Académique Documents
Professionnel Documents
Culture Documents
Programmes For Parents With A Mental Illness
Transféré par
Mareeze HattaDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Programmes For Parents With A Mental Illness
Transféré par
Mareeze HattaDroits d'auteur :
Formats disponibles
Journal of Psychiatric and Mental Health Nursing, 2011, 18, 257264
Programmes for parents with a mental illness
A . R E U P E R T 1 p h d & D . M AY B E RY 2 p h d
1
jpm_1660
257..264
Senior Lecturer, Faculty of Education, and 2Associate Professor of Rural Mental Health, Department of Rural and Indigenous Health, Faculty of Medicine, Nursing and Health Sciences, Monash University, Moe, Vic., Australia
Keywords: parental mental health, parenting programmes Correspondence: A. Reupert Faculty of Education Monash University PO Box 6 Clayton Vic. 3800 Australia E-mail: andrea.reupert@monash.edu Accepted for publication: 24 October 2010 doi: 10.1111/j.1365-2850.2010.01660.x
Accessible summary
Despite the benets of parenting interventions for parents and children, there are few documented programmes for parents who have a mental illness, with older children. Interviewing clinicians responsible for programmes specically developed for parents with a mental illness identies what clinicians believe is important for these parents and is one way of developing an evidence base. According to clinicians, programmes need to be responsive to parents with a mental illness through exibility in programme content, time and/or follow-up with case management or house visits. Providing opportunities to learn from and with other parents who have a mental illness is also important. Clinicians require support in articulating a sound theoretical basis for their programmes and when implementing evaluation strategies.
Abstract Parents with a mental illness experience the same parenting stressors that other parents do, and at the same time need to manage their mental illness. However, few programmes are designed for parents who have a mental illness, with older children (as opposed to interventions for mothers with infants). This study identied the common components across six programmes developed for parents with a mental illness who have older children. Australian clinicians, responsible for six parenting programmes for those with a mental illness, participated in individual, semi-structured interviews, during 2008. Programme manuals and evaluation reports were also sourced. Analyses involved thematic analysis, inter-rater reliability and respondent validation. Data were organized in three main areas: (1) programme description (format, goals, length and participants inclusion criteria); (2) theoretical framework (including clinicians beliefs and evidence underpinning programmes); and (3) evaluation designs and methodologies. It was found that clinicians facilitated education and support via a peer intervention model for parents with various mental illness diagnoses, responsive to the needs of parents and in a time exible manner. At the same time, clinicians found it difcult to articulate the theoretical framework of their programmes and employed mostly simplistic evaluation strategies.
Introduction
Mental illness is a family issue, especially where a custodial parent has the mental health problem. Having a mental
2010 Blackwell Publishing
illness does not preclude a parent from parenting well, but it can create a range of challenges that negatively impact on the family, including children (Oyserman et al. 2000). It has been estimated that 21% to 23% of children live in
257
A. Reupert & D. Maybery
families with at least one parent with a mental illness (Maybery et al. 2009). Given the prevalence of such families and the difculties some face, it is essential that appropriate interventions are developed. In this paper, we aim to identify core programme components of programmes specically developed for such parents, in order to consolidate information that can be used to guide the development of future parenting programmes. There are several mechanisms by which parental mental illness increases risks for families and children involving both genetic and environmental factors (Hosman et al. 2009). One signicant risk factor for children is the parenting capacity of the parent. Oyserman et al. (2000) found that mothers with a serious mental illness have signicantly less adequate parenting skills than other mothers in the community. A more recent study by some of the same researchers found a signicant association between maternal mental health problems and permissive (lack of parenting condence, lack of follow through) parenting and verbal hostility (Oyserman et al. 2005). Of interest is that a lack of parenting condence fully mediated the negative effective of poor maternal functioning on childrens academic outcomes, indicating that supporting mothers in their parenting can ameliorate at least some of the negative effects of maternal mental illness (Oyserman et al. 2005). At the same time, however, it needs to be pointed out that not all families where a parent has a mental illness are equally at risk. Maybery et al. (2009) found that of the 2123% of families affected by parental mental illness, only 1.3% have a parent with a severe and chronic mental illness. In a sample of 405 children living with parental mental illness, Howe et al. (2009) showed that 25% were also exposed to parental drug and/or alcohol problems, 42% were exposed to domestic violence and 16% were currently involved with child protection services, indicating that some children are exposed to multiple variables of risk, while others are not. Thus, families where a parent has a mental illness are not homogenous and parenting programmes and family interventions developed for this group need to reect this diversity. While there are several generic parenting programmes available, these are often developed as health promotion programmes for the whole community and fail to address the needs of parents with a mental illness (Craig 2004). The didactic method of instruction usually found in many such programmes tends to be problematic for those with a mental illness while the severity of a parents mental illness might make it difcult for a parent to generalize the strategies of the programme to home (Ackerson 2003). Issues with motivation and stigma can also impede parents attendance to generic parenting programmes (Thomas & Kalucy 2002).
258
There are some, albeit few, parenting programmes specically developed for parents with a mental illness. Solely targeting maternal depression, Sanders & McFarland (2000) describe a cognitive behavioural parenting programme, which resulted in a reduction in participants depression and child disruptive behaviour. Phelan et al. (2006) evaluated a programme for parents with various diagnoses, and found positive outcomes in childrens behaviour and parenting practices. However, the dropout rate of parent participants in this programme was high, with almost 50% of participants not completing the programme; in addition, a control group was not employed, limiting the utility of this evaluation. There have been several studies outlining interventions for mothers and young infants, such as motherbaby units (Buist et al. 2004, Glangeaud-Freudenthal & Barnett 2004, Wilson et al. 2004) and programmes for parents with children under 5 years of age (Bassett et al. 2001, Steele et al. 2010). As there is already some research on interventions for parents with very young children, and given the very different parenting requirements of infants vs. older children, this study will focus on parenting programmes for parents with older children only. The aim of this paper is to review available Australian programmes targeting parents who have a mental illness and their 5- to 18-year-old children. Hinden et al. (2006) argue that analysing existing programmes and identifying core programme components developed for particular contexts and clientele is one way of establishing an evidence base. Thus, analysing existing programmes provides an insight into what clinicians believe is important when supporting a particular community group. Additionally, based on the lack of research in this area, identifying core components across programmes can identify the elements that might be rigorously evaluated when developing future parenting programmes.
Aim
The aim of this study was to identify core components across programmes according to: 1. Programme description: format, topics, length of programme, inclusion criteria for parent participants (including age of children) and programme goals; 2. Theoretical framework: theory (or combination of theories), beliefs, assumptions and evidence underlying the programme; 3. Evaluation strategies and methodologies employed.
Method
In 2008, six individual, telephone interviews with clinicians were undertaken. With written permission, 1-h telephone
2010 Blackwell Publishing
Programmes for parents with a mental illness
interviews were audiotaped, with questions based on the three study objectives. Clinicians were also asked to email/ send relevant materials about their programme, such as manuals and evaluation reports. Ethical approval was obtained from the university human ethics committee. All names of clinicians, programmes and organizations were removed.
Findings
Programme description
Five of the six programmes presented here had been developed either by the interviewee or by a former colleague and the interviewee had inherited the programme. The remaining programme was an adaptation of a well-known (Australian) parenting programme. Specic modications to this programme included the provision of home visits to participants and an inclusion of parents with a mental illness only. Two programmes only accepted mothers. While the remaining four accepted any parent with a mental illness, participants tended to be mothers; any parent is accepted but to date only mothers have participated. Clinicians reported that parents mostly came from lower socioeconomic backgrounds. Specic cultural groups were not targeted, with parents background being more dependent on the programmes locality. There was no criterion for a specic mental health diagnosis with one clinician reporting that she accepted mothers with any severe and on-going mental illness, who cares for children and lives in [the area] is welcome. Five programmes accepted parents with children aged up to 18 years, with one targeting parents with children 10 years of age and under. All programmes were based on a peer support model, ve programmes in a peer group setting and one offering mentoring, where mothers were matched to other mothers with similar interests, mental illness diagnoses and geographical location. Other variables included the length of the programme, whether individual support was also provided and whether topics were predetermined (see Table 1). Predetermined topics typically focused on parenting strategies but at the same time acknowledged a parents mental illness. For example, in one programme, topics included care of self, as well as strategies for guiding childrens behaviour (Table 2). While some programmes involved predetermined topics, these were still responsive to participants needs:
Yes, we do have pre-determined topics but if someone wants to discuss something else that is important we do try to incorporate that as well . . . and spend less time on that weeks topic.
Participants
Clinicians were identied via an Australian public database (http://www.copmi.net.au/jsp/copmi_programs/index.jsp), which regularly advertises programmes targeting parents with a mental illness. Clinicians were also invited to identify others who work in this area (snowballing: Rubin & Babbie 2008). Six clincians, responsible for facilitating six different programmes, agreed to participate, including two nurses, two psychologists and two social workers, who worked in community health, welfare and outreach services. It should be noted that other professionals were also involved in the running of the programme such as psychiatrists, occupational therapists and consumers. The clinicians interviewed in this study self-identied as the main facilitator of the programme.
Data analysis
Individual interview transcripts were analysed independently by the two researchers using a thematic analytic process. This process involved an open coding system of analysis, attaching labels to lines or paragraphs of data and then describing the data at a concrete level, involving, at times, frequency counts of the various programme components. Given that data were sought in three distinct areas (programme description, theoretical framework and evaluation), the content analysis process employed can be described as a guided or directed content analysis approach (Hickey & Kipping 1996). The two researchers then met to reach a consensus for each of the transcripts (inter-rater reliability: Rubin & Babbie 2008). Rather than reach a numerical index of agreement, consensus was reached through discussion. To add further trustworthiness to the data, respondent validation was sought, whereby clinicians were invited to review the researcher identied themes and their individual transcripts, with an invitation to change, delete and/or add anything they believed important (Kitto et al. 2008). After incorporating clinicians feedback, across-interview analysis of the six transcripts was again independently conducted by the two researchers. Finally, one of the researchers scoped the various written materials about the programmes, as a further source of data.
2010 Blackwell Publishing
All clinicians report being sensitive to how the information is conveyed and what messages are presented, for example:
. . . we know that sometimes our parents need more time processing information . . . or in the morning for example, they arent going to be completely responsive to their kids so parents need to be gentle with themselves at that time of the day . . . 259
A. Reupert & D. Maybery
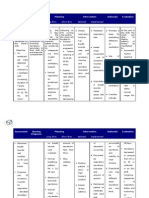
Table 1 Programme variables Programme 1 2 3 4 5 6
n/a, not available.
Peer format Group Group Group Group Group Mentoring: one to one
Programme length 6 weeks Unlimited 6 weeks 6 weeks 8 weeks 1 year
Additional individual support Case management None Home visits 4 home visits Case management Clinician supports mentor relationship
Predetermined topics Yes No Yes Yes No n/a
Table 2 An example of one programmes topics over 6 weeks Week 1 2 3 4 5 6 Topic Styles of parenting, parenting skills and parenting traps Childhood development/developing strong family relationships Communication, parental efcacy Guiding childrens behaviour Putting it all together Care of self, early warning signs, developing a personal plan and nal celebration
Table 3 Goals of parenting programmes Parenting programme goals Enhance parenting skill and condence Provide peer support Self-care, improve coping strategies Help parents identify strengths Link parents with other services Enhance parents understanding about the impact of mental illness on parenting Help parents help their children understand mental illness No. of programmes 6 5 4 3 3 3 2
Clinicians who ran programmes within a set time frame acknowledged that many parents might not be able to attend all sessions because of illness or other circumstance. Accordingly, in these parenting programmes, topics were not sequential and parents were able to miss one session and still attend the following week.
If a parent misses 1 week, we are quick to let them know that they can still come back. We have found that many of these parents cant always make a weekly committment but then feel bad about coming back after missing a session. [We let them know] that it is okay to miss a session and that each week we start on something different.
dont have and so can provide support to each other that is different from what a professional might provide. Parents being together is an important way to normalize, to provide hope to each other.
Programmes had multiple goals, the two most important to enhance parenting skill and condence, and facilitate peer support (Table 3). Thus, while managing mental illness was a focus, it was interrelated to other goals.
[We aim to . . .] to place parenting centrally in the recovery process so their treatment and support options are not just about the management of their illness but the management of its impact on their relationships, their self-concept and role identity.
One programme ran continually, with parents coming and going, according to need:
It is up to the individual and their needs as to how long the mother stays involved in the program. Mothers tend to come in and out of the program as their needs may change.
Theoretical framework
Most clinicians found it difcult to articulate the theoretical framework of their programme although three mentioned systems theory, two identied recovery theory with other theories including feminist theory, solution and strength-based therapy. Clinicians were clearer about the beliefs that underpinned the programme. All expressed the belief that parents with a mental illness had the right and the capacity to parent.
I strongly believe that these mothers have a right to parent . . . and that at times while they need support, it is the best thing for them and for their children that they remain the primary caregivers.
2010 Blackwell Publishing
Flexibility of content was also noted in two of the parenting programmes.
[the] group is consulted on what areas they would like to address and learn more about.
Learning with other parents was important for pragmatic reasons:
It makes more sense to work with a group of parents . . . it saves resources and time.
Another rationale for group work was the belief that parents would learn and access support from other parents:
. . . [The] premise of the program is that parents have a degree of knowledge and empathy that we as clincians 260
Programmes for parents with a mental illness
In terms of an evidence base, programmes were primarily developed on the basis of clinicians prior experiences of working with parents. Another source was other parenting programme evaluations although this was qualied:
. . . [there is] not much of an evidence base specically available on parenting programs for those with a mental illness though there is for other more general parenting programs which is what we have drawn on.
Discussion
The development of effective parenting programmes for parents with a mental illness offers a critical opportunity for early intervention and prevention that benets all family members. According to the clinicians interviewed here, learning from and with other parents was the primary strategy employed, for pragmatic reasons as well as a means of providing support and education. While referring to low-income families, Webster-Stratton (1997) describes the social support or buffering that parenting peer groups can provide, a nding conrmed here. Whether this peer support is sustained in the longer term, and the impact such support has on overall well-being and actual parenting behaviour for parents with a mental illness is as yet unclear, however, because of the mostly simplistic evaluation designs employed. This study demonstrates the importance in being responsive to the needs of parents, by being exible in time, programme content and/or following up with case management or house visits. Indeed, exibility was considered highly signicant; programmes that were time-limited ensured that topics were not sequential so that parents were able to miss a week without feeling that they could not return and programmes with predetermined topics were accommodated to the immediate needs of participants. One programme allowed parents to come and go, depending on their needs and life circumstances. Overall, clinicians describe acknowledging a parents mental illness, within the context of parents child caring responsibilities, relationships and self-concept. However, rather than incorporate broader pathways of risk for parents with a mental illness, such as poverty and housing (Reupert & Maybery 2007), the programmes reported in this study focused on individual factors. In addition, the programmes targeted, or attracted, only mothers, and there appears to be a service gap of programmes for fathers and specic cultural groups. It should be noted that only those clinicians identied via a network predominately orientated towards the public health sector were interviewed, which might have missed those working in the non-government sector. How other countries address the needs of parents with a mental illness is another obvious avenue for future research. Moreover, clinicians found it difcult to articulate the theoretical framework of their programme with only a passing reference to theories such as systems and recovery theory, without elaborating how these theories drove or inuenced the programme. While it is not unusual for practitioners to nd it difcult to nominate the theory that underpins their work (Dustin 2006), theory can assist programme developers to think more broadly about
261
One clinican described the evidence for the programme in this way:
There is a general evidence base [to this program] . . . the mode of delivery is efcacious, that is, peer group work where [the] group has heterogeneous qualities to it around a marginalizing and stigmatizing issue that they share.
Evaluation
The evaluation measures and designs employed by clinicians are reported in Table 4 alongside their responses to the question What have your evaluation measures showed you? Five clinicians identied participants satisfaction, post programme, either by questionnaire (three) or verbally (two). Five clinicians employed pre- and post-standardized measures such as the Eyberg Child Behaviour Inventory (ECBI: Eyberg & Pincus 1999), the Parenting Sense of Competence (PSOC: Johnston & Mash 1989) and the Parenting Scale (PS: Arnold et al. 1993). Clinicians were not able to provide more information on some of the standardized scales such as a quality of life questionnaire. Post-evaluation for all programmes occurred immediately after programme completion and none of the programmes tracked participants over time. All clinicians reported overall participant satisfaction with the programme and positive outcomes on the various measures employed, post intervention (Table 4). Other issues were raised by clinicians relating to programme evaluation. For example, one clinician highlighted the sensitive nature of the evaluation process.
. . . it is vital to the programs delivery to ensure ongoing evaluation, we all need to be creative in what and how we deliver programmes, to ensure ongoing participation and interest to shared goals within the community . . .
Across all six programmes, there was no systematic way of measuring dropout rates. One suggested that this was not necessary because
. . . parents drop in and out as they please . . . there are no set sessions and its more informal than many traditional parent programs . . .
None of the evaluation designs employed control or comparison groups.
2010 Blackwell Publishing
A. Reupert & D. Maybery
Table 4 Evaluation measures, design and outcomes for each programme Evaluation outcome/s, from participants responses to the question: What have your evaluation measures showed you? Across all measures the clinician found: Twelve months is not long enough for some of the client group, it can take twelve months or more on occasions to feel safe in the environment before realising the effects of the group
Programme 1
Measures used Generic evaluation questionnaire used in all programmes across the clinicians organization; according to the clinician this is a standardized questionnaire that measures the numbers [of participants] who have moved on to bigger and better things. No further information on the scale was available Clinician reviews individual case notes and family plan Group discussion to gauge participant satisfaction
Evaluation design Pre and post
Pre and post Post programme, group provides feedback and discusses experiences with the clinician. This process also involves matching the groups expectations at the beginning of the programme with how they feel at the end Post Women got a lot out of program . . . especially the non-clinician nature of the program Being able to bring kids along is very important [Parents] loved outings Participants demonstrate increased knowledge about talking about mental illness in their family
Self-constructed satisfaction questionnaire
Self-constructed, open ended questionnaire that measures condence in looking after mental health and well-being, relationships with children, knowledge of impact on children (Likert scaled) Parenting Sense of Competence (Johnston & Mash 1989) Self-constructed self-care questionnaire Parenting Scale (PS: Arnold et al. 1993) Self-constructed satisfaction questionnaire
Pre and post
Pre and post Pre and post Pre and post Post Pre, during and post On a quarterly basis over the 12 months Pre and post Pre and post
An increase in parents self-condence Improvements in self-care (descriptive statistics only) Improvements in discipline (descriptive statistics only) Participants satised with the programme Too early to say Programme has been modied based on feedback Decreased from clinical to non-clinical range on ECBI . . . perception of [childs] behaviour problem is lessened and their knowledge and parenting skills have improved following the program Parents are satised with the programme Parents are satised with the programme
Quality of life questionnaire (not specied) Clinician meets with two women in the mentoring relationship to obtain feedback, including satisfaction with the programme Eyberg Child Behaviour Inventory (ECBI, parent form: Eyberg & Pincus 1999) PS (Arnold et al. 1993)
Self-constructed satisfaction questionnaire (based on particular session) Self-constructed satisfaction questionnaire (based on overall programme)
End of every session Post
intervention as well as evaluation designs. Domahidy (2003, p. 76) points out, Theory is powerful because it organizes what professionals pay attention to and how they pay attention. It shapes beliefs that in turn shape action. Given the ecological nature of parental mental
262
illness, a theoretical framework is required that acknowledges both individual (including, for example, the respective needs of children and parents) and societal (such as poverty and stigma) factors. For example, the theoretical framework posed by Hosman et al. (2009), which
2010 Blackwell Publishing
Programmes for parents with a mental illness
incorporates risk and protective factors related to child, parent, family and social domains, might be one model used to guide the development of multi-component programmes for families where a parent has a mental illness. Furthermore, as evaluation and theory are interrelated, evaluation methodologies need to be aligned with the theoretical framework underpinning any particular programme. Important ndings from this study were the evaluation methods and designs employed by clinicians. Five clinicians identied participant satisfaction either through a self-constructed satisfaction questionnaire or verbally, where clinicians responsible for facilitating the programme sought participant feedback. However, while participant satisfaction is important, we do not believe that it is sufcient as an evaluation outcome to demonstrate the efcacy or value of an intervention. There are also issues where clinicians responsible for a programme are obtaining participant feedback, especially verbally, given that the clinicians may not be as objective as those external to the programme and it might well be difcult for participants on these occasions to be honest about negative aspects of the programme. Five programmes used standardized measures, pre and immediately post programme, including the ECBI (Eyberg & Pincus 1999), the PSOC (Johnston & Mash 1989) and the PS (Arnold et al. 1993). The ECBI is considered a reliable and valid instrument for efcient screening and tracking of disruptive behaviours in children and adolescents (Burns & Patterson 1990). The PS has been found to be a valid self-report measure of parental discipline (Rhoades & OLeary 2007) while the PSOC contains three factors that reect satisfaction with the parental role, parenting efcacy and interest in parenting (Gilmore & Cuskelly 2008). It is interesting to note that clinicians considered it important to measure changes in parenting behaviour and condence as well as childrens behaviour. According to clinicians, when standardized questionnaires such as these are employed as pre-/post-evaluation measures, participants demonstrate improved parenting knowledge, skill and condence as well as a reduction in childrens disruptive behaviour. Additionally, qualitative evaluative feedback indicates that a considerable amount of time (over 12 months) is required to build trust among with these parent groups. Comparison or control groups were not employed in any of reported programmes, making it difcult to ascertain how effective the programmes were under strict evidence criteria. It is essential that rigorous evaluation designs are developed so that programme factors that best
meet the needs of parents and their children are identied. While randomized controlled trials (RCTs) are often considered the gold standard of programme evaluation, given the heterogeneous nature of this target group, RCTs may not be feasible; indeed, it has been suggested that RCTs are less sensitive to contextual issues and unanticipated causal factors that can exist in community settings than other evaluation approaches (Patton 2008). The small-scale nature of the programmes as outlined here and the ethical issues of randomly assigning participants, especially to a placebo control group (Rothman & Michels 1994), preclude the use of RCTs as an evaluation methodology for many clinicians. Moreover, many mental health professionals lack the knowledge, resources and time to implement rigorous evaluation processes such as RCTs (Reupert et al. 2009). Alternative evaluation strategies, with a particular focus on qualitative processes based in community settings, might be employed (Patton 2008) although clinicians need to be provided with the training, time and resources to do so. The programme goals identied here, particularly enhanced parenting skill and condence and peer support, provide some indication of the factors that programme evaluators might target. Finally, participant dropout was not routinely identied by clinicians. Clinicians need to identify how many participants dropout of programmes, why they dropout and when, to further inform programme development. In summary, while the data generated are limited to Australia, the ndings have important implications for others when designing and delivering programmes for parents with a mental illness. Flexible and responsive interventions, based on a peer support framework, are favoured by clinicians when supporting parents who have a mental illness with older children. Addressing parenting issues in conjunction with parents mental health needs is important when working with this group. At the same time, programme evaluation that examines the long-term impact of programmes on parenting behaviours and family well-being is required to provide empirical evidence for this clinical work.
Acknowledgments
This project was funded by the COPMI national initiative (AICAFMHA) in association with the Australian Government Department of Health and Ageing. We would like to thank the clinicians and their respective organizations for the time and support given to us in this project.
2010 Blackwell Publishing
263
A. Reupert & D. Maybery
References
Ackerson B. (2003) Coping with the dual demands of severe mental illness and parenting: the parents perspective. Families in Society 84, 109 118. Arnold D., OLeary S., Wolff L., et al. (1993) The Parenting Scale: a measure of dysfunctional parenting in discipline situations. Psychological Assessment 5, 137144. Bassett H., Lampe J. & Lloyd C. (2001) Living with under-ves: a programme for parents with a mental illness. British Journal of Occupational Therapy 64, 2328. Buist A., Minto B., Szego K., et al. (2004) Motherbaby psychiatric units in Australia the Victorian experience. Archives of Womens Mental Health 7, 8187. Burns G.L. & Patterson D.R. (1990) Conduct problem behaviors in a stratied random sample of children and adolescents: new standardization data on the Eyberg Child Behavior Inventory. Psychological Assessment 2, 391397. Craig E. (2004) Parenting programs for women with a mental illness who have young children: a review. The Australian and New Zealand Journal of Psychiatry 38, 923928. Domahidy M. (2003) Using theory to frame community practice. Journal of the Community Development Society 34, 7584. Dustin D. (2006) Skills and knowledge needed to practice as a care manager: continuity and change. Journal of Social Work 6, 293313. Eyberg S. & Pincus D. (1999) Eyberg Child Behavior Inventory & Sutter-Eyberg Student Behavior Inventory Revised. Psychological Assessment Resources, Odessa. Gilmore L. & Cuskelly M. (2008) Factor structure of the Parenting Sense of Competence Scale using a normative sample. Child: Care, Health and Development 35, 4855. Glangeaud-Freudenthal N. & Barnett B. (2004) Mother-baby inpatient psychiatric care in different countries: data collection and issues: introduction. Archives of Womens Mental Health 7, 4951.
Hickey G. & Kipping C. (1996) Issues in research. A multi-stage approach to the coding of data from open-ended questions. Nurse Researcher 4, 8191. Hinden B., Biebel K., Nicholson J., et al. (2006) A survey of programs for parents with mental illness and their families: identifying common elements to build the evidence base. The Journal of Behavioral Health Services & Research 33, 2138. Hosman C., van Doesum K. & van Santvoort F. (2009) Prevention of emotional problems and psychiatric risks in children of parents with a mental illness in Netherlands. Australian e-Journal for the Advancement of Mental Health 8, 250263. Available at: http:// www.atypon-link.com/EMP/doi/pdf/10.5172/ jamh.8.3.250 (accessed 14 May 2010). Howe D., Batchelor S. & Bochynska K. (2009) Estimating consumer parenthood within mental health services: a census approach. Australian e-Journal for the Advancement of Mental Health 8, 231249. Available at: http://www. atyponlink.com/EMP/doi/pdf/10.5172/jamh. 8.3.231 (accessed 28 April 2010). Johnston C. & Mash E.J. (1989) A measure of parenting satisfaction and efcacy. Journal of Clinical Child Psychology 18, 167175. Kitto S., Chesters J. & Grbich C. (2008) Quality in qualitative research. The Medical Journal of Australia 188, 243246. Maybery D., Reupert A., Goodyear M., et al. (2009) Prevalence of children whose parents have a mental illness. Psychiatric Bulletin 33, 2226. Oyserman D., Mowbray C.T., Meares P.A., et al. (2000) Parenting among mothers with a serious mental illness. The American Journal of Orthopsychiatry 70, 296315. Oyserman D., Bybee D., Mowbray C., et al. (2005) When mothers have serious mental health problems: parenting as a proximal mediator. Journal of Adolescence 28, 443463. Patton M. (2008) Utilization-Focused Evaluation, 4th edn. Sage, St Paul, MN. Phelan R., Lee L., Howe D., et al. (2006) Parenting and mental illness: a pilot group programme
for parents. Australasian Psychiatry 14, 399 402. Reupert A. & Maybery D. (2007) Families affected by parental mental illness: issues and intervention points for stakeholders. The American Journal of Orthopsychiatry 77, 362369. Reupert A., Goodyear M., Eddy K., et al. (2009) Australian programs and workforce initiatives for children and their families where a parent has a mental illness. Australian e-Journal for the Advancement of Mental Health 8, 277285. Available at: http://www.atypon-link.com/EMP/ doi/pdf/10.5172/jamh.8.3.277 April 2010). Rhoades K. & OLeary S. (2007) Factor structure and validity of the parenting scale. Journal of Clinical Child and Adolescent Psychology 36, 137146. Rothman K. & Michels K. (1994) The continuing unethical use of placebo controls. The New England Journal of Medicine 331, 394 398. Rubin A. & Babbie E. (2008). Research Methods for Social Work. Thomson Brooks/Cole, Belmont, CA. Sanders M. & McFarland M. (2000) Treatment of depressed mothers with disruptive children: a controlled evaluation of cognitive behavioral family intervention. Behavior Therapy 31, 89112. Steele M., Murphy A. & Steele H. (2010) Identifying therapeutic action in an attachmentcentred intervention with high risk families. Clinical Social Work Journal 38, 6172. Thomas L. & Kalucy R. (2002) Parents with mental illness: a qualitative study of the effects on their families. Journal of Family Studies 8, 3852. Webster-Stratton C. (1997) From parent training to community building. Families in Society: The Journal of Contemporary Human Services 78, 156171. Wilson D., Bobier C. & Macdonald E. (2004) A perinatal psychiatric service audit in New Zealand: patient characteristics and outcomes. Archives of Womens Mental Health 7, 71 79. (accessed 28
264
2010 Blackwell Publishing
Copyright of Journal of Psychiatric & Mental Health Nursing is the property of Wiley-Blackwell and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
Vous aimerez peut-être aussi
- Blood and ImmunityDocument4 pagesBlood and ImmunityMareeze HattaPas encore d'évaluation
- List of Successful Examinees in The May 2014 Nurse Licensure ExaminationDocument225 pagesList of Successful Examinees in The May 2014 Nurse Licensure ExaminationofwwatchPas encore d'évaluation
- Key Nursing SkillsDocument359 pagesKey Nursing Skillsmordanga100% (6)
- Nursing Care Plan For Ineffective Airway ClearanceDocument7 pagesNursing Care Plan For Ineffective Airway Clearancearlee marquez96% (118)
- Product of Your Own Personal Library Research and Creative Thinking. If You Are Not Certain About The LevelDocument5 pagesProduct of Your Own Personal Library Research and Creative Thinking. If You Are Not Certain About The LevelMareeze HattaPas encore d'évaluation
- Pathophysiology of Acute GastroenteritisDocument1 pagePathophysiology of Acute GastroenteritisJohn Glenn Bianzon79% (29)
- Family Planning Allows People To Attain Their Desired Number of Children and Determine The Spacing of PregnanciesDocument6 pagesFamily Planning Allows People To Attain Their Desired Number of Children and Determine The Spacing of PregnanciesMareeze HattaPas encore d'évaluation
- NCP-Risk For InfectionDocument2 pagesNCP-Risk For Infectioneihjay-bravo-804175% (80)
- Pathophysiology AGEDocument2 pagesPathophysiology AGEMareeze Hatta100% (1)
- Pathophysiology AGEDocument2 pagesPathophysiology AGEMareeze Hatta100% (1)
- TAHBSO PathophysiologyDocument5 pagesTAHBSO Pathophysiologybregette50% (2)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- 2014 Impacted Wisdom TeethDocument18 pages2014 Impacted Wisdom TeethkaarlaamendezPas encore d'évaluation
- Update On Hidradenitis Suppurativa: Connecting The TractsDocument11 pagesUpdate On Hidradenitis Suppurativa: Connecting The TractspancholarpancholarPas encore d'évaluation
- Jurnal 2Document7 pagesJurnal 2dania lailiPas encore d'évaluation
- How To Form An Answerable Pico QuestionDocument32 pagesHow To Form An Answerable Pico QuestionkxviperPas encore d'évaluation
- Jospt 2019 8825 PDFDocument12 pagesJospt 2019 8825 PDFLuis Sepulveda PincheiraPas encore d'évaluation
- Otitis Media Report 130504Document399 pagesOtitis Media Report 130504Yanna RizkiaPas encore d'évaluation
- The Effect of Combined Inhalation Aromatherapy With Lemon and Peppermint On Nausea and Vomiting of Pregnancy RCT 2020Document6 pagesThe Effect of Combined Inhalation Aromatherapy With Lemon and Peppermint On Nausea and Vomiting of Pregnancy RCT 2020aisyalfi pratimiPas encore d'évaluation
- The Use of Proton Pump Inhibitors in Treating and Preventing NSAID-induced Mucosal DamageDocument6 pagesThe Use of Proton Pump Inhibitors in Treating and Preventing NSAID-induced Mucosal DamageFriska Rachmanita PrayogoPas encore d'évaluation
- What Is Program EvaluationDocument42 pagesWhat Is Program EvaluationDoru ConstantinPas encore d'évaluation
- Effect of 5 Day Nitrofurantoin Vs Single Dose Fosfomycin On Clinical Resolution of Uncomplicated LUTI in WomenDocument9 pagesEffect of 5 Day Nitrofurantoin Vs Single Dose Fosfomycin On Clinical Resolution of Uncomplicated LUTI in WomenMr. LPas encore d'évaluation
- Shakespeare-Finch, Jane E. Shochet, Ian M. Roos, Colette R. Armstrong, Deanne Young, Ross Mcd. Wurfl, AstridDocument20 pagesShakespeare-Finch, Jane E. Shochet, Ian M. Roos, Colette R. Armstrong, Deanne Young, Ross Mcd. Wurfl, AstridManuel Alejandro Conejera IdígorasPas encore d'évaluation
- How I Use Platelet TransfusionsDocument12 pagesHow I Use Platelet TransfusionsJovanna OrtuñoPas encore d'évaluation
- Geriatric Care TreatmentDocument332 pagesGeriatric Care TreatmentHamss Ahmed100% (1)
- Oral Health Pregnancy Res GuideDocument36 pagesOral Health Pregnancy Res GuidemargauxPas encore d'évaluation
- 2013 ASA Guidelines Difficult AirwayDocument20 pages2013 ASA Guidelines Difficult AirwayStacey WoodsPas encore d'évaluation
- Validation of A New Tool For The Assessment of Study Quality and Reporting in Exercise Training Studies: TestexDocument10 pagesValidation of A New Tool For The Assessment of Study Quality and Reporting in Exercise Training Studies: TestexMatias Santis OlivaresPas encore d'évaluation
- III Putman, H. Paul - Rational Psychopharmacology - A Book of Clinical Skills-American Psychiatric Association Publishing (2020)Document336 pagesIII Putman, H. Paul - Rational Psychopharmacology - A Book of Clinical Skills-American Psychiatric Association Publishing (2020)Carlos Oliveira100% (4)
- Herbal Medicine Research-The Current PictureDocument6 pagesHerbal Medicine Research-The Current PictureMastermind247Pas encore d'évaluation
- The Effectiveness of Cannabinoids in The Treatment of Posttraumatic Stress Disorder PTSD A Systematic ReviewDocument21 pagesThe Effectiveness of Cannabinoids in The Treatment of Posttraumatic Stress Disorder PTSD A Systematic ReviewAnonymous opV0GNQtwPas encore d'évaluation
- ROBINS-E - LAUNCH-VERSION - 1jun2022Document76 pagesROBINS-E - LAUNCH-VERSION - 1jun2022Natalia BocanegraPas encore d'évaluation
- Effect of Music InterventionsDocument17 pagesEffect of Music InterventionsdocjenniferfranciadamoPas encore d'évaluation
- 2015 The State of Readiness For Evidence-Based Practice ADocument13 pages2015 The State of Readiness For Evidence-Based Practice Apig5evans30Pas encore d'évaluation
- Cognitively-Based Compassion Training (CBCT) in Breast Cancer Survivors: A Randomized Clinical Trial StudyDocument13 pagesCognitively-Based Compassion Training (CBCT) in Breast Cancer Survivors: A Randomized Clinical Trial StudyMuthya GhitaPas encore d'évaluation
- ESCRS EndophthalmitisDocument52 pagesESCRS EndophthalmitisKaveh Vahdani100% (2)
- Ubc 2017 September Howren AlyssaDocument104 pagesUbc 2017 September Howren AlyssaSumaiya Islam KhanPas encore d'évaluation
- UntitledDocument26 pagesUntitledAounAbdellahPas encore d'évaluation
- Clinical Standing DocumentDocument15 pagesClinical Standing DocumentPrivat EtavirpPas encore d'évaluation
- Connections of Dental ImplantsDocument8 pagesConnections of Dental ImplantsVijay Prabu GPas encore d'évaluation
- Neurodevelopmental Treatment (Bobath) For Children With Cerebral Palsy: A Systematic ReviewDocument8 pagesNeurodevelopmental Treatment (Bobath) For Children With Cerebral Palsy: A Systematic ReviewMayco BiasibettiPas encore d'évaluation
- Class II High Pull TreatmentDocument7 pagesClass II High Pull TreatmentMargarida Maria LealPas encore d'évaluation