Académique Documents
Professionnel Documents
Culture Documents
Sanitization of Pharmaceutical Facilities
Transféré par
Tim SandleCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Sanitization of Pharmaceutical Facilities
Transféré par
Tim SandleDroits d'auteur :
Formats disponibles
Sanitization of Pharmaceutical Facilities
By Dr. Tim Sandle (E-mail: timsandle@btinternet.com / website: www.pharmamicro.com) Introduction This paper provides an introduction to the sanitization and biodecontamination of pharmaceutical facilities. Pharmaceutical facilities are made up of a series of rooms called cleanrooms. Cleanrooms and zones are typically classified according to their use (the main activity within each room or zone) and are confirmed by the cleanliness of the air by the measurement of particles. Cleanrooms are used in several industries, including the manufacture of pharmaceuticals and in the electronics industry. For pharmaceutical cleanrooms, air cleanliness is either based on EU GMP guidance for aseptically filled products, and the EU GMP alphabetic notations are adopted; or by using the International Standard ISO14644, where numerical classes are adopted. The cleanliness of the air is controlled by an HVAC system (Heating, Ventilation and Air Conditioning).
July 2012 GBPR, Inc. Newsletter
Evelyn Heitman, Editor
Figure 1: Processing within a pharmaceutical cleanroom (c) Tim Sandle Cleanrooms are designed to minimize and to control contamination. There are many sources of contamination. The atmosphere contains dust, microorganisms, condensates, and gases. Manufacturing processes will also produce a range of contaminants. Wherever there is a process which grinds, corrodes, fumes, heats, sprays, turns, etc., particles and fumes are emitted and will contaminate the surroundings (1). Maintaining environmental control in a pharmaceutical manufacturing environment is in large part dependent on the facilitys cleaning and disinfection program. The program requires the selection of the appropriate disinfectants, their proper application, and validation of their capability to inactivate vegetative cells.
July 2012 GBPR, Inc. Newsletter
Evelyn Heitman, Editor
Types of Sanitization Room Sanitization Cleanrooms and clean areas must be regularly cleaned and disinfected. This is normally undertaken using a detergent step, followed by the application of a disinfectant. It may be necessary to remove the residue of the disinfectant using water. When cleaning rooms, the equipment used (mops and buckets) should be of an appropriate design for the grade of cleanroom. When undertaking cleaning, a strict cleaning regime should be followed. Cleaning and disinfection using cloths and mop heads is ideally performed by saturating the cleaning item and wiping the area using a series of parallel, overlapping strokes (with an approximate one-quarter overlap)-never in circular motions. The direction of the cleaning should be towards the operator (from top to bottom, from back to front). Only one application of the disinfectant or detergent should be applied to avoid overconcentration. Cleaning and disinfection should begin with the visually cleanest area first, and towards the dirtiest area last. Cleaning is normally undertaken in each process area before use. In general, the frequency of cleaning should be established through risk assessment. Equipment Sanitization Effective cleaning and sanitization of equipment is important, because equipment may not be amenable to visual inspection, and it may be prone to biofilm formation. The main method for cleaning industrial equipment is by making the mechanism for cleaning integral to the equipment itself. This can be achieved by use of pressure, heat, steam sterilization, mechanical removal, or chemicals, and is termed Clean-inPlace (CIP) or Steam-in-Place (SIP). Prior to chemical or heat treatment, attempts must be made to remove process residues and particles using steam or high-pressure water cleaning. Alkali-based disinfectants and detergents are commonly used for CIP systems, with sodium hydroxide among the most widely used. Such caustic alkalis can readily remove organic deposits without affecting the equipment. It is important that equipment cleaning is validated. Glove Sanitization For staff undertaking critical activities, gloved hands should be sanitized on a frequent basis using an effective hand sanitizer. Disinfected glove hands can aid staff who needs to carry out aseptic practices, although the sanitizing agent itself is not a replacement for poor aseptic technique.
July 2012 GBPR, Inc. Newsletter
Evelyn Heitman, Editor
There are many commercially available hand sanitizers, with the most commonly used types being alcohol-based gels. To ensure that the hand sanitizer selected is effective, within Europe there is a standard describing the approach for their validation [EN 1499 (2) and EN 150025A (3)]. The test determines if a hand sanitizer can reduce the number of transient microflora under simulated practical conditions. The standard outlines the approach for the evaluation of hygienic hand rubs. Most hand sanitizers are ethanol or isopropanol alcohol based (4). There are three key variables that affect the use of hand sanitizers. These are the act of agitation and rubbing the hand sanitizer into the glove, the frequency of application, and the quantity applied (5).
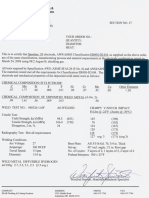
Figure 2: Testing sanitizing agents in a microbiology laboratory (c) Tim Sandle
July 2012 GBPR, Inc. Newsletter
Evelyn Heitman, Editor
Types of Sanitizing Agents A disinfectant is one of a diverse group of chemicals which reduces the number of microorganisms present (normally on an inanimate object). Disinfectants kill vegetative microorganisms but do not necessarily kill bacterial spores. To be effective, disinfectants must meet either European standards (the CEN series) or US standards (the AOAC standards). These standards involve challenging disinfectants with high populations of a range of different microorganisms and noting the log reduction over time. Such studies are undertaken for the disinfectant solution (the suspension test), on surfaces, and in the field (to develop appropriate cleaning frequencies). Disinfectants vary in their spectrum of activity, modes of action, and efficacy. Some are bacteriostatic, in which the ability of the bacterial population to grow is halted. Here, the disinfectant can cause selective and reversible changes to cells by interacting with nucleic acids, inhibiting enzymes, or permeating into the cell wall. Once the disinfectant is removed from contact with bacteria cells, the surviving bacterial population could potentially grow. Other disinfectants are bactericidal, in that they destroy bacterial cells through different mechanisms, including causing structural damage to the cell, autolysis, cell lysis, and the leakage or coagulation of cytoplasm (6). There are many different types of disinfectants for use within the pharmaceutical industry, with different spectrums of activity and modes of action. The mechanisms of action are not always completely known and continue to be investigated. A range of different factors needs to be considered as part of the process of selection, including the mode of action, efficacy, compatibility, cost and current health and safety standards (7). Surface disinfectants have varying modes of action against microbial cells due to their chemical diversity. Different disinfectants target different sites within the microbial cell. These include the cell wall, the cytoplasmic membrane (where the matrix of phospholipids and enzymes provide various targets) and the cytoplasm. Some disinfectants, on entering the cell either by disruption of the membrane or through diffusion, proceed to act on intracellular components. There are different approaches to the categorization and subdivision of disinfectants, including grouping by chemical nature, mode of activity, or by bacteriostatic and bactericidal effects on microorganisms (8).
July 2012 GBPR, Inc. Newsletter
Evelyn Heitman, Editor
There are many different types of disinfectants, and space does not permit a list of all possible types. This guide describes some of the more commonly used types of disinfectants. Surface disinfectants can be divided into: Nonoxidizing Disinfectants a) Alcohols The effectiveness of alcohols against vegetative bacteria and fungi increases with their molecular weight (therefore, ethanol is more effective than methanol, and in turn, isopropyl alcohols are more effective than ethanol). Alcohols act on the bacterial cell membrane by making it permeable, and efficacy is increased with the presence of water leading to cytoplasm leakage, denaturation of protein, and eventual cell lysis. The advantages of employing alcohols include a relatively low cost, little odor, and a quick evaporation (9). b) Aldehydes Aldehydes include formaldehyde and glutaraldehyde. Aldehydes have a nonspecific effect in the denaturing of bacterial cell proteins and can cause coagulation of cellular protein. There are some safety concerns about the use of some aldehydes (10). c) Amphoterics Amphoterics have both anionic and cationic character and possess a relative wide spectrum of activity, but they are limited by their inability to damage endospores. Amphoterics are frequently used as surface disinfectants. Examples include the alkyl di (aminoethyl) glycine group of compounds. d) Phenolics Synthetic phenols are widely available, such as the bis-phenols (triclosan) and halophenols (chloroxylenol). Phenols are bactericidal and antifungal but are not effective against spores. Some phenols cause bacterial cell damage through disruption of proton motive force, while others attack the cell wall and cause leakage of cellular components and protein denaturation. e) Quaternary Ammonium Compounds (QACs) QACs are cationic salts of organically substituted ammonium compounds and have a fairly broad range of activity against microorganisms. They are ineffective against bacterial spores. QACs are possibly the most widely used of the nonoxidizing
July 2012 GBPR, Inc. Newsletter
Evelyn Heitman, Editor
disinfectants within the pharmaceutical industry; examples include cetrimide and benzalkonium chloride. Their mode of action is on the cell membrane leading to cytoplasm leakage and cytoplasm coagulation through interaction with phospholipids (11). Oxidizing Disinfectants This group includes oxygen-releasing compounds (peroxygens) such as peracetic acid and hydrogen peroxide. They function by disrupting the cell wall, causing cytoplasm leakage and denaturing bacterial cell enzymes through oxidation. Oxidizing agents have advantages, in that they are clear and colorless, thereby avoiding surface staining. Sanitization Regime There are a number of important steps involved with respect to cleaning and disinfection. These are: Cleaning Cleaning, in the context of pharmaceutical manufacturing, is the process of removing residues and soil from surfaces to the extent that they are visually clean. This involves defined methods of application and often the use of a detergent. Detergents generally work by penetrating, soiling, and reducing the surface tension (which fixes the soil to the surface) to allow its removal. For cleanrooms, such cleaning steps are necessary prior to the application of a disinfectant. It is essential that a surface or item of equipment has been properly cleaned before the application of a disinfectant in order for the disinfectant to work efficiently.
July 2012 GBPR, Inc. Newsletter
Evelyn Heitman, Editor
Figure 3: Cleaning within a pharmaceutical facility (c) Tim Sandle Disinfection Disinfectants are applied to surfaces which have been cleaned. When applying a disinfectant, as previously discussed, the critical aspect is the contact time. The disinfectant is only effective when left in contact with the surface for the validated time. This can be achieved more easily when the disinfectant is applied in overlapping strokes. When rotation of disinfectants is required, a water rinse (normally employing WFI) is employed between the changeover of disinfectants. This is in order to remove traces of disinfectant and detergent residue (such as anions) which may act to reduce the efficacy of the new disinfectant. For a disinfectant to achieve the desired effectiveness, it must remain on the targeted surface for an appropriate length of time. Determining the optimal contact time often means striking a balance between what is necessary to achieve the desired microbial reduction and what is practical for real-time use in the facility. At minimum, the manufacturers recommended contact time should be tested. Additional contact times
July 2012 GBPR, Inc. Newsletter
Evelyn Heitman, Editor
may also be evaluated if the manufacturers recommended time is demonstrated to be ineffective, or if a shorter contact time is desired (12). Rotation of Disinfectants In selecting disinfectants, many pharmaceutical manufacturers will opt to have two in-use disinfectants and sometimes to have a third disinfectant as a reserve in case a major contamination incident arises, such as a bioburden contamination build-up, which appears resistant or difficult to eliminate using the routinely used disinfectants. The reserve disinfectant will often be more powerful and sporicidal, such as an oxidising agent, the routine use of which is restricted because of likely damage to the equipment and premises. Typically the two primary disinfectants are rotated. This is a requirement of regulatory bodies with, for example, the EU GMP Guide stating that where disinfectants are used, more than one type should be employed (Annex 1). Cleaning and Disinfection Procedures Cleaning and disinfection must be detailed in a Standard Operating Procedure (SOP) to ensure consistency of practice. Furthermore, sufficient detail in SOPs is important, because detergents and disinfectants are only partially effective if they are not applied correctly. An SOP should describe: The type of detergents and disinfectants to be used (which are compatible) The frequency of rotation of disinfectants A list of suitable cleaning materials Cleaning techniques Contact times Rinsing Frequency of cleaning and disinfection Procedure for the transfer of cleaning agents and disinfectants into and out of clean areas (including the procedure for sterilization of disinfectants) Holding times for detergents and disinfectants
Assessing Sanitization Effectiveness The effectiveness of cleanroom sanitization is assessed through the environmental monitoring regime. Environmental monitoring is a program which examines the numbers and occurrences of viable microorganisms and nonviable particles (that is, particles in the area other than microorganisms, such as dust or skin cells). Ideally, environmental monitoring is targeted to those areas of the production process where the risk cannot be adequately controlled. It thereby, through trend analysis, provides an indication if the cleanroom is moving out of control (13).
July 2012 GBPR, Inc. Newsletter
Evelyn Heitman, Editor
Figure 4: A microbiology technician undertaking environmental monitoring (c) Tim Sandle Viable monitoring is designed to detect levels of bacteria and fungi present in defined locations/areas during a particular stage in the activity of processing and filling a product. Samples are taken from walls, surfaces, people and the air (each of which represents a potential contamination source). Viable monitoring is designed to detect microorganisms and answer the questions: How many? How frequent? When do they occur? Why do they occur? (14).
July 2012 GBPR, Inc. Newsletter
Evelyn Heitman, Editor
Viable monitoring is undertaken using a substance called agar (a jelly-like growth medium) in different sized containers. It is important that the culture media used for environmental monitoring contains a neutralizer to eliminate any residues of the disinfectant. The environmental monitoring program is normally controlled by the Microbiology Department who establish the appropriate frequencies and durations for monitoring based on a risk assessment approach. The sampling plan takes into account the cleanliness level required at each site to be sampled. Validation Regulatory agencies expect the pharmaceutical manufacturer to have evaluated the efficacy of disinfectants. Qualification of a disinfectant is demonstrated through performance testing to show that the disinfectant is capable of reducing the microbial bioburden found on manufacturing area surfaces. Representative manufacturing surface samples are inoculated with a selection of microbial challenge organisms. A disinfectant is applied to the inoculated surfaces and exposed for a predetermined contact time, after which the surviving organisms are recovered using a qualified disinfectant-neutralizing broth and test method (surface rinse, contact plate, or swab). The number of challenge organisms recovered from the test samples (exposed to a disinfectant) is compared to the number of challenge organisms recovered from the corresponding control sample (not exposed to a disinfectant) to determine the ability of the disinfectant to reduce the microbial bioburden. Successful completion of the validation qualifies the disinfectant evaluated for use. The disinfectant efficacy validation should provide documented evidence that the disinfectant demonstrates the bactericidal, fungicidal, and/or sporicidal activity necessary to control microbial contamination in the facility (15). Of the different methods for disinfectant validation, the surface or carrier test is the most representative. For this, a range of surfaces should be considered. Given that all surfaces within pharmaceutical manufacturers facilities will be exposed to the cleaning and disinfection program, a pragmatic view should be taken. Where the surface is considered critical in terms of cleaning and disinfection, i.e., contact with product and personnel, it should be considered for disinfectant surface testing. The USP Chapter <1072> lists common materials used in cleanrooms that should be considered when setting up disinfectant surface testing. Along with stainless steel, other surfaces within the manufacturing facility should be tested. For example, different grades of vinyl and stainless steel, different types of plastic, glass from windows, and vessels. The test works by examining preparations of microorganisms dried onto surfaces. To such a dried suspension, a prepared sample of the disinfectant is added. The surface is
July 2012 GBPR, Inc. Newsletter
Evelyn Heitman, Editor
then transferred to a previously validated neutralization medium, and tests are performed to measure the reduction in viable counts. The test involves drying 0.05 ml suspensions of the microorganisms (with interfering substances such as bovine serum albumin) onto different surfaces. The microorganisms should have a population range of 1.5 - 5.0 x 108 for bacteria and 1.5 - 5.0 x 107 for fungi and are equilibrated to 25oC before use. Once applied to the surface, the drying of the microorganisms may be accelerated using an incubator operating at 36-38oC. Disinfectant solutions (where disinfectants are made with Water of Standard Hardness (WSH) are added to the surfaces. After the specified contact time (five minutes is the target) the surfaces are transferred to the validated neutralization medium, and then pour plates are prepared for incubation and counting. An alternative method is available using a soaked swab step (16). To demonstrate the effectiveness of a disinfectant, it must be challenged using a panel of organisms that is reflective of the natural microflora of the facility. The biocidal activity of the disinfectant should be taken into account when selecting the panel of organisms. The surface test, however, cannot demonstrate the effect of a range of environmental factors such as temperature, pH, detergent residues, mechanical stress, and attachment. For these reasons, a disinfectant which appears effective for the surface test can show marked variability when applied to practical conditions. The reasons for this are due to problems in drying and differences between surfaces. In terms of drying microbial suspensions, there is a marked loss in the viability of a population when dried onto a surface, and attempts to speed up the drying process do not significantly reduce the variability of the actual number of microorganisms challenged. Surfaces introduce another variation, because surfaces, even of the same grade of material, are not truly identical, and there have been marked problems in achieving reproducibility and repeatability for the surface test between laboratories, particularly in estimating the concentration of disinfectant that is required to be effective. Some of these limitations can be addressed through field trials. Field trials are an important part of the qualification of a sanitizer, for they determine if the cleaning techniques are suitable and if the cleaning frequencies of cleanrooms require modification. Filed trials involve a considerable amount of environmental monitoring, for the counts before and after disinfection and the types of microorganisms recovered must each be evaluated. Summary This paper has presented an overview of the application of the sanitization of pharmaceutical facilities and has emphasized that sanitization is a key part of contamination control within cleanrooms. The paper has examined some the
July 2012 GBPR, Inc. Newsletter
Evelyn Heitman, Editor
techniques and controls required and has compared some of the different types of disinfectants available for use within cleanrooms. The paper has also emphasized the importance of qualifying disinfectants in order to demonstrate their effectiveness, and for undertaking a vigorous monitoring regime in order to show that the cleanroom environment remains in control. References 1. Halls, N. (2004): Effects and Causes of Contamination in Sterile Manufacturing, in Hall, N. (ed.): Microbiological Contamination Control in Pharmaceutical Clean Rooms, CRC Press, Boca Raton, pp. 1-22. 2. EN 1499. 1997: Chemical Disinfectants and Antiseptics. Hygienic Handwash. Test Method and Requirements (Phase 2/Step 2). 3. EN 1500. 1997: Chemical Disinfectants Quantitative Carrier Test to Evaluate the Bactericidal Activity of a Hygienic Handrub Solution (Phase 2/2). Chemical Disinfectants and Antiseptics. Hygienic Handrub. Test Method and Requirements (Phase 2/Step 2). 4. Best, M. and Kennedy, M.E.: Effectiveness of Handwashing Agents in Eliminating Staphylococcus Aureus from Gloved Hands, Journal of Applied Bacteriology, (1992) 73: pp. 6366. 5. Larson, E., Mayur, K., and Laughon, B.: Influence of Two Handwashing Frequencies on Reduction in Colonizing Flora with three Handwashing Products Used by Health Care Personnel, American Journal of Infection Control, (1989) 17(2): pp. 8388. 6. Sandle, T. (2003): Selection and Use of Cleaning and Disinfection Agents in Pharmaceutical Manufacturing, in Hodges, N. and Hanlon, G.: Industrial Pharmaceutical Microbiology Standards and Controls, Euromed Communications, England. 7. Block, S. (1977): Disinfection, Sterilisation and Preservation, Third Edition, Lea and Febiger, Philadelphia. 8. Denyer, S.P. and Stewart, G.S.A.B.: Mechanisms of Action of Disinfectants, International Biodeterioration and Biodegradation, (1998) 41: pp. 261-268. 9. McDonnell, G. and Russell, A.: Antiseptics and Disinfectants: Activity, Action and Resistance, Clinical Microbiology Reviews, (Jan. 1999): pp. 147 179. 10. Angelillo, I.F., Bianco, A., Nobile, C.G.A. and Pavia, M.: Evaluation of the Efficacy of Glutaraldehyde and Peroxygen for Disinfection of Dental Instruments, Letters in Applied Microbiology, (1998) 27: pp. 292296. 11. Bergan, T. and Lystad, A.: Evaluation of Disinfectant Inactivators, Acta Path Microbiol. Scand., (1972) Section B; 80: pp. 507510.
July 2012 GBPR, Inc. Newsletter
Evelyn Heitman, Editor
12. Bessems, E.: The Effect of Practical Conditions on the Efficacy of Disinfectants, International Biodeterioration and Biodegradation, (1998) 41: pp. 177-183. 13. Johnson, S. M. (2004): Microbiological Environmental Monitoring in Hodges, N. and Hanlon, G.: Microbiological Standards and Controls, Euromed, London. 14. Vincent, D.: Validating, Establishing and Maintaining a Routine Environmental Monitoring Program for Cleanroom Environments: Part 1, Journal of Validation Technology, (August 2002) Vol. 8, No. 4. 15. Vina, P., Rubio, S. and Sandle, T. (2011): Selection and Validation of Disinfectants, in Saghee, M.R., Sandle, T., and Tidswell, E.C. (Eds.): Microbiology and Sterility Assurance in Pharmaceuticals and Medical Devices, New Delhi: Business Horizons, pp. 219-236. 16. Bloomfield, S.F., Arthur, M., Van Klingeren, B., Pullen, W., Holah, J.T. and Elton, R.:An Evaluation of the Repeatability and Reproducibility of a Surface Test for the Activity of Disinfectants, Journal of Applied Bacteriology, (1994) 76, pp. 86-94.
July 2012 GBPR, Inc. Newsletter
Evelyn Heitman, Editor
Vous aimerez peut-être aussi
- Disinfectants in Pharmaceutical Industry Tim SandleDocument8 pagesDisinfectants in Pharmaceutical Industry Tim SandleshwampaPas encore d'évaluation
- Sanitation of Pharmaceutical FacilitiesDocument5 pagesSanitation of Pharmaceutical FacilitiesDoan Chi ThienPas encore d'évaluation
- Sterilisation and Disinfection: Pharmaceutical MonographsD'EverandSterilisation and Disinfection: Pharmaceutical MonographsÉvaluation : 5 sur 5 étoiles5/5 (3)
- Biocontamination Control for Pharmaceuticals and HealthcareD'EverandBiocontamination Control for Pharmaceuticals and HealthcareÉvaluation : 5 sur 5 étoiles5/5 (1)
- Production of Plasma Proteins for Therapeutic UseD'EverandProduction of Plasma Proteins for Therapeutic UseÉvaluation : 3 sur 5 étoiles3/5 (5)
- Environmental Monitoring and Control A Complete GuideD'EverandEnvironmental Monitoring and Control A Complete GuidePas encore d'évaluation
- Regulatory Aspects of Pharmaceutical Quality System: Brief IntroductionD'EverandRegulatory Aspects of Pharmaceutical Quality System: Brief IntroductionPas encore d'évaluation
- Aseptic ProcessingDocument13 pagesAseptic ProcessingAshok Kumar100% (1)
- Continuous Manufacturing of PharmaceuticalsD'EverandContinuous Manufacturing of PharmaceuticalsPeter KleinebuddePas encore d'évaluation
- Environment Monitoring, Result Evaluation and Common Contaminants Study of Vaccine Manufacturing FacilityDocument12 pagesEnvironment Monitoring, Result Evaluation and Common Contaminants Study of Vaccine Manufacturing FacilityIJRASETPublicationsPas encore d'évaluation
- Cleaning Validation in Pharmaceutical IndustriesDocument5 pagesCleaning Validation in Pharmaceutical IndustriesAbhishek RajPas encore d'évaluation
- Validation Master Plan A Complete Guide - 2020 EditionD'EverandValidation Master Plan A Complete Guide - 2020 EditionPas encore d'évaluation
- Cleanroom Surface ContaminationDocument4 pagesCleanroom Surface ContaminationTim SandlePas encore d'évaluation
- Design of Aseptic Process SimulationDocument5 pagesDesign of Aseptic Process SimulationFranck BurePas encore d'évaluation
- Pharmaceutical Cleaning A Comprehensive Approach - 0Document15 pagesPharmaceutical Cleaning A Comprehensive Approach - 0Mina Maher MikhailPas encore d'évaluation
- A Comprehensive Text Book on Self-emulsifying Drug Delivery SystemsD'EverandA Comprehensive Text Book on Self-emulsifying Drug Delivery SystemsPas encore d'évaluation
- Pharmaceutical Water - Pharmaceutical GuidelinesDocument6 pagesPharmaceutical Water - Pharmaceutical GuidelinesAbou Tebba SamPas encore d'évaluation
- Validation master plan Complete Self-Assessment GuideD'EverandValidation master plan Complete Self-Assessment GuidePas encore d'évaluation
- Contamination Control in Pharmaceutical FaclityDocument3 pagesContamination Control in Pharmaceutical FaclityAnkush PandeyPas encore d'évaluation
- Portfolio, Program, and Project Management in the Pharmaceutical and Biotechnology IndustriesD'EverandPortfolio, Program, and Project Management in the Pharmaceutical and Biotechnology IndustriesPete HarpumPas encore d'évaluation
- Validation Master Plan A Complete Guide - 2019 EditionD'EverandValidation Master Plan A Complete Guide - 2019 EditionPas encore d'évaluation
- Disinfection ValidationDocument25 pagesDisinfection ValidationSumitPas encore d'évaluation
- Testing Compressed Air Lines For Microbiological ContaminationDocument8 pagesTesting Compressed Air Lines For Microbiological Contaminationmuzammil21_adPas encore d'évaluation
- Good Manufacturing Practices (GMP) Modules for Pharmaceutical ProductsD'EverandGood Manufacturing Practices (GMP) Modules for Pharmaceutical ProductsPas encore d'évaluation
- ICH Quality Guidelines: An Implementation GuideD'EverandICH Quality Guidelines: An Implementation GuideAndrew TeasdalePas encore d'évaluation
- Bioprocessing Technology for Production of Biopharmaceuticals and BioproductsD'EverandBioprocessing Technology for Production of Biopharmaceuticals and BioproductsClaire KomivesPas encore d'évaluation
- GMP in Pharmaceutical Industry: Global cGMP & Regulatory ExpectationsD'EverandGMP in Pharmaceutical Industry: Global cGMP & Regulatory ExpectationsÉvaluation : 5 sur 5 étoiles5/5 (2)
- Media Fill For Validation of A Good Manufacturing - ARTIGODocument9 pagesMedia Fill For Validation of A Good Manufacturing - ARTIGOBiancaPas encore d'évaluation
- Molecular Biological Markers for Toxicology and Risk AssessmentD'EverandMolecular Biological Markers for Toxicology and Risk AssessmentPas encore d'évaluation
- Usp Review AlbuterolDocument82 pagesUsp Review Albuterolsrayu2603Pas encore d'évaluation
- Environmental Monitoring and Microbiological Manufacture of Sterile DrugsDocument8 pagesEnvironmental Monitoring and Microbiological Manufacture of Sterile DrugsKristian Uriel DelgadoPas encore d'évaluation
- APIC Guideline SupplierQualification Appendix 4 1 Checklist 2009Document1 pageAPIC Guideline SupplierQualification Appendix 4 1 Checklist 2009dinu344Pas encore d'évaluation
- CreatingaCleaningValidationPlan TOCDocument1 pageCreatingaCleaningValidationPlan TOCOnichan21Pas encore d'évaluation
- Microbial Monitoring - Bioburden - Pda Journal May June 2015Document15 pagesMicrobial Monitoring - Bioburden - Pda Journal May June 2015Kinomi100% (2)
- Data Integrity and Compliance: A Primer for Medical Product ManufacturersD'EverandData Integrity and Compliance: A Primer for Medical Product ManufacturersPas encore d'évaluation
- Cleaning Validation in Pharmaceutical IndustryDocument21 pagesCleaning Validation in Pharmaceutical IndustrysvengotoPas encore d'évaluation
- Cross ContaminationDocument47 pagesCross ContaminationAKKAD PHARMAPas encore d'évaluation
- What Is Disinfectant ValidationDocument4 pagesWhat Is Disinfectant Validationrouss1906Pas encore d'évaluation
- Leachables and Extractables Handbook: Safety Evaluation, Qualification, and Best Practices Applied to Inhalation Drug ProductsD'EverandLeachables and Extractables Handbook: Safety Evaluation, Qualification, and Best Practices Applied to Inhalation Drug ProductsDouglas J. BallPas encore d'évaluation
- Validation of Sterilization ProcessesDocument3 pagesValidation of Sterilization ProcessesNovitra DewiPas encore d'évaluation
- Cleanroom Management in Pharmaceuticals and HealthcareDocument1 pageCleanroom Management in Pharmaceuticals and HealthcareTim SandlePas encore d'évaluation
- A Final Floor Show For Bugs (Sandle)Document4 pagesA Final Floor Show For Bugs (Sandle)Tim Sandle100% (1)
- Preventing of Cross ContaminationDocument27 pagesPreventing of Cross ContaminationOmar FaruqPas encore d'évaluation
- Cleaning-in-Place: Dairy, Food and Beverage OperationsD'EverandCleaning-in-Place: Dairy, Food and Beverage OperationsPas encore d'évaluation
- Cleaning Validation and Its Importance in Pharmaceutical IndustryDocument5 pagesCleaning Validation and Its Importance in Pharmaceutical Industrymichael_payne3532Pas encore d'évaluation
- Good Distribution Practice A Complete Guide - 2021 EditionD'EverandGood Distribution Practice A Complete Guide - 2021 EditionPas encore d'évaluation
- Global Perspectives in Cleaning ValidationDocument17 pagesGlobal Perspectives in Cleaning ValidationYusuf SalahamanaPas encore d'évaluation
- Conducting Compliant InvestigationsDocument10 pagesConducting Compliant InvestigationsTim Sandle100% (1)
- Digital Transformation and Regulatory Considerations For Biopharmaceutical and Healthcare Manufacturers Volume 1 Digital Technologies For Automation and Process ImprovementDocument8 pagesDigital Transformation and Regulatory Considerations For Biopharmaceutical and Healthcare Manufacturers Volume 1 Digital Technologies For Automation and Process ImprovementTim SandlePas encore d'évaluation
- Digital Transformation in Pharmaceuticals and HealthcareDocument1 pageDigital Transformation in Pharmaceuticals and HealthcareTim Sandle100% (1)
- Publications by Tim Sandle - 5th EditionDocument92 pagesPublications by Tim Sandle - 5th EditionTim SandlePas encore d'évaluation
- Cleanroom Contamination Prevention & Control: A Practical Guide To The ScienceDocument13 pagesCleanroom Contamination Prevention & Control: A Practical Guide To The ScienceTim Sandle56% (9)
- Pharmaceutical Microbiology NewsletterDocument12 pagesPharmaceutical Microbiology NewsletterTim SandlePas encore d'évaluation
- NOW IS THE TIME For Animal Welfare in PharmaDocument2 pagesNOW IS THE TIME For Animal Welfare in PharmaTim SandlePas encore d'évaluation
- Pharmigs 26th Annual Conference Programme Interactive 2018 FinalDocument8 pagesPharmigs 26th Annual Conference Programme Interactive 2018 FinalTim SandlePas encore d'évaluation
- Digital Transformation of Pharmaceuticals (New Book)Document2 pagesDigital Transformation of Pharmaceuticals (New Book)Tim SandlePas encore d'évaluation
- Biotechnology: From Idea To MarketDocument4 pagesBiotechnology: From Idea To MarketTim Sandle100% (1)
- Audit and Control For Healthcare Manufacturers: A Systems-Based ApproachDocument13 pagesAudit and Control For Healthcare Manufacturers: A Systems-Based ApproachTim Sandle100% (1)
- Audit and Control For Healthcare Manufacturers: A Systems-Based ApproachDocument13 pagesAudit and Control For Healthcare Manufacturers: A Systems-Based ApproachTim Sandle100% (1)
- Publications by Tim Sandle - July 2019Document53 pagesPublications by Tim Sandle - July 2019Tim SandlePas encore d'évaluation
- Cleaning and CleanroomsDocument7 pagesCleaning and CleanroomsTim SandlePas encore d'évaluation
- An Interview With DR Tim Sandle - March 2019Document4 pagesAn Interview With DR Tim Sandle - March 2019Tim Sandle100% (1)
- Real-Time Mycoplasma Contamination Detection For BiomanufacturingDocument3 pagesReal-Time Mycoplasma Contamination Detection For BiomanufacturingTim SandlePas encore d'évaluation
- Biocontamination Control For Pharmaceuticals and HealthcareDocument2 pagesBiocontamination Control For Pharmaceuticals and HealthcareTim Sandle100% (1)
- The New Concept of Automatic Gloved Hand SanitizationDocument3 pagesThe New Concept of Automatic Gloved Hand SanitizationTim SandlePas encore d'évaluation
- Aseptic and Sterile Processing: Control, Compliance and Future TrendsDocument1 pageAseptic and Sterile Processing: Control, Compliance and Future TrendsTim SandlePas encore d'évaluation
- Burkholderia Cepacia Complex: Characteristics, Products Risks and Testing RequirementsDocument17 pagesBurkholderia Cepacia Complex: Characteristics, Products Risks and Testing RequirementsTim Sandle100% (1)
- Data Integrity BookDocument2 pagesData Integrity BookTim Sandle100% (1)
- CleanroomMicrobiology Flyer Order FormDocument2 pagesCleanroomMicrobiology Flyer Order FormTim SandlePas encore d'évaluation
- Aseptic and Sterile Processing: Control, Compliance and Future TrendsDocument2 pagesAseptic and Sterile Processing: Control, Compliance and Future TrendsTim Sandle100% (1)
- Publications by Tim Sandle (3rd Revision)Document42 pagesPublications by Tim Sandle (3rd Revision)Tim SandlePas encore d'évaluation
- Products For Microbiological ControlDocument120 pagesProducts For Microbiological ControlTim Sandle100% (2)
- PDA Europe Microbiology Conference 2017Document18 pagesPDA Europe Microbiology Conference 2017Tim SandlePas encore d'évaluation
- Contamination Control in Healthcare Product Manufacturing, Volume 4Document2 pagesContamination Control in Healthcare Product Manufacturing, Volume 4Tim Sandle0% (1)
- Cleanroom Management (2017 Ed)Document1 pageCleanroom Management (2017 Ed)Tim Sandle50% (2)
- PDA Bookstore ESeries Flyer - OrderformDocument2 pagesPDA Bookstore ESeries Flyer - OrderformTim SandlePas encore d'évaluation
- CleanroomMicrobiology Flyer Order FormDocument2 pagesCleanroomMicrobiology Flyer Order FormTim SandlePas encore d'évaluation
- ESAB Welding & Cu Ing Products: A515 516 4 In. Thick 2 In. Root GapDocument1 pageESAB Welding & Cu Ing Products: A515 516 4 In. Thick 2 In. Root Gapalok987Pas encore d'évaluation
- Understanding Omega Fatty AcidsDocument5 pagesUnderstanding Omega Fatty Acidsdrubwang100% (1)
- Introduction of Organic Chemistry by Eyes of Ajnish Kumar Gupta (AKG)Document24 pagesIntroduction of Organic Chemistry by Eyes of Ajnish Kumar Gupta (AKG)ajju_208180% (5)
- Urea UV Freeze DriedDocument1 pageUrea UV Freeze DriedJanos ImrePas encore d'évaluation
- Insulation System ClassDocument2 pagesInsulation System ClassVictor Hutahaean100% (1)
- Lin Jingwei - A Nomadic Furniture For College StudentsDocument129 pagesLin Jingwei - A Nomadic Furniture For College StudentsAarish Netarwala100% (2)
- Description and Solubility - MTZDocument6 pagesDescription and Solubility - MTZPityu PíPas encore d'évaluation
- RNA Structure, Functions WebDocument25 pagesRNA Structure, Functions WebEmad ManniPas encore d'évaluation
- Rna Qualitative TestsDocument5 pagesRna Qualitative TestsPeter Paul RecaboPas encore d'évaluation
- FT Schedule RM Phase 1Document1 pageFT Schedule RM Phase 1Virat ValiPas encore d'évaluation
- ASTM Method D5134-92Document1 pageASTM Method D5134-92Sylab InstrumentsPas encore d'évaluation
- CE4105 Surface Production Operations: Operasi Produksi Permukaan Hidrokarbon / Operasi Hulu Minyak Dan GasDocument41 pagesCE4105 Surface Production Operations: Operasi Produksi Permukaan Hidrokarbon / Operasi Hulu Minyak Dan GasRickyWisaksonoPas encore d'évaluation
- ASTM D874 - 2000 - Sulfated Ash From Lubricating Oils and AdditivesDocument5 pagesASTM D874 - 2000 - Sulfated Ash From Lubricating Oils and AdditivesConstantinos ChristodoulouPas encore d'évaluation
- ENVIROMENTAL Civic Education 10 To 12 PDF - RepairedDocument9 pagesENVIROMENTAL Civic Education 10 To 12 PDF - RepairedRichard シPas encore d'évaluation
- Nanofabrication For Pattern Transfer Purpose.: Etching Is Done Either in "Dry" or "Wet" MethodsDocument19 pagesNanofabrication For Pattern Transfer Purpose.: Etching Is Done Either in "Dry" or "Wet" MethodsPRAVEEN MPas encore d'évaluation
- NuclearDocument10 pagesNuclearUsman MunirPas encore d'évaluation
- Ets InternacionalDocument72 pagesEts InternacionalRicardo MarquesPas encore d'évaluation
- E Grout Mc050Document2 pagesE Grout Mc050Tori SmallPas encore d'évaluation
- FDA-356h 508 (6.14)Document3 pagesFDA-356h 508 (6.14)sailaja_493968487Pas encore d'évaluation
- ASTM B188-2002 Tubos de CobreDocument10 pagesASTM B188-2002 Tubos de Cobrelinealmen100% (1)
- Semester/Concrete Technology (9021) /experiment-02 PDFDocument14 pagesSemester/Concrete Technology (9021) /experiment-02 PDFjestinvthomasPas encore d'évaluation
- List Drug Food InteractionsDocument8 pagesList Drug Food InteractionsAliza Raudatin SahlyPas encore d'évaluation
- Light ExperimentsDocument12 pagesLight ExperimentsmamosPas encore d'évaluation
- Astm A 240-18Document12 pagesAstm A 240-18Giann' Andreh'xd100% (2)
- Normal HS 2073 - 2016-12-02-12-30-16 PDFDocument562 pagesNormal HS 2073 - 2016-12-02-12-30-16 PDFSandeep JoshiPas encore d'évaluation
- tmp12B1 TMPDocument29 pagestmp12B1 TMPFrontiersPas encore d'évaluation
- Stoichiometry: Calculations With Chemical Formulas and EquationsDocument47 pagesStoichiometry: Calculations With Chemical Formulas and EquationsAngelo Miguel GarciaPas encore d'évaluation
- CDB2043 - CH 03 - StoichiometryDocument36 pagesCDB2043 - CH 03 - StoichiometryAqilah HanimPas encore d'évaluation
- Review of Related LiteratureDocument7 pagesReview of Related LiteratureJamie HaravataPas encore d'évaluation
- Titanium WeldingDocument16 pagesTitanium WeldingMuhammad IrdhamPas encore d'évaluation