Académique Documents
Professionnel Documents
Culture Documents
Periop Anaemia
Transféré par
Abdelwahab MukhtarDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Periop Anaemia
Transféré par
Abdelwahab MukhtarDroits d'auteur :
Formats disponibles
HAEMOLYMPHOID SYSTEM
50% increase in middle cerebral artery blood flow velocity. This peaks at about 24 minutes and returns to normal within 810 minutes. The resultant increased cerebral blood volume can contribute to secondary brain injury. Normocapnoea maintained by hyperventilation following tourniquet deflation can prevent the increase in intracranial pressure. Haematological effects: pain caused by the tourniquet and surgery provoke the release of catecholamines, which promote platelet aggregation and may initially result in systemic hypercoagulability. However, limb tissue ischaemia following tourniquet inflation promotes tissue plasminogen activator release, activating the antithrombin III and thrombomodulinprotein-C anticoagulant systems in the occluded limb and causing systemic thrombolysis when the tourniquet is deflated. Tourniquet deflation can be associated with post-tourniquet bleeding caused by a brief (30 minutes) increase in thrombolytic activity in peripheral blood. Reports of fatal pulmonary emboli associated with lower limb exsanguination, tourniquet inflation and deflation suggest that tourniquets are contraindicated in patients at high risk of deep vein thrombosis (e.g. previous history of venous thrombosis, prolonged immobilization, pelvic and lower limb fractures). Echogenic small (miliary) and large venous emboli can be detected by transoesophageal echocardiography following tourniquet deflation during total knee arthroplasty. Potentially fatal pulmonary embolisms have occurred after intramedullary guide insertion, femoral reaming and cementing of long-stemmed femoral prostheses. There is approximately a 5-fold increased risk of large venous embolism associated with the use of a tourniquet in patients undergoing total knee arthroplasty. Low doses of heparin administered intraoperatively (e.g. 1000 U before tourniquet inflation in knee arthroplasty) may prevent fatal pulmonary embolism during and after total joint arthroplasties. Metabolic changes: after 12 hours of ischaemia, arterial serum potassium and lactate concentrations increase by 0.280.32 mmol/l and by 2.13 mmol/l, respectively, for about 30 minutes following deflation. Lactic acid released from the ischaemic limb and the increase in arterial partial pressure of CO2 causes a transient (1030 minutes) decrease in arterial pH. Oxygen consumption and carbon dioxide production are increased by 55% and 80% respectively, two minutes after tourniquet release and return to pre-release values within 8 minutes. These changes are dependent on the duration of tourniquet inflation. Temperature changes: a rise in body core temperature occurs during the inflation of arterial tourniquets because of reduced metabolic heat transfer from the central compartment to the peripheral compartment, and also from decreased heat loss from distal skin. After tourniquet deflation, a transient decrease in core temperature by 12 C results from the redistribution of body heat and the return of hypothermic venous blood from the tourniquet limb into the systemic circulation. Antibiotic administration Prophylactic antibiotics for surgery should be administered intravenously at least 5 minutes before tourniquet inflation to ensure adequate tissue penetration. u
Perioperative Anaemia and its Management
Susan V Mallett
Anaemia may be either chronic (haematological disorders, malnutrition, chronic disease, malignancy or occult blood loss) or acute, secondary to sudden blood loss. Traditionally in surgical practice, red cell transfusion was prescribed when haemoglobin (Hb) levels reached the magic trigger of 10 g/dl. This was based on the concept of providing an adequate margin of safety during anaesthesia and surgery and the belief that levels of Hb above 10 g/dl improved wound healing and general patient well-being. Over the last decade, there has been a move towards accepting lower Hb values because there is no evidence that this practice improves patient outcome and, indeed, there is an increasing body of literature that suggests the contrary. Seventy percent of all transfusions are administered in the perioperative period. It is crucial that transfusion decisions are based on a thorough knowledge of the physiological principles involved and the existing evidence for transfusion triggers, and that consideration is given to alternative strategies that avoid using or reduce the need to use allogeneic blood.
Red blood cells
The usual component provided by blood banks is red cell concentrate. This contains the red blood cells (RBCs) from 450 ml of blood with sufficient plasma, anticoagulant and adenine-saline additive solution to give a haematocrit of around 60%. The total volume of each unit is approximately 300350 ml. With these additives blood may be stored for up to 42 days. Red cell concentrates do not contain any viable platelets or plasma clotting factors. The primary function of red cells is oxygen transport, as well as providing a significant part of the intravascular volume. One unit of red cells will raise the plasma haemoglobin concentration by 1.1 g/dl in the average 70 kg adult. In acute blood loss without volume resuscitation, it may take several hours for the Hb concentration to equilibrate and reflect the true extent of blood loss as fluid is drawn into the intravascular space from the extravascular tissues. However, in the controlled
Susan V Mallett is a Consultant Anaesthestist at the Royal Free Hospital, London, UK. She qualified from St Bartholomews Hospital, London, and trained in anaesthesia in London and the Presbyterian University Hospital, Pittsburgh, USA. Her clinical interests are hepatobiliary and cardiothoracic surgery. Her research interests include coagulation and transfusion.
SURGERY
221
2002 The Medicine Publishing Company Ltd
HAEMOLYMPHOID SYSTEM
situation where fluid losses are replaced with crystalloid or colloid solutions to maintain normovolaemia, the Hb and haematocrit values rapidly equilibrate (in under 15 minutes) and this enables rapid assessment of the effects of transfusion or of recurrence of bleeding. Near patient testing of Hb with a Haemocue is very useful in the acute situation. When Hb results are not immediately accessible, transfusion is often considered on the basis of estimated blood loss (EBL). However, this must always be considered in terms of the patients estimated circulating volume (70 ml/kg) and preoperative Hb. An EBL of 1000 ml in a 100 kg male (12% loss) with a preoperative Hb of 15 g/dl will be of very different significance to a 1000 ml loss in a 50 kg female (30% loss) with an Hb of 11 g/dl.
Benefits of red cell transfusion
There is no evidence from the available literature that transfusing patients to an Hb of 10 g/dl or above has any impact on wound healing, morbidity, or rehabilitation following surgery. A recent randomized study in over 800 critically ill patients demonstrated that a restrictive red cell transfusion policy (maintaining Hb at 79 g/dl) was as least as effective and possibly superior to a more liberal regime (transfusion when Hb fell below 10 g/dl). At the current time there are very few well-conducted studies available to support existing clinical practice guidelines. For obvious reasons randomized controlled trials comparing risk/benefit ratios of red cell transfusions to no transfusions are not generally feasible. The best available surrogate trials are those reporting on the surgical outcome of patients who refuse transfusions for religious reasons. In the absence of coronary artery disease, all patients whose death was related to anaemia died with an Hb less than 5 g/dl, usually in the context of active bleeding. Many surgical patients have survived with significantly lower haemoglobins, the lowest reported to date being 1.4 g/dl. One often ignored benefit of RBC transfusion is an improvement in haemostatic function. At very low haematocrits (56 g/dl), normal axial streaming is lost and the platelet/ endothelial reaction is significantly impaired.
Oxygen transport and the physiological response to anaemia
The aim of transfusing red blood cells is to improve or maintain the oxygen-carrying capacity of the blood. Oxygen delivery (DO2) is determined by the product of cardiac output and arterial oxygen content (CaO2), where: CaO2 = 1.34 x Hb (g/dl) x %O2 saturation + (0.003 x PaO2) The adequacy of oxygen supply is determined by the balance of its supply and demand (tissue oxygen extraction), which is called the extraction ratio (ER). In normal circumstances, ER is 25%, giving a reserve of 75%. As with many systems in the body there is built-in redundancy so that, provided normovolaemia is maintained, Hb can fall to levels well below 10 g/dl without compromising tissue oxygenation (Figure 1). The physiological compensations to falling Hb include increased cardiac output.
Bulk viscosity of blood increases exponentially with haematocrit and the resistance to blood flow increases with increased viscosity, limiting cardiac output. In terms of whole-body oxygen delivery, the optimal Hb (greatest oxygen delivery at lowest energy cost) is around 1011 g/dl. The reduced viscosity compared to that at higher haemotocrits leads to improved flow due to a fall in vascular resistance and improved cardiac output. Between 10 and 15 g/dl Hb, total oxygen delivery remains relatively constant, and at levels above this, the increased viscosity actually reduces oxygen delivery. The relationship of blood viscosity and oxygen transport capacity with haematocrit is shown in Figure 2. Acute versus chronic anaemia In acute anaemia, the most important clinical features are the amount and rate of blood loss, together with the likelihood of continuing blood loss. The primary treatment goals are to restore intravascular volume, ensure sufficient oxygen-carrying capacity and stop haemorrhage. In chronic anaemia the patient is often hypervolaemic as plasma volume expands to maintain an increased cardiac output and oxygen delivery. In addition, another compensatory response to chronic anaemia is the
SURGERY
222
2002 The Medicine Publishing Company Ltd
HAEMOLYMPHOID SYSTEM
A recent study found that in high-risk vascular surgery patients, haematocrits less than 28% were independently associated with a significantly increased incidence of death, myocardial infarction and unstable angina. In contrast, in a randomized study of over 400 patients undergoing coronary artery bypass grafting it was found that lowering the transfusion trigger to 8 g/dl postoperatively did not result in any increased morbidity, emphasizing the importance of coronary revascularization and improved flow.
When to transfuse: the transfusion trigger
Generally, most practice guidelines advise against a single figure at which transfusion is triggered; indeed, it would be illogical to assume that a single trigger threshold is appropriate for all patients: male, female, young, old and those with associated comorbidity. Most, such as the American Society of Anesthesiologists, recommend a range of values between 6 and 10 g/dl, and that the decision to transfuse should be based on the individual patients risk for complications from inadequate oxygenation, as well as important physiological and surgical factors. The question is not what is the lowest haemoglobin that a patient will tolerate, but what Hb concentration provides an acceptable level of safety for that particular individual. A single unit of blood may be perfectly adequate therapy to achieve a target Hb, and there is absolutely no justification for the entrenched practice of prescribing a minimum of two units of RBC if transfusion is deemed necessary.
Risks of transfusion
Transfusion cannot be considered to be risk-free. Known risks include allergic reactions, incompatibility, transfusion-related lung injury, sepsis, graft-versus-host disease and transmission of bacterial and viral infections. The Serious Hazards of Transfusion (SHOT) reporting system found that almost 50% of the morbidity and mortality associated with transfusion is due to procedural errors (wrong blood to wrong patient), with resultant incompatibility mismatch reactions. Infection: despite the fact that the blood supply is the safest it has ever been, much of the concern centres on the possibility of viral infection transmission. Testing may fail to detect viral replication early on in the infectious window. Overall, the risk is extremely low and estimated by the Retrovirus Epidemiology Donor Study (REDS) in the USA at 1 in 676,000 for HIV-1, 1 in 103,000 for hepatitis C and 1 in 63,000 for hepatitis B. There is increasing concern over the possibility of transmission of prion and variant Creutzfeld-Jacob disease (CJD), despite the fact that there is no epidemiological evidence of transmission in humans by blood transfusion. Universal leukodepletion of all labile blood components was introduced in the UK in November 1999 in response to this perceived risk, and also because of its other beneficial effects, such as the reduction of immunomodulatory effects and HLA alloimmunization. In the UK, children under the age of six must receive fresh frozen plasma donated in the USA (a country free of bovine spongiform encephalopathy) due to concerns over the transmission of prions.
increased intracellular production of 2,3-diphosphoglycerate (2,3-DPG) by red cells. This has the effect of shifting the oxygen dissociation curve to the right, facilitating oxygen unloading and delivery to the tissues. Many patients will chronically tolerate an Hb of 78 g/dl without any obvious symptoms. It is important to establish the cause of anaemia and treat appropriately. Where RBC transfusion is required in chronic, compensated anaemia for symptoms such as severe fatigue, shortness of breath or angina, all transfusions (particularly in the elderly) must be administered very slowly, possibly with diuretic cover, because of the increased circulatory volume and the risk of precipitating congestive cardiac failure. Elderly patients and cardiovascular disease The elderly generally do not tolerate severe anaemia as well as the young. They have reduced physiological compensatory mechanisms and also a higher incidence of coronary artery disease. Electrocardiographic evidence of ischaemia (ST depression) was described in 22% of patients with pre-existing impaired left ventricular function with modest haemodilution, but was not seen in patients with normal ventricular function. This suggests that in the presence of moderate coronary artery stenosis, flow may not increase sufficiently to offset the loss of oxygen-carrying capacity caused by haemodilution and ischaemic cardiac dysfunction may result. Patients with critical vessel stenosis may not tolerate haemodilution to any degree.
SURGERY
223
2002 The Medicine Publishing Company Ltd
HAEMOLYMPHOID SYSTEM
Immunomodulatory effects: early studies that appeared to demonstrate that perioperative allogeneic transfusion was associated with reduced survival in patients with cancers were initially dismissed, because it was thought that the need for transfusion was associated with lower initial Hb and increased surgical blood loss, both of which could be surrogate markers for more advanced cancers. However, a meta-analysis by Chung et al of over 20 trials (5236 patients) in patients with colorectal carcinoma supports the hypothesis that perioperative transfusion increases the risk of disease recurrence and death, with a cumulative odds ratio of a negative outcome of 1.69. A number of recent studies have demonstrated that transfusion of allogeneic blood is independently associated with longer hospital stays, an increased risk of postoperative infection and higher treatment costs. In patients undergoing orthopaedic procedures, the incidence of postoperative infection is significantly reduced if patients avoid transfusion or receive only autologous blood.
anaemia needs careful consideration and monitoring. ANH is acceptable to most Jehovahs Witness patients, providing that certain principles (continuous contact with circulation) are respected. Perioperative cell salvage: intraoperative use of cell savers can reduce the need for banked blood by 3070%. There are various types available, and some require the presence of a dedicated operator (increasing expense). The CATS system allows continuous processing of collected blood (as opposed to batched processing), which is an advantage when blood loss is heavy, as in liver transplantation. Haemostatic drugs: anti-fibrinolytics (e.g. tranexamic acid) have been shown to reduce blood loss in cardiac surgery. High-dose aprotinin (anti-kallikrein) is an effective haemostatic agent and reduces blood loss in cardiac surgery and liver transplantation. It is particularly valuable in high-risk patients, such as those undergoing re-operation, those who have sepsis and patients on aspirin therapy. Blood substitutes: there are three major blood substitute technologies being developed: cell-free polymerized haemoglobin, liposome encapsulated haemoglobin and perfluorocarbon emulsions. Many are currently undergoing phase III trials, but there are still some unresolved problems and they are unlikely to be available in routine clinical practice for several years. u
Limiting allogeneic blood transfusion
Clearly, there are good reasons for avoiding unnecessary transfusion with allogeneic blood. Simple measures such as measuring Hb before transfusion and using single-unit transfusions where appropriate will significantly reduce the total number of transfusions. Other strategies for limiting the use of allogeneic blood include increasing preoperative haemoglobin, collection of autologous blood, acute normovolaemic haemodilution, perioperative cell salvage and the use of haemostatic drugs and blood substitutes. Increasing preoperative haemoglobin: haematinics such as ferrous sulphate or recombinant human erythropoietin (EPO) should be considered. Patients who are anaemic prior to surgery can benefit from these therapies and, if started some weeks before the surgery, the increased red cell mass and haematocrit will reduce their chance of requiring intraoperative transfusion. Preoperative autologous blood donation (PAD): this can be considered where facilities are available and if there is a significant probability of the patient requiring intraoperative transfusion with two or more units of red cells. There are logistic constraints, including the need to delay surgery for several weeks while blood is collected (average donation is one unit per week, one unit per 34 days if the patient is on EPO therapy), the need for the patient to attend the collection centre on a number of occasions, and the need to guarantee a date for surgery. Acute normovolaemic haemodilution (ANH): blood is collected from the patient at the start of the procedure and the volume replaced with appropriate volumes of crystalloid or colloid solutions. Any blood lost during surgery consequently has a lower haematocrit and total red cell loss is reduced. The fresh whole blood is then re-infused at the end of the procedure or at any point when transfusion criteria are met. This technique can reduce the need to use allogeneic blood and donor unit exposure. Individual patient tolerance to acute compensated
FURTHER READING American Society of Anesthesiologists Task Force on Blood Component Therapy. Practice guidelines for blood component therapy. Anesthesiology 1996; 84: 73247. Herbert P C, Wells G, Blajchman M D et al. A multicentre, randomized, controlled clinical trial of transfusion requirements in critical care. N Eng J Med 1999; 340: 40917. Spiess B D, Counts R B, Gould S A, Eds. Perioperative Transfusion Medicine. Baltimore: Lippincott Williams & Wilkins, 1998.
SURGERY
224
2002 The Medicine Publishing Company Ltd
Vous aimerez peut-être aussi
- Hemorrhagic ShockDocument2 pagesHemorrhagic ShockPharhana PuteriePas encore d'évaluation
- Maternal Anemia Management and Anaesthesia ConsiderationsDocument46 pagesMaternal Anemia Management and Anaesthesia ConsiderationsNivedita PrabhakarPas encore d'évaluation
- Physiology of Transfusion TherapyDocument34 pagesPhysiology of Transfusion Therapyterara0% (1)
- 1998 Lippincott WilliamsDocument27 pages1998 Lippincott WilliamsAnonymous KyjOD6qPas encore d'évaluation
- ABC of Management of Hypovolaemic Shock: Major TraumaDocument5 pagesABC of Management of Hypovolaemic Shock: Major TraumakatybabyyyPas encore d'évaluation
- 5 Volume and Electrolyte Management: Concezione TommasinoDocument20 pages5 Volume and Electrolyte Management: Concezione TommasinoTayyab SiddiquiPas encore d'évaluation
- Managing Obstetric HemorrhageDocument11 pagesManaging Obstetric HemorrhageClara VerlinaPas encore d'évaluation
- Management of HemorrhageDocument11 pagesManagement of Hemorrhagemerin sunilPas encore d'évaluation
- Adverse Effects of Crystalloid and Colloid Fluids: ReviewsDocument6 pagesAdverse Effects of Crystalloid and Colloid Fluids: Reviewsdhania husnainiPas encore d'évaluation
- Impact of Albumin RL For BTDocument10 pagesImpact of Albumin RL For BTSandeep BhaskaranPas encore d'évaluation
- Sistem Imun & Hematologi: Transfusi Darah dan KomponennyaDocument65 pagesSistem Imun & Hematologi: Transfusi Darah dan KomponennyaBaiq Harsani AuroraPas encore d'évaluation
- cc2851 (PDF - Io)Document15 pagescc2851 (PDF - Io)Aquardoleo ValentinoPas encore d'évaluation
- Dapus 3Document7 pagesDapus 3Dhea NadhilaPas encore d'évaluation
- Fluid & Blood Therapy Key ConceptsDocument31 pagesFluid & Blood Therapy Key ConceptsMohammad Pino HakimPas encore d'évaluation
- JurnalDocument17 pagesJurnalDay EnPas encore d'évaluation
- Hypovolemic ShockDocument10 pagesHypovolemic ShockUsran Ali BubinPas encore d'évaluation
- Burn Fluid Resuscitation GuideDocument35 pagesBurn Fluid Resuscitation GuideNur Anniesa100% (2)
- Pathophysiology and Etiology of Edema - IDocument9 pagesPathophysiology and Etiology of Edema - IBrandy MaddoxPas encore d'évaluation
- 7 3 Transfusion Management of Major HaemorrhageDocument6 pages7 3 Transfusion Management of Major HaemorrhageKoas Neuro UnpattiPas encore d'évaluation
- Postoperative Hemorrhagic Shock Class Iii Following Transurethral Resection of The Prostate (Turp) PatientDocument20 pagesPostoperative Hemorrhagic Shock Class Iii Following Transurethral Resection of The Prostate (Turp) Patientanang raharjoPas encore d'évaluation
- Damage Control Management in Surgical EmergencyDocument61 pagesDamage Control Management in Surgical Emergencyofficial.drjainPas encore d'évaluation
- Emergency Fluid Therapy in Companion Animals - PPitneyDocument9 pagesEmergency Fluid Therapy in Companion Animals - PPitneyUmesh GopalanPas encore d'évaluation
- DrHSMurthy HiPECDocument11 pagesDrHSMurthy HiPECReddyPas encore d'évaluation
- Pharmacology of Crystalloids and ColloidsDocument16 pagesPharmacology of Crystalloids and ColloidsarliniePas encore d'évaluation
- Fluid Therapy For Septic Shock Resuscitation: Which Fluid Should Be Used?Document6 pagesFluid Therapy For Septic Shock Resuscitation: Which Fluid Should Be Used?MagnusPas encore d'évaluation
- Fluid Choice for Resuscitation Based on Deficit CauseDocument4 pagesFluid Choice for Resuscitation Based on Deficit CauseshanabsinPas encore d'évaluation
- Conduct of Cardiovascular PerfusionDocument24 pagesConduct of Cardiovascular PerfusionBranka KurtovicPas encore d'évaluation
- Evidence and Triggers For The Transfusion of Blood and Blood ProductsDocument9 pagesEvidence and Triggers For The Transfusion of Blood and Blood Productscahaya tinggiPas encore d'évaluation
- Fluid Therapy FinalDocument3 pagesFluid Therapy Finallaureeate100% (1)
- Blood Transfusion TherapyDocument5 pagesBlood Transfusion TherapyHayes CloverPas encore d'évaluation
- Hypovolemic Shock - StatPearls - NCBI BookshelfDocument1 pageHypovolemic Shock - StatPearls - NCBI BookshelfRoselyn VelascoPas encore d'évaluation
- Fluid & Electrolite Management in Surgical WardsDocument97 pagesFluid & Electrolite Management in Surgical WardsBishwanath PrasadPas encore d'évaluation
- Hypervolemia Increases Release of Atrial Natriuretic Peptide and Shedding of The Endothelial GlycocalyxDocument8 pagesHypervolemia Increases Release of Atrial Natriuretic Peptide and Shedding of The Endothelial GlycocalyxbayanganPas encore d'évaluation
- Blood Transfusion 2Document12 pagesBlood Transfusion 2Helene AlawamiPas encore d'évaluation
- Central Pontine Myelinolysis During Treatment of Hyperglycemic Hyperosmolar Syndrome: A Case ReportDocument6 pagesCentral Pontine Myelinolysis During Treatment of Hyperglycemic Hyperosmolar Syndrome: A Case ReportHaribabuBabuPas encore d'évaluation
- Hypovolemic Shock: by DR Teh W.CDocument29 pagesHypovolemic Shock: by DR Teh W.CTeh Wai Choon100% (1)
- Addison K May, MD John P Reilly, MD, Msce Scott Manaker, MD, PHD Arthur J Silvergleid, MD Geraldine Finlay, MD Contributor DisclosuresDocument12 pagesAddison K May, MD John P Reilly, MD, Msce Scott Manaker, MD, PHD Arthur J Silvergleid, MD Geraldine Finlay, MD Contributor DisclosuresAlvaro HaroPas encore d'évaluation
- Pembimbing: Dr. R. Vito Mahendra E, M.Si Med, SP.B M. Adri Kurniawan 30101306981Document31 pagesPembimbing: Dr. R. Vito Mahendra E, M.Si Med, SP.B M. Adri Kurniawan 30101306981Adek AhmadPas encore d'évaluation
- FiiiiiiixDocument22 pagesFiiiiiiixYeni dwi anggra sudarmajiPas encore d'évaluation
- Surgery 1.1 Fluid and Electrolyte Balance - Azares PDFDocument7 pagesSurgery 1.1 Fluid and Electrolyte Balance - Azares PDFAceking MarquezPas encore d'évaluation
- Bundle 3 Hour Step4 FluidsDocument4 pagesBundle 3 Hour Step4 FluidsgythriePas encore d'évaluation
- Hypovolemic Shock 09Document58 pagesHypovolemic Shock 09Joanne Bernadette Aguilar100% (2)
- Use of Blood Products in The Critically Ill - UpToDateDocument13 pagesUse of Blood Products in The Critically Ill - UpToDateOscar F RojasPas encore d'évaluation
- Anaestetic Management of Liver DiseaseDocument86 pagesAnaestetic Management of Liver DiseaseVarun Reddy VPas encore d'évaluation
- Evidencia Transfusion HemoderivadosDocument13 pagesEvidencia Transfusion HemoderivadosHernando CastrillónPas encore d'évaluation
- Fluid ManagementDocument10 pagesFluid ManagementdradaadPas encore d'évaluation
- Management of Dengue: Bridget WillsDocument22 pagesManagement of Dengue: Bridget Wills25172519Pas encore d'évaluation
- TURP SYNDROMEDocument9 pagesTURP SYNDROMEyaminduhairPas encore d'évaluation
- Perioperativefluid Therapy: Denise Fantoni,, Andre C. ShihDocument12 pagesPerioperativefluid Therapy: Denise Fantoni,, Andre C. ShihDaniela BenavidesPas encore d'évaluation
- Indications and Hemoglobin Thresholds For Red Blood Cell Transfusion in The Adult - UpToDateDocument39 pagesIndications and Hemoglobin Thresholds For Red Blood Cell Transfusion in The Adult - UpToDateAhmed MostafaPas encore d'évaluation
- Hemorrhagic ShockDocument5 pagesHemorrhagic ShockGhina RahmadiantiPas encore d'évaluation
- Dr. Sunatrio - Management Hypovolemic ShockDocument59 pagesDr. Sunatrio - Management Hypovolemic ShockArga Putra SaboePas encore d'évaluation
- Artikel Tramed InfusDocument7 pagesArtikel Tramed InfusZsa Zsa OllyviaPas encore d'évaluation
- Blood and Blood ComponentsDocument51 pagesBlood and Blood ComponentsMinlun ChongloiPas encore d'évaluation
- Artificial Blood and Blood Substitute Options ExplainedDocument34 pagesArtificial Blood and Blood Substitute Options ExplainedASHISH RANJANPas encore d'évaluation
- Blood TransfusionDocument74 pagesBlood Transfusiontefesih tube ተፈስሕ ቲዮብPas encore d'évaluation
- CH 19 Case Study 1 Answer KeyDocument3 pagesCH 19 Case Study 1 Answer KeyBryanPas encore d'évaluation
- Why Do Some Low-Dose Aspirin Formulations Intended For Use As Anti-Platelet Medications Contain Glycine?Document10 pagesWhy Do Some Low-Dose Aspirin Formulations Intended For Use As Anti-Platelet Medications Contain Glycine?Hueysha KhorPas encore d'évaluation
- The Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?D'EverandThe Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?Pas encore d'évaluation
- Investigations For Diseases of The Tongue A Review PDFDocument6 pagesInvestigations For Diseases of The Tongue A Review PDFShantanu DixitPas encore d'évaluation
- Hand Injuries & Their ManagementsDocument78 pagesHand Injuries & Their ManagementsKuruPas encore d'évaluation
- Pulse Oximetry: Review Open AccessDocument7 pagesPulse Oximetry: Review Open AccessAlain SoucotPas encore d'évaluation
- Schedule - Topnotch Moonlighting and Pre-Residency Seminar Nov 2022Document2 pagesSchedule - Topnotch Moonlighting and Pre-Residency Seminar Nov 2022Ala'a Emerald AguamPas encore d'évaluation
- Science ProposalDocument7 pagesScience ProposalDimple EstelPas encore d'évaluation
- Emergency Drug Doses - PBS Doctor's Bag Items - Australian PrescriberDocument4 pagesEmergency Drug Doses - PBS Doctor's Bag Items - Australian PrescriberChhabilal BastolaPas encore d'évaluation
- Ophthalmology 7th Edition (Oftalmología 7a Edición)Document1 671 pagesOphthalmology 7th Edition (Oftalmología 7a Edición)Víctor SaRi100% (1)
- Chronic Cough in Dogs: Published With The Permission of LAVC Close Window To Return To IVISDocument4 pagesChronic Cough in Dogs: Published With The Permission of LAVC Close Window To Return To IVISJuanEstebanOspinaPas encore d'évaluation
- Building An ArgumentDocument9 pagesBuilding An ArgumentunutulmazPas encore d'évaluation
- Tinea IncognitoDocument1 pageTinea IncognitoJana AtanasovaPas encore d'évaluation
- LESSON 1 and LESSON 2Document5 pagesLESSON 1 and LESSON 21234567werPas encore d'évaluation
- Cwu 1 OrthoDocument14 pagesCwu 1 OrthoHakimah K. Suhaimi100% (1)
- AFP Hemoptysis - 2022Document9 pagesAFP Hemoptysis - 2022Joshua DiaoPas encore d'évaluation
- Drug Price ListDocument68 pagesDrug Price ListYadi Vanzraso SitinjakPas encore d'évaluation
- Staples Worklife Magazine - Winter 2019Document68 pagesStaples Worklife Magazine - Winter 2019Anonymous fq268KsS100% (1)
- CBLM-BEAUTY CARE - FinalDocument75 pagesCBLM-BEAUTY CARE - FinalQuimby Quiano100% (3)
- One Compartment Open Model IV BolusDocument81 pagesOne Compartment Open Model IV Bolusanon_937994778Pas encore d'évaluation
- Lateral SMASectomy FaceliftDocument8 pagesLateral SMASectomy FaceliftLê Minh KhôiPas encore d'évaluation
- Psihogeni Neepileptički Napadi Kao Dijagnostički Problem: AutoriDocument4 pagesPsihogeni Neepileptički Napadi Kao Dijagnostički Problem: AutorifhdhPas encore d'évaluation
- The Woman in The Body A Cultural Analysis of ReproductionDocument299 pagesThe Woman in The Body A Cultural Analysis of ReproductionAndhra Shen100% (5)
- Nursing School Necessities Cheat SheetDocument3 pagesNursing School Necessities Cheat SheetRevPas encore d'évaluation
- ASHRAE Std 62.1 Ventilation StandardDocument38 pagesASHRAE Std 62.1 Ventilation Standardcoolth2Pas encore d'évaluation
- UntitledDocument221 pagesUntitledlaljadeff12Pas encore d'évaluation
- Diabetes and Hearing Loss (Pamela Parker MD)Document2 pagesDiabetes and Hearing Loss (Pamela Parker MD)Sartika Rizky HapsariPas encore d'évaluation
- Climate Change and National Security - Shakeel RamayDocument43 pagesClimate Change and National Security - Shakeel RamayBashir AhmedPas encore d'évaluation
- HIV Prevention: HSCI 225 BY Mutua Moses MuluDocument23 pagesHIV Prevention: HSCI 225 BY Mutua Moses MuluJibril MohamudPas encore d'évaluation
- HRFuture Sept 2020 MJLKJDocument59 pagesHRFuture Sept 2020 MJLKJGlecy KimPas encore d'évaluation
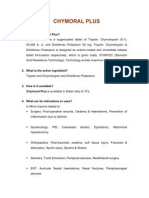
- Chymoral Plus'Document3 pagesChymoral Plus'Neha SureshPas encore d'évaluation
- Angina Pectoris: Causes, Symptoms and TreatmentsDocument17 pagesAngina Pectoris: Causes, Symptoms and TreatmentsGaming ModePas encore d'évaluation
- Vector and Pest Control in DisastersDocument10 pagesVector and Pest Control in DisastersTaufik RizkiandiPas encore d'évaluation