Académique Documents
Professionnel Documents
Culture Documents
Assessment and MDG
Transféré par
Ma Rafaela Rosales PalomponDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Assessment and MDG
Transféré par
Ma Rafaela Rosales PalomponDroits d'auteur :
Formats disponibles
Bullets: NIGHTINGALE EDUCATIONAL REVIEW SYSTEM Millennium Development Goals (2015) The Millennium Development Goals (MDGs) are
eight international development goal s that 189 United Nations member states and at least 23 international organizations have ag reed to achieve by the year 2015. They include reducing extreme poverty, reducing child mortality r ates, fighting disease epidemics such as AIDS, and developing a global partnership for developm ent. In 2001, recognizing the need to assist impoverished nations more aggressively, UN member states adopted the targets. The MDGs aim to spur development by improving social and ec onomic conditions in the world's poorest countries. They derive from earlier international development targets, and were officially established at the Millennium Summit in 2000, where all world leaders present adopted the United Na tions Millennium Declaration, from which the eight goals were particularly promoted. Progress towards reaching the goals has been uneven. Some countries have achieve d many of the goals, while others are not on track to realize any. To accelerate progress towards the MDGs, the G-8 Finance Ministers met in London in June 2005 (in preparation for the G-8 Gleneagles Summit in July) and reached an agreement to provide enough funds to the World Bank, the IMF, and the African Development Bank (ADB) to cancel an additional $40-55 billion in debt owed by HIPC nations. This would allow impover ished countries to re-channel the resources saved from the forgiven debt to social programs for imp roving health and education and for alleviating poverty. Backed by G-8 funding, the World Bank, the IMF, and the ADB each endorsed the Gl eaneagles plan and implemented the Multilateral Debt Relief Initiative ("MDRI") to effectuate t he debt cancellations. The MDRI supplements HIPC by providing each country that reaches the HIPC comple tion point 100% forgiveness of its multilateral debt. Countries that previously reached the decision point became eligible for full debt forgiveness once their lending agency confirmed th at the countries had continued to maintain the reforms implemented during HIPC . Other countries that subsequently reach the completion point automatically receive full forgiveness of their multi lateral debt under MDRI. While the World Bank and ADB limit MDRI to countries that complete the HIPC prog ram, the IMF's MDRI eligibility criteria are slightly more expansive so as to comply with the I MF's unique "uniform treatment" requirement. Instead of limiting eligibility to HIPC countries, any c ountry with annual per capita income of $380 or less qualifies for MDRI debt cancellation. The IMF adop ted the $380 threshold because it closely approximates the countries eligible for HIPC. The Millennium Development Goals (MDGs) were developed out of the eight chapters
of the United Nations Millennium Declaration, signed in September 2000. The eight goals and 21 targets include 1. Eradicate extreme poverty and hunger o Halve, between 1990 and 2015, the proportion of people whose income is l ess than one dollar a day. o Achieve full and productive employment and decent work for all, includin g women and young people. o Halve, between 1990 and 2015, the proportion of people who suffer from h unger. 2. Achieve universal primary education o Ensure that, by 2015, children everywhere, boys and girls alike, will be able to complete a full course of primary schooling. 3. Promote gender equality and empower women o Eliminate gender disparity in primary and secondary education preferably by 2005, and at all levels by 2015. 4. Reduce child mortality o Reduce by two-thirds, between 1990 and 2015, the under-five mortality ra te. 5. Improve maternal health o Reduce by three quarters, between 1990 and 2015, the maternal mortality ratio. o Achieve, by 2015, universal access to reproductive health 6. Combat HIV/AIDS, malaria, and other diseases o Have halted by 2015 and begun to reverse the spread of HIV/AIDS. o Achieve, by 2010, universal access to treatment for HIV/AIDS for all tho se who need it. o Have halted by 2015 and begun to reverse the incidence of malaria and ot her major diseases. 7. Ensure environmental sustainability o Integrate the principles of sustainable development into country policie s and programmes; reverse loss of environmental resources. o Reduce biodiversity loss, achieving, by 2010, a significant reduction in the rate of loss. o Halve, by 2015, the proportion of people without sustainable access to s afe drinking water and basic sanitation (for more information see the entry on water supply). o By 2020, to have achieved a significant improvement in the lives of at l east 100 million slum-dwellers. 8. Develop a global partnership for development o Develop further an open trading and financial system that is rule-based, predictable and non-discriminatory. Includes a commitment to good governance, development and poverty reduction-nationally and internationally. o Address the special needs of the least developed countries. This include s tariff and quota free access for their exports; enhanced programme of debt relief for heavi ly indebted poor countries; and cancellation of official bilateral debt; and more g enerous
official development assistance for countries committed to poverty reduction. o Address the special needs of landlocked and small island developing Stat es. o Deal comprehensively with the debt problems of developing countries thro ugh national and international measures in order to make debt sustainable in the lon g term. o In cooperation with pharmaceutical companies, provide access to affordab le essential drugs in developing countries. o In cooperation with the private sector, make available the benefits of n ew technologies, especially information and communications. ***BASIC NURSING SKILLS REVIEW Assessing Heart Rate Overview _ Provides valuable data regarding the integrity of the cardiovascular system. _ The most common sites of heart rate measurement are the apical and radial puls es. _ Other sites include temporal, carotid, brachial, femoral, popliteal, posterior tibial, and pedal pulses. _ The pulse is assessed for rate, rhythm, strength, and equality Preparation _ Patient should be resting for measurement. _ Factors such as exercise, anxiety, pain, and postural change should be control led to obtain an accurate measurement of heart rate. _ Heart rate is affected by certain medications and disease processes. Special Considerations Pediatric Patients _ The most accurate site for pulse assessment in infants he apical site. _ Resting heart range for newborns ranges from 80 to 180 _ Children 1 to 3 years of age have a resting heart rate 140 beats per minute. Children 6 to 8 year olds have a resting heart rate that eats per minute. _ By 10 years of age, children have a resting heart rate 90 beats per minute. and small children is t beats per minute. that ranges from 80 to ranges from 75 to 120 b that ranges from 50 to
Elderly Patients _ The resting heart rate should range between 60 and 100 beats per minute in the healthy older adult. _ The healthy older adult has a normal cardiac rate and rhythm. _ Older adults with cardiovascular, pulmonary, or other chronic illnesses are at risk for rapid, slow, or irregular heart rate and rhythms, and their heart rates should be assessed with an apical pulse. Equipment _ Wristwatch with second hand or digital display _ Stethoscope (for apical heart rate)
_ Pen, pencil, and flow sheet or record form Procedure Radial Pulse Assessment ?Wash hands. Reduces transmission of microorganisms. ? Explain purpose and method of assessment to the patient. If the patient was recently active, wait 5 to 10 minutes. ( This relieves patien t anxiety and promotes cooperation. Activity and anxiety may increase patient's heart rate. ) ? Have the patient get into a sitting or supine position. > If in a supine position, place the patient's arm across lower chest with the wrist extended and palm down. > If sitting, bend patient's elbow 90 degrees and support the lo wer arm on a chair or your arm. Extend the patient's wrist with the palm down. Proper positioning of the ar m fully exposes the radial artery for palpation. ? Place the tips of the first two or three fingers of your hand over the groove along the radial or thumb side of the patient's inner wrist. The fingertips are the most sensitive parts o f the hand to palpate arterial pulsations. Avoid use of the thumb because it has pulsation and may int erfere with accuracy. ? Lightly compress your fingers against the radius, initially obliterate pulse, and then relax the pressure so that the pulse becomes easily palpable. The pulse is assessed more a ccurately with moderate pressure. Too much pressure occludes the pulse and impairs the blood fl ow. ? When the pulse can be felt regularly, use a watch's second hand or seconds ela psed display and begin to count the rate, starting with 0, then 1, etc. The rate is accurately de termined only after the assessor is certain that a pulse can be palpated. Timing should begin with 0 and the count of 1 is the first beat that is felt after the timing begins. ? If the pulse is regular, count for 30 seconds and multiply by 2. A 30-second p ulse check is the most accurate for rapid pulse rates. ? If the pulse is irregular, count for 1 full minute. Counting for a full minute ensures an accurate count. ? Assess regularity and frequency of any dysrhythmia. Inefficient contraction of the heart fails to transmit a pulse wave and can interfere with cardiac output. ? Determine the strength of the pulse. Note whether the thrust of the pulse agai nst the fingertips is bounding, strong,weak, or thready. The strength of the pulse reflects the volume of the blood that is
ejected against the arterial wall with each contraction of the heart. ? Assist patient to return to a comfortable position. Promotes comfort. ? Record characteristics of the pulse in the medical record or the flow sheet. R eport any abnormalities to the physician. This provides data for monitoring of changes in the patient's condition. Detection of abnormalities may determine the need for medical interve ntion. Apical Pulse Assessment ? Clean the earpieces and the diaphragm of the stethoscope with an alcohol swab. This controls the transmission of microorganisms when nurses share a stethoscope. ?Wash hands. This reduces the spread of microorganisms. ? Explain procedure to patient. If patient was recently active, wait 10 to 15 mi nutes before obtaining measurement. This relieves anxiety and promotes patient cooperation. Activity an d anxiety may increase the patient's heart rate. ? Close the room door and/or draw curtains around the patient's bed. This mainta ins patient privacy. ? With the patient in a supine or sitting position, remove patient's upper garme nts to expose the sternum and left side of the chest. This exposes the portion of the chest for se lection of the auscultatory site. ? Palpate the point of maximal impulse (PMI), located at the fifth intercostals space to the left of the sternum at the midclavicular line. The use of anatomic landmarks allows the corr ect placement of the stethoscope over the apex of the heart. This position enhances the ability t o hear heart sounds clearly. The PMI is located over the apex of the heart. ? Place the diaphragm of the stethoscope in the palm of your hand for 5 to 10 se conds. This warms the diaphragm and reduces the risk for startling the patient. ? Place the diaphragm of the stethoscope over the PMI, and auscultate for normal S1 and S2 (lub, dub) heart sounds. Heart sounds are the result of blood moving through the valve s of the heart. ? When S1 and S2 sounds are heard with regularity, observe the watch's second ha nd and count one sound (lub) for 30 seconds, then multiply the number by 2. An accurate rate is determined only after the nurse is able to clearly auscultate the sounds. ? If the heart rate is irregular or the patient is on cardiovascular medications , count for 1 full minute. The rate is determined more accurately when heard over a longer period. ? Replace patient's garments. Provides comfort and privacy to the patient.
? Record characteristics of the pulse on the flow sheet. Report any abnormalitie s to the physician. This provides data to monitor changes in the patient's condition. Abnormalities may require medical intervention. Apical-Radial Pulse Assessment (Two-nurse Technique) ? Explain the procedure to the patient. This decreases the patient's anxiety. ? Assist the patient into a supine position, and expose the chest area. This exp oses the portion of the chest wall for the site of the apical pulse. ? Place a watch where it will be seen by both nurses. This facilitates accuracy in the beginning and the ending. ? Position one nurse to take the radial pulse. Locates the radial pulse. ? The second nurse places the stethoscope on the patient's chest at the fifth in tercostal space to the left of the sternum at the midclavicular line. Locates the apical pulse. ? The nurse taking the radial pulse states "Start" when ready to begin and "Stop " when completed. This ensures that both counts are done simultaneously. ? Both nurses count the pulse for 1 full minute at the same time. Counting for 1 full minute is necessary for an accurate assessment of any discrepancies that may exist between the two sites. ? Compare the rates obtained. If a difference is noted between the rates, subtra ct the radial rate from the apical rate. This determines if a pulse deficit exists. A pulse deficit repr esents the number of ineffective or nonperfused heartbeats. ? Replace the patient's clothing, and place patient in position of comfort. This restores patient's privacy ? Notify the physician if a pulse deficit was noted. Provides prompt medical int ervention. Assessing Blood Pressure Overview _ Establish a baseline measurement of arterial blood pressure for subsequent eva luation. _ Determine the patient's hemodynamic status (e.g., stroke volume of the heart a nd blood vessel resistance). _ Identify and monitor changes in blood pressure resulting from a disease proces s and medical therapy (e.g., presence or history of cardiovascular disease, renal disease, cir culatory shock, or acute pain; rapid infusion of fluids of blood products).
Preparation _ Readings reflecting a 20-mm Hg change in blood pressure should be reported. _ Although a diastolic pressure can be obtained by palpation, frequent errors oc cur in obtaining results. _ If the patient has had a mastectomy or has a hemodialysis shunt or IV infusion , avoid taking blood pressure in the affected extremity. Special Considerations Pediatric Patients _ Newborns have a mean systolic pressure of about 75 mm Hg. _ The pressure rises with age, reaching a peak at the onset of puberty, and then tends to decline somewhat. _ One quick way to determine the normal systolic blood pressure of a child is to use the following formula: Normal systolic BP=80 + (2 x child's age in years ). Elderly Patients _ In older people, elasticity of the arteries is decreased-the arteries are more rigid and less yielding to the pressure of the blood. _ This produces an elevated systolic pressure. _ Because the walls no longer retract as flexibly with decreased pressure, the d iastolic pressure is also higher. Equipment _ Sphygmomanometer with cuff (size must be appropriate for patient) _ Stethoscope Procedure ? Check to determine if patient smoked or had caffeine prior to blood pressure a ssessment. This allows the nurse to assess blood pressure accurately and to identify significant changes. ? Instruct patient to refrain from both prior to measurement. ? Determine the proper cuff size for the patient. The bladder should completely encircle the arm without overlapping. The cuff should be long enough to encircle the arm several times. Proper cuff si ze is required for the correct amount of pressure to be applied over the artery. ? Determine the best site for the cuff placement. Application of pressure from a n inflated cuff can temporarily impair blood flow and compromise patient's circulation.
? Explain the purpose of the procedure to the patient. This reduces anxiety. ?Wash hands. Reduces spread of microorganisms. Did you find this download useful? Get more nursing-related stuff at http://ward class.blogspot.com ? Assist the patient to a comfortable sitting position, with the upper arm sligh tly flexed, the forearm supported at heart level, and the palm turned up. Placing the arm above the leve l of the heart produces false-low readings. This position facilitates cuff application. ? Fully expose the patient's upper arm. This ensures proper cuff placement. ? Palpate the brachial artery (on the lower medial side of the biceps muscle) an d position the cuff 1 in. (2.5 cm) above the pulsations. The stethoscope will be placed over the arter y without touching the cuff. ? Center the arrows marked on the cuff over the brachial artery. Inflating the b ladder directly over the brachial artery ensures that proper pressure is applied during inflation of the cuff. ? With the cuff fully deflated, wrap it evenly and snugly around the upper arm. A loose-fitting cuff will cause a false elevation in the blood pressure measurement. ? Keep manometer at eye level. The nurse should be no more than approximately 1 yard away. This ensures accurate reading of the mercury level. ? Palpate the brachial or radial artery while rapidly inflating the cuff. Inflat e to a pressure 30 mm Hg above the point at which the pulse disappears. Slowly deflate the cuff, and noti ce when the pulse reappears. This identifies the patient's approximate systolic pressure and deter mines the maximal inflation point for an accurate reading. It also prevents an auscultatory gap. ? Place the stethoscope earpieces in the ears, and be sure that sounds are clear , not muffled. Each earpiece should follow the angle of the ear canal to facilitate hearing. ? Deflate the cuff, and wait 30 seconds. Prevents venous congestion and false-hi gh readings. ? Relocate the brachial artery, and place the diaphragm of the stethoscope over it. Ensures optimal reception of sound. ? Close the valve of the pressure bulb by turning it clockwise until tight. Prev ents air leaking during inflation. ? Inflate the cuff to 30 mm Hg above the patient's palpated systolic level. This ensures an accurate pressure measurement.
? Slowly open the valve and allow the mercury to fall at a rate of 2 to 3 mm Hg per second. A decline in mercury that is too fast or too slow may lead to an inaccurate measurement. ? Note the point on the manometer when the first clear sound is heard. The first Korotkoff sound indicates the systolic pressure. ? Continue to deflate the cuff gradually making note when the muffled or dampene d sound appears, and the point on the manometer when the sound disappears in adults. (Note the pr essure to the nearest 2 mm Hg.) A fourth Korotkoff sound may be detected as a diastolic pressu re in adults with hypertension. ? Continue to deflate the cuff, noticing the point to the nearest 2 mm Hg when t he sound disappears. The fifth Korotkoff sound is recommended as the diastolic reading in an adult. ? Deflate the cuff rapidly and remove from the patient's arm, unless the measure ment needs to be repeated. Continuous inflation causes arterial occlusion, which will result in n umbness and tingling of the patient's arm. ? If the procedure needs to be repeated, wait 30 seconds. This prevents venous c ongestion and a false-high reading. ? Fold the cuff and store it in its proper place. Proper maintenance of the equi pment contributes to the accuracy of the instrument. ? Assist the patient to a comfortable position and cover upper arm. ( Promotes c omfort. ) ? Record findings on the medical record or the flow sheet. ( This documents the procedure and the patient's status. ) Blood Pressure Assessment by Palpation ? Explain the procedure to the patient ( This decreases anxiety and promotes pat ient cooperation. ) I Wash hands. ( Prevents transmission of microorganisms. ) ? Locate the patient's brachial or radial pulse. ( This locates the pulse that o ffers the best palpable volume for the procedure. ) ? Place the cuff on the patient's arm. ( This will position the cuff for inflati on. ) ? Palpate again for the pulse. ( When the pulse is felt, continue to palpate. Th is relocates the pulse for the procedure. ) ? Inflate the cuff until unable to palpate the pulse. ( This occludes the arteri al blood flow. )
? Inflate the cuff until the measurement gauge is 20 mm Hg past the point at whi ch the pulse was lost on palpation. ( This identifies the point of pulse return. ) ? Slowly deflate the cuff at a rate of 2 to 3 mm Hg per second. ( This prevents the nurse from missing the first palpable beat. ) ? Note the reading on the measurement gauge when the pulse returns. Remove cuff from the patient's arm. ( This identifies the systolic blood pressure reading. )
Assessing Body Temperature Overview _ Establish baseline data. _ Determine if core temperature is within normal range. _ Determine changes in core temperature in response to specific therapies (e.g., antipyretic medication, immunosuppressive therapy, invasive procedures _ Monitor patients who are at risk for temperature alterations (those exposed to extreme temperatures; patients at risk for or with a diagnosis of infection; patients wi th a leukocyte count below 5000 or above 12,000). _ Most common sites for measuring body temperature are sublingual, rectal, axill ary, and tympanic. _ Site most often used for body temperature measurement is sublingual. Preparation _ Assess patient to determine appropriate method to obtain body temperature. _ For an oral temperature, obtain reading 15 to 30 minutes after ingestion of ho t or cold food or fluids or smoking. _ Oral route is contraindicated if patient is unable to hold thermometer properl y or if there is a risk that patient may bite thermometer. _ Rectal thermometer must be held securely in place and never left unattended. Fahrenheit to Centigrade Conversion Table Fahrenheit (F) Centigrade 96.8 97.7 98.6 99.5 100.4 101.0 102.2 103.1 (C) 36.0 36.5 37.0 37.5 38.0 38.3 39.0 39.5
104.0
40
Note: To convert degrees F to degrees C subtract 32, then multiply by 5/9. To convert degrees C to degrees F multiply by 9/5, then add 32. Special Considerations Pediatric Patients Oral temperature measurement is not used on infants or small children. Rectal temperature measurement is contraindicated in newborns. Prevent infants and young children from kicking their legs or rolling to their s ide while the thermometer is in place. Tympanic membrane thermometers quickly obtain a child's temperature and may prov ide less of a threat to the child. Elderly Patients Disturbances in temperature regulation that normally occur with aging can cause the older adult to have a lower-than-normal body temperature. Equipment _ Oral, rectal, axillary, or tympanic thermometer _ Probe covers if electronic thermometer is used _ Lubricant and tissue if rectal site is used _ Towel if axillary site is used Procedure Oral Temperature Assessment ?Wash hands and apply disposable gloves. Reduces transmission of microorganisms. ? Explain procedure to patient. Reduces anxiety and promotes cooperation. ? Hold color-coded end of glass thermometer between fingertips. Prevents contami nation of bulb. ? Slowly rotate thermometer at eye level to read mercury level Mercury should be below 96_F (35.5_C). Thermometer reading must be below patient's actual temperature before use. ? If mercury is higher than desired level, shake thermometer downward. Hold uppe r end of thermometer securely between thumb and forefinger and stand away from solid obje cts. Sharply flick wrist downward until mercury is at appropriate level. Brisk shaking lowers mercury level in the glass tube. Standing in an open area away from objects prevents the breakage of the thermometer. ? Place thermometer in a plastic sheath according to agency policy. Prevents spr ead of microorganisms. ? Ask patient to open mouth and gently place thermometer at the base of the tong ue to the right or left of the frenulum, in the posterior sublingual pocket. Reflects the core temp
erature of the blood in the larger blood vessels. ? Ask patient to close the lips, not the teeth, around the thermometer. Maintain s the proper position of the thermometer. Biting could cause the thermometer to break and can injure t he oral mucosa and cause mercury poisoning. ? Leave the thermometer in place for 3 minutes or according to agency policy. Mi nimum amount of time recommended obtaining an accurate reading with this type of thermometer. ? Carefully remove thermometer, discard plastic sheath, and read results at eye level. Gentle handling prevents discomfort to patient and ensures an accurate reading. Rectal Temperature Assessment ?Wash hands and apply disposable gloves. Reduces transmission of microorganisms. ? Explain procedure to patient. Reduces anxiety and promotes cooperation. ? Draw curtains around the patient's bed and/or close the door. Keep the patient 's upper body and lower extremities covered. This maintains privacy for the patient and minimizes patient embarrassment. ? Assist patient into Sims' position, with the upper leg flexed to expose anal a rea. Children may be placed in a prone position. This provides for optimal exposure of the anal area for correct placement of the thermometer ? Squeeze a liberal amount of water-soluble lubricant onto a tissue. Apply lubri cant to the thermometer. Insertion of the thermometer into the lubricant container would con taminate contents of the container. Use of lubrication minimizes trauma to the rectal mucosa durin g insertion. ? With the nondominant hand, raise the patient's upper buttock to expose the anu s. Full retraction of the buttocks completely exposes anus. ? Gently insert the thermometer into the anus in the direction of the umbilicus. Insert the thermometer 11/2 in. (3.5 cm) for adults and 1/2 in. (1.2 cm) for infants or children. Do no t force the thermometer. Ask the patient to take a deep breath and blow out. Insert the thermometer as th e patient takes in a breath. If resistance is felt, immediately remove the thermometer. Proper insert ion of the thermometer ensures adequate exposure to the blood vessels in the rectal wall. G entle insertion prevents trauma to the mucosa or the breakage of the thermometer. Having the pat ient take a deep breath helps to relax the anal sphincter. ? Hold the thermometer in place for a minimum of 2 minutes or according to agenc
y policy. It may be necessary to hold patient's legs. Holding the thermometer in place prevents inju ry to the patient. Axillary Temperature Assessment ?Wash hands and apply disposable gloves. Reduces transmission of microorganisms. ? Explain procedure to patient. Reduces anxiety and promotes cooperation. ? Draw curtains around the bed and/or close the door. Provides privacy and minim izes embarrassment for the patient. ? Assist the patient into a supine or sitting position.Move clothing away from t he patient's shoulder and arm. Be sure the axillary area is dry. Provides optimal exposure of the pati ent's axilla. ? Place the thermometer into the center of the patient's axilla, lower the arm o ver the thermometer, and place the patient's forearm across the chest. Maintains the proper position of the thermometer against the blood vessels in the axilla. ? Hold the thermometer in place for; 5 to 10 minutes or according to agency poli cy. The recommended time varies among agencies; 5 minutes is the time most often recomme nded for children. ? Remain with the patient and hold the thermometer in place if the patient is un able to do so. Prevents injury to the patient. ? Remove the thermometer, remove plastic sheath, and read results at eye level. Wash the thermometer in tepid, soapy water, rinse in cold water, and dry. Shake down the thermometer and return it to its container. Cleaning the thermometer after use reduces the sprea d of infection. Assessing Respiratory Rate Overview _ Establish baseline data. _ Monitor respiratory rate, depth, and rhythm. _ Assess patient for presence of dyspnea or cyanosis. _ Assess for abnormal lung sounds, such as rales, rhonchi, or wheezes. _ Note respiratory rate, rhythm, and depth. _ Note labored, difficult, or noisy respirations or cyanosis. _ Identify alterations in respiratory pattern resulting from disease conditions. _ Assess if accessory muscles are used for breathing. Preparation _ Assess rate when patient is at rest. Special Considerations Pediatric Patients
_ Respirations range from 30 to 80 per minute in newborns. Children 1 to 3 years of age have a normal respiratory range of 20 to 40 breaths per minute. Children 6 to 8 years o lds have respiratory rates that range from 15 to 25 breaths per minute, as do 10-year-old children. Elderly Patients _ Chronic illness in the older population can affect respiratory patterns. Equipment _ A watch with a second hand Procedure ? Place the patient in a position of comfort, preferably sitting. Discomfort can cause the patient to breathe more rapidly. ? Place the patient's arm in a relaxed position across the abdomen or lower ches t, or place your hand directly over the patient's upper abdomen. This is the same position used d uring the assessment of the pulse. Both the patient's and the nurse's hands rise and fall during the respiratory cycle. Measurement of the respirations is done immediately after the pulse asses sment and is not perceived by the patient. ? Observe the complete respiratory cycle (consists of one inspiration and one ex piration). This ensures that the count will begin with a normal respiratory cycle. ? Once a cycle is observed, monitor the watch's second hand and begin to count t he rate of respirations. When the second hand reaches a number on the dial, count "one" to begin the first cycle. Timing of the respirations begins with a count of 1. Respirations occur m ore slowly than the pulse; therefore, the count begins with 1. ? For adults, count the number of respirations in 30 seconds, then multiply by 2 . For infants or young children, count the respirations for 1 full minute. The respiratory rate is equi valent to the number of respirations per minute. ? If an adult's respirations have an irregular rhythm or they are abnormally fas t or slow, count for 1 full minute. This ensures an accurate measurement. ? While counting, note whether the depth of respirations is shallow, normal, or deep and whether the rhythm is regular or altered. The character of ventilatory movements may indicat e specific alterations in respirations or disease states. ? Record the results in the chart or the flow sheet. Report any signs of respira tory alterations to the physician. This provides data to monitor for changes in the patient's condition.
Abnormalities require medical intervention. Respiratory Rates and Rhythms Kussmaul's respiration: Respirations that are regular but abnormally deep and in crease in rate Biot's respiration: Periods of respiration of equal depth, alternating with peri ods of apnea (absence of breathing) Cheyne-Stokes respiration: Gradual increase in depth of respirations, followed b y gradual decrease and then a period of apnea Apnea: Absence of breathing Giving A Complete Bed Bath Overview _ Ensures cleanliness of patients who cannot bathe themselves. _ Promotes circulation. _ Provides comfort. _ Maintains muscle tone and joint mobility through active and passive movement. _ Provides an opportunity for thorough assessment. Preparation _ Assess patient's ability to perform his or her own care. _ Discuss patient preferences for bathing. _ Provide privacy. _ Avoid chilling the patient. _ Wash your hands; wear gloves if you will come in contact with body fluids or h andle a bedpan. _ Gather all supplies in room before you begin. _ Ask patient if he or she needs to use the bedpan _ Check to see if patient is allergic or sensitive to soap. Special Considerations _ It is always preferable to have the patient assist with the bath as much as po ssible, particularly with perineal care. _ The bed bath is a good time to establish rapport and expand the nurse-patient relationship. _ During and after the bath, the bed linen is changed, and the two activities ar e usually combined. _ After giving a bed bath, always ask the patient if he feels comfortable; make sure the bed is in low position, side rails up, and call bell is within reach. Equipment _ Basin of warm water _ Soap and soap dish _ Towels and washcloths (two or three of each, if possible) _ Laundry bag or hamper _ Clean gown _ Clean gloves Procedure ? Discuss procedure with patient and ensure privacy. Promotes cooperation and de creases anxiety. ? Place all supplies within reach. Organizes task and prevents unnecessary steps .
? Wash hands. Reduces transmission of microorganisms. ? Position bed at comfortable height. Reduces nurse's back strain. ? Fill basin with warm water, and test temperature on wrist. Testing temperature helps prevent accidental scalding. ? Help patient to side of bed closest to you, and lower side rail. Provides acce ss to patient, and reduces back strain of nurse. ? Remove patient's clothes while providing warmth and privacy with a covering su ch as a bed blanket. Provides access to body parts; provides modesty and warmth. ? Take washcloth and wrap the cloth around your hand tightly, forming a mitt. Pr events splashing water on patient and bedclothes. ? Be careful of the patient's eyes. Use clear water to clean them, starting from the inner canthus to the outer canthus. If patient is not sensitive to soap, lather washcloth and gen tly wash the patient's face, starting from the forehead down. Some patients are sensitive to soap or ha ve very dry skin, and soap could increase dryness and lead to irritation and skin breakdown. Bathe from cleanest area and work downward toward feet, going from areas of cleanest to dirtiest. At tention to the eyes prevents eye irritation and infection. ? Bathe ears and front and back of neck. Perspiration accumulates on the back of the neck when patients lie in bed for long periods. ? Bathe upper body and extremities, stroking arms from wrist to shoulder. Includ e axillary area. Stimulates circulation. ? Soak hands in basin if indicated. Dirt accumulates under fingernails, especial ly in incontinent patients. ? Keep chest covered with towel and wash under breasts on female patients. Apply powder if patient desires. This area stays moist on many females and can lead to skin excoriation. ? Bathe abdomen using side-to-side strokes on skin folds. Moisture and debris ca n accumulate in skin folds leading to irritation. ? Bathe legs and feet, being sure perineal area is draped. Prevents unnecessary exposure. ? Soak feet in basin if indicated, and if patient is able to hold leg in positio n. Soaking will soften rough skin and facilitate cleaning toenails. ? Change bath water if necessary. Bath water may be cool or dirty.
? Assist patient to side-lying position and wash back. Give backrub. Side-lying position gives access to patients back for backrub. ? Put on clean gloves and bathe perineal area. Dry thoroughly. Prevents cross co ntamination of organisms. Excess moisture contributes to skin breakdown. ? Remove gloves and assist patient to put on clean gown. Promotes dignity and re duces exposure. ? Conduct other personal hygiene activities as needed. Promotes patient's body i mage. ? Lower bed, raise side rails, put call bell in reach, and dispose of used equip ment and linen. Provides safety. ? Wash your hands. Reduces transmission of microorganisms. Providing Foot Care Overview _ Prevents infection and injury to soft tissues. _ Patients with peripheral vascular disease or diabetes mellitus need to be refe rred to a specialist, such as a podiatrist. _ Many institutions do not allow staff to perform foot care especially with diab etic patients-toenail clipping . Referral to a podiatrist is made (if applicable). Preparation _ Assess the ability of the patient to perform his or her own nail care before i ntervening. _ Assess condition of feet, toes, and toenails. _ Inspect all surfaces of the nails. _ Assess color, pulses, and temperature of toes and feet. _ Check water temperature. Special Considerations (for patients with diabetes or circulatory disorders) _ Diabetic patients may lack sensation in their feet and cuts, if unnoticed, by lead to infection. _ Feet, including soles, heels, and areas between toes should be inspected daily . _ Clean socks or stockings should be worn daily; walking on barefoot is never al lowed. _ Feet should be dried properly, esp. between toes; lotion is applied for dry, f laky feet _ Insides of shoes should be checked for stones, tears, of foreign objects. _ Instruct patient not to cut corns or calluses. Equipment _ Basin _ Nail clippers _ Emery board or nail file _ Disposable gloves _ Towel _ Orange stick Procedure ? Inspect all surfaces of each foot. Check in between toes and around nail bed t
o detect early skin breakdown. Check pulse, skin color, and temperature, and compare to other foot. Early detection of break in skin integrity. Identify circulatory problems. ? Soak feet in basin filled with warm, soapy water before trimming the toenails. Gently wash each foot, between nails, and all surfaces. Soaking softens the nails and allows them to be trimmed and cleaned easily. Washing removes dirt. ? Thoroughly dry each foot including bet. toes. Excess moisture leads to skin br eakdown, possible fungal infections. ? Perform nail care if allowed given facility policy and patient risks. Improper ly performed nail care can lead to nonhealing injuries, including the potential for amputation in patie nts with impaired circulation. ? Push cuticle gently back with orange stick. Reduces incidence of irritated, cr acked, loose fragmented cuticles. ? After soaking the nails and if appropriate (if nails are not thick), use a toe nail clipper and clip nail straight across. Take care not to trim the nail too short. Cutting straight across prevents forma tion of sharp nail spikes that can irritate nail margins. ? Slowly trim all toenails as previously described. Take time to trim slowly, av oiding cutting toenails at corners, which may damage tissues. ? After all nails have been trimmed, lightly apply lotion to feet. To lubricate dry skin and retain moisture. Providing Mouth Care Overview _ Removes plaque and bacteria-producing agents from the oral cavity, and removes unpleasant tastes and odors. _ Teaches proper oral hygiene. _ Assesses oral mucosa, teeth and throat at this time. _ Procedure includes brushing the teeth, flossing, and caring for dentures, if a pplicable Preparation _ Determine if the patient wears dentures. _ Assess whether the patient can perform his or her own mouth care. _ Inquire about oral hygiene practices. Special Considerations _ Patients with an oral airway, NG tube, or tube feeding, and patients who are r eceiving oxygen need frequent oral hygiene _ Provide type of oral care most acceptable to the patient. _ At the end of the procedure, make sure that unpleasant odors, tastes, and exce ss secretions have been removed Equipment _ Toothbrush
_ Dental floss _ Cup of water _ Emesis basin _ Towel _ Clean gloves _ Additional equipment for denture care: denture cup, denture cleanser _ Additional equipment for unconscious patients: mouth swabs, 20 ml syringe, ton gue blades Procedure Mouth Care ? Wash hands. Reduces transmission of microorganisms. ? Gather all equipment. Promotes efficiency. ? Discuss procedure with patient. Discover hygiene preferences. ? Put on clean gloves. Prevents contact with microorganisms or body fluids. ? Assess oral mucosa, teeth, and throat. Determines status of oral cavity and pa tient's need for care and teaching. ? Hold emesis basin beneath chin. Catches spilled water and irrigation water. ? Taking the soft toothbrush in hand, brush the teeth starting from the top fron t and moving to the back molars. Do not brush in a circular motion, but begin at the gum line and sw eep toward teeth. Brush gently. Stimulates gums and removes food particles from gum line. With var ious disease states, gums become sensitive and easily fragile making them more susceptible to micro tears. ? Lightly brush the tongue. Improves the breath, cleans the tongue of coated foo d particles and sputum. ? Allow patient to rinse his or her mouth and expectorate into emesis basin. Irr igation removes food particles. ? Ask the patient if he or she uses dental floss. If acceptable to the patient, floss between each tooth, using approximately 12-15 inches of easy-glide floss, taking care not to get flo ss lodged between teeth. Removes particles caught between teeth that was not removed by brushing. ? Allow patient to rinse his or her mouth and expectorate into emesis basin. Rem oves food particles. ? Remove equipment. Proper disposal of equipment prevents spread of infection. ? Remove gloves and wash hands. Reduces spread of microorganisms. ? Check to see if patient is comfortable. Verifies comfort status. Denture Care
? Wash hands, and put on clean gloves. Reduces transmission of microorganisms, a nd prevents contact with body fluids. ? Help patient remove dentures or remove them by placing your finger on the uppe r denture and gently pressing downward. Breaks the seal at the roof of the mouth and allows th e upper denture to slide out. Lowers usually lift out easily. ? Place a washcloth on the bottom of the sink, if washing dentures over the sink . Prevents dentures from breaking in case they are dropped in sink. ? Take the patient's soft toothbrush and gently brush the dentures with toothpas te and rinse under running water. Removes food particles and bacteria. ? Replace dentures in patient's mouth or store in denture cup full of water. Den tures need to be kept in a wet area to avoid warping. ? Remove gloves and wash hands. Reduces transmission of microorganisms. Mouth Care (Unconscious Patients) ? Wash hands, and put on clean gloves. Reduces transmission of microorganisms an d prevents contact with body fluids. ? Place the patient in a side-lying position or, if patient does not have any he ad or neck injury, turn the head to the side. Allows fluid to drain from mouth and prevents aspiration. ? Place clean towel under the patient's mouth. Keeps bedclothes dry and free fro m debris. ? Brush teeth and tongue with brush or sponge toothettes, using tongue blade to move cheek and lips to allow visibility of area. Removes food particles and bacteria. ? Rinse with very small amount of water using a 20-mL syringe and gently irrigat ing the teeth and sides of the mouth, catching water in emesis basin. Large amounts of water can i ncrease the patient's chances for aspiration. ? Repeat this step if patient's mouth has dried sputum/saliva to loosen dried de bris gently. Repeated gentle irrigation will loosen dried debris and prevent mucosal breakdown. ? Lubricate lips and tongue with lip protector lubricant. Provides moisture and helps with control of halitosis. ? Remove emesis basin and towel from under patient's chin, ensuring that the pat ient is dry and free from wetness. Reduces transmission of microorganisms.
? Reposition patient as necessary. Frequent checks ensure correct body alignment . ? Remove gloves and wash hands. Reduces transmission of microorganisms. Get more nursing-related stuff at http://wardclass.blogspot.com Common Problems Among Elderly Aging is a normal progressive process, beginning at conception and ending in de ath. Aging is not synonymous with diseases but diseases become more common as age progresses. Usua lly the diseases present with non-specific multiple symptoms that involve many organs. I ncreasing age in the elderly is associated with the higher morbidity and frequent use of health s ervices. Their illness tends to be chronic with no simple cure. This makes them more dependent on the f amily, society and health services. As the population ages, the nurse practitioner will be more involved in geriatri c care. There are solutions that nurse practitioners can offer elderly patients to improve day-today functioning. Problems Nursing Intervention Confusion/Dementia 1. Spend time with the Patient 2. Use touch to convey concern 3. Provide frequent reiteration of orienting data (e.g. time, place) 4. Have clocks or calendars in the environment 5. Explain all actions, procedures and routines to the patient 6. Address the patient by his/her name 7. Keep a routine activities Constipation 1. Increase Fluid Intake 2. Daily Exercise 3. Increase fiber intake (e.g. fruits and vegetables) Complications associated with constipation include hemorrhoids from straining, anal fissures, rectal prolapse, and fecal impaction. Untreated constipation in institutionalized patients can lead to cemented lesions in the colon, megacolon, bowel blockage and perforation, peritonitis, and sepsis. Osteoporosis 1. Have adequate calcium in diet: ? Milk/dairy products ? Fish ? Beans ? Orange Juice ? Cereal or read that have added calcium ? Take calcium supplements 2. Get regular exercise 3. Avoid alcohol, quit smoking. Alcohol and smoking reduce bone mass. 4. Avoid large amounts of protein - rich or salty and caffeine foods. They can cause loss of calcium from the body. 5. Make the home safe to avoid accidents. 6. Practice good posture.
4. Use good body mechanics when lifting objects (e.g. bend the knees instead of the back). 5. Do back exercises to improve posture. 6. Wear rubber-soled, low-heeled shoes that grip well. 7. Don't lift heavy objects. 8. Avoid using a stool or bending over. 9. Put items frequently used within easy reach. 10. Use handrails when going up and down stairs. 11. Hormonal Replacement Therapy (HRT) for menopausal women as prescribed. Postural Hypotension (PH) 1. Get out of bed slowly and in stages. 2. Sleep with head of bed elevated several inches. 3. Have a daily fluid intake of 2 to 3 liters. 4. Avoid hot showers or baths, may cause venous dilatation thereby, venous pooling. 5. Avoid straining at stool. This may cause fall of BP 6. Avoid bending down and suddenly standing up again. 7. Rest for 60 minutes after meals. 8. Avoid hyperventilation. This lowers the BP. 9. Exercise regimen must be recommended. 10. Use thigh-length elastic stockings to reduce venous pooling. 11. Avoid prolonged standing. 12. Heed warning signs of PH (e.g., dizziness, faintness, visual disturbances) 13. Pharmacotherapy: Fludrocortisone (a mineralocorticoid that promotes retention of water and sodium) Hypertension 1. Encourage stress reduction and relaxation. 2. Encourage exercise such as swimming and walking. 3. Encourage healthy diet (fresh fruits, rice, vegetable). 4. No weightlifting. 5. Quit smoking, no alcohol, 6. Reduce intake of saturated fats. 7. Reduce salt intake to 1 to 6 gm per day. 8. Take prescribed medications at regular basis. Elder abuse There are many types of abuse used against the elderly. They include: 1. Psychologic abuse such as instilling fear, threatening or making the elderly perform demeaning tasks, 2. Physical abuse such as hitting, slapping, or burning. 3. Financial abuse such as taking their money or forcing them to sign over their assets. 4. Neglect such as withholding food, medications or basic care. 5. Infringement of personal rights such as restraining for long periods of time against their will or isolating them from normal social interactions. 6. Sexual abuse 7. The perpetrator of abuse is usually the spouse or the children of the victim. Caregivers who abuse their elderly family members are often middle-aged or older or have emotional problems such as alcoholism or substance abuse. Resources: http://Medscape.com
Vous aimerez peut-être aussi
- Community Health NursingDocument13 pagesCommunity Health NursingMa Rafaela Rosales PalomponPas encore d'évaluation
- Case Study: Acute GlomerulonephritisDocument28 pagesCase Study: Acute GlomerulonephritisMa Rafaela Rosales Palompon91% (11)
- Nursing Care PlanDocument2 pagesNursing Care PlanMa Rafaela Rosales PalomponPas encore d'évaluation
- Cs AGNDocument177 pagesCs AGNMa Rafaela Rosales PalomponPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- BK Tant 007549Document78 pagesBK Tant 007549Nicholas MachaPas encore d'évaluation
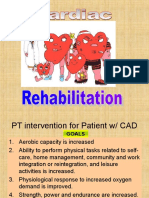
- Cardiac RehabilitationDocument87 pagesCardiac RehabilitationMaya Vil100% (2)
- PhysioEx Exercise 5Document21 pagesPhysioEx Exercise 5Sinisa Ristic100% (1)
- Stress Management Techniques Evidencebased Procedures That Reduce Stress and Promote Health PDFDocument16 pagesStress Management Techniques Evidencebased Procedures That Reduce Stress and Promote Health PDFMaica MagbitangPas encore d'évaluation
- CSORDocument136 pagesCSORLimun100% (3)
- Bangsbo, J. (2006) - Physical and Metabolic Demands of Training and Match-Play in The Elite Football Player.Document10 pagesBangsbo, J. (2006) - Physical and Metabolic Demands of Training and Match-Play in The Elite Football Player.Marko BrzakPas encore d'évaluation
- Medsurg Cardio Ana&PhysioDocument6 pagesMedsurg Cardio Ana&Physiorabsibala80% (10)
- PE and Health 1 Midterm Exam - My Fitness JourneyDocument4 pagesPE and Health 1 Midterm Exam - My Fitness JourneyCedrik AustriaPas encore d'évaluation
- 3M CVP Monitoring - Assisting in BMA ECG Interpretation - Final Draft - 3CDocument65 pages3M CVP Monitoring - Assisting in BMA ECG Interpretation - Final Draft - 3CAlexa GoteraPas encore d'évaluation
- Trimline 7600Document22 pagesTrimline 7600Mark Cuff100% (1)
- Vicorder List of Tests and Parameters PDFDocument4 pagesVicorder List of Tests and Parameters PDFHatem FaroukPas encore d'évaluation
- Music, Arts, Physical Education and Health Department: Lesson 1: Physical Fitness TestsDocument22 pagesMusic, Arts, Physical Education and Health Department: Lesson 1: Physical Fitness TestsMary Jean MagdayPas encore d'évaluation
- Of Our Mission: at The HeartDocument6 pagesOf Our Mission: at The Heartkhairul ihsanPas encore d'évaluation
- Nursing Care of Patients With HypertensionDocument13 pagesNursing Care of Patients With HypertensionDon Chiaw Manongdo100% (1)
- A Non-Intrusive Multi-Sensor System For Characterizing Driver BehaviorDocument5 pagesA Non-Intrusive Multi-Sensor System For Characterizing Driver BehaviorQazi Khubaib AlamPas encore d'évaluation
- Effects of Lidocaine On Pulse RateDocument7 pagesEffects of Lidocaine On Pulse RateMichael DiabPas encore d'évaluation
- Uterine Blood Flow During Supine Rest and Exercise After 28 Weeks of GestationDocument9 pagesUterine Blood Flow During Supine Rest and Exercise After 28 Weeks of GestationMD Luthfy LubisPas encore d'évaluation
- The Effect of Music On Stress and Anxiety ReductionDocument5 pagesThe Effect of Music On Stress and Anxiety ReductionMutuma GakulePas encore d'évaluation
- Funda Notes Compilation Lecture and SkillsDocument21 pagesFunda Notes Compilation Lecture and SkillsmysterioushumanePas encore d'évaluation
- Provide Nursing Care in First Line PDFDocument219 pagesProvide Nursing Care in First Line PDFMisaw KasyePas encore d'évaluation
- PHD Thesis Proposal Gokhan KazarDocument29 pagesPHD Thesis Proposal Gokhan Kazarserhat yaşpalaPas encore d'évaluation
- Handheld RelaxationDocument8 pagesHandheld RelaxationSiska Prima OlimvianiPas encore d'évaluation
- Workshop On Early Warning Score System - Ali HaedarDocument61 pagesWorkshop On Early Warning Score System - Ali HaedarGede Kevin Adhitya SaputraPas encore d'évaluation
- Perbandingan Dosis Induksi Ketamin 1 MG/KGBB Dan 2 MG/KGBB Terhadap Tekanan Darah Dan Frekuensi Denyut JantungDocument13 pagesPerbandingan Dosis Induksi Ketamin 1 MG/KGBB Dan 2 MG/KGBB Terhadap Tekanan Darah Dan Frekuensi Denyut JantungAprimansahPas encore d'évaluation
- Total Fitness in 30 Minutes A Week CompressDocument260 pagesTotal Fitness in 30 Minutes A Week CompressPatriciaPas encore d'évaluation
- DF Hebb: Industries, IncDocument25 pagesDF Hebb: Industries, IncRetro SeasonsPas encore d'évaluation
- P.Fitness and Self Testing Activities NewDocument28 pagesP.Fitness and Self Testing Activities NewAriane MangunePas encore d'évaluation
- LH C1 Advanced - WBDocument96 pagesLH C1 Advanced - WBfelipegomez24041Pas encore d'évaluation
- EssentialMathFormulas FinalDocument2 pagesEssentialMathFormulas FinalAmir ValizadehPas encore d'évaluation
- Adventure Plus: Treadmill Owner'S ManualDocument28 pagesAdventure Plus: Treadmill Owner'S ManualJohn DavidPas encore d'évaluation