Académique Documents
Professionnel Documents
Culture Documents
Bacteriology Midterm Lec Outline 2012
Transféré par
Kesha Marie TalloDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Bacteriology Midterm Lec Outline 2012
Transféré par
Kesha Marie TalloDroits d'auteur :
Formats disponibles
BACTERIOLOGY
LECTURE 6
Antimicrobial Drugs
Antimicrobial Sensitivity Testing
Mechanisms of Microbial
Pathogenicity Principles of Disease
Part I. Antimicrobial Sensitivity Testing
LEARNING OBJECTIVES:
Explain the concepts behind Antimicrobial
Susceptibility testing
Differentiate between the two types of
antimicrobial susceptibility testing
Discuss significant advantages &
disadvantages of each method of sensitivity
test
Interpret test results
ANTIMICROBIAL DRUGS
Recall:
Antimicrobial control methods
Physical Methods Chemical Methods
Heat
Low T
Filtration
Dessication
Osmotic Pressure
Radiation
Non-selective
phenol, etc.
Selective
antimicrobial drugs
ACTIONS of ANTI-MICROBIAL DRUGS
Inhibits cell wall synthesis
Inhibits protein synthesis
Injures plasma membrane
Inhibits nucleic acid synthesis
Competitive inhibitors
1. Penicillin
Acts by inhibiting ________________
(enzymes that catalyze cross-linking
steps in peptidoglycan synthesis)
2. Isoniazid (INH)
Inhibits ____________ synthesis
Inhibitors of Cell Wall Synthesis:
Antibacterial Antibiotics
1. Chloramphenicol
Binds 50S subunit, inhibits peptide bond
formation
2. Aminoglycosides
inhibition of initiation & misreading of mRNA
Inhibitors of Protein Synthesis
Rifampin
Binds to the DNA - dependent RNA
polymerase & inhibit synthesis of RNA
Polymyxin B
Disrupts bacterial cell membrane
Topical w/ bacitracin & neomycin
Injury to the Plasma Membrane
Inhibitors of Nucleic Acid Synthesis
a. Trimethoprim
b. Sulfonamides
Targets folic acid pathways
Differs in the enzyme inhibited
inhibit specific metabolic steps necessary
for bacterial growth
Trimethoprim-sulfamethoxazole
COMPETITIVE INHIBITION
Effects of Combinations of
Drugs
Synergy
Indifference
Antagonism
REASONS FOR USE OF
MULTIPLE THERAPY:
Polymicrobial infections
Achieving more rapid bactericidal activity
than use of a single agent
No single agent is lethal
Minimizing the risk of resistance
organisms emerging during therapy
PRINCIPLE:
It measures the ability of an antibiotic or
other antimicrobial agent to inhibit
bacterial growth in vitro.
ANTIMICROBIAL SENSITIVITY TESTING
To guide the clinician in selecting the
appropriate antimicrobial agent
To gather epidemiological data on microbial
resistance
PURPOSE:
STANDARDIZATION:
1. Bacterial inoculum size
2. Growth medium
thickness
pH
Composition
3. Incubation atmosphere
4. Incubation Temperature
5. Incubation Duration
6. Antimicrobial concentration tested
GENERAL
CONSIDERATIONS
Inoculum Preparation
+Pure inoculum
+McFarland Turbidity Std
1%H
2
SO
4
+ 1.175%BaCl
1.5x10
8
CFU/ml
Selection of Antimicrobial
Agents for Testing
Antimicrobial battery or panel
CLSI provides up-to-date list of
potential antimicrobial agents for
testing against a particular
organism.
I. Diffusion method
II. Dilution method
III. E- test
Diffusion Method
C antibiotic paper discs are placed on
agar medium seeded with the test
organism.
1. Disk Diffusion Method
2. Agar Overlay Disk Diffusion
I. DISK DIFFUSION:
Kirby-Bauer Technique
1. Inoculum preparation
2. Inoculation of agar plates
3. Application of disks to agar surface
4. Incubation of plates
5. Reading & interpretation of results
Appropriate Media for Sensitivity
Testing
Mueller-Hinton agar
MH w/ 5% sheep blood
MH w/ 2% NaCl
HTM - H. influenzae
GC agar w/ PolyVitex
Disk Application :
Apply disks within 15 mins. after
inoculation of agar surface.
Proper spacing of antibiotic disks
Ideal: 18-24 hours @ 37C
For fastidious organisms like:
H. influenzae
N. gonorrhoeae
S. pneumoniae
35C w/
5-7% CO
2
Incubation
Reading & Interpretation
of Results
Measure the zone of
inhibition around each disk
Record in mm
Compare results using
NCCLS interpretative chart
Report as susceptible,
intermediate or resistant
Organism
Antimicrobial
agent
(disk
content)
Zone diameter
Equivalent
MIC
Breakpoint
(g/ml)
R
I
S
R
S
S. aureus
1 g
< 10
11-12
> 13
> 4
< 2
CNS
1 g
< 17
> 18
> 0.5
< 0.25
1. Sensitivity
2. Intermediate
3. Resistance
ADVANTAGES:
Convenient & user friendly
Up to 12 antimicrobial agents can be
tested
Minimal use of extra materials & devices
II. AGAR OVERLAY DISK DIFFUSION
METHOD
DISADVANTAGES:
Lack of interpretative criteria
Inability to provide more precise
data regarding the level of an
organisms resistance or
susceptibility as can be provided by
MIC methods
DILUTION METHODS
A. BROTH DILUTION
MIC: The lowest antimicrobial concn that
completely inhibits visible bacterial growth
MBC: Lowest antimicrobial concn that kills
bacteria
B. AGAR DILUTION
uniformly diluted antibiotic concn are
incorporated in MH
DILUTION METHODS
combination of ease in disk
diffusion & accuracy of broth
dilution mtd.
Uses rectangular plastic strips
with predetermined gradient of
antibiotic concn that correspond
to MIC dilution
Elliptical zone of inhibition
Estimates MIC
E- test (Epsilometer test)
A. Methicillin-Resistant S. aureus
pathogenic
common causes of nosocomial infection
transmissible
vancomycin (severe MRSA)
Specific Testing Procedures for
Organisms of Medical Interest
Reading and Interpretation of results
Incubation at 35C for full 24 hours
Application of 1ug Oxacillin disk
Inoculation on MH (with 2% NaCl)
Test Inoculum
Points to Remember
For MRSA and MRS
Penicillins, cephems, carbapenems &
other -lactams are not effective clinically.
Reported as resistant or not reported at
all.
B. Vancomycin Resistant Enterococci
Mueller-Hinton agar
Direct colony suspension
35C ambient air for 24 hrs
Cephalosporins, clindamycin,
trimethoprim/sulfamethoxazole
are not clinically effective.
Chloramphenicol
Erythromycin
Tetracycline
Rifampin
Points to Remember
For Enterococcus spp.:
Part II. Microbial Mechanisms of
Pathogenicity & Principles of Disease
and Epidemiology
LEARNING OBJECTIVES:
1. Define terms.
2. Correlate factors of pathogenecity &
virulence.
3. Discuss the mode of transmission of
bacterial infections.
Microbial Mechanisms of
Pathogenicity
Pathogenicity
Virulence
I. Portals of Entry:
Mucous membranes
Skin
Parenteral route
II. Portals of Exit:
RT Skin
GIT Blood
GUT
Adhesins / Ligands bind to receptors on
host cells:
Glycocalyx
Fimbriae
M protein
Opa protein
Tapered end
III. Adherence
Capsules & organs of locomotion also contribute to
microbial pathogenicity.
Coagulase
Kinases
Hyaluronidase
Collagenase
IgA proteases
Siderophores
IV. Enzymes
Antigenic variation
V. Toxins
Toxin
Toxigenicity
Toxemia
Toxoid
Antitoxin
Exotoxins
Figure 15.4a
Endotoxin
Type I toxins
Cause intense immune response due to release
of cytokines from host cells
Exotoxins
Type II toxins
Disrupting phospholipid bilayer making protein
channels
Type III toxins
with active & binding components
alters cell function by inhibiting protein synthesis
Figure 15.6
Endotoxins Exotoxins
Source
Metabolic
product
Present in
LPS of outer
membrane
By-products of
growing cell
Chemistry
Fever
Neutralized
by antitoxin
LECTURE 7
Principles of Disease
Pathology Study of disease
Etiology
Pathogenesis Development of disease
Infection
Disease An abnormal state in w/c
the body is not normally
functioning
Symptom
Sign A change that can be measured
or observed as a result of
disease.
Syndrome
Classifying Infectious Diseases
Communicable A disease that is easily
spread from one host
to another.
Noncommunicable A disease that is
not transmitted from
one host to another.
Acute disease Symptoms develop
rapidly
Chronic disease Disease develops
slowly
Subacute disease Bet. acute & chronic
Latent disease inactive infection; a
period of no symptoms
Severity or Duration of a Disease
Local infection Pathogens limited to
an area of the body
Systemic infxn An infxn throughout the
body
Focal infection Systemic infxn that
began as a local
infection
Bacteremia Bacteria in the blood
Septicemia Bacterial Growth in blood
Toxemia
Primary infxn Acute infxn that
causes the initial
illness
Secondary Opportunistic infxn
infection after a primary
infection
Subclinical dse No noticeable S/S
Age
Gender
Genes
Climate & weather
Lifestyle (Fatigue / Stress)
Race
Chemotherapy
Pre-existing conditions
The Stages of Disease
Figure 14.5
Continual Sources Of Infection
(RESERVOIRS):
Human
Animal
Nonliving (Soil)
A. Contact
Direct
Indirect
Droplet
B. Vehicle
C. Vectors
Mechanical
Biological
Transmission of Disease
Bacteria were once classified as plants
Microbiota
+ Transient microbiota
+ Normal microbiota
+ Opportunistic microbiota
Symbiotic relationship
Commensalism
Mutualism
Parasitism
NORMAL MICROBIOTA
Figure 14.2
Normal Microbiota and the Host:
prevent growth of pathogens by
occupying niches that pathogens might
occupy
produce growth factors such as folic acid
and vitamin K
Probiotics
BENEFICIAL EFFECTS of the
NORMAL MICROBIOTA:
GRAM POSITIVE COCCI
Staphylococcus
Streptococcus
LEARNING OBJECTIVES
At the end of this unit, the student is able to:
1. Describe Staphylococcus & Streptococcus in
terms of their general properties and
pathogenesis
2. Discuss the identification of characteristics in
terms of morphology, culture media, colony
characteristics, biochemical test, and serological
test
3. Explain the principles/concepts of different
identification techniques used
4. Prepare a schematic diagram for identification
3 SPECIES OF CLINICAL
IMPORTANCE:
Staphylococcus aureus
Staphylococcus epidermidis
Staphylococcus saprophyticus
General Characteristics
Most important genus in the family
_________________
Gram positive spherical cells in grape-like
clusters
Non-motile, non-encapsulated*, non-
sporeforming
aerobic or microaerophilic
strongly catalase (____)
pyogenic
formerly ______________________________
fastidious organism
most strains on primary isolation produce a
____________ pigment
often hemolytic on blood agar
+ OF
grow at a temperature range of _______ C
grow at NaCl concentrations
produce coagulase
Staphylococcus aureus
1. Peptidoglycan
Elicits production of _______ & __________
by monocytes
Chemoattractant for PMNs
Have endotoxin-like activity
Activates complement
2. Protein A
binds to Fc region of IgG
Anti-opsonization
Major Virulence Factors
ANTIGENIC STRUCTURES
3. Clumping Factor
Binds to fibrinogen & fibrin
causing bacterial aggregation
4. Teichoic Acid
mediates adhesion by binding to
tissue fibronectin
ENZYMES
1. Coagulase
Binds to ___________ causing fibrin
polymerization
prevents opsonization & phagocytosis
2. Catalase
Breaksdown ________
into ______ & _____
3. Staphylokinase
Major Virulence Factors
3. Lipase: plays role in pathogenesis of
boils and acne
4. Hyaluronidase: hydrolyzes hyaluronic
acid
5. Nucleases: cleave DNA and RNA
Toxins
1. Hemolysin
2. Leukocidin
3. Enterotoxin: heat-labile; resistant to
GIT enzymes
4. Exfoliative Toxin
5. Toxic Shock Syndrome Toxin 1
Prototype ___________
TSS: fever, shock, desquamative rash,
multisystem involvement
Modes of Transmission:
Person to person
Ingestion of contaminated food
Aspiration of nasopharyngeal
secretions
Types of Staphylococcal Diseases:
Local Abscesses
Focal Suppuration
Diseases caused by toxin elaboration
Pathogenesis and Clinical
Manifestations
LOCAL
ABSCESSES
Folliculitis
Furuncles
Carbuncles
Osteomyelitis
Pneumonia
Meningitis
Empyema
Endocarditis
Sepsis
Skin infections
FOCAL
SUPPURATION
EXOTOXIN ELABORATION
Gastroenteritis
S. aureus (on food) = Toxin ingested =
Interacts with mucosa = Vomiting, Diarrhea
Toxic shock syndrome
S. aureus (on tampons) = TSST-1 enters the
bloodstream = Fever, rash, hypotension
Scalded skin syndrome
Diagnostic Laboratory Tests
A. SPECIMEN: blood, surface swab, pus, etc.
B. MICROSCOPIC: gram (+) cocci in clusters
C. CULTURE: 18-24 hrs. @ 37C
BAP: large, creamy, opaque colonies, usually
-hemolytic; golden yellow pigment
D. BIOCHEMICAL :
Catalase (__), MSA (__), Coagulase (___)+
Staphylococcus epidermidis
Normal flora but can be opportunistic
Frequent skin contaminant in blood culture
Colonizes prosthetic devices
Produces slime-layer
1. Gram Stain: GPC in clusters
2. Culture: gamma hemolytic (BAP)
________ colonies on primary isolation
3. Biochemical:
Catalase (___)
Coagulase (___)
MSA (___)
Diagnostic Laboratory Tests
Staphylococcus saprophyticus
An important cause of UTI
2
nd
to E. coli
Up to 30% of UTI in young, sexually active
women
1. GS: GPC in clusters
2. Culture: -hemolytic
3. Biochem:
Catalase (___)
Coagulase (___)
4. Resistant to _________ &
___________
Diagnostic Laboratory Tests
Treatment and Prevention
For S. aureus :
Handwashing; local antisepsis
Drainage of pus
Surgical drainage, removal of tissue
Antimicrobial Therapy:
Methicillin, nafcillin, cloxacillin etc.
Vancomycin
Tetracyclines
For S. epidermidis:
Difficult to treat. Removal of the
prosthetics may be done.
40% of coagulase(-) staphylococci are
resistant to -lactamase resistant
antibiotics
vancomycin
Rifampin & gentamicin
Group Characteristics:
Gram-positive cocci in _______
Catalase (____)
Nutritionally fastidious
Hemolytic
Some are encapsulated
facultative anaerobes
requires enriched medium
Clinically Significant Pathogens:
Grp A
Grp B
Grp D
Streptococcus pneumoniae
Viridans group
Smith & Brown Classification:
________________ of streptococcus in BAP
Bergeys/Academic Classification
based on the physiologic divisions of
streptococcus or __________________.
Lancefields Classification
based on the presence of serologically active
______________________ (cell wall CHO)
Classification of Streptococci
Smith & Brown Classification
Alpha
hemolytic
partial hemolysis of RBC
greenish discoloration
Beta
hemolytic
complete hemolysis of
RBC
clear zone of hemolysis
surrounding bacterial
colony
Gamma
hemolytic
non-hemolytic or
indifferent strep
no hemolysis of RBC
Bergeys/Academic Classification
Pyogenic
Streptococci
neither 45C nor 10C
produce pus
mostly - hemolytic
Viridans
Streptococci
grows at 45C not at 10
normal mouth flora
Enterococcus
Group
grows at 45 & 10C
Lactic Group
grows at 10C but not at
45C
LANCEFIELDS
CLASSIFICATION
Group A
predominantly pathogenic for man
beta hemolytic
causes strep throat, rheumatic fever, post-
streptococcal glomerulonephritis, scarlet
fever
the most virulent for humans.
obligate human parasite.
person to person; spread by respiratory
secretions.
1. Capsule
2. M protein:
precipitates _________________
clumps platelets & leucocytes, inhibits
migration of leucocytes
inhibits activation of complement
Major Virulence Factors
ANTIGENIC STRUCTURES
3. IgG & IgA-binding proteins:
Binds to _________ of IgG or IgA.
4. C5a protease:
cleaves C5a component of complement
inhibits neutrophil chemotaxis in vitro
5. Lipoteichoic acid:
Attachment of organism to __________
6. Group-specific cell wall antigen:
basis of serologic grouping
TOXINS & ENZYMES
1. Streptokinase
2. Streptodornase
3. Hyaluronidase
4. Pyrogenic Exotoxins:
A, B, C
Associated with ___________ & ___________
5. Diphosphopyridine Nucleotidase
Associated with the organisms ability to destroy
____________
6.Hemolyins:
Streptolysin O :
destroys red & WBC (hemolysis)
Inactivated by oxygen
Antigenic ASO
Streptolysin S :
responsible for hemolysis (BAP)
Elaborated by serum
Non-antigenic
Pyogenic Diseases
Erysipelas
Cellulitis skin infections
Impetigo
Streptococcal Pharyngitis
Pathogenesis and Clinical
Manifestations
Toxigenic Diseases
Necrotizing fasciitis
Scarlet Fever
Streptococcal Toxic Shock Syndrome:
S. pyogenes grows in ______________
Bacteria enter the bloodstream & produce ________
Fever, rash, shock, bacteremia, respiratory failure
Poststreptococcal Diseases
Acute rheumatic fever
Acute glomerulonephritis
Preceeded by skin or respiratory infections
Represents a hypersensitivity response
Diagnostic Laboratory Tests
A. SPECIMEN: depends on nature of infection
B. MICROSCOPIC: gram (+) cocci in pairs or chains
C. CULTURE: 18-24 hrs. @ 37C
BAP: -hemolytic, discoid, matte or glossy
colonies
Grows in 10%CO2
D. BIOCHEMICAL :
Catalase (-), Taxo A/Bacitracin Disk test (S)
PYR Test : L-pyrolidonyl-B-naphthylamide
PRINCIPLE:
PYR Hydrolysis of by GAS (enterococcal
group can also hydrolyze PYR)
RESULTS:
(+) = bright cherry red color after the
addition of PYR reagent (N,N dimethyl-amino
cinnamaldehyde)
E. Serological test: ASO (anti-streptolysin O)
SCARLET FEVER SUSCEPTIBILITY TESTS
1. Dicks Test :
inject 0.1ml toxin & 0.1ml toxoid
Observe for 24 hrs.
(+) ___________ in test arm
2. Schultz-Charlton Test:
Inject anti-toxin into test arm
(+) _______________
Group B Streptococcus:
Streptococcus agalactiae
has polysaccharide capsule (w/ sialic acid)
antiphagocytic
inhibits complement activation
Its ability to mimic host molecules enhances
pathogenicity.
Beta hemolytic
URT, GIT & GUT (female) normal flora
Adults: GBS is part of the normal
___________ flora in _______ of adults.
Children: more susceptible than adults.
Infants/ Neonates:
Organisms ascend from the vagina and infect the
amniotic fluid through the placental membranes.
passage through the birth canal.
Modes of Transmission:
1. CAMP Test in BAP
(+): ____________________
2. Hydrolysis of Na Hippurate
Diagnostic Laboratory Tests
0.4 ml 1%
Na
hippurate
loopful of
organisms
incubate 32C
for 10 mins.
+
reincubate 37
for 10 mins
0.2ml
ninhydrin
solution
+
(+) __________________
Normal GIT and fecal flora
_____________ and _____________
Grows on ___________ media
Non-hemolytic or -hemolytic
May be weakly catalase (+)
UTI, Endocarditis, abscesses, Wound
infection
Group D (Genus Enterococcus)
2 Classifications
Species 6.5%
NaCl
penicillin
resistance
PYR
Entero-
coccal
group
S. faecalis,
S. durans,
S. faecium,
S. avium
Non-entero
coccal
group
S. bovine,
S. equinus
Streptococcus pneumoniae
Pneumococcus
formerly ______________________
Gram(+) _______________diplococcus
encapsulated, non-motile, non-spore
forming, facultative anaerobe,
Capnophilic; alpha-hemolytic; fastidious
Major Virulence Factors
Capsule:
Antiphagocytic
Antigenic; immunologically distinct for each type
vaccine component
Pneumolysin:
facilitates adherence to the host during
______________
damages host cells by forming spores during
______________
interferes with the host immune response during
______________
Epidemiology, Pathogenesis &
Clinical Manifestations
Present in the nasopharynx:
* 10% of healthy adults
* 40% of asymptomatic children
RT = sinuses & middle ear = _______ &
_________
Major cause of community-acquired
_______________; most common in U.S.
1. Microscopic:
Gram(+) lancet-shaped diplococci
2. Culture:
Mucoid, dome shape colonies which later
develops a "crater" like appearance
BAP: -hemolytic;____________% CO2
3. Lab Test:
Optochin Test
Bile Solubility Test
Quellung Test
Diagnostic Laboratory Tests
S. salivarius
S. sanguis
S. mitis
S. intermedius
S. mutans
S. constellatus
VIRIDANS GROUP
BAP: -hemolytic w/
_______ discoloration
URT Normal Flora
seen in nasopharynx
& gingival crevices
3 Main Types of Infection:
1. Dental Infections:
bind to teeth & ferment sugar = acid ________
2. Endocarditis:
implanted on endocardial surfaces of the heart
(damaged heart valves) cling to valves =
_______________________
3. Abscesses
S. intermedius, S. constellatus, S.anguinosus
form abscess in brain or abdominal organs
Penicillin G
Clindamycin
Erythromycin
Ampicillin or vancomycin
1
st
generation cephalosporin
3
rd
generation cephalosporin with or without
vancomycin
TREATMENT & CONTROL
CONTROL
Multivalent pneumococcal vaccine
(splenectomized and immunocompromised)
ASSIGNMENT
Micrococcus and Peptostreptococcus are the
other groups of gram positive cocci. In tabular
form, show the similarities as well as the
differences of these organisms to the 2 coccal
groups that were discussed earlier in terms of
general, microscopic, cultural and biochemical
characteristics.
(Answers must be handwritten on legal sized
bond paper.)
Learning Objectives
Each student will be able to:
Identify the medically significant Gram-negative
cocci;
Differentiate based on phenotypic
characteristics, pathogenicity and virulence
factors;
Recognize the importance of performing
appropriate laboratory procedures in the
diagnosis of neisserial infection or disease
Genera & species to be
considered
Neisseria
N. gonorrheae = _____________
(GC)
N. meningitidis =
_____________(MGC)
Other Neisseria spp.
N. cinerea, N. lactamica, N.
polysaccharea, N. sicca, N. subflava,
N. mucosa, N. flavescens, N.
elongata
Moraxella catarrhalis
(formerly Branhamella catarrhalis,
Neisseria catarrhalis)
Morphology & Identification
A. Typical neisseria
o Gram-negative diplococci
o Nonmotile
o Approximately 0.8 m in diameter
o Individual cocci kidney-shaped
o In pairs, the flat or concave sides
are adjacent
Morphology & Identification
B. Culture
o On enriched media in 48 hours
o Gonococci/meningococci
o Convex, glistening, elevated,
mucoid colonies 1-5 mm in
diameter
o Transparent or opaque,
nonpigmented, nonhemolytic
Morphology & Identification
B. Culture
o N. flavescens, N. cinerea, N.
subflava, N. lactamica
o May have _________ pigmentation
o N. sicca
o Opaque, brittle, wrinkled colonies
o Moraxella catarrhalis
o Nonpigmented or pinkish gray
opaque colonies
Morphology & Identification
C. Growth/Biochemical
Characteristics
o Neisseriae grow best under
aerobic conditions
o some grow best in anaerobic
environment
o atmospheric requirement: 5%
CO
2
(__________)
Cultivation / Isolation
o MTM
o ML
o GC-Lect
o NYC
Morphology & Identification
Antibiotic component:
o vancomycin, 3 g/mL
o __________, 7.5 g/mL
o amphotericin B, 1 g/mL
o trimethoprim, 3 g/mL
Growth on MTM, ML, NYC
POSITIVE GROWTH:
N. gonorrheae
N. meningitidis
N. lactamica
VARIABLE GROWTH:
N. cinerea, N. polysaccharea
NEGATIVE GROWTH:
N. sicca, N. subflava, N. mucosa, N.
flavescens, N. elongata, Moraxella
catarrhalis
Morphology & Identification
C. Growth/Biochemical Characteristics
o _______ test a key test for ID
o DARK PURPLE
o rapid test filter paper soaked with
tetramethylparaphenylene diamine
hydrochloride
o Most oxidize carbohydrates producing acid
but not gas
o CARBOHYDRATE PATTERNS means
of distinguishing them
o ___________________ (CTA) sugars
Species
Tests/Results
CTA Carbohydrates
Oxidase
Glucose Maltose Lactose Sucrose
N.
gonorrhoeae
- - -
N.
meningitidis
- -
N.
lactamica
-
M.
catarrhalis
- - - -
M. catarrhalis = DNAse positive
Morphology & Identification
C. Growth/Biochemical
Characteristics
o Inhibited by toxic constituents
o Rapidly killed by _______, sunlight,
moist heat, and many disinfectants
o Produce autolytic enzymes
typical _________ colonies with
__________ GC on selective
subculture
larger colonies with ________
GC on nonselective subculture
Opaque and transparent colony
variants occur
T1, T2, T3, T4 colonies
Antigenic heterogeneity of gc
A.Pilin
B.Por protein
A.PorA, 18 subtypes
B.PorB, 28 subtypes
C.Opa
D.Rmp
E. Lipooligosaccharide
F. Fbp
G.Lip
H.IgA1 protease
Antigenic heterogeneity of gc
A. Pilin
B. Opa (protein II)
C. Lipooligosaccharide (LOS)
gonococcal LPS without long O-antigen side chains;
endotoxic effects, cause ciliary loss and mucosal cell
death;
molecular mimicry of human glycosphingolipids
All 3 are surface-exposed antigens; molecules rapidly
switch to elude the host immune system.
Antigenic heterogeneity of gc
D. Por protein
E. Rmp (protein III) reduction-modifiable protein;
associates with Por in the formation of pores in the
surface
Poorly defined roles:
F. Fbp (ferric-binding protein)
G. Lip (H8) heat modifiable protein like Opa
H. IgA1 protease 1
PATHOGENESIS, PATHOLOGY & CLINICAL
FINDINGS
GC attack mucous membranes
(GUT, eye, rectum, throat)
acute suppuration
tissue invasion
chronic inflammation & fibrosis
Uncomplicated GC infection
Uncomplicated infections in males: incubation=
1- 4 days
Acute URETHRITIS
with profuse purulent discharge
filled with GC
painful urination; some asymptomatic
If untreated : PROSTATITIS, EPIDIDYMITIS.
PHARYNGITIS: mild With oropharyngeal
infection
PROCTITIS: With rectal infection.
PATHOGENESIS, PATHOLOGY & CLINICAL
FINDINGS
Uncomplicated infections in females:
increased vaginal discharge, burning or frequency of
urination and menstrual abnormalities, dyspareunia;
URETHRITIS, minimal urethral discharge; more likely
asymptomatic
gonococcal ___________ neonatorum
Infected mothers transmit GC to their babies at birth.
blindness; all babies are given
erythromycin/tetracycline/silver nitrate eye drops
at birth to prevent this.
PATHOGENESIS, PATHOLOGY & CLINICAL
FINDINGS
Complicated infections occur more frequently in
women.
Spread from the cervix into the fallopian tubes
ENDOMETRITIS, SALPINGITIS, & OOPHORITIS =
_____________________________________ (PID)
Symptoms include lower abdominal pain, abnormal
vaginal and cervical discharge, and uterine
tenderness.
Complications: ectopic pregnancy, infertility,
peritonitis, peri-hepatitis (Fitz-Hugh-Curtis
syndrome).
PATHOGENESIS, PATHOLOGY & CLINICAL
FINDINGS
Complicated infections of GC
Spread to the bloodstream may result in
disseminated gonococcal infection (DGI) in both
men and women (1%)
Gonococcal bacteremia: ENDOCARDITIS,
ARTHRITIS, MACULOPAPULAR RASH, & MENINGITIS
Septic arthritis common in young, sexually
active individuals
Diagnostic Laboratory Tests
Gram-negative cocci
CATALASE &
OXIDASE POSITIVE
CTA SUGARS
GLUCOSE ONLY
Others:
Coagglutination
Immunofluorescence
staining
Immunoblotting, RIA,
ELISA
Neisseria
gonorrheae
Specimens
PUS/SECRETIONS (Urethra, cervix, rectum,
conjunctiva, throat, synovial fluid)
Blood culture (special system-SPS susceptible)
Treatment
+Rise of gonococcal resistance to penicillin
___________-producing N. gonorrheae (PPNG)
Tetracycline, spectinomycin, Fluoroquinolones
+CDC recommended:
ceftriaxone (125 mg) IM single dose,
add azithromycin 1 g orally, single dose or with
doxycycline 100 mg orally 2x a day for 7 days
(for possible concomitant chlamydial infection)
Neisseria meningitidis
+13 serogroups: immunologic specificity of
___________ POLYSACCHARIDES
+Disease causing: A, B, C, X, Y, and W-135
+Group A polysaccharide
a polymer of N-acetylmannosamine phosphate
Group C polysaccharide
a polymer of N-acetyl-O-acetylneuraminic acid
Meningococcal antigens found in blood and
CSF with active disease.
Pili - bind to specific nasopharyngeal
receptors
Type IV pili of MGC interact w/ brain
endothelial cells
Opc protein attachment and invasion
LOS with same functions as GC LOS
Pili, Opa, LOS, and to a lesser extent,
Opc, undergo antigenic variation
Neisseria meningitidis
Neisseria meningitidis
Class 1,2, and 3 OUTER MEMBRANE
PROTEINS (analogous to Por) porins
for intracellular survival
Class 5 outer membrane protein (Opa) -
attachment, induced uptake (invasion)
Class 4 outer membrane protein (rmp) -
blocks host serum bactericidal (IgG)
action
Clinical significance
endemic and epidemic
CEREBRAL ___________
Most common in children under
1year, adolescents, and young adults.
Can be part of the normal flora of the
nasopharynx
Asymptomatic carriers 1 source of
aerosol spread
Colonization of the nasopharynx usually
results in a subclinical infection or a mild
upper respiratory tract infection like the
common cold.
MGC infections
Bloodstream invasion occurs only in
individuals lacking bactericidal antibodies or
deficient in certain complement components
(C5-C8).
Predisposing factors: Chronic irritation or
damage to the respiratory mucosa.
Invasion of the bloodstream may result in
septicemia (meningococcemia) or
meningitis.
Meningococcemia
high fever, shaking, chills, muscle pain, hypotension
& ______________(hallmark of MGC infections).
Disease may be chronic, moderate or fulminant.
Fulminant type: ________________________________
Characterized by disseminated intravascular coagulation
(DIC), with hemorrhaging into the skin, adrenal glands
and other internal organs.
Acute generalized toxemia & shock Rapid death
Symptoms due to endotoxin activity (LOS).
Patients may lose their limbs from tissue necrosis (gangrene of
the skin and soft tissues).
MGC infections - Meningitis
+Fever, headache, stiffness of back and neck
(nuchal rigidity), and petechial rash
+Severe cases = severe cerebral hyperemia
+May progress to convulsions and coma
+Invariably fatal without rigorous antimicrobial
therapy.
+Patients who recover 11%-19% have
permanent hearing loss or
________________
Clinical significance
Other Neisseria species - rarely associated
with endocarditis, septicemia, and
meningitis.
M. catarrhalis - may be a significant cause
of ________ and maxillary sinusitis in
children
May cause pneumonia and bronchitis in
immunocompromised individuals.
May also occasionally cause endocarditis,
meningitis and septicemia.
DIAGNOSTIC LABORATORY
TESTS
Blood for culture
method (without SPS)
CSF for smear,
culture, & chemical
determinations
Nasopharyngeal swab
cultures for carrier
surveys
Puncture material from
petechiae for smear
and culture
Chocolate agar or
TM/MTM
37C, 5% CO
2
Oxidase
Test
Agglutination with type-
specific or polyvalent
serum
GLUCOSE &
MALTOSE
Treatment
oMGC- I.V. penicillin G (drug of choice)
If allergic, chloramphenicol, erythromycin or a
third-generation cephalosporin, eg,
cefotaxime or ceftriaxone.
Prophylaxis with rifampin, ciprofloxacin, or
ceftriaxone for household and other close
contacts
O Vaccines are available for the virulent
types of MGC.
O They are given to those at risk (e.g. college
students in dorms, army recruits) in endemic areas.
Gram Positive Bacilli
LEARNING OBJECTIVES
1. Describe GRAM POSITIVE BACILLI in terms of their
general properties & pathogenesis.
2. Discuss & explain the identification of characteristics
in terms of morphology, cultural characteristics,
biochemical & serological test.
3. Differentiate pathogenic from nonpathogenic
members of the genus .
4. Prepare a schematic diagram for identification
At the end of this unit, the student is able to:
SPORE-FORMING GRAM
POSITIVE BACILLI
Bacillus
Clostridium
Spore-forming Bacilli :
BACILLUS
Bacillus anthracis
Bacillus cereus
Large gram(+) rods
endospore-forming
non-motile
Mostly saprobic (soil)
Aerobic ; catalase (+)
Bacillus anthracis
Large, square ended, encapsulated, non-
motile Gram (+) bacilli
Ellipsoidal to oval centrally located spore
Occur in long chains (bamboo appearance)
Determinants of Pathogenicity
Capsule
Anthrax toxin
Protective Antigen
binds to specific cell receptors
Allows entry of LF & EF into cells via channels
Lethal factor
LF + PA
LT
Edema factor
EF + PA
Clinical
Syndromes
Cutaneous anthrax
_____________________
Transmission: skin abrasions
Pulmonary anthrax
______________disease
Transmission: inhalation of spores
Gastrointestinal anthrax
_________ enteritis
Ingestion of spores
Invasion, ulceration of GI mucosa
Laboratory Diagnosis
SPECIMENS:
Swabs (pus)
Sputum, Stool
Blood
MICROSCOPY
GS, India ink & FAT
SEROLOGY
Use of gamma bacteriophage
IHA, ELISA
Laboratory Diagnosis
Culture
Optimal growth temperature is at 35
O
C
(BAP)
non-hemolytic, raised, opaque, grayish white;
cut glass appearance
irregular fringe-like margin
(PLET)
(GELATIN)
Chemotherapy and Control
CHEMOTHERAPY
Ciprofloxacin
Penicillin G, streptomycin, gentamicin
CONTROL
Active immunization
Bacillus cereus
Similar to B. anthracis; motile
-hemolytic, small, shiny, compact or
large feathery and spreading colonies
Cause food poisoning:
SHORT INCUBATION TYPE
LONG INCUBATION TYPE
TREATMENT:
Chloramphenicol, aminoglycosides,
clindamycin
Erythromycin and Vancomycin
Other clinical infections:
Eye infections
Local and systemic infections
B. cereus
B. anthracis
Motility motile
non-motile
Capsule
Hemolysis Beta hemolytic Non-hemolytic
Growth at 45
O
C
Salicin
fermentation
(+) (-)
Penicillin
sensitivity
Gamma phage R S
+obligate anaerobe
+Most are motile with peritrichous flagella
+Spores may be terminal, subterminal or
centrally located.
+Many can produce zones of hemolysis on
BAP.
Spore-forming Bacilli :
CLOSTRIDIUM
Clostridium botulinum
Motile w/ peritrichous flagella
Produces heat-resistant spores when
grown on Alkaline Glucose Gelatin
Heat resistance is diminished at acid pH
or high salt concentrations
VIRULENCE FACTORS
Exotoxin
the most potent toxin
released on autolysis of bacteria
blocks release of acetylcholine resulting
in flaccid paralysis
Destroyed at 100C for 20 mins.
DISEASES
Food-borne botulism
Infant botulism
Wound botulism
CULTURAL CHARACTERISTICS
BAP
Strict anaerobe
All strains, except type G, are beta hemolytic
Clostridium tetani
Peritrichous flagella; Terminal spore
Drumstick/ tennis racket appearance
Virulence Factors:
Tetanolysin
Tetanospasmin
Blocks inhibitory neurotransmitters
Leads to muscle spasms,spastic paralysis
CULTURAL
CHARACTERISTICS
BLOOD AGAR PLATE
Swarming colonies
w/ delicate flat edge of
projecting filaments
Faint beta hemolysis
Does not ferment any carbohydrates
TREATMENT
Antitoxin (250-500 units of tetanus Ig)
Tetanus toxoid
Debridement of wound & removal of
foreign bodies
Penicillin, tetracyclin or metronidazole
Barbiturates, diazepam (spasms)
Clostridium perfringens
C. welchii, Bacillus aerogenes
capsulatus
Gas Gangrene bacillus
Short, plump, encapsulated, non-motile
No spores in ordinary media
Virulence Factors
-toxin = Lecithinase; in Type A strains
-toxin = with similar hemolytic & necrotizing
properties
Enterotoxin = spore coat component
= Formed when _____ vegetative
cells are ingested
DNAse, Hyaluronidase
CLINICAL INFECTION
Wound & soft tissue infxn
Type A strains C. perfringens
Food poisoning
Type A strains w/ spores & minimal amount
of -toxin
Necrotizing enteritis or pig-bel
Ingestion of inadequately cooked pork
S/S are due to -toxin of Type C strains
LABORATORY DIAGNOSIS
SPECIMEN: wound, tissue, pus
CULTURAL: anaerobic
BAP: circular smooth colonies
CHOPPED-MEAT GLUCOSE
abundant growth; (+) gas
BIOCHEMICAL:
Milk Media : STORMY fermentation
Lecithinase Test
lecithinase splits lecithin into insoluble
diglycerides
Clostridium difficile
Motile (peritrichous flagella); Non-encapsulated
TOXINS:
Toxin A = Potent enterotoxin; weakly cytotoxic
Toxin B = potent cytotoxin
Antibiotic associated pseudomembranous
enterocolitis
Watery/bloody diarrhea, abdominal cramps,
leukocytosis, fever
LABORATORY DIAGNOSIS
SPECIMEN: Stool or rectal swabs
MICROSCOPY:Gram stain (+)
CULTURE:
Cycloserine Cefoxitin Fructose Agar
SEROLOGY:
Rapid Latex Agglutination Test
toxin A detection
TREATMENT
Discontinue administration of offending
drug
Metronidazole , vancomycin (oral)
Gastrointestinal stimulants
Stool softeners and enemas
NONSPORE-FORMING GRAM
POSITIVE BACILLI
AEROBIC
Corynebacterium
Listeria
Erysipelothrix
Nocardia
ANAEROBIC
Actinomyces
Propionibacterium
Corynebacterium diphtheriae
__________________ bacillus
non-AF, non-motile, non-spore forming,
^G-C
Palisade, Chinese character appearance
club-shaped
___________ granules
DIPHTHERIA
fever, malaise, mild sore throat
bull neck appearance
Virulence Factor:
Diphtheria Toxin
produced after _____________________
Cause epithelial destruction, inflammation
Laboratory Diagnosis
SPECIMEN:
Nasopharyngeal swabs
MICROSCOPY:
GS and AFS
CULTURE:
BAP
Tinsdale
Pais coagulated egg medium
Loefflers coagulated serum slant
BIOCHEMICAL
Nitrate reduction (see table)
Catalase (+), Urease & pyrazinamidase (-)
Ferment glucose, maltose but not sucrose
1. Elek plate gel diffusion test
(+) a white precipitin band appears at 45
between filter paper & streak
2. PCR to detect diphtheria toxin gene
3. ELISA, Immunochromatographic strip assay
TOXIGENICITY TEST
Treatment & Prevention
TREATMENT:
Antitoxin
Penicillin G
Erythromycin for penicillin allergic patients
PREVENTION:
DPT (below 7 years old); Td(7 yrs old & above)
Booster dose of toxoid
Completion of immunization & antibiotics
DIPHTHEROIDS
NON-LIPOPHILIC,
FERMENTATIVE :
1) C. ulcerans
2) C. pseudotuberculosis
3) C. minutissimum
4) C. xerosis
5) C. amycolatum
6) C. striatum
NON-LIPOPHILIC, NON-
FERMENTATIVE :
1) C. auris
2) C. pseudodiph-
theriticum
3) C. glucoronolyticum
LIPOPHILIC GROUP:
1. C. jeikeium
Most common isolate from acutely ill patients
Cause bacteremia in immunecompromised
^ mortality rate
2. C. urealyticum
Multi-drug resistant; urease (+)
Associated with chronic UTI
DIPHTHEROIDS
LISTERIA
Listeria monocytogenes
Facultative anaerobe, short GPB, non-AF,non-SF
Tumbling motility
Umbrella motility
Less or non-motile at 35-37
O
C
Catalase & esculin hydrolysis (+)
CHO Fermentation (+) w/ acid, no gas
VIRULENCE FACTORS
Adhesin proteins
Internalin A
Listeriolysin O
ActA
Siderophores
Disease:
LISTERIOSIS
Early onset syndrome:
Granulomatous infantiseptica
Neonatal sepsis
Pustular lesions
Granulomas in organs
Late onset syndrome:
Neonatal meningitis
Meningoencephalitis
bacteremia
Laboratory Diagnosis
SPECIMEN: CSF, blood, amniotic fluid
MICROSCOPY: Short, Gram (+) rods
MOTILITY:
Umbrella shaped
Tumbling motility pattern
CULTIVATION:
BAP: smooth, translucent gray colonies
w/ a narrow zone of hemolysis
Trypticase agar or NA: smooth, translucent
blue-green colonies
CULTURE:
Sheeps BAP, Tryptose Agar, PEA agar
McBride Agar; Nalidixic acid media
BIOCHEMICAL TEST:
Catalase (+)
Ferments glucose, trihalose + salicin
TREATMENT:
ampicillin
erythomycin
trimethoprim-sulfamethoxazole
ERYSIPELOTHRIX:
Erysipelothrix rhusiopathiae
Non-SF, non-motile, no capsule, microaerophilic
single, short chains, long non-branching filaments
Ferments glucose and lactose
BHI w/ 1% glucose; 5% CO
2
at 35-37
O
C
Erysipeloid
Raised, purplish lesion w/ pain,
itchiness, swelling (fingers)
Laboratory Diagnosis
SPECIMEN: aspirates, blood, biopsy specimen
CULTIVATION:
BAP
Gelatin media
Tellurite agar
BIOCHEMICAL TEST:
Catalase-, oxidase-, nitrate-, indole-negative
(+)H2S in TSI
NOCARDIA
Gram (+),catalase & urease (+); partially AF
Long, thin, branching, Strictly aerobic bacilli
Non-fastidious, isolation (1 week or more)
heaped irregular waxy colonies or aerial
filaments
Impairs cell-mediated immune response
DISEASES:
NOCARDIOSIS
Inhalation of the
organism
Begins as chronic
lobar pneumonia
Mimics TB
Dissemination may
occur
Madura foot
Localized,slow
progressing chronic
infection;destructive
but often painless
Caused by a
filamentous branching
bacteria or a fungus
DISEASES:
ACTINOMYCETOMA
LABORATORY DIAGNOSIS
SPECIMEN: Sputum, pus, CSF, biopsy
MICROSCOPY:
GS = rods, coccobacillary form or tangled
masses of branching rods
Modified AFS = mostly acid fast
CULTURAL CHARACTERISTICS
+ waxy, _____________ colonies with aerial hyphae
+ urease (+); growth in milk enhances acid fastness
TREATMENT
Trimethoprim-Sulfamethoxazole
Amikacin, imipenem, Minocycline,
cefotaxime
Surgical drainage or resection
ACTINOMYCES
Non-acid fast; facultatively anaerobe
Rod, coccoid or coryneform
No mycelium; branching filaments may be
produced
DISEASE:
Actinomycosis
A chronic, suppurative & granulomatous
infection
pyrogenic lesions w/ interconnecting sinus
tracts that contain granules
Initiated by trauma
Cervicofacial, thoracic, abdominal
SPECIMEN: Pus,sputum,tissue
CULTURE:
BHI and THIO at 37
O
C
Filaments break into short
chains & coccobacillary forms
after 24 - 48 hours
MOLAR TOOTH colonies
LABORATORY DIAGNOSIS
PROPIONIBACTERIUM
Facultative anaerobic organism
Non-spore forming, non-motile
Irregular rods, branched forms
Optimum temperature at 30
O
C
Normal flora of skin, oral, GIT, ears
Metabolize carbohydrate and lactate
Convert lactic acid to propionic acid and CO
2
Propionibacterium acnes
Considered opportunistic
Implicated in acne vulgaris, endocarditis, shunt
infections
Produce lipases that split free FA from skin lipids
CULTURE:
On anaerobic BAP
1-2mm in diameter, circular, entire, convex,
glistening and opaque
some produce a narrow zone of hemolysis
Assignment :
Discuss the purpose & procedures of the
following tests
a. Strings of Pearl Test
b. Ascoli test
c. Naglers reaction
d. Schicks Test
e. Cold enrichment technique
Mycobacterium
Acid Fast Bacilli
LEARNING OBJECTIVES
At the end of this unit, the student is able to:
Identify the medically significant Mycobacterium
species;
Differentiate based on phenotypic characteristics,
pathogenicity and virulence factors of M.
tuberculosis and M. leprae;
Recognize the importance of performing
appropriate laboratory procedures in the
diagnosis of mycobacterial infection or disease.
Mycobacterium tuberculosis
Mycobacterium leprae
Mycobacterium avium-intracellulare
Complex (MAC) or (M. avium)
Important Human Pathogens
Tuberculosis
A major public health problem (Phil)
5
th
in 10 leading causes of death
5
th
in 10 leading causes of illness
Philippines ranks 2
nd
to Cambodia in
terms of new smear-positive TB
notification rate (WHO Western Pacific
Region, 1999)
NTP National Tuberculosis Program
Directly Observed Treatment
(DOT)
A strategy to ensure treatment compliance,
providing constant and motivational
supervision to TB patients.
Treatment partner to watch TB patient take
medicines everyday during the whole
course of treatment
H- ISONIAZID (300mg) E- ETHAMBUTOL (800mg)
R- RIFAMPICIN (450mg) S- STREPTOMYCIN (1g)
Z- PYRAZINAMIDE (1g)
Mycobacterium tuberculosis
Characteristics
thin straight rods, 0.4 x 3 m (tissue)
coccoid, filamentous forms (media)
Strongly acid-fast, weakly gram-positive,
obligate aerobic bacilli
acid-fastness due to mycolic acid (lipid)
Resistant to dyes, antibacterial agents,
acids, alkalies; resistant to drying
Lipid-Rich Cell Wall of Mycobacterium
Mycolic acids
CMN Group:
Unusual cell wall lipids
(mycolic acids,etc.)
(Purified Protein Derivative)
M. Tuberculosis
Virulence Factors
Mycoside
Wax D
adjuvant
Sulfatides
Inhibit
phagosome-
lysosome fusion
Cord factor
virulent strains
serpentine
cords
Pathogenesis of Tuberculosis
Inhalation of small (>25 m) droplet
nuclei containing M. tuberculosis
expelled by coughing, sneezing, or
talking of another individual with cavitary
tuberculosis
Deposited into alveoli;
Primary infection of non-immune
alveolar macrophages with
unrestrained proliferation within the
infected macrophages
Pathogenesis of Tuberculosis
A. Two Principal lesions
1. Exudative type acute inflammatory
reaction, seen in lung tissue, resembles
bacterial pneumonia; tuberculin test
positive
2. Productive type fully developed,
chronic granuloma with 3 zones:
i. Central area, multinucleated giant cells
ii. Mid zone, pale epitheloid cells
iii. Peripheral zone, lymphocytes, other cells
Diagram
of
Granuloma
NOTE: ultimately a
fibrin layer develops
around granuloma
(fibrosis), further
walling off the
lesion.
Typical progression
in pulmonary TB
involves caseation,
calcification and
cavity formation.
The Ghon lesion
Pathogenesis of Tuberculosis
B. Spread of Organisms in the Host
Dissemination of infected macrophages
through the draining lymphatics into the
bloodstream (to all organs miliary), &
via bronchi and GIT (swallowed)
C. Intracellular Site of Growth
Establish in tissue, in monocytes, RES,
giant cells (difficult to treat)
Clinical Features of Tuberculosis
COUGH
DYSPNEA
FEVER
WEIGHT LOSS
*Apical cavitary
lesions (x-ray)
* Positive tuberculin
skin test with PPD
(purified protein
derivative)
*not diagnostic of TB
wasting condition
Laboratory Diagnosis of Tuberculosis
Specimens:
fresh sputum, gastric washings, urine,
pleural fluid, CSF, joint fluid, biopsy
material, blood, or other suspected
material
Decontamination & Concentration of
Specimens:
Liquefied w/ N-acetyl-L-cysteine
Decontaminated w/ NaOH
Neutralized w/ buffer
Concentrated by centrifugation
STAINS (Review previous notes)
Ziehl-Neelsen technique (hot)
Kinyoun stain (cold)
95% ethyl alcohol containing 3%
hydrochloric acid (acid alcohol)
Fluorochrome stains more sensitive
yellow-orange fluorescence
auramine, rhodamine
Laboratory Diagnosis of
Tuberculosis
Confirmatory Tests:
Culture, Identification & Susceptibility Testing
DNA detection
Culture of acid-fast bacilli
Selective agar parallel with broth media
35-37C in 5-10% CO
2
, up to 8 weeks
2 sets: light and dark conditions
Lwenstein-Jensen: Egg Base Medium
Buff-colored, irregular grainy, bumpy, cauliflower
appearance of TB colonies
Middlebrook 7H10: Agar Base Medium
Liquid broth: BACTEC 12B Medium
10 days isolation
RUNYON CLASSIFICATION
important to characterize and separate
M. tuberculosis from all other species of
mycobacteria.
RUNYON CLASSIFICATION
TB COMPLEX
M. tuberculosis, M. leprae, M. bovis
I SLOW GROWING PHOTOCHROMOGENS
pigment in light condition
II SLOW GROWING SCOTOCHROMOGENS
pigment in light and dark conditions
III SLOW GROWING NONCHROMOGENS
M. Avium complex
IV RAPID GROWERS
Biochemical Tests for the
Identification of Mycobacteria
Niacin accumulation
Nitrate reduction
Pyrizinamidase
Tween 80 hydrolysis
Urease
Arylsulfatase
Iron uptake
Differential Characteristics of Commonly
Isolated Mycobacterium spp.
Mycobacterial Clinical Syndromes
Mycobacterium leprae
Morphology is similar to M. tuberculosis
Unable to be cultured on artificial
media
Diagnosis:
Ospecific skin test (tuberculoid form)
O acid fast stain, microscopy
(lepromatous form)
oCulture cannot be used
Mycobacterium leprae
Virulence:
Capable of intracellular growth
Disease primarily from host response
Epidemiology:
oCommon in Asia, Africa
oArmadillos naturally infected (reservoir)
oDirect contact or inhalation of infectious
aerosols
Mycobacterium leprae
Disease Hansen disease/LEPROSY:
Tuberculoid leprosy (TT)
Lepromatous leprosy (LL)
Intermediate form (Borderline)
Treatment, Prevention, & Control
Dapsone w/ or w/ rifampin for TT
Add clofazimine for LL
Control prompt recognition &
treatment of infected people
Tuberculoid vs. Lepromatous Leprosy
Clinical Manifestations and Immunogenicity
Mycobacterium avium-intracellulare
Physiology and structure similar to M.
tuberculosis
Capable of intracellular growth
Occurs worldwide, acquired by ingestion
of contaminated water or food or
inhalation of infectious aerosols
Greatest risk immunocompromised
(patients w/ AIDS); long-standing
pulmonary disease
Mycobacterium avium-intracellulare
Asymptomatic
colonization
Chronic localized
pulmonary disease
Disseminated
disease, AIDS
patients
Tx: clarithromycin or
azithromycin w/
ethambutol & rifabutin
M. avium-intracellulaire Complex (MAC)
Progression vs. CD4 Count in AIDS Patients
223
Mycobacteria bovis
similar to M. tuberculosis
the primary cause of tuberculosis in
cattle
Humans can acquire M. bovis from cattle
by drinking unpasteurized milk if the cow
has not been vaccinated
A unique identifying characteristic - it
is susceptible to Thiophene-2-carboxylic
acid hydrozide (TCH)
Vous aimerez peut-être aussi
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
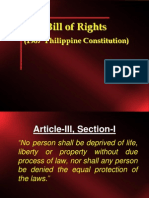
- Bill of Rights: (1987 Philippine Constitution)Document19 pagesBill of Rights: (1987 Philippine Constitution)Kesha Marie TalloPas encore d'évaluation
- D. Concept of Constitution: Philippine Government and ConstitutionDocument13 pagesD. Concept of Constitution: Philippine Government and ConstitutionKesha Marie TalloPas encore d'évaluation
- Billofrightslecture 3Document17 pagesBillofrightslecture 3Kesha Marie TalloPas encore d'évaluation
- Bill of Rights: (1987 Philippine Constitution)Document41 pagesBill of Rights: (1987 Philippine Constitution)Kesha Marie TalloPas encore d'évaluation
- Philippine Government in HistoryDocument25 pagesPhilippine Government in HistoryKesha Marie TalloPas encore d'évaluation
- 09 Metabolism Part 2Document34 pages09 Metabolism Part 2Kesha Marie TalloPas encore d'évaluation
- 09 Metabolism Part 1Document31 pages09 Metabolism Part 1Kesha Marie TalloPas encore d'évaluation
- Nutrition BiochemDocument45 pagesNutrition BiochemKesha Marie TalloPas encore d'évaluation
- Lipids Chemistry GuideDocument88 pagesLipids Chemistry GuideKesha Marie TalloPas encore d'évaluation
- Kesha BiochemDocument4 pagesKesha BiochemKesha Marie TalloPas encore d'évaluation
- Nucleic acidsLECTUREDocument116 pagesNucleic acidsLECTUREKesha Marie TalloPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Daftar Obat High AlertDocument2 pagesDaftar Obat High Alertayu aPas encore d'évaluation
- Multiple Births Definition, Causes & CareDocument11 pagesMultiple Births Definition, Causes & CareCacing UcilPas encore d'évaluation
- Firstaid ModuleDocument143 pagesFirstaid Moduleretni wulandariPas encore d'évaluation
- DetailsDocument21 pagesDetailskanthavelPas encore d'évaluation
- (ANES) Mon 01 Epidural For Labor Analgesia (A2021)Document3 pages(ANES) Mon 01 Epidural For Labor Analgesia (A2021)Miguel SantosPas encore d'évaluation
- CEO Administrator Healthcare Management in San Antonio TX Resume Robert WardDocument3 pagesCEO Administrator Healthcare Management in San Antonio TX Resume Robert WardRobertWard2Pas encore d'évaluation
- Atlantis Implant Compatibility Chart 79214-US-1107Document2 pagesAtlantis Implant Compatibility Chart 79214-US-1107Jean-Christophe PopePas encore d'évaluation
- Care of High Risk Newborn - ChaboyDocument9 pagesCare of High Risk Newborn - Chaboychfalguera0% (1)
- 11th Zoology EM Practical NotesDocument11 pages11th Zoology EM Practical NotesBhavana Gopinath100% (1)
- OT AssistantDocument9 pagesOT AssistantIshfaq LonePas encore d'évaluation
- Subfalcine Herniation Damages Cingulate GyrusDocument34 pagesSubfalcine Herniation Damages Cingulate GyrusLorenzo FrancisPas encore d'évaluation
- MRI Monitoring System Provides Safety and MobilityDocument4 pagesMRI Monitoring System Provides Safety and MobilityAchiyat WinataPas encore d'évaluation
- Maths On The Move' - Effectiveness of Physically-Active Lessons For Learning Maths and Increasing Physical Activity in Primary School StudentsDocument22 pagesMaths On The Move' - Effectiveness of Physically-Active Lessons For Learning Maths and Increasing Physical Activity in Primary School Studentsiisu-cmse libraryPas encore d'évaluation
- Sickle Cell Diet and NutritionDocument30 pagesSickle Cell Diet and NutritiondaliejPas encore d'évaluation
- 110 TOP SURGERY Multiple Choice Questions and Answers PDF - Medical Multiple Choice Questions PDFDocument11 pages110 TOP SURGERY Multiple Choice Questions and Answers PDF - Medical Multiple Choice Questions PDFaziz0% (1)
- Statement On Controlled Organ Donation After Circulatory DeathDocument10 pagesStatement On Controlled Organ Donation After Circulatory DeathHeidi ReyesPas encore d'évaluation
- CQC Inspection ReportDocument17 pagesCQC Inspection ReportMark RushworthPas encore d'évaluation
- The Art of Healthy Eating KidsDocument122 pagesThe Art of Healthy Eating KidsSenka SkenderovicPas encore d'évaluation
- Anderson2008 Levofloxasin A ReviewDocument31 pagesAnderson2008 Levofloxasin A ReviewFazdrah AssyuaraPas encore d'évaluation
- Nexthealth - Semantic Web Sparks Evolution of Health 2.0 - A Road Map To Consumer-Centric HealthcareDocument7 pagesNexthealth - Semantic Web Sparks Evolution of Health 2.0 - A Road Map To Consumer-Centric HealthcareMaarten den Braber100% (43)
- Malaysia - Kontrak - Pusat - Ubat-Ubatan - KKM - 20.03.12Document21 pagesMalaysia - Kontrak - Pusat - Ubat-Ubatan - KKM - 20.03.12Anuj Mairh0% (1)
- BSP Price List Agustus 2020Document46 pagesBSP Price List Agustus 2020Anonymous aaAQ6dgPas encore d'évaluation
- 2023 - Clinical Scales For Headache Disorders (Pınar Yalınay Dikmen Aynur Özge)Document318 pages2023 - Clinical Scales For Headache Disorders (Pınar Yalınay Dikmen Aynur Özge)César Escobar100% (1)
- Jan Marc Bulatao 10-Einstein BiologyDocument3 pagesJan Marc Bulatao 10-Einstein BiologyNomer SenadorPas encore d'évaluation
- Nursing Management of Pressure Ulcers in Adults PDFDocument33 pagesNursing Management of Pressure Ulcers in Adults PDFAnindi Vivia MuktitamaPas encore d'évaluation
- HEALTHY JUICES AND THEIR BENEFITSDocument7 pagesHEALTHY JUICES AND THEIR BENEFITSdeepaliPas encore d'évaluation
- Hypertension: Rojina Bhurtel Lecturer MmihsDocument36 pagesHypertension: Rojina Bhurtel Lecturer MmihsRojina Bhurtel100% (2)
- ICU protocol 2015 قصر العيني by mansdocsDocument227 pagesICU protocol 2015 قصر العيني by mansdocsWalaa YousefPas encore d'évaluation
- Desai - Palliative Medicine in Myelodysplastic Syndromes - Patients and Caregivers - A Qualitative StudyDocument5 pagesDesai - Palliative Medicine in Myelodysplastic Syndromes - Patients and Caregivers - A Qualitative StudyRafael TerceiroPas encore d'évaluation
- DLP in MAPEH - Grade 9 Myths and Misconceptions About DrugsDocument4 pagesDLP in MAPEH - Grade 9 Myths and Misconceptions About DrugsMa. Reina Gail T. Lizaso100% (5)