Académique Documents
Professionnel Documents
Culture Documents
Immuno - Lec 7
Transféré par
www_rooro_30Description originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Immuno - Lec 7
Transféré par
www_rooro_30Droits d'auteur :
Formats disponibles
MHC
25 77 7
Ziad AlIbrahim Monday, Migdady Nasser 11/7/2011
MHC
Ibrahim Migdady Ziad Al-Nasser Monday, 11/7/2011
Immunology Monday, July 11th. By:- Ibrahim Miqdady (A long unsure-about introduction/revision ahead! Don't judge upon it, the lecture is nice. Sit back, relax and play some Yanni's!). We had been discussing so far the antigen recognition molecules, immunoglobulin, T-cell receptors. And today we'll be talking about MHC. We talked about antigens and antibodies and their nature, structure, diversity and we discussed in details how we answered their question how did we get to the number 10^11 different specificities of immunoglobulin, and also we had concentrated on when we talked about the specificity on the variable region, and the V region is the one that determines the specifity while the constant region is the one that determines the biological function. And going form that concept into the variable region which is formed of variable genes (joining genes of the light and joining genes of the heavy chains) and how those genes get rearranged and one of the them is going to be selected. Also we talked about in the primary immune response how the first antibody is developed as a monomer of IgM and how a monomer of IgD is going to be present on the surface in order to complete the function of the T-cell receptor. So the first antibody that's going to develop is the IgM monomer, whether it was surface or it is going to be excreted it depends on the part that is going to be activated; the one that goes to the cytoplasmic membrane. And the simple immune response here, that the other constant genes (gamma 1,2,3 .. alpha 1,2 .. epsilon) all are there. They have not been deleted. In the secondary immune response there'll be the isotype switching or class switching where the variable region stays the same, only in the development instead of selecting Mu or Delta, one of the others will be selected and the rest will be deleted. So that particular cell will be committed in the secondary immune response to produce antibody of the same specifity of the IgM and IgD, the difference here is in the constant region. And what really triggers this switch into that area depends on the cytokines that are produced and how cytokines are going to modify the cell and switch that particular areas. (e.g. To produce IgE antibody interluken 4 is required which comes from T-helper cell. ) I want you to remember that in the secondary immune response isotype switching is going to take place to produce a new antibody for that antigen. So advanced functions are going to take place in the secondary immune response. So remember when we talk about isotype switching we mean keeping the variable region which is very specific constant (not changed), we only switch from (Mu,Delta) into others. And the switching here is by the action of cytokines that are produced by the T-helper cells. The other constant genes are going to be deleted. That memory cell will keep producing only that particular antibody isotype. We also talked about the allelic execlusion And how these allotypic markers can be inherited one from each parent but one of them only is going to be expressed and the other is going to be deleted or non-functional so we don't see it. We talked about the idiotypic antibodies and the significance of the hypervariable region. And in comparison with the T-cell receptors where we have 2 types. TCRs are formed of two peptides (alpha
and Beta) that are forming 95% of the TCR-1 and 5% of TCR-2 (gamma and delta). (not sure of what he said!). And I told you the number of those genes responsible for those regions, they are so many, so the diversity is going to be much much higher. The difference between (Gamma Delta) and (alpha beta) is that the first is less specific; non-polypeptide antigens can be presented (mainly on the skin or the mucus membranes rather than other tissues) .. and here the difference is that we aren't going to have what we call ''somatic hypermutation";a better fit. We said that in the TCR requires that the antigen has to be presented with a MHC, while those others can bind without that MHC. And finally about the molecules that are so important for the function of the T cell. We talked about the Cluster Designation/Differentiation Antigens (The CD system; 1,2,3,4) ; we consider them as cell markers, and each one of those have special function in the context of its presence (where it comes). For example when I say CD2, this is present on all lymphocytes (irrespective of the type of that lymphocyte I can target the CD2). CD3 is so important for the signal transduction and present on all T cells. CD 4 is present on Thelper cells. We said how the CD4 plays a major role in the function of the T-helper and how it has to match with Class 2 MHC . While CD8 (T-cytotoxic cells) has to match with class 1 MHA. You will see how the matching is so important for the signal to pass through into the cell, and also the lymphocyte functional antigen, the ICam-1 and so on. We said those are so important accessory molecules and if we are lacking any of those we are going to have immune compromise condition; diseases. Or if one of the enzyme we have talked about is missing ; RAG1 or 2 that is very important for the gene rearrangement at the germ line ; the patient is going to be immune-deficient, and the diseases that are associated with those. TODAAAAAAAAY (yes, finally!) we will be talking in more details on the third part of the antigen recognition molecules. And those differ from antibodies and T-cell receptors in that they are not that specific compared to those two. They are simply proteins that are coded by genes present on the short arm of chromosome 6. Each of us have on chr6 areas of genes (called loci). Those genes are divided into 3 classes; class 1,2 and 3. The ones that are involved in the immune system are simply class 1 and class 2. Class 3 might be involved in other things; enzymes, some complement components.... So we are talking about classes; we called them loci on the chromosome, and those areas have different allelic forms; variations of the same gene. And we inherit those allelic forms from our parents; half from each. So both are going to be expressed on the surface of that cell. It's important to differentiate this from the allelic exclusion. If the mother and the father are related to each other, then the chance that these variations will be less, and vice versa. Many allelic forms are present, each one of us will have two of these allelic forms, so the total number in type 1 MHC is 6 forms and minimum of 3. And in class 2 the same thing, a minimum of 3 and a maximum of 6; with a total of 12 (Maximum) to 6 (Minimum). And those form what we call a haplotype (It is a combination of alleles at 3
different places (loci) on the chromosome that are transmitted together); its like a stamp for each one of us, those antigens that are expressed we call them HLA antigens; or transplantation antigens, or MHC antigens. The major role of those HLA antigens is to regulate the immune response, its not that their role is just to reject grafts. Rejection of a graft is one of the mechanisms of our immune system; that those grafts are foreign so we don't want them to be there. If they are similar to our tissue then we want them to be there, or we can modify our immune system to accept those tissues and so on. Remember that all MHC antigens that we have on our tissues are the same, and those are determined by our genetic setup that we have inherited from our parents. If yours and mine are the same then we can exchange grafts, if different then we are going to reject grafts from each other. We are talking about genes on chromosomes. The Short arm of chromosome number 6 codes for proteins; Class 1 and Class 2 MHC genes. Class 1 codes for a single polypeptide chain; alpha (45 kD) attached to it a 12 kD Beta-2 microglobulin that has nothing to do with the function of the alpha chain; it just adds up support to the Alpha chain; it will make it do its function much better, and its coded by a different chromosome rather than chromosome 6. Any nucleated cell in our body is going to have class 1 MHC antigen. So RBCs do have neither class 1 nor class 2, and this makes them easy to be transplanted; we don't have to look for MHC because they are not expressed on the surface of the cell, but they are present on the surface of white blood cells; because they are nucleated.
# So does our body produce antibodies against HLA antigens on white blood cells when we do blood transfusion? Yes of course! But those are not going to annoy us, because when we do blood transfusion we are concerned about RBCs, we are not concerned with the WBC; those might sometimes cause a little of fever. Class 1 is present on all nucleated cells of our body and class 2 is present on the surface of the antigen presenting cells (APCs), so the APCs are going to have class 1 and class 2, while others are only going to have class 1. 4
Class 2 are formed of 2 polypeptide chains; alpha and beta. And those are going to be present on APCs of our body. The MHC molecules are concerned with antigen recognition, we will see that in each allelic type the shape of the alpha and the groove that they form has to do with antigen recognition, so the antigen has to fit in the groove between alpha1 and alpha2 domains , and this is going to be presented onto a T-cell, so heres what I called dual recognition; one recognition on MHC; the group has to fit to the antigen, and the other side, you need the Tcell receptor to go in into the MHC antigen and the antigen at the same time. So were talking about antigen-recognition antigen, in humans we call it the HLA (Human Leukocyte Antigen), in Murines, mice and so on we call them H2, in dogs they have different name etc. On the Short arm of chromosome number 6 we have areas called loci; three loci for class 1 [ locus A, B and C] and other 3 for class 2 [DP, DQ, DR]; and these have extensive polymorphism meaning that people are so diverse of the HLA antigen, so its so difficult to have a match (i.e. tissue match) and here when we say polymorphism we mean many different haplotypes; and this haplotype is what we need to identify when we do tissue transplantation; identify the map (haplotype) for each the donor and the receptor, and if they match then we accept the grafts, but if they dont, the grafts will be ultimately rejected.
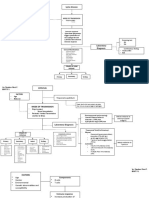
This is the short arm of chromosome number 6 here, this is the centromere over here (can you see it? I can't. blah!) , this is how those genes are located, and in the farthest end we have locus A then C then B , so remember B, C, A just going to the end here. And then we have class 3, then class 2, this is how those are arranged. So class 1 encoding molecule that present the antigen to the T cytotoxic cell (CD8+ T cells); this is the main function of class 1 MHC, and it makes sense (Ah sure does!); class 1 MHC antigen 5
is located in all nucleated cells, if these cells are tumor cells or virally infected cells then their antigen has to be presented with class 1 MHC antigen to the T cytotoxic cell, so the T cytotoxic cell will refuse to do the killing unless the tumor or virally infected cell is presented with class 1 MHC antigen. Locus A has many different allelic forms, maybe the highest number is for locus B ('maybe' he said!) , over 7oo or 1000,and you are going to have two of each, one from the father and one from the mother, remember that; for the B, for the C and for the A, I think the C is the lowest, but the majority of allelic forms are present in B, and every year they discover new allelic forms and they add them up. Class 3 is able to encode complement or cytokine molecules, and some other enzymes for steroid metabolism, proteins and so on. Then we have class 2, and as you can see class 2 MHC antigens are formed from two chains, alpha & beta, and as you can see the DR, DC, & DQ); (check the figure above), this is how they are arranged. And in between in class 2 we have areas that will code for proteins that are needed for the processing of the MHC antigens like the low molecular weight protein LMP, and the transporter associated protein TAP. Those (LMP and TA) are needed genes involved in antigen processing; they process the antigen, and then they will be mixed with the MHC, and then it will be presented to the T helper cell. This is all present in the short arm of chromosome 6. (Remember that in Class I MHC antigens in locus A, B, & C, in each of these there are two allelic forms; one from the father and one from the mother.) These are the different allelic forms that we inherit from our parents on each locus; locus A has 414 different allelic forms, we have two of those on the surface of our cells. On locus B we have over 700 (around 1000 of those have been discovered). Locus C is the lowest ; 210 different allelic forms. And then we talk about Class two (DP,DQ,DR); alpha and beta. And you can see how many allelic forms and the variations that we're going to get. The DRbeta is the highest form (over 500 different allelic forms). The MHC genes are extensively polymorphic. We have so many of those in the human population; existence of multiple alleles at a locus; 2 at each locus for one person. HLA-B and DR-beta are the most polymorphic loci shown here.
This inheritance is a comdomionance type of inheritance, and you can see here the chromosomes (diploid) . (The child is different from the father and from the mother)
For example if I want to do a transplantation from child (1) to child (2) , actually you are going to introduce something foreign into the other child, while for example if we introduce from the mother or the father into the child then this is accepted much better in a away, because here the amount of tissue that will be added at least matches half of the genes that the mother or father have. None of family members have identical combinations of HLA alleles and thats the main reason why tissue transplantation is difficult. The easiest way for transplantation is to have a match between haplotypes and the best place to have a 100% match is to use a tissue from one place from our body to another. This is done in birds.
Autologous; taking a tissue from one place in your body and transplant it on another place, for example in our hospital we do autologous bone marrow transplantation; we take the bone marrow of the patient out and then you expose the patient to radiotherapy, cytotoxic drugs, or make suppression. Then the bone marrow is transferred back to the body. So autologous is the one that have almost 100% match with almost no reactions at all. Syngeneic; in the case of identical twins. The haplotypes are the same in this case. So we can take grafts without any problem. Allogeneic ; You have to do the haplotype for the donor and the recipient to get the best match. Its impossible to find a 100% match but some choices are better than others (e.g: parent to child, brothers and sisters, 1st cousins then 2nd cousins and so on). Those are genetically diverse. Xengeneic. Animals are used and the pig is the closest animal genetically to human. The immune system of pigs is almost
identical to immune system of humans. So insulin body samples and heart valves were used in the past, which were taken from pigs. Now they are trying to have to transplant pigs heart into human, but to do that they have to make the patient severely immune suppressed in order to accept the grafts. This is the expression of the genes when you inherit them. You can see the haplotypes; for the father the green and blue (no colors? You need to have a wide imagination!), and for the mother the pink and the orange. And the child has one from the father and one from the mother and both will appear on the surface. So there will be diversity and the children wont have identical haplotypes as those of the parents.
( the figure above) So when we look at the structure of class 1 MHC; -> Class 1 is composed of: 1) a single polypeptide chain (alpha chain); which has 3 domains alpha 1, alpha 2 and alpha 3 and its about 45,000 daltons. Which are external. 2) Another part that goes inside the endoplasmic membrane. 3) And theres another protein thats called beta 2 microglobulin which is around 12,000 dalton and is adherent to alpha chain. This protein is encoded on chromosome number 15. 4) The sensitive part thats going to bind is between alpha 1 and alpha 2 domains. After the intake of the antigen by the cell it will be processed and presented to the surface with class 1 MHC antigen. So we need to present that to the T cytotoxic cell that has CD8 on its surface. (The doctor started to give further explanation about the same figure) > In a 3D structure youll see that alpha 1 and alpha 2 represents a groove , if you have more grooves here (or polymorphism) then the possibility of helping in the immune system is higher.
For example; the presence of 6 grooves is better and stronger than 3. Here we are talking about the shape of the groove; alpha1, alpha 2, alpha 3 and so on. You can see the beta 2 microglobulin and that the beta pleated sheat is going to fit into that. Many of the polymorphic amino acids in MHC class 1 are found here. This molecule structure doesnt include the membrane standing region of the alpha chain. Beta 2 microglobulin is the protein required for folding and expression of class 1 molecules. The alpha 3 domains and the Beta 2 microglobulin pair to form a region of a very similar immunoglobulin domain. So the structure of that belong to the immunoglobulin supergene family. You can see domains like these in immunoglobulins, variable region and a constant region (very similar to immunoglobulin ).
( figure above) Class 2 : There are 2 polypeptide chains alpha (1 &2) and beta (1&2). The sensitive part here is between alpha 1 and beta 1 which will fix into the antigen. This is on the surface of antigen presenting cell (APC); (e.g. macrophage, dendretic cell or B cell). These APC present the antigen to T helper cell which must have a T cell receptor that fits the antigen and CD4 and this CD4 antigen must match that of class 2 MHC antigen. This is the most specific part forming the groove between alpha 1 and beta 1. The regulation of the gene expression of class 1 MHC antigens is on locus A, locus B, locus C antigens. And of class 2 MHC antigens is on DP, DQ, DR. Characteristics of gene expression of MHC antigens: o Co-dominant mode of inheritance; half from the father and half from the mother. o They are very similar to Immunoglobulins and TCRs in their specificity, so we have dual recognition; which means that the antigen must fit in the groove of MHC antigen and then to be presented on T cell .
o Theres no Allelic exclusion. Unlike Immunoglobulins and TCRs. So both genes are going to be expressed on the surface.
Structures of MHC Ags:
Class 1 alpha chain (around 45 kD) is attached to B2 globulin that comes from other chromosome, allelic forms have more than 90% similarity (e.g. between A1 & A2) so the specificity difference between the alleles is about 10% , this 10% is important but its minor . (This is different than in the antibodies and the TCR allelic forms), the resulting groove will be shallow in a way so that it will accept many antigenic determinants. No gene rearrangements is going to take place, both is going to be expressed. Precise sequence vs. amino acid residues; here the precise sequence is very important in the immune recognition and response. Class II : consist of two polypeptide chains (33 kD ) and (29 kD) chains, in addition to the trans-membrane glycoproteins. MHC molecule can accommodate a wide range of peptides (one at a time); as long as you have 90% similarity, a wide range of peptides can fit in that groove.
Antigen recognition restriction
The antigen has to be presented with a self MHC in order to bind with the TCR, so the antigen-MHC complex has to fit in the receptor of the T-cell, meaning the T-cell is specific for both of them (the antigen and the MHC together form a new shape to fit in the t-cell receptor) and this is called restriction rule. MHC must be self and this is the dual recognition of the T-cell, if the MHC was nonself , the immune response will not take place. The selection of the self MHC to bind with the antigen takes place in the thymus gland, so the thymus recognizes the self MHC and the strength of binding so that the self MHC will be released in the circulation and the modified or the non-self MHC will be deleted or become anergic, and any problem in this process will lead to the development of an autoimmune phenomena. The MHC has a binding site for non-self antigen, the antigen has to be non-self (foreign) and together they form a ligand for T-cell receptor . So the formula is simple: non-self antigen binds with a self MHC both binds with the TCR.
10
This picture emphasizes the idea of the dual recognition. The one on the left is the normal case where the non-self antigen binds with the self MHC and together fit in the TCR and this is the only case where the t-cell will be activated to do its killing functions. In the middle, the MHC is non-self so the complex is not going to fit in the TCR and on the right , the antigen does not match the specificity of the self MHC, also no immune response is going to take place
( .. continue Antigen recognition restriction) Altered peptide ligand used for treatment : the antigen that is going to fit in the TCR has to have all the characteristics mentioned above in order for the immune response to take place , sometimes If I dont want the immune response to take place , I could modify the antigen so it wont have a perfect fit , this altered antigen can be used as a vaccine in order to suppress the immune system (suppression of the immune system is needed when the patient is suffering from an autoimmune disease like multiple sclerosis and others we ). If I know the antigen that is going to bind with the lymphocyte and I modified it so it doesnt have a perfect fit , its going to give a negative signal and the lymphocytes will not be stimulated (immune suppression).
This is the normal immune response having the target cell, MHC, antigen and TCR. If magnified the picture, you can see the yellow antigen binding to specific areas of the green class I MHC and both the antigen and the MHC bind to the TCR in specific places as well. (No need for imagination here, it's pretty clear without the colors!). So if you altered the antigen in a way it will
11
give a negative signal that will not let the T-cell to be activated, release its cytokines or to act against the antigen. As you can see amino acids side chains from the peptide antigen interact with MHC and TCR and the MHC interacts with peptide antigen (anchor residues) and the TCR.
Also, they have noticed that certain autoimmune diseases have association with certain HLA alleles; this is called relative risk: meaning that having a certain HLA may increase the risk of having this specific autoimmune disease For example: - Both Positive and Negative P27 people can develop Ankylosing Spondylitis but people who have HLA P27 (positive) are at higher risk (90 times) of developing Ankylosing Spondylitis than those who dont have P27 (negative). P27 is a risk factor of Ankylosing Spondylitis. Its like saying smokers are at higher risk (120 times) of developing lung cancer, some smokers develop cancer and others dont but they all at a higher risk of developing it. Ankolosing spondalitis is an autoimmune disease where antibodies attack intervertebral disks and cause a problem with bending of vertebral column. We use the term bamboo spine to describe this because their vertebral column is not flexible just like bamboo. It seems that p27 allelic form patients have a modification in a way with other factors that will let their immune system to develop antibodies more in those patients compared to others. - In Insulin-dependent diabetes mellitus where PQ2 allelic form are at higher risk of it. The Ig will attack the beta-langerhan cells in pancreas. Why do they do so ? Some say Coxsackie B virus could attack and then the immunoglobulins for Coxsackie B virus will cross react with beta-langerhan cells, or sometimes other infections will cross react with beta-langerhan cells, complement will be activated and cells will disappear. PQ2 positive are at higher risk compared to PQ2 negative people. - In Multiple sclerosis PR2 allelic form are at higher risk compared to PR2 negative, myelin sheath will be attacked by our immune system. - Acne vulgaris is a skin disease where skin will be attacked. - In RA the synovial membrane of joints will be attacked by our immune system. And SLE where anti-DNA Ig against DNA and so the cells they will be broken and complement activated and PMN will be called into the area and damage could be occur systematically.
CH.9: Review of Ag recognition
This chapter is a review of the previous three chapters. We talked about: Ig, TCR, MHC all are antigen recognition molecules which means they all are specific and members of Ig family and its members all have Ig domain. -MHC:polymorphism/diversity, co-dominant expression.
12
-TCR: recombination/diversity. - Ig: recombination/diversity, somatic hypermutation.
In the figure to the right you can see: - Ig : made of 4 polypeptide chains; 2 light, 2 heavy. -TCR: alpha, beta, gamma and delta. You can see a specific part between alpha and beta. - MHC class 1 and 2. - KIR we will talk about it later. - CD4, CD8 and ICAM. All these proteins belong to Ig supergene family.
(Now dr.Ziad just read the tables from the remaining slides PLEASE go and read them. And remember in Table 1: You should know where D gene exisst: in Igs heavy chain and in TCRs beta and delta gene; that's what he said). ~ That's it for today, thanks for enjoying the lecture, I know # Yousef Odeibat I would like to do what you demanded but; putting your pic over here is not really a good thing to do, no need for more followers you know :D Thanks my great friend for your great help # Oday Younes I appreciate the effort your artistic fingers have done for me, keep up the good music my friend<3 # And to the crazy driver (they say :D ), and to the future painter wannabe. And at last but not least, to the in-search-of-madhouse boy<3
There is in every madman a misunderstood genius whose idea, shining in his head, frightened people, and for whom delirium was the only solution to the strangulation that life had prepared for him. -Antonin Artaud
By: Ibrahim Miqdady
13
Vous aimerez peut-être aussi
- Impression Material Lecture3student 2Document30 pagesImpression Material Lecture3student 2www_rooro_30Pas encore d'évaluation
- Material PropertiesDocument51 pagesMaterial PropertiesAbdallah Essam Al-ZireeniPas encore d'évaluation
- Immunology Lecture #2Document19 pagesImmunology Lecture #2Dr-Rmz RabadiPas encore d'évaluation
- Immuno - Lec 9Document18 pagesImmuno - Lec 9www_rooro_30Pas encore d'évaluation
- Immuno - Lec 8Document9 pagesImmuno - Lec 8www_rooro_30Pas encore d'évaluation
- Immuno - Lec 1Document15 pagesImmuno - Lec 1AbeerDirawiPas encore d'évaluation
- Immuno - Lec 10Document19 pagesImmuno - Lec 10www_rooro_30Pas encore d'évaluation
- Immuno - Lec 5Document18 pagesImmuno - Lec 5www_rooro_30Pas encore d'évaluation
- Immuno - Lec 6Document20 pagesImmuno - Lec 6www_rooro_30Pas encore d'évaluation
- Immuno - Lec 4Document14 pagesImmuno - Lec 4AbeerDirawiPas encore d'évaluation
- Immuno - Lec 3Document15 pagesImmuno - Lec 3AbeerDirawiPas encore d'évaluation
- Immuno - Lec 3Document15 pagesImmuno - Lec 3AbeerDirawiPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- MT632 Unit 1 Introduction Human Anatomy and Physiology Chapter 1 The BasicsDocument12 pagesMT632 Unit 1 Introduction Human Anatomy and Physiology Chapter 1 The BasicsTia MallariPas encore d'évaluation
- CCO TNBC Immune and Targeted Downloadable 3Document15 pagesCCO TNBC Immune and Targeted Downloadable 3Yasar HammorPas encore d'évaluation
- Illuminating The Mother of Qi: Intravenous and Transcutaneous Laser Blood Irradiation As Well As ExtracorporealDocument0 pageIlluminating The Mother of Qi: Intravenous and Transcutaneous Laser Blood Irradiation As Well As ExtracorporealfghjhgfPas encore d'évaluation
- Human Inborn Errors of Immunity: An Expanding Universe: ReviewDocument17 pagesHuman Inborn Errors of Immunity: An Expanding Universe: ReviewCony GSPas encore d'évaluation
- Smolen 2016Document16 pagesSmolen 2016downloadcmpPas encore d'évaluation
- Vitamin D in Hashimoto's Thyroiditis and Its Relationship With Thyroid Function and Inflammatory StatusDocument9 pagesVitamin D in Hashimoto's Thyroiditis and Its Relationship With Thyroid Function and Inflammatory StatusMedicina UNIDEP T3Pas encore d'évaluation
- Biology ThesisDocument25 pagesBiology ThesisValli RamalingamPas encore d'évaluation
- Copa (Inglés)Document10 pagesCopa (Inglés)XIMENA ORTIZ MARTINEZPas encore d'évaluation
- Antinuclear Antibodies (ANA) : Fast FactsDocument4 pagesAntinuclear Antibodies (ANA) : Fast FactsLucille Isidro CruzPas encore d'évaluation
- Systemic Lupus ErythemathosusDocument23 pagesSystemic Lupus ErythemathosusFransisca HardimartaPas encore d'évaluation
- ANA PatternsDocument11 pagesANA PatternsSathish KumarPas encore d'évaluation
- Autoimmune Encephalopathies and Dementias Continuum 2016Document21 pagesAutoimmune Encephalopathies and Dementias Continuum 2016Habib G. Moutran BarrosoPas encore d'évaluation
- Pathophysiology of Selected Autoimmune Diseases: Lecture From Pathological Physiology November 11, 2004Document50 pagesPathophysiology of Selected Autoimmune Diseases: Lecture From Pathological Physiology November 11, 2004Meity ElvinaPas encore d'évaluation
- Catalytic Antibodies PDFDocument16 pagesCatalytic Antibodies PDFKc ChiangPas encore d'évaluation
- Handbook of Multiple Sclerosis 4th Ed - S. Cook (Taylor and Francis, 2006) WW PDFDocument546 pagesHandbook of Multiple Sclerosis 4th Ed - S. Cook (Taylor and Francis, 2006) WW PDFGigiEnergie100% (1)
- Plasmapheresis For AutoimmunityDocument14 pagesPlasmapheresis For AutoimmunityEliDavidPas encore d'évaluation
- (03241750 - Acta Medica Bulgarica) T Helper Cells in The Immunopathogenesis of Systemic Sclerosis - Current TrendsDocument7 pages(03241750 - Acta Medica Bulgarica) T Helper Cells in The Immunopathogenesis of Systemic Sclerosis - Current TrendsTeodorPas encore d'évaluation
- Autoimmune Hepatitis - SLE Overlap SyndromeDocument2 pagesAutoimmune Hepatitis - SLE Overlap SyndromeMulyono Aba AthiyaPas encore d'évaluation
- Pink Panther - Diabetes Management - Chapter 3Document6 pagesPink Panther - Diabetes Management - Chapter 3jennmoyerPas encore d'évaluation
- Autoimmunity and Autoimmune DiseasesDocument89 pagesAutoimmunity and Autoimmune DiseasesImmas Wahyu FajariniPas encore d'évaluation
- Handbook of Multiple SclerosisDocument546 pagesHandbook of Multiple SclerosisLaura FrenchieChan100% (4)
- Autismo y AutoinmunidadDocument50 pagesAutismo y AutoinmunidadPsicoterapia InfantilPas encore d'évaluation
- Hallowell Et Al-2016-Annals of The American Thoracic SocietyDocument7 pagesHallowell Et Al-2016-Annals of The American Thoracic SocietyDmitri KaramazovPas encore d'évaluation
- Cell - 28 July 2016Document262 pagesCell - 28 July 2016Paulo EstevãoPas encore d'évaluation
- Mixed Connective Tissue DZ (SLE + Scleroderma)Document7 pagesMixed Connective Tissue DZ (SLE + Scleroderma)AshbirZammeriPas encore d'évaluation
- Rheumatological Manifestations in HIV Infection: Review ArticleDocument9 pagesRheumatological Manifestations in HIV Infection: Review Articlemonica mahechaPas encore d'évaluation
- Concept MapDocument10 pagesConcept MapStephen YorPas encore d'évaluation
- A Case of Subcorneal Pustular Dermatosis Successfully Treated With AcitretinDocument3 pagesA Case of Subcorneal Pustular Dermatosis Successfully Treated With Acitretindr_RMPas encore d'évaluation
- WADIA S LeucodermaDocument22 pagesWADIA S LeucodermasgfdsgegPas encore d'évaluation
- Theories of Aging 1Document8 pagesTheories of Aging 1Jake CaballoPas encore d'évaluation