous vaginal births: a randomised controlled trial. Lancet 359: 221723 Low J, Reed A (2000) Electrotherapy Explained. Principles and Practice 3rd edn. Butterworth Heinemann, Oxford McGuiness M, Norr K, Nacion K (1991) Comparison between different perineal outcomes on tissue healing. J Nurse Midwifery 36(3): 1928 McMasters WC (1977) A literary review on ice therapy in injuries. Am J Sports Med 5(3): 1246 Moffatt H, Lavender T, Walkinshaw S (2001) Comparing administration of paracetamol for perineal pain. British Journal of Midwifery 9(11): 6904 Moher D, Schulz KF, Altman DA (2001) The consort statement: Revised recommendations for improving the quality of reports of parallel-group randomized trials. Lancet 357: 11914 Palastanga NP (1994) Heat and cold. In: Wells PE, Frampton V, Bowsher D, eds. Pain management by Physiotherapy 2nd edn. Butterworth Heinemann, Oxford RCOG (2004) Methods and Materials in Perineal Repair, Guideline no 23, RCOG, London Rhodes MA, Barger MK (1990) Perineal care: Then and now. J Nurse Midwifery 35(4): 22031 Sleep J (1990) Postnatal perineal care. In: MacMillan, eds. Midwifery practice: postnatal care. Alexander, Levy & Roch, London Steen MP (2001) Do we care enough about perineal wounds? British Journal of Midwifery 9(5): 31620 Steen MP (2002) A randomised controlled trial to evaluate the effectiveness of localised cooling treatments in alleviating perineal trauma: The APT Study, MIDIRS. Midwifery Digest 12(3): 3736 Steen MP (2005) I cant sit down. Easing genital tract trauma. British Journal of Midwifery 13(5): 3114 Steen M (2007) Perineal tears and episiotomy: how do wounds heal? British Journal of Midwifery 15(5): 2739 Steen M, Briggs M, King D (2006) Alleviating Postnatal Perineal Trauma. To cool or not to cool? British Journal of Midwifery 14(5): 3048 Steen MP, Cooper KJ (1997) A tool for assessing perineal trauma. J Wound Care 6(9): 4326 Steen MP, Cooper KJ (1998) Cold therapy and perineal wounds: Too cool or not too cool? British Journal of Midwifery 6(9): 5729 Steen MP, Cooper KJ (1999) A new device for the treatment of perineal wounds. J Wound Care 8(2): 8790 Steen MP, Cooper KJ, Marchant P, Griffiths-Jones M, Walker J (2000) A randomised controlled trial to compare the effectiveness of ice packs and Epifoam with cooling maternity gel pads at alleviating postnatal perineal trauma. Midwifery 16(1): 4855 Steen MP, Marchant PR (2001) Alleviating Perineal Trauma: the APT Study. RCM Midwives 4(8): 2569 Steen M, Marchant P (2007) Ice packs and cooling gel pads versus no localised treatment for relief of perineal pain: A randomised controlled trial. Evidence-Based Midwifery Journal 5(1): 1622 Walker P (1990) Episiotomy: issues for practice. Wound care. Nursing 4(15): 1822 Williams FLR, Florey C du V, Mires GJ, Ogston SA (1998) Episiotomy and perineal tears in low risk UK primigravidae. J Public Health Med 20: 4227
Conclusions
Treatments to alleviate perineal pain without any adverse affects on wound healing and womens views are important aspects of midwifery care. It appears that women gain some pain relief from systemic and localized approaches and these should be readily available throughout the world. This trial has demonstrated evidence that localized cooling of the perineum reduces the intensity of pain and cooling gel pads appear to be the most effective treatment. More women reported higher levels of satisfaction when using cooling gel pads to alleviate perineal pain and this localized treatment also appears to assist in wound healing. BJM
Acknowledgments Monireh Poorjava, Gynecologist and Habibollah Esmaeilli, Statistician Mashhad university of Medical science-Iran Albers LL, Sedler KD, Bedrick EJ, Teaf D, Peralta P (2005) Midwifery care measures in the second stage of Labor and reduction of genital tract trauma at birth: A randomized trial. J Midwifery Womens Health 50(5): 36572 Davidson NS (1974) REEDA: evaluating postpartum healing. J Nurse Midwifery 19: 68 East CE, Begg L, Henshall NE, Marchant P, Wallace K (2007) Local cooling for relieving pain from perineal trauma sustained during childbirth. Cochrane Database of Systematic Reviews 2007, Issue 4. Art. No.: CD006304. DOI: 10.1002/14651858.CD006304.pub2 Greenshields W, Hulme H (1993) The perineum in childbirth: a survey conducted by the National Childbirth Trust. NCT, London Grundy L (1997) The role of the midwife in perineal wound care following childbirth. Wound Care Clinic. Br J Nurs 6(10): 5848 Hill (1989) Effects of heat & cold on the perineum after episiotomy/laceration. J Obstet Gynecol Neonatal Nurs 18: 1249 Kettle C, Hills RK, Ismail KMK (2007) Continuous versus interrupted sutures for repair of episiotomy or second degree tears. Cochrane Database of Systematic Reviews. Issue 4. Art. No.: CD000947. DOI: 10.1002/14651858.CD000947.pub2 Kettle C, Johanson RB (2004) Absorbable synthetic versus catgut suture
BRITISH JOURNAL OF MIDWIFERY, NOVEMBER 2009, VOL 17, NO 11
729
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Psych Nursing Complete Edited Royal PentagonDocument32 pagesPsych Nursing Complete Edited Royal PentagonRichard Ines Valino100% (68)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Orthopedic EquipmentsDocument64 pagesOrthopedic EquipmentsJasmin Jacob100% (8)
- The Psychiatric Dimensions of Sleep Medicine2008, Vol.3, Issues 2, PDFDocument168 pagesThe Psychiatric Dimensions of Sleep Medicine2008, Vol.3, Issues 2, PDFRamon Alberto Portillo MedinaPas encore d'évaluation
- Manpower Planning FinalDocument108 pagesManpower Planning FinalDevi PrasannaPas encore d'évaluation
- Female Narration THE HOUSE OF THE SPIRITSDocument14 pagesFemale Narration THE HOUSE OF THE SPIRITSKarla Katrina CajigalPas encore d'évaluation
- Understanding Hemangiomas: Causes, Types and TreatmentsDocument18 pagesUnderstanding Hemangiomas: Causes, Types and Treatmentsplastic guardiansPas encore d'évaluation
- Plan de Nutritie in HipotiroidismDocument48 pagesPlan de Nutritie in Hipotiroidismalbinuta100% (1)
- The Paired T-Test: (A.K.A. Dependent Samples T-Test, or T-Test For Correlated Groups)Document22 pagesThe Paired T-Test: (A.K.A. Dependent Samples T-Test, or T-Test For Correlated Groups)Karla Katrina CajigalPas encore d'évaluation
- Emotion Modulation in PTSD: Clinical and Neurobiological Evidence For A Dissociative SubtypeDocument8 pagesEmotion Modulation in PTSD: Clinical and Neurobiological Evidence For A Dissociative SubtypeKarla Katrina CajigalPas encore d'évaluation
- Ch10 Nonexperimental and Quasi-Experimental StrategiesDocument17 pagesCh10 Nonexperimental and Quasi-Experimental StrategiesRadu GordanPas encore d'évaluation
- Introduction To Rizal Course: Lecture # 1Document7 pagesIntroduction To Rizal Course: Lecture # 1Karla Katrina CajigalPas encore d'évaluation
- Crit Care BiblioDocument9 pagesCrit Care BiblioKarla Katrina CajigalPas encore d'évaluation
- DermaDocument4 pagesDermaKarla Katrina CajigalPas encore d'évaluation
- The Bedside Oral Exam and The Barrow Oral Care ProtocolDocument2 pagesThe Bedside Oral Exam and The Barrow Oral Care ProtocolKarla Katrina CajigalPas encore d'évaluation
- Anabolic Steroids and Performance-Enhancing Substances TrainingDocument44 pagesAnabolic Steroids and Performance-Enhancing Substances TrainingKarla Katrina CajigalPas encore d'évaluation
- Death and Dying HandoutDocument3 pagesDeath and Dying HandoutKarla Katrina CajigalPas encore d'évaluation
- Death and Dying HandoutDocument3 pagesDeath and Dying HandoutKarla Katrina CajigalPas encore d'évaluation
- Common Behavioural Problems in Infants and Role of The NurseDocument8 pagesCommon Behavioural Problems in Infants and Role of The NurseKarla Katrina CajigalPas encore d'évaluation
- Statistic Probability ModelDocument5 pagesStatistic Probability ModelKarla Katrina CajigalPas encore d'évaluation
- Forces and Newton's Laws of MotionDocument59 pagesForces and Newton's Laws of Motionkristine_silangPas encore d'évaluation
- PBL 1Document6 pagesPBL 1Karla Katrina CajigalPas encore d'évaluation
- Cutnell PPT ch02Document46 pagesCutnell PPT ch02Karla Katrina CajigalPas encore d'évaluation
- Common Behavioural Problems in Infants and Role of The NurseDocument8 pagesCommon Behavioural Problems in Infants and Role of The NurseKarla Katrina Cajigal100% (1)
- Introduction and Mathematical ConceptsDocument39 pagesIntroduction and Mathematical ConceptsKarla Katrina CajigalPas encore d'évaluation
- Pathophysiology NCADocument1 pagePathophysiology NCAKarla Katrina CajigalPas encore d'évaluation
- 1 s2.0 S009042950101514X MainDocument5 pages1 s2.0 S009042950101514X MainKarla Katrina CajigalPas encore d'évaluation
- Why Is Exercise Important?: Article No. 1Document4 pagesWhy Is Exercise Important?: Article No. 1Eunice AgustinPas encore d'évaluation
- Part 3-ADocument153 pagesPart 3-ALy LyPas encore d'évaluation
- Questions PneumoniaDocument8 pagesQuestions PneumoniaMeliza BancolitaPas encore d'évaluation
- Aitc 2021Document2 pagesAitc 2021Jetbar Dolok SaribuPas encore d'évaluation
- WB CE Act Registration RegulationDocument42 pagesWB CE Act Registration RegulationDipak Ranjan MukherjeePas encore d'évaluation
- Tsca Toxic Substanteces Control ActDocument1 pageTsca Toxic Substanteces Control ActAlbert Casanova FernandezPas encore d'évaluation
- Nursing Student Cover LetterDocument8 pagesNursing Student Cover Letterafmrpaxgfqdkor100% (1)
- Systemic Ophthalmology Disorders GuideDocument4 pagesSystemic Ophthalmology Disorders GuideAslesa Wangpathi Pagehgiri100% (1)
- Venous Thromboembolism Deep Vein Thrombosis (DVT) Diagnosis AlgorithmDocument1 pageVenous Thromboembolism Deep Vein Thrombosis (DVT) Diagnosis AlgorithmImam Nur Alif KhusnudinPas encore d'évaluation
- Course Outline - PBH101Lab - Fall 2023Document5 pagesCourse Outline - PBH101Lab - Fall 2023Nusrat ShoshiPas encore d'évaluation
- Sepsis Fact SheetDocument4 pagesSepsis Fact SheetJoana MoreiraPas encore d'évaluation
- Jets Pay Payroll OfferDocument2 pagesJets Pay Payroll OfferMishra SanjayPas encore d'évaluation
- Assessing The Ears and Hearing Acuity: Return Demonstration Tool Evaluation ForDocument3 pagesAssessing The Ears and Hearing Acuity: Return Demonstration Tool Evaluation Forclint xavier odangoPas encore d'évaluation
- Final Project 3Document35 pagesFinal Project 3api-666429985Pas encore d'évaluation
- Herbal medicine: A guide to history, uses, and safetyDocument6 pagesHerbal medicine: A guide to history, uses, and safetyMprado DelgadoPas encore d'évaluation
- Essay 3 Final DraftDocument8 pagesEssay 3 Final Draftapi-270571146Pas encore d'évaluation
- Fever in Children With ChemoteraphyDocument23 pagesFever in Children With ChemoteraphyImanuel Far-FarPas encore d'évaluation
- EU Digital COVID Vaccine CertificateDocument2 pagesEU Digital COVID Vaccine Certificatekrasota izdoroviePas encore d'évaluation
- Registration Requirments of Animal Derived Non Medicated ProductsDocument2 pagesRegistration Requirments of Animal Derived Non Medicated ProductsValeria DumitrescuPas encore d'évaluation
- 2013 Sample Psychology Cover LettersDocument2 pages2013 Sample Psychology Cover LettersLavander Meggie100% (1)
- 2014 Windsor University Commencement Ceremony PROOFDocument28 pages2014 Windsor University Commencement Ceremony PROOFKeidren LewiPas encore d'évaluation
- Methods of Public RelationsDocument3 pagesMethods of Public RelationsAnusha Verghese100% (2)
- Pediculosis: Pubis (Pubic Louse)Document4 pagesPediculosis: Pubis (Pubic Louse)christian quiaoitPas encore d'évaluation
- RX MistakesDocument5 pagesRX MistakesSandeep Kumar SenguptaPas encore d'évaluation
- ADEC - Al Tharawat Private School 2016-2017Document19 pagesADEC - Al Tharawat Private School 2016-2017Edarabia.comPas encore d'évaluation
- Kumpulan Journal Kompartemen SindromDocument6 pagesKumpulan Journal Kompartemen SindromBrinna Anindita SatriaPas encore d'évaluation