Académique Documents
Professionnel Documents
Culture Documents
PaperClaims FAQs
Transféré par
sa0063Description originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
PaperClaims FAQs
Transféré par
sa0063Droits d'auteur :
Formats disponibles
Frequently Asked Questions
MISSING/INVALID INFORMATION WHAT TO DO?
Days supply is the number of days medication is to be taken. This is not the quantity of medication dispensed. See below for quantity. Contact your pharmacy to obtain a new receipt or itemized printout that includes the days supply in addition to the quantity and directions for use. Once you have the receipt or itemized printout, please resubmit the original claim form and receipt or itemized printout for processing. As an alternative, you may contact your pharmacy for this information and write it on the claim form by hand. The NDC number is a unique 11-digit number assigned to each medication by the U.S. Food and Drug Administration (FDA). Contact your pharmacy to obtain a new receipt or itemized printout that shows the NDC number. Once you have the receipt or itemized printout, please resubmit the original claim form and receipt or itemized printout for processing. As an alternative, you may contact your pharmacy for this information and write it on the claim form by hand.
Days Supply
National Drug Code (NDC) Number
Original Receipts
Contact your pharmacy to obtain a new receipt or itemized printout. Please make sure the receipt or itemized printout includes the patients name, prescription number, date filled, dispensing pharmacy name and address, drug name, strength/form, quantity, ingredient cost, gross amount due, days supply and price. Once you have the receipt or itemized printout, please resubmit the original claim form and receipt or itemized printout for processing. An original cash register receipt is acceptable for diabetic supplies. The National Provider Identifier (NPI), National Council for Prescription Drug Programs (NCPDP) or National Boards of Pharmacy (NABP) number is the unique number assigned to each pharmacy. Contact your pharmacy to obtain a new receipt or itemized printout with their valid pharmacy number. Once you have the receipt or itemized printout, please resubmit the original claim form and receipt or itemized printout for processing. You also may contact your pharmacy for this information and write it on the claim form by hand. Your member ID number is found on your benefit ID card. Your member ID can't be located or matched in our system. Please provide the member ID number that was valid on the date the pharmacy filled the prescription. Always ensure the member ID is correct on the claim form you submitted. If you have additional questions, call the toll-free number on your benefit ID card. Every prescription is assigned a unique prescription number (Rx#) by the pharmacy. Contact your pharmacy to obtain a new receipt or itemized printout that includes the prescription number. Once you have the receipt or itemized printout, please resubmit the original claim form and receipt or itemized printout for processing. As an alternative, you may contact your pharmacy for this information and write it on the claim form by hand. Date of fill is the date the pharmacy filled the prescription. Contact your pharmacy to obtain a new receipt or itemized printout that includes the date the prescription was filled. Once you have the receipt or itemized printout, please resubmit the original claim form and receipt or itemized printout for processing.
NPI, NCPDP or NABP Number
Member ID Number
Prescription Number
Date of Fill
Quantity
Quantity is the total number of tablets, milliliters or grams of medication that was dispensed. Contact your pharmacy to obtain a new receipt or itemized printout that includes the quantity of your prescription. Once you have the receipt or itemized printout, please resubmit the original claim form and receipt or itemized printout for processing. You also may contact your pharmacy for this information and write it on the claim form by hand.
To avoid or reduce the likelihood of having to submit a paper claim in the future: Have your card available at the time you pick up your prescription Use a pharmacy that is within the network chosen by your plan sponsor Consider medication from your Preferred Drug List Refer to the claim form for required information Please note: Submission of the requested information does not guarantee payment of your claim.
106-16362a Revised 05/13/09
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Policies and Procedures For Sound-Alike and Look-Alike MedicationsDocument6 pagesPolicies and Procedures For Sound-Alike and Look-Alike Medicationsrelena badrPas encore d'évaluation
- Sasot vs. People GR No. 143193 (June 29,2005)Document11 pagesSasot vs. People GR No. 143193 (June 29,2005)Airah MacabandingPas encore d'évaluation
- 02-Pharmaceutical Care ProcessDocument42 pages02-Pharmaceutical Care ProcessBalsam Zahi Al-Hasan100% (1)
- Galafold - ProspectDocument45 pagesGalafold - ProspectgeorgepanciuPas encore d'évaluation
- Monazol, Ovule Spc-EngDocument6 pagesMonazol, Ovule Spc-EngAhmad Muhammad EmamPas encore d'évaluation
- Potassium - Sparing DiureticsDocument12 pagesPotassium - Sparing Diureticsrhimineecat71Pas encore d'évaluation
- CDC's Expiry List and Biologically Active Lots: by Craig PaardekooperDocument29 pagesCDC's Expiry List and Biologically Active Lots: by Craig PaardekooperMarco SalviPas encore d'évaluation
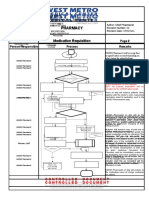
- Pharmacy Pharmacy: Medication Requisition Medication RequisitionDocument1 pagePharmacy Pharmacy: Medication Requisition Medication RequisitionSharie Grace ImlanPas encore d'évaluation
- Direct Detection For Concentration Ratio of HbA1c To Total HemoglobinDocument4 pagesDirect Detection For Concentration Ratio of HbA1c To Total HemoglobinNur Aisyah Karima100% (1)
- Methods of Drug ClassificationDocument11 pagesMethods of Drug ClassificationArvic Pascua MaltizoPas encore d'évaluation
- Rasagiline Hemitartrate: Synthesis, Characterization and RP-HPLC Validation For Its Estimation in Bulk FormDocument6 pagesRasagiline Hemitartrate: Synthesis, Characterization and RP-HPLC Validation For Its Estimation in Bulk FormRatnakaram Venkata NadhPas encore d'évaluation
- Moh Approved ListDocument108 pagesMoh Approved ListninadbhidePas encore d'évaluation
- Daftar Harga ObatDocument4 pagesDaftar Harga ObatKadek Soga Prayaditya PutraPas encore d'évaluation
- Bactericidal Activity of Flavonoids Isolated From Muntingia CalaburaDocument7 pagesBactericidal Activity of Flavonoids Isolated From Muntingia CalaburaSSR-IIJLS JournalPas encore d'évaluation
- CMC Review - XolairDocument71 pagesCMC Review - XolairMing GuPas encore d'évaluation
- Drug Information Bulletin 52 06Document10 pagesDrug Information Bulletin 52 06amritaryaaligarghPas encore d'évaluation
- Drugs (Licensing, Registering and Advertising) RULES, 1976Document61 pagesDrugs (Licensing, Registering and Advertising) RULES, 1976sadafPas encore d'évaluation
- Gees Linctus: What Is in This LeafletDocument7 pagesGees Linctus: What Is in This LeafletAlvin bissetPas encore d'évaluation
- National DP 2016 E VersionDocument27 pagesNational DP 2016 E VersionRiky HidayatPas encore d'évaluation
- Lagochilascar Ecuador 98Document2 pagesLagochilascar Ecuador 98MaikellSegoviaPas encore d'évaluation
- Plasma Protein BindingDocument2 pagesPlasma Protein BindingKavish ChhajedPas encore d'évaluation
- LevemirDocument36 pagesLevemirsigitPas encore d'évaluation
- Pharmacy 1 Year Pharmaceutics 1 2111 Dec 2019Document2 pagesPharmacy 1 Year Pharmaceutics 1 2111 Dec 2019Sachin NagarPas encore d'évaluation
- Index From Desperate HousewivesDocument9 pagesIndex From Desperate HousewivesPickering and ChattoPas encore d'évaluation
- Carrier-Based Strategies For Targeting Protein and Peptide DrugsDocument22 pagesCarrier-Based Strategies For Targeting Protein and Peptide DrugsKaragate KomintaPas encore d'évaluation
- Introduction To Pharmaceutics: Rashid Ali Arbani Pharm-D, Mphil (Pharmaceutics) Lecturer SALUDocument14 pagesIntroduction To Pharmaceutics: Rashid Ali Arbani Pharm-D, Mphil (Pharmaceutics) Lecturer SALUSimmiPas encore d'évaluation
- Handouts For Drug CalculationDocument19 pagesHandouts For Drug CalculationEmeroot RootPas encore d'évaluation
- Kofarest LS SyrupDocument3 pagesKofarest LS SyrupGAUTAMPas encore d'évaluation
- Powers, Duties & Qualification of Drug Inspector PDFDocument4 pagesPowers, Duties & Qualification of Drug Inspector PDFNuwaira Baloch63% (8)
- Annex I Summary of Product CharacteristicsDocument54 pagesAnnex I Summary of Product CharacteristicsDr. RajibPas encore d'évaluation