Académique Documents
Professionnel Documents
Culture Documents
COPD Exacerbation
Transféré par
justhoangDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
COPD Exacerbation
Transféré par
justhoangDroits d'auteur :
Formats disponibles
UptoDate: COPD Exacerbation
Definition: exacerbation of COPD defined as acute increase in one or more of the following symptoms: Cough increases in severity and frequency Sputum production increases in volume and or changes character Dyspnea increases Precipitants 70-80% of COPD exacerbations are due to respiratory infections (most common: H. influenza, M. catarrhalis, S. pneumo, P. aeruginosa) Risk factors for exacerbation: DDx CHF exacerbation Pulmonary thromboembolism PNA Advanced age Productive cough Duration of COPD Hx of antibiotic therapy COPD-related hospitalization within previous year Comorbidities (eg ischemic heart dz, CHF, DM)
O2 Tx: target PaO2 of 60 70 mmHg, with saturation of 90-94%. Adequate oxygenation must be assured, even if it leads to hypercapnia, which is well tolerated by patients whose PaCO2 is chronically elevated. However, mech ventilation may be required if hypercapnia is associated with depressed mental status, profound academia, or cardiac dysrhythmias. Pharmacologic Tx: Beta adrenergic agonists Inhaled short-acting beta adrenergic agonists (eg, albuterol) are the mainstay of therapy because of their rapid onset of action and efficacy in producing bronchodilation. These may be administered via a nebulizer or a metered dose inhaler (MDI) with a spacer device. o Albuterol 2.5 mg (diluted to a total of 3 mL) by nebulizer q1-4 hours prn, or four to eight puffs (90 mcg per puff) by MDI (metered dose inhaler) with a spacer q1-4 hours prn. Anticholinergic agents Inhaled short-acting anticholinergic agents (eg, ipratropium bromide) are used with inhaled short-acting beta adrenergic agonists. Combination therapy produces bronchodilation in excess of that achieved by either agent alone. o Atrovent 500 mcg by nebulizer q4 hours prn. Alternatively, two puffs (18 mcg per puff) by MDI with a spacer q4 hrs Systemic glucocorticoids- when added to the bronchodilator therapy, improve symptoms and lung function, and decrease the length of hospital stay. Oral glucocorticoids appear equally effective as IV glucocorticoids. o Prednisone 30 to 40 mg daily or methylprednisolone 60 to 125 mg, two to four times daily for 10 to 14 days. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines advise using equivalents of prednisone 30 to 40 mg qday Antibiotics Antibiotics are indicated for many patients having a COPD exacerbation. See table flow chart Mucoactive agents little evidence supports the use of mucoactive agents (eg, N-acetylcysteine) in acute exacerbations of COPD. Methylxanthines Aminophylline and theophylline are NOT recommended for the treatment of COPD exacerbations.
Prognosis It is estimated that 14% of patients admitted for an exacerbation of COPD will die within three months of admission. Prevention - Measures should be taken to prevent future exacerbations, including smoking cessation, pulmonary rehabilitation, proper use of medications (including metered dose inhaler technique), and vaccination
UptoDate: COPD Exacerbation
Managing patients with both COPD with CAD Coronary artery disease (CAD) and chronic obstructive pulmonary disease (COPD) share tobacco abuse as a risk factor, therefore these two disorders commonly exist. 50% of patients over 50 years old with COPD also had CAD, HTN, or heart failure. Exacerbation of COPD may strain an already diseased heart, through hypoxemia and increased work of breathing, while an exacerbation of ischemic heart disease can further impair gas exchange by incrementally raising airway resistance or reducing the oxygen saturation. Because its hard to distinguish which organ is causing the symptoms, empiric treatment of both conditions is warranted. Treatment of either condition has the potential to worsen the other. Inhaled beta-2 agonists are of special concern because, even though they are relatively selective for beta-2 adrenergic receptors, they may have the following deleterious effects that could be a problem in patients with CAD: o The possible induction of arrhythmias by stimulation of cardiac beta-adrenoreceptors o Reflex activation of adrenergic mechanisms by causing peripheral vasodilation o Downregulation of myocardial beta-2-receptors, worsening heart failure associated with left ventricular systolic dysfunction o Provocation of hypokalemia and hypoxemia through worsened matching of ventilation and perfusion Recommendation consider first prescribing alternative, potentially safer drug like inhaled glucocorticoid or tiotropium. Beta blockers Beta blockers, which are useful in managing ischemic heart disease, may induce bronchospasm in those with COPD, in particular, nonselective beta blockers. The dosage required for this effect might be as low as that found in topical eye preparations such as timolol. o Beta-1 selective beta blockers (eg, atenolol or metoprolol) appear to be safe in patients with COPD, even when there is a bronchospastic component. Recommendation Many patients with emphysema and chronic bronchitis have been successfully treated with beta blocker therapy, with few adverse events. A cardioselective beta blocker, such as atenolol or metoprolol, or a combined beta and alpha blocker, such as carvedilol, can be cautiously prescribed. Salmeterol plus fluticasone It is assumed that the cardiovascular effects of this combination are directly related to the long acting betaagonist component. This combination was evaluated in the TORCH trial. The incidence of cardiovascular events was not increased in this group, compared to placebo Recommendation While the data is not yet conclusive, when a long-acting bronchodilator is indicated, we suggest initiating a long-acting anticholinergic agent first. However, the combination of an inhaled glucocorticoid plus a long-acting beta-2 agonist can be added safely if the anticholinergic alone is insufficient.
Vous aimerez peut-être aussi
- Mechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingD'EverandMechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingH. RaškováPas encore d'évaluation
- 2&3-Pharmacology of Drugs Used in Bronchial Asthma & COPDDocument58 pages2&3-Pharmacology of Drugs Used in Bronchial Asthma & COPDKishan SethPas encore d'évaluation
- Anti EmeticsDocument29 pagesAnti EmeticsBezawit Tsige100% (1)
- Clinical Pharmacology: Proceedings of the 7th International Congress of Pharmacology, Paris 1978D'EverandClinical Pharmacology: Proceedings of the 7th International Congress of Pharmacology, Paris 1978P. Duchêne-MarullazPas encore d'évaluation
- Pharmacotherapy of PneumoniaDocument56 pagesPharmacotherapy of Pneumoniahoneylemon.co100% (1)
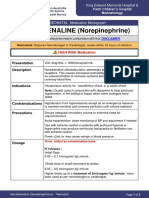
- NORADRENALINE (Norepinephrine) : Presentation DescriptionDocument3 pagesNORADRENALINE (Norepinephrine) : Presentation DescriptionMutiaraPas encore d'évaluation
- Pharmacology of The GITDocument31 pagesPharmacology of The GITmarviecute22Pas encore d'évaluation
- Optimized Clinical Case StudiesDocument4 pagesOptimized Clinical Case StudiesAassh DcmbrPas encore d'évaluation
- MCQ 1-7Document9 pagesMCQ 1-7جعغر آل حيدرPas encore d'évaluation
- Lung Metabolism: Proteolysis and Antioproteolysis Biochemical Pharmacology Handling of Bioactive SubstancesD'EverandLung Metabolism: Proteolysis and Antioproteolysis Biochemical Pharmacology Handling of Bioactive SubstancesAlain JunodPas encore d'évaluation
- Pharmacology Questions1Document2 pagesPharmacology Questions1أبوأحمد الحكيمPas encore d'évaluation
- AMH Must FlagDocument2 pagesAMH Must FlagpurnibaPas encore d'évaluation
- Renal PharmacologyDocument52 pagesRenal PharmacologyashrafPas encore d'évaluation
- Lung Development Biological and Clinical Perspectives: Biochemistry and PhysiologyD'EverandLung Development Biological and Clinical Perspectives: Biochemistry and PhysiologyPhilip FarrellPas encore d'évaluation
- Therapeutic Hypothermia - Principles, Indications, Practical ApplicationD'EverandTherapeutic Hypothermia - Principles, Indications, Practical ApplicationPas encore d'évaluation
- Ion Channels in Health and DiseaseD'EverandIon Channels in Health and DiseaseGeoffrey S. PittPas encore d'évaluation
- Drugs Acting on the Gastrointestinal TractDocument27 pagesDrugs Acting on the Gastrointestinal TractJames PerianayagamPas encore d'évaluation
- Antidotes and The Clinical Applications Antidote: An Antidote Is A Substance Which Can Counteract A Form ofDocument2 pagesAntidotes and The Clinical Applications Antidote: An Antidote Is A Substance Which Can Counteract A Form ofManohar Chowdary KovvuriPas encore d'évaluation
- Code of Ethics for Kenyan PharmacistsDocument20 pagesCode of Ethics for Kenyan PharmacistsKevin Chapley50% (2)
- Type A Choice Questions (Only One Answer Is Correct) : A. B. C. D. EDocument10 pagesType A Choice Questions (Only One Answer Is Correct) : A. B. C. D. ERAED GhunaimPas encore d'évaluation
- Name Honor Pledge (Signature) : Questions 1 - 2 Refer To The Following CaseDocument9 pagesName Honor Pledge (Signature) : Questions 1 - 2 Refer To The Following CasegregstevensPas encore d'évaluation
- 3 - March 2021Document116 pages3 - March 2021SEIYADU IBRAHIM KPas encore d'évaluation
- General Pharmacology - Sources of Drugs and Routes of AdministrationDocument48 pagesGeneral Pharmacology - Sources of Drugs and Routes of AdministrationDhriti Brahma78% (9)
- Cal Pharmaspirit PH Cal Q ADocument49 pagesCal Pharmaspirit PH Cal Q AAriadne BalmacedaPas encore d'évaluation
- Acute Ischemic Stroke: by Steven H. Nakajima, Pharm.D., BCCCP and Katleen Wyatt Chester, Pharm.D., BCCCP, BCGPDocument26 pagesAcute Ischemic Stroke: by Steven H. Nakajima, Pharm.D., BCCCP and Katleen Wyatt Chester, Pharm.D., BCCCP, BCGPCristian Florin CrasmaruPas encore d'évaluation
- Drug Interactions of Antianginal Drugs..Document40 pagesDrug Interactions of Antianginal Drugs..Kamal SikandarPas encore d'évaluation
- Bronchodilator & Other Drugs Used in AsthmaDocument15 pagesBronchodilator & Other Drugs Used in AsthmaGenta JagadPas encore d'évaluation
- AntiemeticsDocument10 pagesAntiemeticsnk999999100% (1)
- Pharmacotherapeutics 140828123349 Phpapp02Document14 pagesPharmacotherapeutics 140828123349 Phpapp02Anonymous s9i0WyKF200% (1)
- Ethiopian National Drug FormularyDocument572 pagesEthiopian National Drug FormularyportosinPas encore d'évaluation
- (9-10-11 2022)Document173 pages(9-10-11 2022)SEIYADU IBRAHIM KPas encore d'évaluation
- 2017 April Exam CompilationDocument8 pages2017 April Exam CompilationabbasyaqobiPas encore d'évaluation
- Shared RX Modules For FinalsDocument11 pagesShared RX Modules For FinalsOdyPas encore d'évaluation
- Matching ActivityDocument26 pagesMatching Activityapi-661456802Pas encore d'évaluation
- Principles and Practice of Pharmacology for AnaesthetistsD'EverandPrinciples and Practice of Pharmacology for AnaesthetistsÉvaluation : 5 sur 5 étoiles5/5 (1)
- 15 - April - 2018: C-Fendaparinux + Low Molecular Weight HeparinDocument8 pages15 - April - 2018: C-Fendaparinux + Low Molecular Weight HeparinAbdul SalamPas encore d'évaluation
- (DownSub - Com) Pharmacology - PHARMACOKINETICS (MADE EASY)Document8 pages(DownSub - Com) Pharmacology - PHARMACOKINETICS (MADE EASY)Stephen VuelbanPas encore d'évaluation
- CV 12-29-19Document7 pagesCV 12-29-19api-507198061Pas encore d'évaluation
- lec2 المعدلةDocument120 pageslec2 المعدلةAhmed FouadPas encore d'évaluation
- 07 Dosage RegimenDocument44 pages07 Dosage Regimenzetttttttttt100% (3)
- CPR SummaryDocument2 pagesCPR SummaryaqsamerajPas encore d'évaluation
- Notes in PharmacologyDocument95 pagesNotes in PharmacologyMylz MendozaPas encore d'évaluation
- QuestionsDocument13 pagesQuestionsMikee MeladPas encore d'évaluation
- APHA-Chapter-34 - Patient Assessment Laboratory: REVIEW OF SYSTEMS - Physical Assessment, Vital Signs& ObservationsDocument13 pagesAPHA-Chapter-34 - Patient Assessment Laboratory: REVIEW OF SYSTEMS - Physical Assessment, Vital Signs& ObservationsDrSamia El WakilPas encore d'évaluation
- Advanced Pharmacology Module 4 DiscussionDocument3 pagesAdvanced Pharmacology Module 4 Discussionapi-634345342Pas encore d'évaluation
- Anti Parkinson Drugs FinallDocument36 pagesAnti Parkinson Drugs FinallandrapradeshssePas encore d'évaluation
- Antihypertensive DrugsDocument52 pagesAntihypertensive Drugsapi-224264169Pas encore d'évaluation
- Management of Common Infections With Antimicrobials Guidance Clinical Practice Guidelines (2019) PDFDocument4 pagesManagement of Common Infections With Antimicrobials Guidance Clinical Practice Guidelines (2019) PDFveerrajuPas encore d'évaluation
- Pharmacology Notes: By: Khurram AbbasDocument48 pagesPharmacology Notes: By: Khurram AbbasAsma AnjumPas encore d'évaluation
- Anti-Anginal and Antiischemic Drugs: Dr. Pradeepa H D Clinical PharmacologistDocument25 pagesAnti-Anginal and Antiischemic Drugs: Dr. Pradeepa H D Clinical PharmacologistpradeephdPas encore d'évaluation
- Community Pharmacy Rutter PDF DownloadDocument2 pagesCommunity Pharmacy Rutter PDF DownloadNicole40% (5)
- Clinical Physiology and Pharmacology: The EssentialsD'EverandClinical Physiology and Pharmacology: The EssentialsÉvaluation : 4 sur 5 étoiles4/5 (1)
- Pharmacology Ain Shams 123 - Compress 1Document552 pagesPharmacology Ain Shams 123 - Compress 1ahmed hoty100% (1)
- Top 10 Drug InteractionsDocument4 pagesTop 10 Drug InteractionsLeyla MajundaPas encore d'évaluation
- Pediatric Nutrition and Nutritional Disorders: PediatricsDocument4 pagesPediatric Nutrition and Nutritional Disorders: Pediatricsapi-3829364Pas encore d'évaluation
- Science ProposalDocument7 pagesScience ProposalDimple EstelPas encore d'évaluation
- Legal Aid ProjectDocument5 pagesLegal Aid ProjectUday singh cheemaPas encore d'évaluation
- Anti-epileptic drugs: Types, Mechanisms & TreatmentDocument7 pagesAnti-epileptic drugs: Types, Mechanisms & TreatmentSampada ghodkiPas encore d'évaluation
- Women in Leadership - South West Conference 2019Document24 pagesWomen in Leadership - South West Conference 2019Gareth NoyesPas encore d'évaluation
- DMDFDocument22 pagesDMDFsujal177402100% (1)
- NOAA Sedimento 122 Squirt CardsDocument12 pagesNOAA Sedimento 122 Squirt CardshensilPas encore d'évaluation
- Sickle-Cell AnemiaDocument11 pagesSickle-Cell Anemiahalzen_joyPas encore d'évaluation
- 2.4 Maxillofacial Trauma (Sia) - Sales&TanDocument11 pages2.4 Maxillofacial Trauma (Sia) - Sales&Tanmr dojimamanPas encore d'évaluation
- Crowding Boarding and Patient Through PutDocument9 pagesCrowding Boarding and Patient Through PutMarwa El SayedPas encore d'évaluation
- Malunggay Para sa PamilyaDocument4 pagesMalunggay Para sa PamilyaJeffrey S. Saballo100% (1)
- Problem - Solution EssayDocument2 pagesProblem - Solution EssayMaría Cecilia Soto RosasPas encore d'évaluation
- Peace Corps Medical Officer (PCMO) Job AnnouncementDocument3 pagesPeace Corps Medical Officer (PCMO) Job AnnouncementAccessible Journal Media: Peace Corps DocumentsPas encore d'évaluation
- Enalapril Maleate TabletsDocument2 pagesEnalapril Maleate TabletsMani SeshadrinathanPas encore d'évaluation
- Siddhant Fortis HealthCareDocument4 pagesSiddhant Fortis HealthCaresiddhant jainPas encore d'évaluation
- Metaphor and MedicineDocument9 pagesMetaphor and MedicineCrystal DuartePas encore d'évaluation
- Hemifacial Spasm A NeurosurgicalDocument8 pagesHemifacial Spasm A NeurosurgicaldnazaryPas encore d'évaluation
- 2001SimulationCompet PDFDocument15 pages2001SimulationCompet PDFdaselknamPas encore d'évaluation
- Which Is More Effective in Treating Chronic Stable Angina, Trimetazidine or Diltiazem?Document5 pagesWhich Is More Effective in Treating Chronic Stable Angina, Trimetazidine or Diltiazem?Lemuel Glenn BautistaPas encore d'évaluation
- HRFuture Sept 2020 MJLKJDocument59 pagesHRFuture Sept 2020 MJLKJGlecy KimPas encore d'évaluation
- Saudi Board Exam - Surgery Questions from 2009 Exam (192/200Document47 pagesSaudi Board Exam - Surgery Questions from 2009 Exam (192/200Rahmah Shah Bahai100% (2)
- Corn SpecDocument4 pagesCorn SpecJohanna MullerPas encore d'évaluation
- UntitledDocument19 pagesUntitledAnna S. LatipPas encore d'évaluation
- Sop Cleaning Rev 06 - 2018 Rev Baru (Repaired)Document20 pagesSop Cleaning Rev 06 - 2018 Rev Baru (Repaired)FajarRachmadiPas encore d'évaluation
- Addressing The Impact of Foster Care On Biological Children and Their FamiliesDocument21 pagesAddressing The Impact of Foster Care On Biological Children and Their Familiesapi-274766448Pas encore d'évaluation
- Investigations For Diseases of The Tongue A Review PDFDocument6 pagesInvestigations For Diseases of The Tongue A Review PDFShantanu DixitPas encore d'évaluation
- C & W Meat Packers Carly Courtney Cynthiana KY Notice of Suspension Humane Treatment LivestockDocument4 pagesC & W Meat Packers Carly Courtney Cynthiana KY Notice of Suspension Humane Treatment LivestockghostgripPas encore d'évaluation
- "We Are Their Slaves" by Gregory FlanneryDocument4 pages"We Are Their Slaves" by Gregory FlanneryAndy100% (2)
- Csa Fodrea 2014 - 2015 Student Handbook FinalDocument37 pagesCsa Fodrea 2014 - 2015 Student Handbook Finalapi-260407035Pas encore d'évaluation
- Reorganizing Barangay Council for Child ProtectionDocument3 pagesReorganizing Barangay Council for Child ProtectionCasim Bailan JrPas encore d'évaluation