Académique Documents
Professionnel Documents
Culture Documents
Otkazivanje Srca I Cirkulatorni Šok
Transféré par
Tatjana PopovicTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Otkazivanje Srca I Cirkulatorni Šok
Transféré par
Tatjana PopovicDroits d'auteur :
Formats disponibles
Otkazivanje srca i cirkulatorni ok
Otkazivanje srca
Function of the heart
Move deoxygenated blood from the venous system through the right heart into the pulmonary circulation Move the oxygenated blood from the pulmonary circulation through the left heart into the arterial system
Right and left heart must maintain an equal output to function properly
Right Heart Failure
Represents failure of the right heart to pump blood forward into the pulmonary circulation
Blood backs up in the systemic circulation
Causes peripheral edema and congestion of the abdominal organs
Left Heart Failure
Represents failure of the left heart to move blood from pulmonary circulation into system circulation
Blood backs up in the pulmonary circulation
Causes of Heart Failure
Myocardial disease
Cardiomyopathies Myocarditis Coronary insufficiency Myocardial infarction
Causes of Heart Failure (cont.)
Valvular heart disease
Stenotic valvular disease Regurgitant valvular disease
Congenital heart defects Constrictive pericarditis
Cardiac Output
Cardiac output: the amount of blood the heart pumps each minute
Cardiac output = heart rate x stroke volume
Heart rate: how often the heart beats each minute
Regulated by a balance between the activity of the sympathetic sympathetic nervous system (increases heart rate), and the parasympathetic nervous system (slows heart rate)
Cardiac Output (cont.)
Stroke volume: how much blood the heart pumps with each beat
A function of preload, afterload, and cardiac contractility
Maintenance of Cardiac Reserve in Heat Failure
Compensatory or adaptive mechanisms
Frank-Starling mechanism Activation of neurohumoral influences such as the sympathetic nervous system The renin-angiotensin-aldosterone mechanism Natriuretic peptides Locally-produced vasoactive substances Myocardial hypertrophy and remodeling
Causes of Heart Failure
Acute myocardial infarction Hypertension Degenerative conditions of the heart muscle known collectively as cardiomyopathies Excessive work demands (hypermetabolic states) Volume overload (renal failure)
Descriptions of Heart Failure
High-output or low-output failure Systolic or diastolic failure Right-sided or left-sided failure
Conditions that restrict blood flow into the lungs Stenosis or regurgitation of the tricuspid or pulmonic valves Right ventricular infarction Cardiomyopathy Persistent left-sided failure Acute or chronic pulmonary disease (cor pulmonale)
Causes of Right-Sided Heart Failure
Acute myocardial infarction Cardiomyopathy
Causes of Left-Sided Heart Failure
Physiologic effects of the impaired pumping ability of the heart Decreased renal blood flow Activation of the sympathetic compensatory mechanisms
Manifestations of Heart Failure
Signs and Symptoms of Heart Failure
Fluid retention and edema Shortness of breath Fatigue and limited exercise tolerance Cyanosis Cachexia and malnutrition Distention of the jugular veins in rightsided failure Diaphoresis and tachycardia
Class I: patients with cardiac disease but without resulting limitations in physical activity Class II: patients with heart disease resulting in slight limitations of physical activity Class III: patients with cardiac disease resulting in marked limitation of physical activity Class IV: patients with cardiac disease
Functional Classification of Patients with Heart Disease (NY Heart Association)
Goals of Treatment for Chronic Heart Failure
Relieving the symptoms and improving the quality of life Long-term goal:
Slowing, halting, or reversing the cardiac dysfunction
Treatment Measures for Chronic Heart Failure
Correction of reversible causes Surgical repair of a ventricular defect or an improperly functioning valve Pharmacologic and non-pharmacologic control of afterload stresses Modification of activities and lifestyle consistent with the functional limitations of a reduced cardiac reserve Use of medications to improve cardiac function and limit excessive
Acute Pulmonary Edema
Capillary fluid moves into the alveoli, causes lung stiffness, makes lung expansion more difficult, and impairs the gas exchange function of the lung With the decreased ability of the lungs to oxygenate the blood, the hemoglobin leaves the pulmonary circulation without being fully oxygenated
Results in shortness of breath and cyanosis
Causes of Cardiogenic Shock
Damage to the heart from myocardial infarction Ineffective pumping caused by cardiac arrhythmias Ventricular septal defect Ventricular aneurysm Acute disruption of valvular function Problems associated with open heart surgery
Hypovolemic
Classification of Circulatory Shock
Loss of whole blood Loss of plasma Loss of extracellular fluid
Obstructive
Inability of heart to fill properly Obstruction to outflow from the heart
Distributive
Classification of Circulatory Shock (cont.)
Loss of sympathetic vasomotor tone Presence of vasodilating substance in the blood Presence of inflammatory mediators
Causes of Hypovolemic Shock
Diminished blood volume with inadequate filling of the vascular compartment Acute loss of 15% to 20% of the circulating blood volume
External loss of whole blood (e.g., hemorrhage), plasma (e.g., severe burns), or extracellular fluid (e.g., gastrointestinal fluids lost in vomiting or diarrhea)
Internal hemorrhage or from third-space losses
Stages of Hypovolemic Shock
Initial stage: the circulatory blood volume is decreased, but not enough to cause serious effects Second stage: Compensatory mechanisms are able to maintain blood pressure and tissue perfusion at a level sufficient to prevent cell damage Third stage: Blood pressure begins to fall, blood flow to the heart and brain is impaired, capillary permeability is
Stages of Hypovolemic Shock (cont.)
Fourth and final stage: irreversible shock, even though the blood volume may be restored and vital signs stabilized, death ensues eventually
Types of Shock
Obstructive shock Distributive shock
Neurogenic shock Anaphylactic shock
Sepsis and septic shock
Complications of Shock
Acute respiratory distress syndrome Acute renal failure Gastrointestinal complications Disseminated Intravascular Coagulation Multiple organ dysfunction syndrome
Signs and Symptoms of Heart Failure in Infants and Children
Fatigue Effort intolerance Cough Anorexia Abdominal pain
Vous aimerez peut-être aussi
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Intradialytic Hypertension Time To Act 10Document7 pagesIntradialytic Hypertension Time To Act 10Nia FirdiantyPas encore d'évaluation
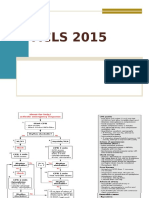
- Acls 2015Document13 pagesAcls 2015I Gede Aditya100% (5)
- Congenital Heart DiseaseDocument120 pagesCongenital Heart Diseasemerin sunilPas encore d'évaluation
- Sympathomimetics in VeterinaryDocument9 pagesSympathomimetics in Veterinaryjose pPas encore d'évaluation
- ACLS Study Guide JULY 2021 UPDATEDocument3 pagesACLS Study Guide JULY 2021 UPDATENina Morada100% (2)
- Endocarditis Pericarditis and Myocarditis Is05 PDFDocument2 pagesEndocarditis Pericarditis and Myocarditis Is05 PDFCeasar Abdilla RahmanPas encore d'évaluation
- Essential Paediatrics Course Book 2023Document88 pagesEssential Paediatrics Course Book 2023alextkijiji_81403773Pas encore d'évaluation
- Aortic Dissection PP PresentationDocument64 pagesAortic Dissection PP PresentationKonstantin DimitrovPas encore d'évaluation
- PR Refkas - Peripartum CardiomyopathyDocument16 pagesPR Refkas - Peripartum CardiomyopathyakmilPas encore d'évaluation
- Cardiovascular System (Anatomy and Physiology)Document93 pagesCardiovascular System (Anatomy and Physiology)Butch Dumdum86% (7)
- Deviriligo Notes 12Document99 pagesDeviriligo Notes 12A Fish100% (1)
- Heart Failure: Dr.K.Sathish Kumar, MD (Hom) .Document11 pagesHeart Failure: Dr.K.Sathish Kumar, MD (Hom) .mnr hmcPas encore d'évaluation
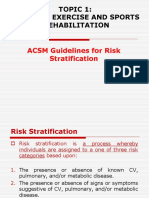
- Chapter 1.2 Algorithym of Risk StratificationDocument26 pagesChapter 1.2 Algorithym of Risk StratificationMUHAMMAD DANISH AMIN BIN BORHANUDDINPas encore d'évaluation
- Management of CRAODocument3 pagesManagement of CRAOvenniePas encore d'évaluation
- Olahraga Sebagai Pencegahan Penyakit Jantung KoronerDocument6 pagesOlahraga Sebagai Pencegahan Penyakit Jantung KoronerGrace YutoPas encore d'évaluation
- Congenital Heart Disease Screening Modified Peds.2017-4065.FullDocument9 pagesCongenital Heart Disease Screening Modified Peds.2017-4065.FullRene H. Framcisco, MDPas encore d'évaluation
- Ekg Primeri PDFDocument21 pagesEkg Primeri PDFStevanovic StojaPas encore d'évaluation
- Myocardial InfarctionDocument43 pagesMyocardial InfarctiondeeptiPas encore d'évaluation
- Indikasi TrombektomiDocument6 pagesIndikasi TrombektomiNatasha BastiaanPas encore d'évaluation
- Acidity Theory of AtherosclerosisDocument46 pagesAcidity Theory of Atherosclerosissecretary6609Pas encore d'évaluation
- CAD - Ischemic Heart Disease: AtherosclerosisDocument5 pagesCAD - Ischemic Heart Disease: Atherosclerosisbri ngPas encore d'évaluation
- CardiomyopathyDocument17 pagesCardiomyopathysarguss1450% (2)
- Bls Study GuideDocument2 pagesBls Study GuideJohnPas encore d'évaluation
- Entresto Marketing PlanDocument1 pageEntresto Marketing PlanSalmanAhmedPas encore d'évaluation
- 1Document24 pages1Noey TabangcuraPas encore d'évaluation
- Singkatan Diagnosa A-ZDocument23 pagesSingkatan Diagnosa A-ZElisabeth AnitaPas encore d'évaluation
- Cases in Cardio PediatricDocument298 pagesCases in Cardio Pediatricmarie saul100% (3)
- Obstetrical Shock FinalDocument25 pagesObstetrical Shock Finalsanthiyasandy100% (1)
- How To Write A Proposal EssayDocument3 pagesHow To Write A Proposal Essaypilav0wutyk3100% (2)
- DefibrillatorDocument2 pagesDefibrillatorVasanth VasanthPas encore d'évaluation